ABSTRACT
Background: The duration of cardiopulmonary resuscitation (CPR) significantly affects long-term survival in patients with in-hospital cardiac arrests (IHCA). In this study, we questioned the long-term clinical benefits of extending CPR beyond twenty minutes for patients with in-hospital cardiac arrest. Additionally, we aimed to compare the outcomes of CPR at different locations of a large tertiary care community hospital.
Methods: This study was a retrospective chart review of 169 patients with IHCA recorded between 1 January 2016, and 31 December 2018, at a large volume tertiary care community hospital.
Results: Of the 169 patients suffering from cardiac arrest during hospitalization, 44.4% arrested in the intensive care unit (ICU) and 55.6% in a non-critical care setting. Return of spontaneous circulation (ROSC) was achieved in 60% of ICU and 70.2% of non-ICU patients. While only 20% of ICU patients survived the cardiac arrest, the overall survival for non-ICU patients was 31.9%. Despite the significant difference in percentage survival, survival difference did not reach statistical significance (p = 0.082) due to the small sample size. Overall survival was 26.6%. An initial shockable rhythm was associated with improved survival compared to a non-shockable rhythm (41% vs. 22.5%, p = 0.022).
In patients who had cardiac arrest for less than 20 minutes, 60.9% of patients achieved ROSC, compared to 37.9% who arrested for more than 20 minutes. Survival to hospital discharge was significantly lower for patients who had cardiac arrest for more than 20 minutes, compared to patients who were arrested for less than 20 minutes (3.1% vs. 41.3%, p = <0.0001). For patients who had a cardiac arrest for more than 30 minutes, ROSC was achieved in only 14.8% of patients. None of these patients survived to be discharged from the hospital (p = <0.0001).
The mean age for the patients in this study was 70 years. 52.6% of subjects were male, and 47.4% were females. Older age was not related to shorter duration of CPR (Pearson correlation: 0.030, P = 0.69).
Conclusion: Survival was significantly lower when CPR was unsuccessful for twenty minutes, and there is no survival benefit of extending CRP for more than 30 minutes. Lowest survival after a cardiac arrest on the general medical floor, compared to telemetry and ICU, may be related to delay in recognizing cardiac arrest and barriers in implementing standardized advanced cardiac life support (ACLS) protocol.
1. Introduction
The field of resuscitation has been evolving for more than two centuries [Citation1]. Cardiopulmonary resuscitation (CPR) is an emergency lifesaving procedure performed when the heart stops beating; immediate CPR can double or triple the chances of survival after cardiac arrest. CPR is a high acuity event, and its adequate performance requires a multidisciplinary approach involving leadership skills and effective communication [Citation2]. Although health care professionals follow the preset Advanced Cardiac Life Support (ACLS) algorithms while doing CPR on hospitalized patients, determining when to stop resuscitation efforts in cardiac arrest patients is difficult. Unfortunately, very little data exist to guide decision-making in this regard. Because of the nature of resuscitation research, few randomized controlled trials have been completed in humans [Citation3,Citation4].
Physician survey data and clinical practice guidelines suggest that factors influencing the decision to stop resuscitative efforts include: duration of resuscitation effort over 30 minutes without a sustained perusing rhythm, patient’s age and comorbidities, absence of brainstem reflexes and initial electrocardiographic rhythm of asystole [Citation5,Citation6].
While the factors mentioned above and physician’ bias remain strong influencers guiding the termination of resuscitation efforts, more objective endpoints of resuscitation have been proposed, including end-tidal CO2 (EtCO2). EtCO2 values are a function of CO2 production and venous return to the right heart and pulmonary circulation. A very low EtCO2 (<10 mmHg) following prolonged resuscitation (>20 minutes) is a sign of absent circulation and a strong predictor of acute mortality [Citation7,Citation8].
According to a study looking at data from the National Registry of Cardiopulmonary Resuscitation (NRCPR), the average survival-to-hospital discharge rate for adults who suffer in-hospital cardiac arrest is 17% to 20% and patients tend to overestimate their chances of surviving arrest by, on average, 60.4%. While another study utilizing data from the nationwide inpatient sample (NIS) concluded the overall survival rate after in-hospital cardiac arrest for non-adult patients was 30.4%. (8) Although the overall return of spontaneous circulation (ROSC) after in-hospital cardiac arrest can be as high as 50%, hospital discharge rates are much lower.
Get with the Guidelines-Resuscitation (GWTG-R) is a data registry and a comprehensive program for supporting quality in-hospital resuscitation, including a library of tools and resources to help improve processes and maximize effectiveness. GWTG-R facilitates the efficient capture, analysis, and reporting of data that empowers and supports the implementation of current guidelines, creation, and dissemination of new knowledge, and development of next-generation, evidence-based practice in resuscitation science.
Survival of in-hospital cardiac arrest (IHCA) has been increasing over the last two decades, and in 2017, survival to hospital discharge was 25% in the GWTG-R registry. Based on data from the GWTG-R registry, the mean age of patients with in-hospital cardiac arrest in the USA is 66 years, 58% are men, and the presenting rhythm is most often (81%) non-shockable (i.e., asystole or pulseless electrical activity). Important characteristics related to outcome after in-hospital cardiac arrest (IHCA) are age, race, significant baseline comorbidities, location of cardiac arrest, duration of cardiac arrest, and presenting rhythms.
Increased age is associated with decreased survival following cardiac arrest in most studies, especially for patients older than 70 years [Citation9]. Studies that investigated the relationship between race and outcomes have found African American and Hispanic patients have lower rates of neurological recovery and survival following in-hospital cardiac arrest compared to Caucasian patients [Citation10].
Factors related to early detection of cardiac arrests, such as the event being witnessed or occurring in a monitored location, are associated with improved outcomes [Citation11,Citation12].
The chance of 30-day survival markedly decreases with the increasing duration of CPR [Citation13].
Two of the factors most strongly associated with outcomes are the presenting rhythm and the duration of the cardiac arrest. Patients with a shockable rhythm have a 2 to 3 times higher survival to hospital discharge compared with patients with a non-shockable rhythm [Citation14]. ().
Figure 1. Comparison of survival percentage based on initial rhythm at the time of cardiac arrest in hospitalized patients [Citation14]
![Figure 1. Comparison of survival percentage based on initial rhythm at the time of cardiac arrest in hospitalized patients [Citation14]](/cms/asset/d7f23ebc-7795-4e97-afb4-420aa39b7684/zjch_a_1877396_f0001_oc.jpg)
Approximately half of the in-hospital cardiac arrests occur inwards, with the remaining half occurring in other locations, such as intensive care units (ICU) and operating rooms. Of patients with the arrest in the ICU, the adjusted mean survival to discharge is reported to be high, compared with the unmonitored wards and telemetry wards [Citation12,Citation15].
Many times clinicians and health care professionals are challenged with a question regarding the appropriate time to call off the code and frequently enough, families and care-takers of the patient look to the health care provider for objective data that can help them reach a decision for their loved one. To our knowledge, very scarce data are available to address this delicate issue, and often, health care providers are compelled to rely only on subjective factors while trying to come up with the best possible answers.
2. Objectives
In our study, we aimed to compare the CPR outcome data from our hospital to the data from GWTG-R to set the current baseline and use the comparisons to help us improve the IHCA care in our hospital. Additionally, we sought to determine if CPR changed the survival and clinical outcome of patients when it was extended beyond 20 minutes duration. Comparing the difference in survival and clinical outcome at different levels of care (ICU vs. non-ICU) after IHCA was a secondary objective of our study.
3. Methods
3.1. Subject selection
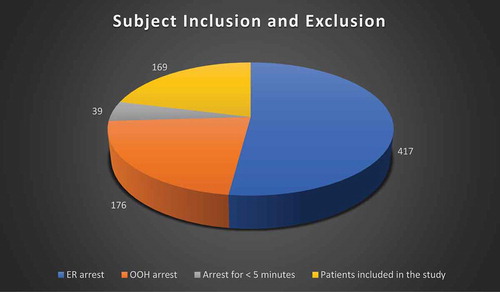
A list of 801 patients with the diagnosis of cardiac arrest admitted to Abington Hospital from 1 January 2016 to 31 December 2018, was obtained from the Information Technology department. The inclusion and exclusion criteria listed in were used to select patients for the study.
Table 1. Selection criteria
3.2. Data collection
A retrospective chart review was performed to complete the data collection for all subjects included in the study. Data collection was divided into two parts: 1) patent’s baseline pre-arrest characteristics, including age, sex, comorbidities, and location of cardiac arrest, and 2) events related to the cardiac arrest, including duration, rhythm, the return of spontaneous circulation (ROSC), and subsequent survival. The study was approved by the institutional review board (IRB) of Abington Memorial Hospital. To maintain anonymity, patients were assigned a unique study identification number. The medical information gathered during the study was treated confidentially.
3.3. Statistical analysis
Data were summarized using descriptive statistics such as mean, standard deviations, medians, and frequencies. Inferential statistics such as t-test and chi-square analyses will be performed where appropriate. All p-values will be two-tailed, and a level of <0.05 will be considered significant. Data were analyzed using IBM SPSS for Windows, version 20.0 (Armonk, NY: IBM Corp.).
4. Results
A total of 801 patients had a cardiac arrest from 1 January 2016, to 31 December 2018, and ended up in Abington hospital. Of these patients, 417 who had a cardiac arrest in the emergency department, and 176 patients who had an out of hospital cardiac arrest, were excluded from the study. In addition, 39 patients who had a cardiac arrest for less than five minutes were excluded from the study. The remaining 169 patients had a cardiac arrest during hospitalization and were included in the study. ()
Figure 2. Demonstrating the inclusion and exclusion of subjects based on the above-mentioned criteria. (ER = Emergency room, OOH = out of hospital cardiac arrest)
Of the 169 patients suffering cardiac arrest during hospitalization, 44.4% had been arrested in the ICU and 55.6% in a non-critical care setting. Return of spontaneous circulation (ROSC) was achieved in 60% of ICU and 70.2% of non-ICU patients. While only 20% of ICU patients survived the cardiac arrest, overall survival for non-ICU patients was 31.9%. Despite the significant difference in percentage survival, survival difference did not reach statistical significance (p = 0.082) due to the small sample size. ()
Figure 3. ROSC and Survival comparison between ICU and Non-ICU patients. (ROSC = return of spontaneous circulation, ICU = intensive care unit) (p = 0.082)
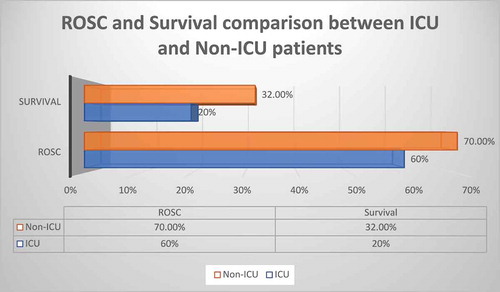
Amongst the non-ICU patients, survival after a cardiac arrest on a telemetry floor was higher (30%), compared to a regular general medical floor (18.2%). Overall survival was 26.6%. 23.1% of cardiac arrests had an initial shockable rhythm. An initial shockable rhythm was associated with improved survival compared to a non-shockable rhythm (41% vs. 22.5%, p = 0.022).
Thirty-eight percent of patients were resuscitated for more than 20 minutes. Our data indicate, the duration of cardiac arrest significantly impacted the achievement of ROSC and subsequent survival to discharge. In patients who had cardiac arrest for less than 20 minutes, 60.9% of patients achieved ROSC, compared to 37.9% who arrested for more than 20 minutes. Survival to hospital discharge was significantly lower for patients who had cardiac arrest for more than 20 minutes, compared to patients who were arrested for less than 20 minutes (3.1% vs. 41.3%, p = <0.0001). ()
Figure 4. Relationship of the duration of CPR with ROSC and survival. (CPR = Cardiopulmonary resuscitation, ROSC = Return of spontaneous circulation) (p < 0.0001)
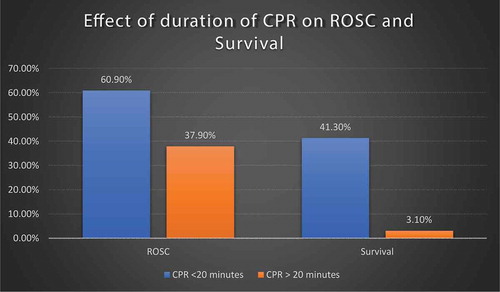
For patients who had a cardiac arrest for more than 30 minutes, ROSC was achieved in only 14.8% of patients. None of these patients survived to be discharged from the hospital (p = <0.0001). The mean age for the patients in this study was 70 years. 52.6% of subjects were male, and 47.4% were females. Age has been documented to be one of the strongest bias to call off the code, but in our study, older age was not related to shorter duration of CPR (Pearson correlation: 0.030, p = 0.69).
5. Discussion
Successful treatment of IHCA requires the rapid implementation of several processes of care within a short and defined period. Our study looked at variables such as duration and location of cardiac arrest and their impact on survival after IHCA. There are no current recommendations or guidelines issued by the American Heart Aassociation (AHA) regarding discontinuation of CPR after in-hospital cardiac arrest. Health care providers leading the CPR team are considered the decision-makers in this regard. Many factors, including the patient’s age, comorbidities, previous cardiac arrest, family’s wishes, and duration of CPR, play a significant role in determining the timing of calling off the code. Despite the lack of guidelines, the duration of cardiac arrest is one of the most significant determinants of when to stop the resuscitation efforts. We categorized the in-hospital cardiac arrest (IHCA) patients in three categories based on the duration of cardiac arrest: <20 minutes, >20 minutes, and >30 minutes. Our data support the previous data indicating lower survival with longer CPR. To the best of our knowledge, there are very little categorical data looking at survival after a specific duration of cardiac arrest. A significant decline in terms of survival is noted when we extend CPR beyond 20 minutes. Our hospital’s overall survival rate after IHCA seems to be similar to (26%), the previously by AHA (24%) [Citation12].
There is no data available at this time to compare the in-hospital survival percentage when we extend CPR beyond 20 minutes. Extending CPR beyond 30 minutes lowered the survival percentage even more. In our study, age was not related to a shorter duration of CPR, as documented in previous studies [Citation15]. Subgroup analysis of the data showed that the chances of survival for patients older than 70 years are very low when CPR duration was more than 20 minutes.
The location of the patient at the time of in-hospital cardiac arrest (IHCA) also has a significant impact on the survival outcome. Previous large database study done using ‘Get with The Guideline- Resuscitation’ (GWTG-R) showed better survival for telemetry patients, compared to non-telemetry patients [Citation12]. Our data also suggested lower survival for patients who are on the non-telemetry floor. Non-ICU telemetry floor has the highest survival percentage, followed by ICU patients. Lower survival on the non-telemetry floor is most likely related to delay in the detection of cardiac arrest (unwitnessed arrest), inability to implement timely and effective resuscitation, poor staff training in CPR, etc.
We propose that greater advances in IHCA survival might be realized with careful attention to the assignment of patient location for individuals at risk for catastrophic events such as cardiac arrest. Identifying the patient most at risk for decompensating is a complex task, and given limitations in resource allocation, it is not feasible to place all patients in critical care beds. However, our findings indicate that patients who suffer IHCA survive at higher rates in monitored settings (ICU and telemetry units). Preventing IHCA will always be the better alternative for improving overall patient health outcomes; however, placing at‐risk patients with a high likelihood for IHCA in monitored settings may contribute to furthering the already observed trends in improved survival after IHCA. Further study to identify these individuals at risk for IHCA will potentially contribute to improved outcomes or, better yet, prevention of IHCA. Finally, observational studies have shown that longer duration of participation in the GWTG-R registry is associated with both improved qualities of care [Citation16].
Our study has several limitations. It was a retrospective chart review performed at a single site. It has a small sample size for a subgroup analysis. Since our hospital does not participate in GWTG-R, we do not have the most recent regional/national data for comparison. Finally, cardiac arrests in the emergency room were not included and it may be difficult to compare the results with previous studies.
6. Conclusion
The optimal duration of CPR remains an unclear area, but in a relatively old and selected population, extending CPR beyond twenty minutes may be clinically futile. Large studies with subgroup analysis directed at the duration of CPR and its effect on survival may be needed to further guide in this regard. The lower survival after a cardiac arrest on the general medical floor, compared to telemetry and ICU, may be related to delay in recognizing cardiac arrest and barriers in implementing standardized ACLS protocol. Hospital-based quality improvement projects to address those barriers and improvement in patient’s triage to telemetry or non-telemetry floor may improve the clinical outcome. Understanding who is at the highest risk for IHCA and placing those individuals in the best setting for high‐level resuscitation is of utmost importance. Further work identifying the patient‐level predictors of cardiac arrest and factors that most contribute to improved outcomes will be valuable in helping providers and hospitals implement systems to prevent IHCA when possible and improve results when inevitable.
Disclosure statement
All authors have declared that no financial support was received from any organization for the submitted work. All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Cakulev I, Efimov IR, Waldo AL. Cardioversion: past, present, and future. Circulation. 2009;120(16):1623–1632.
- Murray WB, Foster PA. Crisis resource management among strangers: principles of organizing a multidisciplinary group for crisis resource management. J Clin Anesth. 2000;12(8):633–638.
- Field JM, Hazinski MF, Sayre MR, et al. Part 1: executive summary: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S640–56.
- Neumar RW, Shuster M, Callaway CW, et al. Part 1: executive summary: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S315–67.
- Mohr M, Bahr J, Schmid J, et al. The decision to terminate resuscitative efforts: results of a questionnaire. Resuscitation. 1997;34(1):51–55.
- de Vos R, Oosterom L, Koster RW, et al. Decisions to terminate resuscitation. Resuscitation committee. Resuscitation. 1998;39(1–2):7–13.
- Levine RL, Wayne MA, Miller CC. End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. N Engl J Med. 1997;337(5):301–306.
- Mallikethi-Reddy S, Briasoulis A, Akintoye E, et al. Incidence and survival after in-hospital cardiopulmonary resuscitation in nonelderly adults: US experience, 2007 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10(2). DOI:10.1161/CIRCOUTCOMES.116.003194
- Chan PS, Spertus JA, Krumholz HM, et al. A validated prediction tool for initial survivors of in-hospital cardiac arrest. Arch Intern Med. 2012;172(12):947–953.
- Larkin GL, Copes WS, Nathanson BH, et al. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National registry for cardiopulmonary resuscitation. Resuscitation. 2010;81(3):302–311.
- Brady WJ, Gurka KK, Mehring B, et al. In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011;82(7):845–852.
- Perman SM, Stanton E, Soar J, et al. Location of In-hospital cardiac arrest in the USA-variability in event rate and outcomes. J Am Heart Assoc. 2016;5(10). DOI:10.1161/JAHA.116.003638
- Rohlin O, Taeri T, Netzereab S, et al. Duration of CPR and impact on 30-day survival after ROSC for in-hospital cardiac arrest—A Swedish cohort study. Resuscitation. 2018;132:1–5.
- Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(1):50–57.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American heart association. Circulation. 2018;137(12):e67–e492.
- Starks MA, Dai D, Nichol G, et al. The association of duration of participation in get with the guidelines-resuscitation with quality of care for in-hospital cardiac arrest. Am Heart J. 2018;204:156–162.
