ABSTRACT
Pneumorrhachis is an extremely rare clinical entity, involving air entrapment within the spinal canal. We present a unique case of epidural pneumorrhachis accompanying pneumomediastinum and pneumopericardium, in the setting of COVID-19 infection in a 62-year-old woman. Diagnostic testing was remarkable for elevated inflammatory markers, along with mild transaminitis and hyponatremia. CT scan of the chest revealed extensive patchy ground-glass opacities, with no evidence of pulmonary embolism. Intravenous antibiotics and steroids were initiated for management of advanced multifocal bilateral COVID-19 pneumonia. Her hospital course was complicated by rapidly worsening hypoxia accompanied by worsening inflammatory markers. Repeat chest CT showed worsening multifocal opacities, extensive pneumomediastinum, pneumopericardium, and subcutaneous emphysema extending into the lower neck soft tissues, posterior mediastinum, and supraclavicular regions. Neck CT confirmed diffuse subcutaneous emphysema from the mediastinum extending into the retropharyngeal space, neck, and anterior chest wall. Right-sided epidural air in the spinal canal spanning C6-T1 was also noted. She was evaluated by neurosurgery, continued on antibiotics for the epidural air, and transferred to the ICU for frequent monitoring of respiratory and neurological status, which remained stable. Although pneumorrhachis is an extremely rare clinical manifestation, prompt recognition can lead to appropriate early interventions and improved patient outcomes.
1. Background
Pneumorrhachis is an extremely rare clinical entity, involving air entrapment within the spinal canal. In most cases it is an asymptomatic epiphenomenon but may produce symptoms associated with the underlying pathology. The vast majority of reported cases are associated with a history of trauma [Citation1], and the association of pneumorrhachis with COVID-19 remains uncommon. We present a unique case of epidural pneumorrhachis accompanying pneumomediastinum and pneumopericardium, in the setting of COVID-19 infection.
2. Case presentation
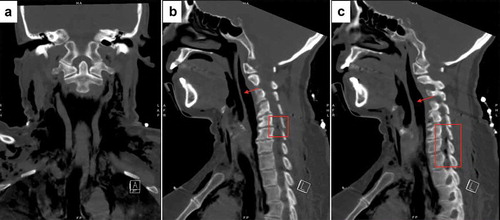
A 62-year-old woman presented to the emergency room with worsening dyspnea and chest heaviness. Her medical history was notable for hypertension, diabetes, hyperlipidemia, hypothyroidism, and a positive COVID-19 test one week prior. On presentation, she was hypertensive, tachypneic, and hypoxic, requiring supplemental oxygen via non-rebreather mask. Physical examination was notable for labored respirations with rhonchorous breath sounds throughout. She had no focal neurological deficits and an intact sensorium. Laboratory diagnostics were remarkable for elevated d-dimer (3.46 mcg/mL; reference ≤0.62 mcg/mL), ESR (65 mm/h; reference <30 mm/h), high sensitivity CRP (152.28 mg/L; reference <3 mg/L), LDH (563 units/L; reference range 120–246 u/L) and ferritin (591.4 ng/mL; reference range 7.3–270.7 ng/mL), along with mild transaminitis and hyponatremia. A CT scan of the chest with intravenous contrast revealed extensive patchy ground-glass opacities (), with no evidence of pulmonary embolism. Intravenous antibiotics and steroids were initiated, and she was admitted for further management of advanced multifocal bilateral COVID-19 pneumonia. Her hospital course was complicated by rapidly worsening hypoxia requiring high flow nasal cannula, accompanied by worsening inflammatory markers. A repeat chest CT showed worsening multifocal opacities, extensive pneumomediastinum, pneumopericardium, and subcutaneous emphysema extending into the lower neck soft tissues, posterior mediastinum, and supraclavicular regions. A CT scan of the neck confirmed diffuse subcutaneous emphysema from the mediastinum extending into the retropharyngeal space, neck, and anterior chest wall. Right-sided epidural air in the spinal canal spanning C6-T1 was also noted (). She was evaluated by neurosurgery, continued on antibiotics for the epidural air, and transferred to the intensive care unit for frequent monitoring of respiratory and neurological status. Her respiratory and neurologic status remained stable. Over the course of a few days, repeat imaging of the neck confirmed resolution of the intraspinal air.
Figure 1. Initial CT scan of the chest (coronal slice, lung window) showing extensive patchy ground-glass opacities

Figure 2. CT scan of the neck without contrast (a) Coronal slice, bone window, revealing diffuse subcutaneous emphysema from the mediastinum extending into lower neck soft tissues. (b) and (c) Sagittal slices, bone window, revealing diffuse subcutaneous emphysema from the mediastinum extending into the retropharyngeal space (red arrow) and epidural air in the spinal canal spanning C6-T1 (red box)
3. Discussion and conclusions
Pneumorrhachis is an uncommon entity characterized by air entrapment in the spinal canal, with most cases occurring in the setting of penetrating or blunt force trauma, instrumentation and spinal cord injuries[Citation1]. Pneumorrhachis in patients with COVID-19 is an extremely rare finding, minimally reported in the literature[Citation2]. We describe a unique case of epidural pneumorrhachis associated with pneumomediastinum and pneumopericardium in the setting of worsening COVID-19 infection, with extensive air tracking into the subcutaneous tissues and retropharyngeal space. Increases in intra-alveolar pressure and alveolar rupture can lead to movement of air into the perivascular interstitium, leading to pneumomediastinum and air tracking in the retropharyngeal space. Continued air dissection from the retropharyngeal space through the neural foramina can subsequently lead to pneumorrhachis [Citation3,Citation4]. In many cases, pneumorrhachis is a self-limiting condition and a conservative treatment approach is appropriate in patients that are stable from a neurological and cardiopulmonary standpoint [Citation3]. Nevertheless, given the volatile nature of this clinical entity, prompt recognition, urgent evaluation by a specialist, close monitoring and appropriate management can lead to improved patient outcomes. We describe a unique case of epidural pneumorrhachis associated with pneumomediastinum and pneumopericardium in the setting of worsening COVID-19 infection. Although this is an extremely rare clinical manifestation, prompt recognition can lead to appropriate early interventions and improved patient outcomes.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Osunronbi T, Sofela A, Sharma H, et al. Traumatic pneumorrhachis: systematic review and an illustrative case. Neurosurg Rev. 2021;44(2):731–739.
- Hochhegger B, de Mattos JN, Marchiori E. Pneumorrhachis: an uncommon finding in patients with COVID-19. Rev Soc Bras Med Trop. 2021;54:e0095–2021.
- Heckman AJ, Mohseni M, Villanueva A, et al. Concurrent spontaneous pneumomediastinum and pneumorrhachis. J Emerg Med. 2018;54(6):e117–e120.
- Ehmann MR, Paziana K, Stolbach AI. Case series: pneumorrhachis secondary to spontaneous pneumomediastinum. J Emerg Med. 2016;50(2):e43–e45.
