ABSTRACT
Background: The Thrombolysis in Myocardial Infarction (TIMI) score is considered a method for early risk stratification in patients with unstable angina/non-ST elevated myocardial infarctions (UA/NSTEMI). It is composed of seven factors and if present, each factor contributes a value of one point toward the TIMI risk score, making it a simple tool that does not require differential weights for each factor. A higher score implies a higher likelihood of adverse cardiac events and/or risk of mortality. A TIMI risk score ≥3 recommends early invasive management with cardiac angiography and revascularization. As per CDC study in 2014, Americans living in rural areas are more likely to die from leading causes such as cardiovascular diseases. An estimated number 25,000 deaths than their urban counterparts, which coincide with a TIMI risk score of ≥3, potentially limit the utility of the TIMI risk score in risk stratification in rural catherization laboratories. The objective of this study was to assess the reliability of TIMI score as early risk stratification in patients with unstable angina/non-ST elevated myocardial infarctions (UA/NSTEMI) in rural hospital.
Methods: A retrospective chart review study in a rural hospital was conducted for subjects that received left heart catheterizations, exercise stress tests, or chemical stress tests for a diagnosis of UA/NSTEMI. A total of 399 subjects who underwent left heart catheterization and/or stress testing were recruited for this study. A total of 153 subjects who were transferred out to a larger facility, transitioned to comfort care, refused intervention, or passed away were excluded from the study. The 246 remaining subjects were classified into two groups, those with TIMI 0–2 compared with those having TIMI ≥ 3. A null hypothesis was postulated that there was no significant difference between the two groups with regard to prevalence of either positive stress test or evidence of obstructive coronary disease following coronary angiography. T-test and Wilcoxon rank-sum analysis were performed through SPSS statistical analysis.
Results: Formal statistical analysis using T-test as well as Wilcoxon rank-sum test comparing the two groups showed p = 0.34 for T-test and p = 0.60 for Wilcoxon rank-sum test. This is consistent with the postulated null hypothesis: that there is no significant difference between the two surgery groups with respect to the mean/median TIMI score.
Conclusion: There was no statistical difference between high and low TIMI score in the intervention of unstable angina/non-ST elevated myocardial infarctions (UA/NSTEMI) in a rural hospital.
1. Introduction
Chest pain accounts for nearly 7.6 million annual visits in the USA [Citation1,Citation2] and is one of the most common diagnoses that warrants an admission in the hospital. In rural hospitals, where resources and specialty services are limited, accurate risk stratification is of essence in order to optimize utilization of limited resources. Multiple predictor models have been used by physicians over the years in order to risk stratify patient populations to warrant further workup. Prior reports have shown that one specific model, the Thrombolysis in Myocardial Infarction (TIMI) risk score, has been found to be predictive of the severity of the vascular disease making it a good tool to predict the potential of coronary circulation involvement in chest pain cases [Citation3]. There are seven components that are used in calculation of the TIMI score. Patients presenting with Unstable Angina (UA) or Non-ST Elevation Myocardial Infarction (NSTEMI) that typically score 3 or more on the TIMI model are recommended to have early invasive management with cardiac angiography and revascularization if necessary. The TIMI score continues to be one of the most commonly utilized risk stratification models in the inpatient setting to warrant further workup. Although the TIMI scoring system is broadly utilized, not much research has been conducted to assess its accuracy as a predictor model in rural hospitals. Therefore, this study was conducted to assess the reliability of TIMI score as early risk stratification in patients with unstable angina/non-ST elevated myocardial infarctions (UA/NSTEMI) in rural hospital.
2. Methods
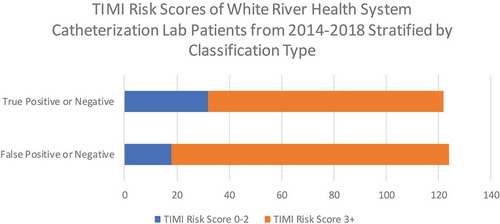
A retrospective chart review study in a rural hospital was conducted for patients who have received left heart catheterizations, exercise stress tests, or chemical stress tests for a diagnosis of UA/NSTEMI. A total of 399 subjects who underwent left heart catheterization and/or stress testing were recruited for this study between years 2014 and 2018. A total of 153 subjects who were transferred out to a larger facility, transitioned to comfort care, refused intervention, or passed away were excluded from the study. The 246 remaining subjects were classified into two groups, those with TIMI 0–2 compared with those having TIMI ≥ 3 (). Final reports for their left heart catheterization and stress testing were reviewed and classified if they have received stents, positive stress test or not. Stratification of the patients into four distinct groups (i.e., False Negative, False Positive, True Negative, and True Positive) was conducted based on the complementary factors of TIMI Risk score and whether or not the insertion of a stent was performed (). Mean and Median were calculated for the TIMI score by error type in which they are still similar, but there is somewhat greater variability for true than for false (). Then, a null hypothesis was postulated that there was no significant difference between the two groups with regard to prevalence of either positive stress test or evidence of obstructive coronary disease following coronary angiography. T-test and Wilcoxon rank-sum analysis were performed through SPSS statistical analysis.
Table 1. Medical tests/procedures performed and TIMI risk scores of White River Health System catheterization lab patients from 2014 to 2018 stratified by classification type
3. Results
When testing the null hypothesis that was postulated of no difference between the two groups of TIMI score using T-test and Wilcoxon rank-sum test that addresses medians, results showed that both the T-test with a p=0.34 and the Wilcoxon rank-sum test with a p=0.60 are consistent in that neither supports evidence of a difference between the error types with respect to the mean/median TIMI score.
4. Discussion
The TIMI scoring system continues to be one of the few leading risk stratification models used commonly in diagnoses of UA or NSTEMI. Accurate risk stratification is essential in rural hospitals where resources and specialty services availability can be limited. In this study, the TIMI scoring system did not prove to be an accurate tool to predict the need for further intervention, as there was no statistical difference between the two groups compared. Inaccurate risk stratification can lead to unnecessary coronary angiograms and place patients at risk for complications such as strokes, hematomas, and coronary aneurysms.
There are quite a few potential explanations that can account for the findings of this study. Prior investigation has shown that rural neighborhoods tend to have increased rates of chronic disease, higher numbers of uninsured citizens, fewer physicians, and nurses per capita and people are less likely to seek out assistance from healthcare providers until later in the disease course [Citation4]. In rural America, healthcare resources are limited, and patients are very easily lost to follow up. Hence, due to the lack of regular primary care follow up, patients are more likely to develop risk factors such as continued smoking, hypertension, and diabetes that can cause elevated TIMI scores in rural settings. Moreover, given the advances in medicine, the average lifespan in rural America has risen to 76.7 years [Citation5]. With an increasing baby boomer population, patients are more likely to automatically earn an extra one point for being over the age of 65 on their risk stratification with TIMI scoring when presenting with UA/NSTEMI. Of the seven components of TIMI scoring system, three factors specifically (positive cardiac markers, EKG ST changes, and known CAD stenosis) are objective accurate predictors of known active or prior Acute Coronary Syndrome (ACS). Given the discrepancies in rural healthcare settings, risk stratification models in UA/NSTEMI should weigh objective coronary risk factors more heavily in order to judiciously use limited healthcare resources and limit patients from unnecessary interventional risk.
Despite the significant findings of this study, there are a few limitations worthy of highlighting. Despite maximum effort that was undertaken to reduce bias, it is important to note that this study was a retrospective study, thus allowing for the presence of selection bias. Moreover, data were harvested at one local rural hospital in North Central Arkansas creating geographical restrictions for application of the conclusions from this data. Further research needs to be conducted at other rural hospitals across the USA in order to test the validity of the findings of this study. Future studies can be conducted as prospective studies in order to limit selection bias that was present in this study.
Prior studies have shown that the TIMI risk score is a useful and simple score for stratification of patients with high risk of 14-day mortality in patients with NSTEMI specifically [Citation3]. However, the TIMI score is not a means for prediction for obstructive CAD. Although its application has evolved into a tool to guide clinical healthcare providers for the next steps in settings of UA and NSTEMI, further consideration needs to be taken into account given the findings of this study. Other risk stratification scoring systems have been created in order to assist with stratification of patient populations with ACS, two of them being The History, Electrocardiogram, Age, Risk Factors, Troponin (HEART) score and Global Registry of Acute Coronary Events (GRACE) score. As the results of this study have shown, low TIMI score does not necessitate a rule out of obstructive CAD. Using additional risk stratification scores as above, HEART and GRACE, can help supplement clinical decision making in patients presenting with ACS-type symptoms. The HEART score has specifically shown to have significant value as an adjunct in its ability to sub stratify low-risk TIMI population (TIMI 0–2) [Citation6]. Therefore, adjunct incorporation of secondary risk stratification models can help reduce costs and prevent unnecessary medical workup in patients being admitted for suspected ACS evaluation.
5. Conclusion
As seen this study, there were no statistical differences between high and low TIMI score in the intervention of unstable angina/non-ST elevated myocardial infarctions (UA/NSTEMI) in a rural hospital. Our study indicates there may be a significant number of unwarranted cardiac catheterization procedures for these diagnoses, potentially resulting in an associated increase in costs, radiation, and contrast exposure. Further studies might be beneficial in exploring the validity of this score in other rural hospital catheterization laboratories.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Garcia MC, Rossen LM, Bastian B, et al. Potentially excess deaths from the five leading causes of death in metropolitan and nonmetropolitan counties — United States, 2010–2017. MMWR Surveill Summ. 2019;68(SS–10):1–11. .
- Bhuiya FA Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. No. 43. US Department of Health and Human Services, Centers for Disease Control and Prevention. National Center for Health Statistics; 2010.
- Rao SS, Agasthi P. Thrombolysis in myocardial infarction risk score. 2020 Apr 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan. PMID: 32310529.
- Van Dis J. Where we live: health care in rural vs urban America. Jama. 2002;287(1):108.
- Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med. 2014 Feb;46(2):e19–29. . PMID: 24439358.
- Marcoon S, Chang AM, Lee B, et al. HEART score to further risk stratify patients with low TIMI scores. Crit Pathw Cardiol. 2013;12(1):1–5.