1. Background
There are many causes for hemorrhage after a Whipple surgery, from surgical techniques to coagulopathies. A true gastrointestinal hemorrhage after a Whipple surgery is rare, and most frequently caused by a pseudoaneurysm (PSA) formation. Usually, there are three different types of anastomoses created during a Whipple surgery. These include two types of pancreatic-intestinal anastomoses, a choledochojejunal anastomosis and a gastrojejunal or duodenojejunal anastomosis. PSA formation is associated with localized inflammation from leakage of one of the three anastomoses, the most common being the pancreaticojejunal anastomosis. Herein, we describe a case of a massive and fatal gastrointestinal bleed after a Whipple surgery due to a PSA formation. Although rare, when gastrointestinal bleeding does occur after a Whipple surgery, mortality is very high. Gastroenterologists should have a high index of suspicion of PSA in post-Whipple patients who present with gastrointestinal bleeding.
2. Case presentation
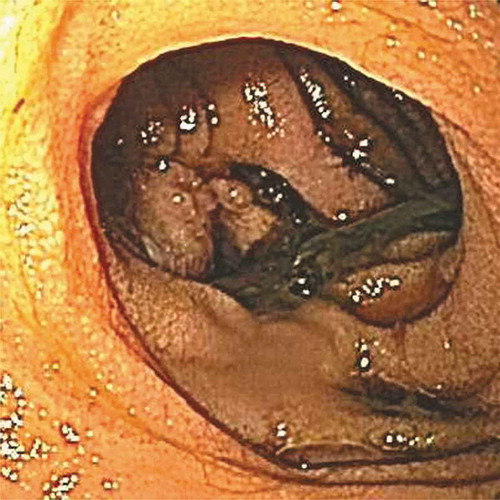
An adult female presented to an outside hospital with hematochezia, shortness of breath, tachycardia and hypotension of 64/52 mmHg. A few weeks prior, the patient had underwent a classic Whipple pancreaticoduodenectomy, which was complicated by a mild choledochojejunal leak. The leak was managed conservatively with a surgical drain. Laboratory results and physical examinations were unremarkable except for a hemoglobin (Hbg) of 7 g/dL. An emergent upper endoscopy revealed large amount of blood in the afferent loop of the jejunum, but no bleeding site was identified. Due to progressive reduction in Hbg, interventional radiologist (IR) performed an angiogram that demonstrated active bleeding from the gastroduodenal artery, and a coil-embolization was performed. Soon thereafter, the patient developed hemorrhagic shock, and required large volumes of blood products. She was then transferred to a level-one trauma center where she continued to have episodes of melena A second upper endoscopy was performed, revealing only superficial gastric erosions and a small clot at the choledochojejunal anastomosis without active bleeding (). The pancreaticojejunal anastomosis appeared normal. However, ten hours later, the patient became unresponsive. Blood was noted at the nose and mouth. She became bradycardic (40 bpm), hypotensive (95/54 mmHg), and quickly developed pulseless electrical activity. Cardiopulmonary resuscitation and massive transfusion protocol were initiated. Following the return of spontaneous circulation, she was emergently taken to IR
Figure 1. Upper endoscopy showing superficial gastric erosions and a small clot at the choledochojejunal anastomosis without active bleeding
where angiography revealed massive contrast extravasation from the hepatic artery (). Coil-embolization was performed and initially appeared successful. However, soon thereafter, the patient developed another cardiac arrest and expired.
3. Discussion/conclusion
Whipple surgery is a complex procedure with an overall complication rate of 41–60% and a postoperative hemorrhage rate of 5–13% [Citation1,Citation2]. When hemorrhage occurs, mortality is as high as 50% [Citation1]. Early bleeding, defined as bleeding within the first 24 hours post-surgery, is usually related to surgical complications, poor surgical techniques or coagulopathy. Delayed bleeding, defined as bleeding 24 hours to 30 days after surgery, is frequently caused by a pseudoaneurysm formation related to localized inflammation from leakage of one of the three types of anastomoses, the most common being the pancreaticojejunal [Citation2]. Our patient’s angiogram revealed a pseudoaneurysm (PSA) of the common hepatic artery with massive extravasation of contrast into the jejunal lumen. When a PSA occurs, it usually involves the gastroduodenal artery or the common hepatic artery, as presented in our patient. Leakage of pancreatic enzymes and bile into the surgical bed can lead to localized inflammation and damage to the blood vessels, resulting in a PSA formation. Our patient’s post-operative choledochojejunal leak increased her risk of a PSA formation. Although a PSA is most often asymptomatic, it can present with complications ranging from mild abdominal pain, anemia and hemobilia, to biliary obstruction and life-threatening hemorrhagic shock. Intervention in all identified visceral pseudoaneurysms is advocated regardless of symptoms because of the high risk of rupture compared to true aneurysms, exsanguinating hemorrhage and subsequent death [Citation3]. Advances in imaging techniques have enhanced the detection rate of pseudoaneurysms. Due to the high mortality associated with surgery for this condition, an endovascular procedure is now the preferred method of intervention [Citation2,Citation3]. Gastroenterologists should have a high index of suspicion of a bleeding PSA in post-Whipple patients who present with acute gastrointestinal bleeding.
Patient consent
This patient is deceased and consent from family/next of kin was not possible as they were not contactable.
Disclosure statement
The authors declare that they have no relevant material or financial interests that relate to this paper and have nothing to disclose.
References
- Roulin D, Cerantola Y, Demartines N, et al. Systematic review of delayed postoperative hemorrhage after pancreatic resection. J Gastrointest Surg. 2011;15(6):1055–1062.
- Lwin T, Leigh N, Iskandar ME, et al. Rare, uncommon, and unusual complications after pancreaticoduodenal resection. Surg Clin North Am. 2018 Feb;98(1):87–94.
- Luckhurst C, Perez C, Collinsworth AL, et al. Atypical presentation of a hepatic artery pseudoaneurysm: A case report and review of the literature. World J Hepatol. 2016 Jun 28;8(18):779–784.