ABSTRACT
Ventricular stand still is an electrophysiologic phenomenon characterized by the absence of ventricular activity or contraction. It is the result of the lack of impulse formation in ventricles (absence of idioventricular automaticity) or the failure of impulse transmission to ventricles (conduction disturbance) [1]. It is an uncommon condition that can affect a wide range of age groups with life threatening consequences. There are no set guidelines on the treatment of ventricular standstill – swift and sound clinical judgment is required. The condition should be treated as a cardiac arrest, with resolution of precipitating factors. Here we present a case of a 59-year-old man with multiple comorbidities, who presented with massive gastrointestinal hemorrhage and recurrent episodes of ventricular standstill during hospitalization, with his immediate treatment and stabilization.
1. Introduction
Ventricular standstill is a rare electrophysiologic phenomenon. As the name implies, the ventricles stop pumping, resulting in no effective cardiac output during the phenomenon. It is a potentially fatal rhythm disorder and need immediate diagnosis and treatment [Citation1,Citation2]. We report a case of recurrent episodes of ventricular standstill in a patient who presented with acute massive gastrointestinal hemorrhage.
2. Case presentation
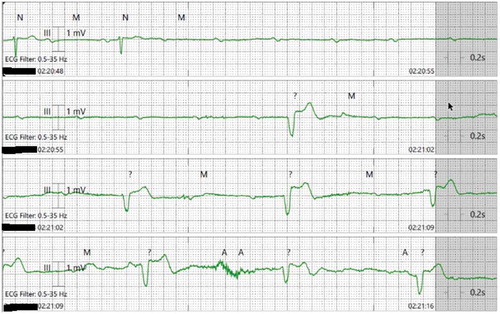
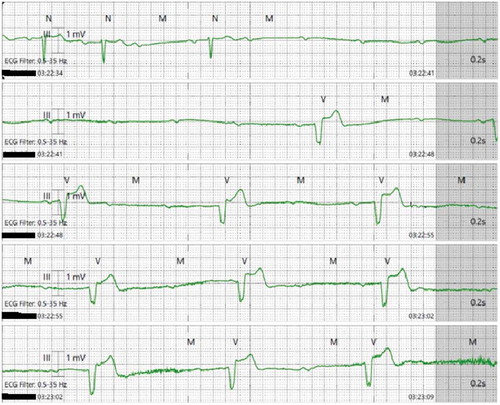
A 59-year-old man was admitted for fatigue and bright red bleeding per rectum. Otherwise he denied other complaints. There was no history of prior bleeding event. He has pertinent medical history of hypertension, diabetes, left ventricular diastolic dysfunction and chronic kidney disease stage 3. He is on metoprolol tartrate 100 mg twice a day (BID), furosemide 40 mg BID, nifedipine 50 mg daily (QD) and hydralazine 75 mg thrice daily (TID), insulin regimen, and duloxetine 100 mg BID. Vital signs were blood pressure (BP) of 146/80 mmHg, heart rate (HR) of 67 beats per minute (bmp), oxygen saturation of 98% on room air. Physical exam was benign except significant pallor. Lab studies showed hemoglobin of 6.0 g/dl, hematocrit 20%, platelet 145 109/L, INR 0.9, creatinine 2.5 mg/dl, eGFR 26 ml/min (baseline Cr 1.9, eGFR 36). He was volume resuscitated and admitted to medical intensive care unit (MICU) for further care. Home BP medications were held. Two units of packed red blood cells (pRBCs) were transfused. Overnight, the patient remained stable without any reported arrhythmias on telemetry, until he had recurrent episodes of rectal bleeding. During the first bout of gastrointestinal (GI) bleeding, the patient had a syncopal episode with spontaneous return of consciousness within 3–5 seconds. Telemetry showed ventricular standstill of 10–11 seconds with ectopic ventricular beats (EVBs) []. The patient was given a dose of intravenous (IV) atropine 0.5 mg and was kept on a transcutaneous pacer. About an hour later, he had another episode of recurrent GI bleeding, associated with a few seconds of syncope. Telemetry showed 9–10 seconds of ventricular standstill with frequent EVBs []. Temporary transvenous pacemaker was placed urgently. Eventually, a permanent dual-chamber pacemaker was implanted. Subsequent esophago-gastro-duodenoscopy (EGD) showed acute gastritis without active bleeding. Colonoscopy showed diverticulosis of sigmoid and descending colon without active bleeding. The patient remained stable without recurrent episodes of bleeding or arrhythmias. The patient was discharged in stable condition. 8 weeks later, he remained stable and the device was functioning properly at follow up in electrophysiology clinic.
3. Discussion
Characterized by absence of ventricular activity or contraction, ventricular standstill is the result of the lack of impulse formation in ventricles (absence of idioventricular automaticity) or failure of impulse transmission to ventricles (conduction disturbance) [Citation1]. It may happen in different age groups from a toddler to an octogenarian [Citation3]. With intact cardiac conduction system, idioventricular pacemakers (slower rate) are suppressed by supraventricular pacemakers (faster rate), mainly the sinoatrial pacemaker. This phenomenon is termed ‘overdrive suppression’ [Citation1,Citation4]. Abnormally prolonged ventricular standstill can be caused by exaggerated overdrive suppression, which happens when the factors promoting overdrive suppression are enhanced or those decreasing overdrive suppression are inhibited. Sander-Jensen et al. reported that bradycardia may occur in acute hemorrhage and is mediated by increased vagal cholinergic tone [Citation5]. Sometimes, increased vagal tone is so strong that it can block not only the AV node, but also the ventricular automaticity [Citation6]. The finding of vagally mediated reflex bradycardia in the setting of hypotensive hemorrhage was proven in animal studies as well [Citation7].
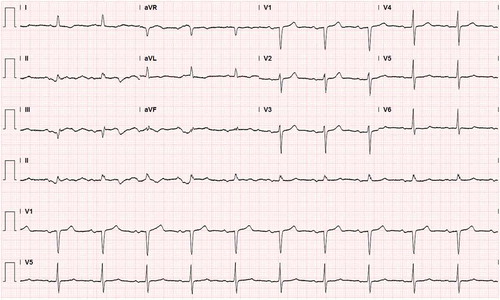
In acute massive hypovolemia, bradycardia could be a protective reflex in order to improve ventricular filling [Citation8]. In our patient, sympathetic adrenergic activity is blocked by his home medication metoprolol. Subsequently, increased vagal cholinergic tone in the setting of acute GI hemorrhage and severe anemia leads to prolonged ventricular standstill. The patient’s pre-existing conduction system disease, as evidenced in baseline EKG (), may have played a role as well.
Both ventricular standstill and ventricular fibrillation clinically manifest as cardiac arrest through different mechanisms. The former is usually due to failure of impulse formation altogether while the latter is owing to the lack of organized ventricular activity despite the presence of continuous chaotic micro-reentrant ventricular depolarizations [Citation1,Citation2]. Since there is no effective cardiac output in ventricular standstill, the patient is clinically dead and cardiopulmonary resuscitation should be initiated immediately for acute management. Temporary pacemakers maybe a bridging therapy. Criley et al. reported VF cardiac arrest patients who ‘self-resuscitated through cough-CPR’. In our patient, no signs of self-resuscitation was noted. Nor was external CPR initiated. The patient regained consciousness spontaneously with EVBs.
There has been no guideline for treatment of ventricular standstill. Treatment is generally based on clinical judgement. In our patient, because of recurrent events of prolonged ventricular standstill and syncope, the decision was made to implant dual chamber pacemaker. The patient remained stable without recurrent events or arrhythmia at 8 weeks’ follow-up.
4. Conclusion
Ventricular standstill is a rare electrophysiologic phenomenon and can be life threatening. Immediate CPR may be necessary to revive the heart or restore the vital circulation. Treatment largely depends on clinical judgment.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Vassalle M. On the mechanisms underlying cardiac standstill: factors determining success or failure of escape pacemakers in the heart. J Am Coll Cardiol. 1985 Jun 1;5(6 Supplement 1):35B–42B.
- Hammond C. Ventricular fibrillation and standstill. RN. 1984 Apr 1;47(4):120–121.
- Lynch RM, Ballesty L, Maicoo R. “Be still my beating heart”: ventricular standstill occurring in different age groups. Afr J Emergency Med. 2014 Dec 1;4(4):e12–5.
- Vassalle M. The relationship among cardiac pacemakers. Overdrive suppression. Circ Res. 1977 Sep;41(3):269–277.
- Sander-Jensen K, Secher NH, Bie P, et al. Vagal slowing of the heart during haemorrhage: observations from 20 consecutive hypotensive patients. Br Med J (Clin Res Ed). 1986 Feb 8;292(6517):364–366.
- Pentousis D, Cooper JP, Cobbe SM. Prolonged asystole induced by head up tilt test. Report of four cases and brief review of the prognostic significance and medical management. Heart. 1997 Mar 1;77(3):273–275.
- Öberg B, White S. The role of vagal cardiac nerves and arterial baroreceptors in the circulatory adjustments to hemorrhage in the cat. Acta Physiol Scand. 1970 Nov;80(3):395–403.
- ColillesCalvet C, Papaceit Vidal J, Laguna Serrano E, et al. Bradicardiaparadojica y shock hemorragico. Urgencesmédicales. 1992;11(6):331–333.