ABSTRACT
Dieulafoy lesions are tortuous vascular malformations characterized by thick walled submucosal arteries/large caliber arterioles protruding through a small mucosal defect surrounded by normal mucosa. They can occur in the jejunum/ileum and can cause massive, life-threatening GI bleeding. We present an 80-year-old female with three weeks of black tarry stools, progressive dyspnea on exertion and generalized body weakness with no significant findings on Esophagogastroduodenoscopy (EGD). Push enteroscopy revealed a Dieulafoy lesion in the proximal jejunum and an overlying clot, with oozing of blood noted after clot removal. The lesion was treated with Argon plasma coagulation (APC) and a post-APC fleshy protuberance was clipped to secure hemostasis. It is therefore important to keep a high index of suspicion for jejunal/ileal Dieulafoy lesions in patients with massive GI bleeding of unclear etiology on EGD/colonoscopy.
An 80-year-old female presented with three weeks of black tarry stools, progressive dyspnea on exertion and generalized body weakness. She denied hematemesis, abdominal pain or recent Nonsteroidal anti-inflammatory drug (NSAID) use, and was up to date with colorectal cancer screening. Esophagogastroduodenoscopy (EGD) showed no significant findings to explain her severe anemia.
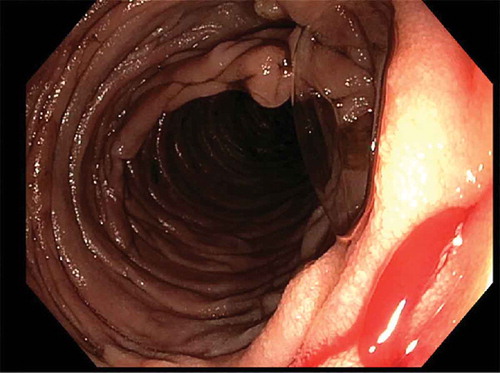
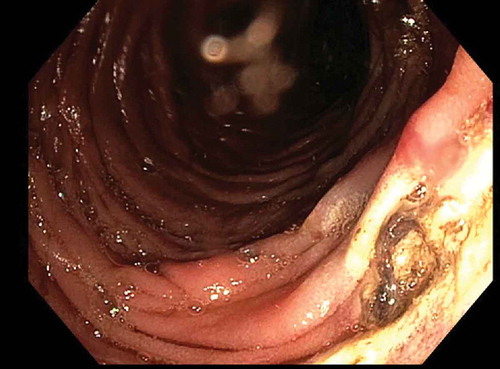
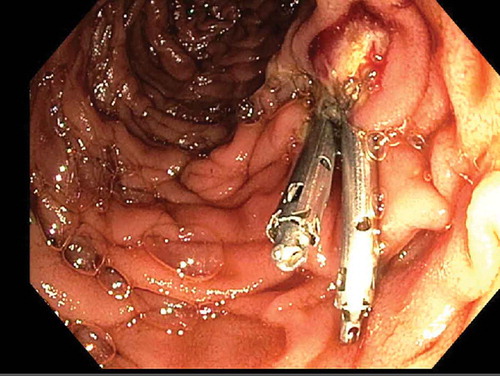
Push enteroscopy revealed a Dieulafoy lesion in the proximal jejunum and an overlying clot, with oozing of blood noted after clot removal (). The lesion was treated with Argon plasma coagulation (APC). There appeared to be a 5–6 mm fleshy protuberance post-APC (), which was clipped (), and hemostasis was achieved. She was subsequently discharged from the hospital with no complications.
Figure 3. Dieulafoy lesion in the proximal jejunum followed by clipping of 6 mm fleshy protuberance.
Dieulafoy lesions are tortuous vascular malformations characterized by thick walled submucosal arteries/large caliber arterioles protruding through a small mucosal defect surrounded by normal mucosa [Citation1–Citation4]. They are uncommon lesions and contribute to 1–2% of acute Gastrointestinal (GI) bleeds [Citation3,Citation5]. Dieulafoy lesions can occur throughout the GI tract- typically in the stomach (61 – 82%) and duodenum (15%), but may be seen in the jejunum or ileum (1%) [Citation5]. Dieulafoy lesions are more commonly seen in elderly males and often associated with NSAID use causing mucosal atrophy and ischemia. However, it may be seen in females without NSAID use. Small mucosal defect and intermittent bleeding can make it difficult to diagnose Dieulafoy lesions but active bleeding may be beneficial in identifying the lesion during EGD [Citation4]. Endoscopic management options include banding, clipping, electrocautery, cyanoacrylate glue, sclerotherapy, epinephrine injection, and laser photocoagulation.
Dieulafoy lesions can cause massive, life-threatening GI bleeding. It is therefore important to keep a high index of suspicion for jejunal/ileal Dieulafoy lesions in patients with massive GI bleeding of unclear etiology on EGD/colonoscopy.
Disclosure statement
The authors report no conflicts of interest.
References
- Johnson A, Oger M, Capovilla M. Dieulafoy lesion of the appendix. Digestive Liver Dis. 2014;46(9):e11.
- Thimmapuram J, Shah M, Srour J. Esophageal Dieulafoy lesion: an unusual cause of GI bleeding. Gastrointest Endosc. 2011;73(5):1055–1056.
- Baxter M, Aly EH. Dieulafoy’s lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010;92(7):548–554.
- Kozan R, Gülen M, Yılmaz TU, et al. Massive lower gastrointestinal bleeding from a jejunal Dieulafoy lesion. Ulus Cerrahi Derg. 2014;30(4):225–227.
- Nojkov B, Cappell MS. Gastrointestinal bleeding from Dieulafoy’s lesion: clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc. 2015;7(4):295–307.