ABSTRACT
Kaposi sarcoma (KS) is caused by Human Herpesvirus 8 (HHV-8), and it affects 15 times more common in men than women. It has varied clinical presentation from classic, endemic, organ transplant-related, and acquired immunodeficiency syndrome (AIDS)-related.
Clinical features of pulmonary KS might be challenging to distinguish from pneumonia in immunocompromised patients and could lead to diagnostic challenges. Hence Pulmonary KS should also be considered in the differential when HIV-infected patients develop rapidly progressive respiratory symptoms after the initiation of glucocorticoid therapy and immunocompromised not responding to antibiotic treatment for pneumonia, especially when CD4 < 100 and viral load >10,000. Early diagnosis and treatment are essential for a better outcome and prevent morbidity and mortality. Highly active antiretroviral therapy (HAART) is the only proven therapy to prevent Kaposi sarcoma. We report the case of a young woman who presented with symptoms of pneumonia and was later found to have pulmonary KS (PKS).
1. Introduction
Moritz von Kaposi first described Kaposi sarcoma (KS) in 1872 as a low-grade mesenchymal tumor involving blood and lymphatic vessels. It is caused by a herpes virus, called Human Herpesvirus 8 (HHV-8), or Kaposi sarcoma-associated herpesvirus (KSHV). It affects 15 times more men than women [Citation1]. Keeping the immune system strong with antiretroviral therapy (HAART) is the best-known way to prevent Kaposi sarcoma. The mucocutaneous sites are primarily affected, typically the skin of the lower extremities, face, trunk, genitalia, and oropharyngeal mucosa; other organs are involved in the disseminated form of the disease. This disease is recognized to arise as four variants, each presenting a different clinical manifestation: classic or sporadic, African or endemic, organ transplant-related or iatrogenic, and acquired immunodeficiency syndrome (AIDS)-related or epidemic
We report the case of a young woman who presented with symptoms of pneumonia and was later found to have pulmonary KS (PKS). It occurred within a few months of the diagnosis of AIDS. Her CD4 count and viral load were 167 and 159447 respectively
2. Case report
A 33 year- old- African female (currently in the US for a visit only), recently diagnosed with HIV and adrenal insufficiency four months back, presented with hemoptysis, fever, left-sided chest pain, and worsening shortness of breath for a couple of days. She had a loss of appetite and unintentional weight loss of 7 LB in a month. The rest of the review of symptoms was negative. On admission, she had a fever with a temperature of 101 F, tachycardia with Pulse of 116 bpm, tachypnea with a respiratory rate of 20, and Blood pressure of 97/69 mmHg. Physical exam was significant for slightly pale conjunctiva, diffuse lymphadenopathy in the cervical, bilateral axillary, inguinal region, and on chest examination bilateral crackles were heard.
She was admitted twice within four months for similar complaints. With the initial provisional diagnosis of Pneumocystis jiroveci (PJP) and community-acquired pneumonia, she was treated with high dose intravenous steroids and broad-spectrum intravenous antibiotics. However, during the first admission, PJP pneumonia and tuberculosis of lungs were ruled out by bronchoscopy with negative BAL and three sets of negative Acid-fast bacilli (AFB), respectively. Again, after three weeks, she presented with similar symptoms, and the course of management remained the same. However, she had persistently low blood pressure, which was responsive to steroids. After the cosyntropin test, she was also diagnosed with Addison's disease and was continued on low dose steroid post-discharge.
As per the patient, the HIV test was negative six months back and was diagnosed with HIV four months ago for the first time during her early admission to this hospital. Patient-reported, she never had unprotected sex, and there was no history of blood transfusion. However, she had a history of being raped 15 years ago. She lives with her husband, who was also recently diagnosed with HIV in Nigeria before visiting the US. He denied a history of multiple sex partners and MSM (Men who have sex with Men).
During this admission, the patient had persistent infiltrate on chest x-ray as compared to the previous admission and remained unchanged even after being treated with antibiotics. CT scan of the chest showed a progression of diffuse airspace consolidation (). The patient was treated with broad-spectrum IV antibiotics, HAART, steroid, and Bactrim. Due to the failure to respond to the treatment, the alternative diagnosis was considered, which included but not limited to diffuse alveolar hemorrhage, Cryptogenic Organizing Pneumonia (COP), Pulmonary vasculitis, nosocomial pneumonia.
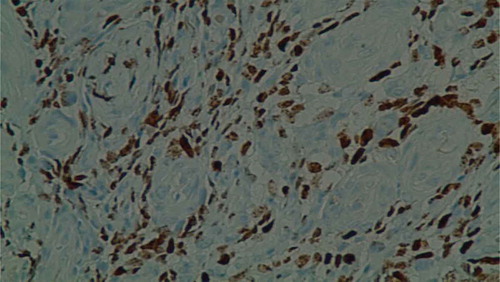
Other investigations included Aspergillus galactomannan Antigen: negative, Gallium scan: negative, CD4 count: 167, Viral load: 159447, Cryptococcal Antigen was positive in serum at 1:20 titer. Although cryptococcal pneumonia is less likely to present with hemoptysis, the patient was treated with fluconazole. During the entire course of the disease, the patient was continued on antiretroviral therapy. During follow up at the clinic, Valganciclovir was also started as the patient presented with tachycardia, and IgG CMV was positive. Vasculitis workup was negative. Sputum showed normal flora, and blood cultures were negative. Left inguinal lymph-node biopsy was done which came back positive for Kaposi sarcoma. Bronchoscopy was repeated with a transbronchial biopsy, which confirmed the KS of the lung (). Due to the failure of treatment with ARVT, antibiotics, antifungal, and antiviral, chemotherapy was considered.
3. Discussion
Kaposi Sarcoma (KS) is the most common malignancy among AIDS-related neoplasm. However, the incidence of KS has decreased significantly with the widespread use of HAART [Citation2]. AIDS associated Kaposi Sarcoma is more common in homosexual or bisexual men and rarely seen in women, especially in resource-rich countries like the USA [Citation3]. These patients with KS typically have a low CD4 cell count (<100 cells per cubic millimeter) and a high HIV viral load (>10,000 copies per milliliter) and less commonly seen in patients who are on HAART [Citation4]. Our patient developed KS while on HAART with a CD4 count of 167, which was not typical but had a higher viral load (159447).
KS at the initial phase, most commonly present with mucocutaneous manifestations like erythematous to violaceous plaque, usually in lower extremities, face (especially the nose), oral mucosa, and genitalia. As the disease progresses, it can involve almost all visceral sites, commonly GI tract and lung. Pulmonary involvement in AIDS-related KS usually occurs in conjunction with a more extensive mucocutaneous disease in about 80 to 90 percent of cases [Citation3,Citation5]. However, pulmonary involvement without mucocutaneous disease as an initial manifestation of KS occurs rarely in about 15 percent as we observe in our patient [Citation6].
The diagnosis of pulmonary KS (PKS) is not straightforward and can be very challenging. This is mainly because of the nonspecific clinical, laboratory presentation and also non-diagnostic radiographic findings. PKS cannot be easily differentiated from other lung diseases that commonly occur in patients with HIV. Thus, clinicians should have a high index of suspicion to diagnose at an early stage.
Apart from clinical suspicion, we also need to look for epidemiological factors (e.g., geographic location, men who have sex with men), presence of mucocutaneous KS lesions, degree of immunodeficiency and radiographic evidence suggestive of KS on chest CT which include hilar densities along peribronchovascular pathways, and a nodular pattern along with pleural effusions [Citation7].
Diagnosis of Pulmonary KS can be made with bronchoscopy without biopsy if characteristic endobronchial lesions (macular red or purple appearance) are present along with radiologic findings, and infection has been excluded. However, in many cases, lung biopsy may be needed to make a definitive diagnosis in cases when the clinical and radiological picture is not typical as in our patients who did not have the characteristic endobronchial lesions, and bronchial biopsy established the diagnosis.
For patients with asymptomatic pulmonary KS, the mainstay of treatment is only ART, whereas the addition of chemotherapy is indicated only for patients who have severe symptomatic pulmonary involvement or evidence of disease progression despite ART. Our patient belonged to the latter group and was planned for chemotherapy.
Atypical nature of clinical and radiographic presentation in a female with relatively higher CD4 count, developing KS while on HAART all these factors made the case complex and more challenging to diagnose. One explanation behind the rapid progression to pulmonary KS in our patient could be the use of systemic glucocorticoids where the patient was taking hydrocortisone for adrenal insufficiency. Research has shown that corticosteroid therapy has been associated with KS induction as well as the exacerbation of preexisting KS in HIV-infected persons [Citation8]. Visceral involvement is also common in KS related to immunosuppression (also known as iatrogenic).
Chemotherapy used for KS is Vinblastine, alitretinoin, pegylated liposomal doxorubicin, or liposomal daunorubicin [Citation9,Citation10]. Systemic chemotherapy is generally used for patients with more advanced KS or when there is evidence of rapid disease progression.
In a case series of 469 cases, the patients with T0 disease had the overall five-year survival of 92 percent, and for those with T1 disease, the five-year survival was 83 percent. T0 group were treated with ART alone, whereas T1 were treated with both ART and chemotherapy [Citation11].
Thus, the possibility of pulmonary KS should be considered strongly with the use of glucocorticoid therapy.
Thus, all clinicians should consider pulmonary KS in HIV-infected patients who present with respiratory symptoms, even without typical mucocutaneous lesion of KS, and have additional risk factors such as the use of immunosuppressant. Early diagnosis and treatment are essential for a better outcome and prevent morbidity and mortality.
4. Conclusion
Kaposi Sarcoma (KS) is the most common malignancy associated with Acquired Immune Deficiency Syndrome (AIDS) and is caused by Human Herpesvirus 8(HHV 8) or Kaposi Sarcoma Herpesvirus (KSHV). Clinical features of pulmonary KS might be challenging to distinguish from pneumonia in immunocompromised patients and could lead to diagnostic challenges. Hence Pulmonary KS should also be considered in the differential when HIV-infected patients develop rapidly progressive respiratory symptoms after the initiation of glucocorticoid therapy and immunocompromised not responding to antibiotic treatment for pneumonia, especially when CD4 < 100 and viral load >10,000. The first-line therapy of KS is with HAART, and the incidence has declined with its use. Systemic chemotherapy may play a role, depending on the extent of the disease.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Antman K, Chang Y. Kaposi’s sarcoma. N Engl J Med. 2000;342(14):1027–1038.
- Lodi S, Guiguet M, Costagliola D, et al. CASCADE Collaboration; Kaposi Sarcoma incidence and survival among HIV-infected homosexual men after HIV seroconversion. J Natl Cancer Inst. 2010;102(11):784–792.
- Beral V, Peterman TA, Berkelman RL, et al. Kaposi’s sarcoma among persons with AIDS: a sexually transmitted infection?. Lancet. 1990;335(8682):123.
- Gill PS, Akil B, Colleti P, et al. Pulmonary Kaposi’s sarcoma: clinical findings and results of therapy. Am J Med. 1989;87(1):57–61.
- Huang L, Schnapp LM, Gruden JF, et al. Presentation of AIDS-related pulmonary Kaposi’s sarcoma diagnosed by bronchoscopy.Am. J Respir Crit Care Med. 1996 Apr;153(4 Pt 1):1385–1390.
- Pinzone MR, Berretta M, Cacopardo B, et al. Epstein-Barr virus- and Kaposi sarcoma-associated herpesvirus-related malignancies in the setting of human immunodeficiency virus infection. Semin Oncol. Apr. 2015;42(2):258–271.
- Wolff SD, Kuhlman JE, Fishman EK. Thoracic Kaposi sarcoma in AIDS: CT findings. J Comput Assist Tomogr. 1993;17(1):60–62.
- Trattner A, Hodak E, David M, et al. The appearance of Kaposi sarcoma during corticosteroid therapy. Cancer. 1993;72(5):1779.
- Epstein JB. Treatment of oral Kaposi sarcoma with intralesional Vinblastine. Cancer. 1993;71:1722.
- Bower M, Collins S, Cottrill C, et al. British HIV association guidelines for HIV-associated malignancies 2008. HIV Med. 2008;9:336.
- Bower M, Dalla Pria A, Coyle C, et al. Prospective stage-stratified approach to AIDS-related Kaposi’s sarcoma. J Clin Oncol. 2014;32(5):409.