ABSTRACT
Neuromyelitis Optica or Devic disease is changed to Neuromyelitis Optica spectrum disorder to include more diverse neurological and autoimmune manifestations. This is a severe relapsing autoimmune demyelinating disorder commonly affecting the optic nerve and spinal cord. It has been reported as either the first manifestation of SLE or as a coexisting condition with other autoimmune disorders commonly included but not limited to SLE and SS. We discussed a case of a 49-year-old female patient who was initially presented with a left-sided weakness that rapidly progressed to quadriparesis and bladder dysfunction within a few days. She had positive autoimmune serology tests for SLE posing a diagnostic challenge as SLE is associated with neurological manifestations. Due to a lack of definitive diagnostic criteria for SLE, presence of AQP-4 antibodies in CSF, and evidence of longitudinal extensive transverse myelitis in MRI cervical spine, we conclude that she has Neuromyelitis Optica spectrum disorder with probable SLE. It is possible that she may develop more signs and symptoms of SLE with time and will need close follow up. Timely diagnosis and prompt treatment are vital to decrease morbidity and mortality, as done in our case. The patient was started on high-dose steroids with significant improvement in her symptoms. These patients may need early treatment with plasmapheresis and long-term follow-up with immunotherapy to prevent relapse. There are few case reports in the literature, and more information is needed to understand and better diagnose NMO with coexisting SLE.
1. Introduction
Neuromyelitis Optica (NMO) spectrum disorder is a rare autoimmune–mediated demyelinating inflammatory disease affecting the central nervous system associated with relapsing events leading to chronic debility with significant morbidity and mortality. It principally involves optic nerves and spinal cord characterized by optic neuritis and acute transverse myelitis [Citation1]. Neuromyelitis optica spectrum disorder has a prevalence of 0.5 to 4.4 per 100,000 people, more common in women than in men. The median age of onset is 35–45 years [Citation2]. NMO spectrum disorder is a separate entity which once believed to be a variant of multiple sclerosis. Neuromyelitis Optica and multiple sclerosis are distinguished by pathogenesis, immunology, imaging features, biomarkers, and neuropathology. Anti-aquaporin-4 IgG also known as NMO IgG antibody, is a highly specific antibody for NMO spectrum disorders, but only has 72% sensitivity [Citation3]. It can overlap with other autoimmune diseases such as systemic lupus erythematosus, Sjogren’s disease and other autoimmune diseases. We present a patient with acute myelitis who was found to have anti-dsDNA, anti-RNP, anti-chromatin and anti-AQP4 (NMO IgG) antibodies supporting the overlapping diagnosis of NMO and SLE.
2. Case report
A 49-year-old African American woman with no significant past medical history presented with left-sided weakness associated with paresthesia and numbness for the last four weeks. Her symptoms started with neck pain 4 weeks ago radiating to the left arm and gradually progressed to the left half of the body, followed by weakness and numbness. Two weeks later, she developed nausea, vomiting, headache followed by urinary and bowel retention associated with perineal numbness. She saw her primary care physician, was given a methylprednisolone dose pack, which did not help. Her last bowel movement was 10 days ago. She noticed a progressive right–sided weakness with the inability to ambulate and decided to come to the Emergency room. She denies fever, chills, headache, lightheadedness, cough, chest pain, shortness of breath, joint pain, joint swelling, oral ulcers, facial rash, or focal neurological deficits. She denies recent falls or trauma. Her past surgical history includes cesarean section and tubal ligation. She is allergic to penicillin, she denies a history of smoking, alcohol, or recreational substance abuse. She works as a security guard. Family history was significant for congestive heart failure in Father.
On admission, vitals are normal. Physical exam revealed a well-built lady who is alert and oriented to time, place and person, normal S1, S2 on cardiovascular exam, respiratory system clear on auscultation bilaterally, abdomen was benign. Neurological exam revealed normal memory, concentration, attention, orientation, cranial nerves II– XII intact. Increased tone on left upper extremities. Strength is 4+/5 on right, 3/5 on left. No abnormal movements or tremors noted. The patient has decreased vibration in bilateral feet and decreased in the left knee. Deep tendon reflexes are 1+ throughout. Toes are downgoing bilaterally to plantar stimulation and clonus was absent. Cerebellar signs are normal on the right side, but unable to be performed on the left side due to weakness. Admission labs are summarized in .
Table 1. Admission labs
Hospital Course: Our patient presented with worsening weakness initially on the left side, which then progressed to the right side, followed by urinary and bowel retention. The MRI of the brain without contrast was negative for acute stroke or demyelination. MRI of cervical spine without contrast showed abnormal finding suggestive of either transverse myelitis or infiltrating cord malignancy. Neurology was consulted, who then recommended MRI cervical, thoracic and lumbar spine with contrast, which showed enhancement of the thickened region of the cervical spinal cord extending from the craniocervical junction to C5-C6 (seen in Images 1 and 2). No abnormality of the thoracic spine and mild degenerative changes on the lumbar spine. Imaging studies are summarized in . Broad differential diagnosis includes inflammation, infection, demyelinating disorder, autoimmune conditions, and spinal cord tumors. ANA with reflex sub-serologies were sent. ANA was positive for anti dsDNA, RNP and chromatin antibodies indicating SLE. Hepatitis panel, HIV, HTLV 2/3, Neisseria gonorrhoeae, rapid plasma reagin (RPR), CSF cultures, gram stains, VDRL, Lyme testing were all negative. Additional laboratory findings are summarized in . CSF showed increased WBC, which is lymphocyte-predominant. However, flow cytometry and cytology was negative. As oligoclonal bands came back negative. CSF results are summarized in . CT of thorax and abdomen showed no malignancy. She was started on empiric intravenous methylprednisolone 1 g per day as there was suspicion for demyelinating disease, and later NMO antibodies came back positive. On further questioning, she did not have any other symptoms related to SLE. Steroids were tapered down to oral prednisone with marked improvement in weakness as well as mobility within days. She was evaluated by physical and occupational therapy and subsequently discharged to a rehab facility. Based on a constellation of the clinical symptoms, characteristic MRI cervical spine findings of longitudinal extensive transverse myelitis, increased WBC with lymphocyte predominance on CSF analysis and presence of NMO IgG AQP-4 Antibodies, a diagnosis of neuromyelitis optica was made and she also had overlapping autoimmune disease as antibodies for Anti dsDNA, anti-RNP, and anti-chromatin were present.
Image 1,2. MRI cervical spine with contrast. Arrow shows contrast enhancement of thickened region of cervical cord from cervicocranial junction to C5-6
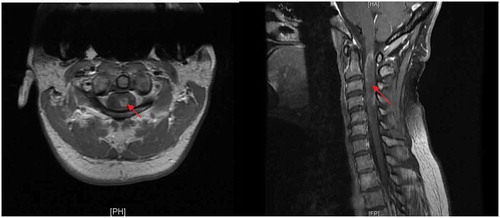
Table 2. Additional labs
Table 3. CSF analysis
Table 4. Imaging studies
3. Discussion
The above patient posed a diagnostic challenge due to clinical findings, laboratory results, and rapidly deteriorating clinical findings warranting early treatment. Although NMO spectrum disorder is the most likely diagnosis based on constellations of symptoms, MRI findings, presence of NMO IgG AQP-4 antibodies and rapid response to steroids. Alternate differential included.
1. Systemic lupus erythematosus: Transverse myelitis is a rare neurological manifestation of SLE and can be presented as an initial manifestation of SLE [Citation4]. Very few cases of optic neuritis are reported in SLE. SLE and NMO are two independent diseases but can coexist in one patient. This patient has dsDNA, RNP, and chromatin antibodies but has no arthritis, classic facial rash, proteinuria, pancytopenia, and renal abnormalities. She most likely has concomitant SLE and NMO as she has both serologies positive.
2. Multiple sclerosis (MS): Patient MRI findings do not meet criteria for diagnosis of MS. More than three vertebral segments are involved on MRI cervical spine, with only one lesion in the cervical spinal cord and no other lesions in MRI brain, MRI thoracic, and lumbar spine, absence of oligoclonal antibodies and presence of NMO antibodies on CSF analysis rules out MS.
3. Sjogren’s syndrome (SS) associated demyelinating syndromes: NMO and Sjogren's syndrome are two independent diseases which can overlap. NMO does not present as a CNS manifestation of SS [Citation5]. She does not have SS based on her clinical history and serologies.
4. Intrathecal spinal cord tumors: primary or metastatic spinal tumor is less likely given rapid response to steroids, absence of neoplastic cells on CSF cytology, absence of tumor on MRI cervical spine and in CT Thorax and abdomen and pelvis.
5. Acute disseminated encephalomyelitis (ADEM): is an autoimmune inflammatory demyelinating disease, most commonly occurs after systemic infection. Absence of encephalopathy and infection makes diagnosis of ADEM less likely.
6. Neuro-Behçet disease: Rarely presents with cervical spine myelitis involving more than three vertebral segments similar to NMO. Clinical history was not suggestive of Behcet disease and the presence of anti NMO antibody makes this diagnosis less likely [Citation6]
7. Transverse myelitis from B12/folate deficiency or infections like HTLV, HIV or lyme disease is unlikely secondary to normal lab studies.
Neuromyelitis optica is a rare relapsing, inflammatory demyelinating disease of the central nervous system primarily affecting optic nerves and spinal cord. The Aquaporin-4 (AQP4) antibody and complement pathway play an important role in the pathogenesis of NMOSD. NMO-IgG selectively binds to the aquaporin-4 water channel located in astrocyte foot processes at the blood-brain barrier [Citation7] and leads to direct injury to the central nervous system as a result of astrocyte injury by antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) [Citation8,Citation9]. As per International consensus, diagnosis can be made based on the presence of one core clinical characteristics as in , NMO IgG antibodies with the exclusion of alternative diagnosis [Citation10]. In the absence of NMO IgG antibodies, two core clinical criteria along with exclusion of alternate diagnosis or additional MRI findings will suffice.
Table 5. Core clinical characteristics as per international consensus diagnostic criteria for neuromyelitis optica spectrum disorders
Anti-AQP-4 antibodies are highly specific for the diagnosis of NMO [Citation3]. NMO can coexist with autoimmune diseases like Sjogren’s syndrome, SLE and other autoimmune disorders [Citation11]. Myelin basic protein, anti-myelin oligodendrocyte glycoprotein (MOG), S100β, CPSF-73, RNF–141, and myosin light-chain antibodies are other autoantibodies that have been found in NMO patients sera and CSF [Citation12]. The presence of antibodies in patients with the first attack of acute myelitis indicates an increased risk of recurrence of myelitis and the development of optic neuritis in less than 1 year [Citation13]. Methylprednisolone 1 gram/day for 3-5 days is the choice of the drug during an acute attack. Plasmapheresis should be considered for patients with severe symptoms who are unresponsive to glucocorticoids. Eculizumab is used for acute prevention and decreases the frequency of a relapse. It inhibits the terminal complement protein C5 which prevents the deposition of complement membrane complex attack C5-9 [Citation14]. Early diagnosis and initiation of high-dose steroids are crucial for NMO patients as mortality rates are high in these patients secondary to respiratory failure due to the extension of cervical lesions into the brainstem or from primary brainstem lesions. NMO has worse outcomes and poor prognosis than MS because of recurrent attacks of optic neuritis and myelitis. Debility accumulates with each attack.
4. Conclusion
Neuromyelitis optica (NMO) spectrum disorder is an uncommon severe relapsing autoimmune mediated CNS demyelinating disease. Internists should be aware of the diagnosis and consider NMO as one of the differential diagnosis for patients presenting with visual field deficits and eye pain mainly with eye movement or neurologic deficits including paraplegia or quadriplegia or bladder dysfunction. Early diagnosis and prompt treatment are crucial in neuromyelitis spectrum disorders in light of its relapsing course, debility accrues with each attack and also increased mortality from respiratory failure during acute attacks. ANA and other autoimmune serologies should be ordered as well even if there is suspicion for NMO as it can coexist with other autoimmune diseases like lupus as presented in our case.
Informed consent
Verbal consent was obtained.
Author contributions
VS, MP collected and reviewed patients chart, MB, GP, SA, VK, SN contributed to writing the introduction, discussion, and conclusion. All authors contributed equally to the preparation of this manuscript and all of the authors reviewed the manuscript and agreed with the findings and interpretation.
Acknowledgments
I thank all the authors who contributed to the case report.
Data availability
From the patient’s chart and PUBMED.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Jacobi C, Stingele K, Kretz R, et al. Neuromyelitis optica (Devic’s syndrome) as the first manifestation of systemic lupus erythematosus. Lupus. 2006;15(2):107–109.
- Mealy MA, Wingerchuk DM, Greenberg BM, et al. Epidemiology of neuromyelitis optica in the USA. Arch Neurol. 2012;69(9):9.
- Waters PJ, McKeon A, Leite MI, et al. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology. 2012;78(9):665–671.
- D’Cruz DP, Mellor-Pita S, Joven B, et al. Transverse myelitis as the first manifestation of systemic lupus erythematosus or lupus-like disease: good functional outcome and relevance of antiphospholipid antibodies. J Rheumatol. 2004 Feb;31(2):280–285.
- Birnbaum J, Atri NM, Baer AN, et al. Relationship between neuromyelitis optica spectrum disorder and sjögren’s syndrome: central nervous system extraglandular disease or unrelated, co-occurring autoimmunity? Arthritis Care Res (Hoboken). 2017;69(7):1069–1075.
- Liu H-M, Dong C, Zhang Y-Z, et al. Clinical and imaging features of spinal cord type of neuro Behçet disease. Medicine (Baltimore). 2017;96(40):e7958.
- Lennon VA, Kryzer TJ, Pittock SJ, et al. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202(4):473–477.
- Graber DJ, Levy M, Kerr D, et al. Neuromyelitis optica pathogenesis and aquaporin 4. J Neuroinflammation. 2008;5(1):22.
- Duan T, Smith AJ, Verkman AS. Complement-independent bystander injury in AQP4-IgG seropositive neuromyelitis optica produced by antibody-dependent cellular cytotoxicity. Acta Neuropathol Commun. 2019;7:1.
- Wingerchuk DM, Banwell B, Bennett JL, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–189.
- Pittock SJ, Lennon VA, de Seze J, et al. Neuromyelitis optica and non–organ-specific autoimmunity. Arch Neurol. 2008;65(1). DOI:10.1001/archneurol.2007.17
- Haase CG, Schmidt S. Detection of brain-specific autoantibodies to myelin oligodendrocyte glycoprotein, S100β and myelin basic protein in patients with Devic’s neuromyelitis optica. Neurosci Lett. 2001;307(2):131–133.
- Weinshenker BG, Wingerchuk DM, Vukusic S, et al. Neuromyelitis optica IgG predicts relapse after longitudinally extensive transverse myelitis. Ann Neurol. 2006;59(3):566–569.
- Pittock SJ, Berthele A, Fujihara K, et al. Eculizumab in Aquaporin-4–Positive neuromyelitis optica spectrum disorder. N Engl J Med. 2019;381(7):614–625.
