ABSTRACT
Introduction
Pneumococcal diseases (PDs) are among the leading causes of mortality and morbidity worldwide. However, the evidence on epidemiology, health economic, and patient-reported outcomes has not been systematically reviewed and published in Japan. This study aimed to assess the burden, treatment adherence and compliance, and serotype distribution associated with PDs in Japan.
Method
One hundred and eight studies were identified between January 2005 and June 2020. The identified studies were mostly regional and with a limited scale, clinical settings, and populations.
Results
In 2013–2017, invasive PD incidence rates were 4.98–9.47/100,000 in <4-year-olds, 0.36/100,000 in 5–14-year-olds, 0.46/100,000 in 15–64-year-olds, and 1.50–5.38/100,000 in the elderly. The incidence of invasive PDs in children decreased from 24.6/100,000 in 2008 to 10.7/100,000 in 2013 after the introduction of PCV7 and further declined to 10.3/100,000 in 2014 after PCV13 was introduced. From 2014, the prevalence of PCV13 serotypes decreased across all age groups along with a decrease of PPV23 serotypes, but an increase of PPV23 serotypes not included in PCV13 among adults and the elderly. No study reported health-related quality-of-life data for PDs. In children, direct costs were 340,905–405,978 JPY (3,099–3,691 USD) per pneumococcal bacteraemia, 767,447–848,255 JPY (6,977–7,711 USD) per pneumococcal meningitis, and 79,000 JPY (718 USD) per pneumococcal acute otitis media episodes. In adults and the elderly, the direct cost of pneumococcal pneumonia was 348,280–389,630 JPY (3,166–3,542 USD). The average hospital stay length was 7.2–31.9 days in children, 9.0 days in adults and 9.0–28.7 days in adults and the elderly.
Conclusions
The epidemiological burden of PDs remains high in Japan, especially among children and the elderly with invasive PDs accounting for a very small proportion of all PDs. A significant impact of the PCV13 vaccine program was reported, while the PPV23’s impact remains unclear. A substantial decrease in quality-adjusted life years in adults and the elderly and a high economic burden may exist.
Introduction
Streptococcus pneumoniae (Pneumococcus) can cause a range of illnesses such as ear infections to serious sepsis, meningitis, and pneumonia with bacteremia or without bacteremia [Citation1]. Infections with S. pneumoniae, named pneumococcal diseases, affect people of all ages, particularly those with underlying illnesses, and pose a major threat [Citation2]. According to the World Health Organization (WHO), pneumococcal diseases are one of the leading causes of mortality and morbidity. It is estimated that up to 1.6 million people die of pneumococcal diseases each year globally, especially young children and the elderly who tend to have more severe symptoms and complications in comparison to adults [Citation3]. In Japan, the Ministry of Health, Labour and Welfare in the statistics for 2019 identifies pneumonia as the 5th most common cause of death in individuals ≥65 years of age, and the 4th most common cause of death in individuals ≥75 years of age [Citation4]. Pneumococcal infections can also result in long-term problems, such as brain damage or hearing loss [Citation5]. Pneumococcal diseases are classified into invasive pneumococcal diseases (IPDs) and non-invasive pneumococcal diseases (non-IPDs), defined by how the bacteria invade parts of the body that are normally sterile. A non-IPD occurs outside of the tissues and fluids of major organs or the blood, while an IPD occurs inside the tissues and fluids of major organs or the blood. In general, IPDs are associated with more severe manifestations than non-IPDs [Citation3]. whereas non-IPDs have a much higher incidence in the elderly and people with a weakened immune system [Citation6]. Therefore, both IPDs and non-IPDs are clinically serious infections.
Given the heavy burden of pneumococcal diseases on morbidity and mortality, in April 2013, the Ministry of Health, Labour and Welfare (MHLW) designated IPDs as a notifiable disease by the Infectious Diseases Control Law [Citation7].
MHLW has also introduced multiple pneumococcal vaccination programs since 2006 for children and the elderly () [Citation8]. The pneumococcal conjugate vaccine (PCV) 7 was first introduced voluntarily for young children below the age of 5 years by a governmental subsidy in November 2010 [Citation9]. PCV7 was then officially incorporated into the national immunization program in April 2013 [Citation10]. Subsequently, PCV13 was introduced and replaced PCV7 in November 2013 [Citation11]. The use of PCV13 expanded to adults of 65 years or older in June 2014 [Citation12]. In October 2014, PPV23 was introduced in Japan’s national immunization program for the elderly [Citation13]. PCV10 was approved for use in children up to 5 years of age in March 2015 [Citation14], although it had yet to be launched on the market in Japan at the time of writing this manuscript (October 2020) [Citation15]. In parallel, a national surveillance system in Japan collects and makes available data on IPDs, yet a national surveillance system for other pneumococcal diseases, including non-IPDs has not been established to date. As a result, surveillance by individual investigators has started in recent years and data on the burden of non-IPDs, such as pneumococcal pneumonia, are gradually being collected [Citation6,Citation16].
Table 1. Timings of approved and publicly funded main vaccines.
Epidemiology, health economic, and patient-reported outcomes are important outcomes for evaluating pneumococcal vaccine programs by decision-makers. Such evidence in Japan has continuously been updated over the years but has not been systematically reviewed and published. Therefore, the objective of the study was to assess the epidemiological, humanistic, and economic burden, as well as treatment adherence and compliance and serotype distribution associated with pneumococcal diseases in Japan.
Methods
The search was performed in the Medline database (access via the OVID interface) and the ICHUSHI database. Additionally, the Database of Grants-in-Aid for Scientific Research (KAKEN) [Citation17] and the National Institute of Infectious Diseases (NIID) [Citation18] websites were searched. Only publications in English and Japanese and studies published between January 2005 and June 2020 were considered. The list of titles, abstracts and full texts were screened by one reviewer according to the defined inclusion and exclusion criteria, in order to select relevant articles pertaining to the topic of interest. Search strategies are presented in Supplementary Table 1–Supplementary Table 6. A simplified search strategy was used for hand searches. ‘Pneumococcus’ was used as the free search term for clinical studies and results were limited to only completed studies (KAKEN, NIID). The inclusion criteria are reported as per the PICOS criteria and presented in Supplementary Table 7. Cost-effectiveness analyses with source data not meeting the inclusion criteria were excluded from the study even if the target population of the cost-effectiveness analysis (CEA) met the inclusion criteria.
When reporting outcomes, point estimate is reported if only one data point from a study was identified and a range is reported if several data points from one or more studies were identified. The findings are categorized by study types. For epidemiology, including incidence, prevalence, and serotype distribution, and economic burden, the following categories are used: all, nationwide or multi-prefecture, large sample size (N ≥ 400), and PD types (IPD, all other PDs). Specifically for epidemiology, nationwide or multi-prefecture and large sample size (N ≥ 400) studies are further categorized into general and specific populations. In this study, the general population is defined as an overall population of the respective study location that includes both healthy and unhealthy people whereas a specific population is defined as those with specific conditions, hospitalized or with community-acquired pneumonia (CAP). For humanistic burdens, the following categories are used: all, nationwide or multi-prefecture, and large sample size (N ≥ 400).
For the JPY to USD conversion, a rate of 1 USD = 110 JPY is used (as of 17 September 2021) [Citation19].
Results
A total of 108 studies were identified across all three domains. The majority of the studies were small scale, regional studies, with limited clinical settings and populations. The included studies varied greatly with respect to population, studied diseases, geographical areas, time-periods, clinical settings, and sample size, leading to a wide range of values for all outcomes.
Epidemiology review
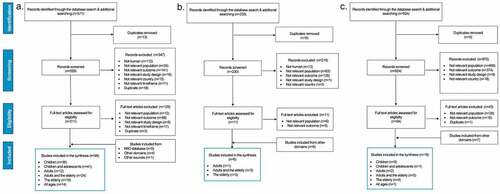
Overall, 96 studies were identified, of which 36 were on children, 41 were on children and adolescents, 12 were on adults, 24 were on adults and the elderly, 19 were on the elderly, and 14 were on all ages (with no age limitation). Regarding reported indices, 69% (66) of studies reported serotype distribution, 35% (34 studies) derived prevalence, and 24% (23 studies) provided incidence. No studies reporting outcomes related to treatment adherence and compliance were identified. depicts the flow of information through the literature search on the epidemiology of pneumococcal diseases. depicts the results of the epidemiology review.
Table 2. Summary of studies for the epidemiology review.
Table 3. Summary of studies for the humanistic burden review.
Figure 1. PRISMA diagram of the search results for the epidemiology (A), humanistic burden (B) and economic burden (C) review.
Incidence
According to nationwide or multi-prefecture surveillance studies, the annual reported numbers of overall incidence of IPDs from 2013 to 2017 were 4.98–9.47 per 100,000 population for children between the ages of 0 and 4 years, 0.36 per 100,000 population for children and adolescents between the ages of 5 and 14 years (from April 2013 to Mar 2014), 0.46 per 100,000 population for adults between the ages of 15 and 64 years (from April 2013 to Mar 2014), and 1.50–5.38 per 100,000 population for the elderly (from 2013 to 2017) [Citation8,Citation20]. They also showed a consistent increase in the numbers of reported IPD cases for children and the elderly after 2013 [Citation8].
In children, studies on the incidence of IPDs, covering time periods before and after the introduction of PCV7 in 2010, showed a reduction from 24.6 cases per 100,000 population in 2008 to 10.7 cases per 100,000 population in 2013 [Citation21]. After the switch from PCV7 to PCV13 in 2013, the incidence of IPDs further decreased to 10.3 in 2014 [Citation21]. Thereafter, the incidence of IPDs showed a gradual increase at about half of the level before the PCV7 introduction [Citation21]. Similar trends of a significant reduction in IPD incidence after the introduction of PCV7 were observed in subsequent years [Citation22]. Conversely, in the elderly, the reported number of IPDs continuously increased from 1.50 cases to 5.38 cases per 100,000 population between 2013 and 2017 [Citation8].
The incidence of community-onset pneumonia (COP) caused by S. pneumoniae for adults was reported to be 0.8–3.8 cases per 1,000 population in 15–64-year-olds and 5.1–16.9 cases per 1,000 population aged ≥65 years in 2012 [Citation6]. Based on the data available, it can be shown that IPD accounts for a very small proportion of all pneumococcal disease. For example, in adults ≥65 years, IPD accounts for approximately 1% of all pneumococcal diseases at most [Citation6,Citation8].
Prevalence
No studies reporting the prevalence of population-based IPD/non-IPD such as surveillance were identified and most of the identified studies reported data for those who have a specific disease/symptom/pathogen among a specific population. According to a large sample size survey conducted at emergency departments between 2002 and 2015, the prevalence of patients with a positive blood culture for S. pneumoniae in children aged 3–36 months old was 0.79% of 22,951 blood samples [Citation23]. Higher prevalence rates of patients with blood culture positive for S. pneumoniae were reported in Chiba (one of the prefectures in eastern part of Japan): 1.2% among 410 children aged <5 years hospitalized for CAP between April 2008 and March 2009 in Chiba [Citation24] and 0.6% of 7,140 blood samples taken from patients aged up to 15 years of age between 2010 and 2016 [Citation25]. The prevalence of adults and the elderly with a positive sputum culture for S. pneumoniae in patients with COP aged ≥15 years was as high as 9% between September 2001 and January 2013 [Citation6]. Conversely, administrative database analysis reported similar results of the prevalence of IPDs among hospitalized CAP patients aged ≥65 years at 1.3% between June 2014 and May 2015 [Citation26].
Serotype distribution
The serotype distribution presented similar trends over time across all age groups.
In children, before the introduction of PCV7 in 2010, the prevalence rates of PCV7 and PCV13 serotypes were as follows: 70.6%–81.3% among IPDs [Citation22,Citation27–31] and 62.7%–68.4% among all other PDs [Citation24,Citation32,Citation33] for PCV7 serotypes; and 83.1% among IPDs [Citation28–30] and 80.4%–86.0% among all other PDs [Citation24,Citation32] for PCV13 serotypes. After the switch from PCV7 to PCV13 in 2013, PCV7 and PCV13 type serotypes became less prevalent (0% among IPDs [Citation21,Citation34,Citation35] and nearly 0% among all other PDs, including acute otitis media [Citation36–38] for PCV7 serotypes; 4.0%–5.0% among IPDs [Citation21,Citation34] and 19.1% among all other PDs [Citation36–38] for PCV13 serotypes).
In children and adolescents, PCV7 and PCV13 serotypes were also reported to be prevalent before 2010 (66.7% [Citation39]–100% [Citation40] among IPDs and 49.3% [Citation41]–69.1% [Citation42] among all other PDs for PCV7 serotypes; 81.0%–100.0% [Citation39] among IPDs and 70.6% [Citation41]–83.2% [Citation42] among all other PDs for PCV13 serotypes). Similar to children, after the introduction of PCV7 and PCV13 in 2013, the vaccine-type serotypes also became less prevalent (0.0% [Citation25,Citation34,Citation36,Citation43]–2.3% [Citation44] among IPDs and 0.0% [Citation45–48]–7.1% [Citation49] among all other PDs for PCV7 serotypes; 0.0% [Citation25]–20.0% [Citation34] among IPDs and 6.2% [Citation47]–30.0% [Citation45] among all other PDs for PCV13 serotypes). When considering nationwide and multi-prefectural studies only, PCV7 and PCV13 serotypes among IPDs before 2010 were reported to be 71.8% [Citation27]–75.4% [Citation50] and 93.7% [Citation50], but decreased to 0.0% [Citation36]–2.3% [Citation44] and 7.0% [Citation36]–17.2% [Citation44] after 2013, respectively.
The NIID reported serotype coverages of PCV13 and PPV23 for IPD adults aged 15 years and over and the elderly between 2013 and 2017 [Citation51]. PCV13 serotype coverage started at 43.7% in 2013, went down to 30.1% in 2016 and then became stable at around 30% in 2017. In contrast, PPV23 serotype coverage started at 64.0% in 2013, then increased to 69.0% in 2014, and gradually decreased to 63.5% in 2017 [Citation51]. Furthermore, PCV13 serotypes in patients with IPDs decreased from 74.1% between April 2010 and March 2011 to 41.3% from April 2014 to March 2017, around the time period of the pediatric vaccine programs [Citation44]. At the same time, PPV23 serotypes also decreased over time from 86.5% in 2010–2011 to 75.0% between 2011 and 2014 and further down to 69.1% between 2014 and 2017 [Citation44]. On the contrary, PPV23 serotypes not included in PCV13 increased from 12.4% between 2010 and 2011 to 27.8% between 2014 and 2017 [Citation44].
A similar trend of PCV13 and PPV23 serotypes was observed in studies focusing on the elderly after 2013 [Citation52]. They also reported a significant reduction in PCV13 serotypes, a decrease of PPV23 serotypes, and an increase of PPV23 serotypes not included in PCV13 [Citation52].
Humanistic burden review
None of the included studies presented results related to health-related quality-of-life (HRQoL) for pneumococcal diseases and only studies on patient reported outcomes were identified. However, CAP severity staging scales such as A-DROP, CURB65, and the Pneumonia Severity Index (PSI), were reported in 6 studies for adults and the elderly. depicts the flow of information through the literature search on the humanistic burden. Among adults, the mean scores for PSI and CURB65 were estimated as 28.2 and 0.5, respectively [Citation53]. Among adults and the elderly, the proportion of patients with pneumococcal pneumonia with a severe and moderate stage measured by PSI were estimated 21.3% [Citation54]–23.4% [Citation52] and 37.1% [Citation54]–41.5% [Citation52], respectively. The elderly reported more severe results than adults, with the estimated mean scores for PSI and CURB65 of 105.6 and 1.9, respectively [Citation53]. The proportion of elderly patients with a CURB65 of 3 (severe) was estimated to be 61.0% [Citation55]. presents the results of a humanistic burden review.
Economic burden review
Overall, 18 studies were identified. Half of the studies (n = 9) focused on children, 1 study focused on children and adolescents, 4 studies focused on adults and the elderly, 4 studies focused on the elderly, and 1 study focused on all ages (no age limit). Sixteen studies reported outcomes related to resource use, followed by direct costs (8 studies), indirect costs (2 studies), and productivity loss (2 studies). No studies reporting indirect costs or productivity loss for adults and the elderly were identified. shows the flow chart of the study selection process focused on the economic burden, while a summary of the studies selected is presented in .
Table 4. Summary of the studies for the economic burden review.
Direct costs
In children, direct costs per episode were estimated at 340,905 [Citation56]–405,978 JPY [Citation57] for pneumococcal bacteremia, 767,447 [Citation56]–848,255 JPY [Citation57] for pneumococcal meningitis, and around 79,000 JPY for pneumococcal acute otitis media [Citation56,Citation58]. Higher direct costs for death cases were reported for pneumococcal bacteremia (1,010,205–1,032,126 JPY [Citation57]) and for pneumococcal meningitis (1,470,421–1,510,669 JPY [Citation57]). In adults and the elderly, direct costs of pneumococcal pneumonia were reported to be 348,280–389,630 JPY [Citation59]. In the elderly, direct costs of pneumococcal pneumonia and CAP with IPD were estimated at 788,343 JPY [Citation60] and 864,405 JPY [Citation26] Footnote1, respectively.
Indirect costs
Indirect costs were only reported for children. Indirect costs related to pneumococcal bacteremia, meningitis, and pneumonia were estimated at 122,176 JPY, 241,164JPY [Citation58] and 104,455 JPY [Citation61], respectively.
Productivity loss
Productivity loss was only reported for children’s caregivers. The productivity loss of hospitalized pneumococcal bacteremia and meningitis cases were reported to be 7.9 days [Citation56] – 11.5 days [Citation58] and 14.6 days [Citation56] – 22.7 days per episode [Citation58], respectively.
Resource use
The average length of hospital stay (ALOS) in children was estimated at 7.2 [Citation56] – 11.5 days [Citation57] for pneumococcal bacteremia and 13.8 [Citation56] – 31.9 days [Citation57] for pneumococcal meningitis. In adults, ALOS was estimated at 9.0 days [Citation53] for pneumococcal pneumonia, while in adults and the elderly, at 9.0 [Citation59]–16.4 days [Citation62] for pneumococcal pneumonia and CAP caused by S. pneumoniae combined and 28.7 days [Citation63] for pneumococcal bacteremia. Other studies reported data on the number of visits to general practitioners and drug use. Among children, the number of visits to general practitioners per episode was estimated at 1.4 [Citation64] – 2.9 [Citation57] for pneumococcal bacteremia and 1.5 [Citation64] – 8.1 [Citation57] for pneumococcal meningitis [Citation65].
Discussion
The epidemiological burden of pneumococcal diseases remains high in Japan, especially among children and the elderly. A significant reduction in the incidence of pediatric IPDs was observed after the PCV7 and PCV13 vaccine programs. Conversely, similar trend was not observed for IPDs on the elderly after the PPV23 vaccine program; in fact, the incidence of IPDs among the elderly increased after 2013 [Citation8]. Further studies are needed to better understand the potential impact of the pneumococcal vaccination program among the elderly. It is expected that the impact of vaccination programs would depend on the coverage rates of PCV13 and PPV23 among the target population. Under the National Immunization Program, the coverage rates of PPV23 vaccine for the elderly were reported as 32–38% after 2014 and PCV13 vaccine for children as 95–100% (after 2013) [Citation66]. Another study reported the coverage of PPV23 and PCV13 vaccines for elderly in 2018 as 32% and 0.7%, respectively [Citation67]. Also, of note, case definition of IPD has changed in November 2016 with the addition of the detection of bacteria from other sterile sites other than blood and spinal fluid to the notification criteria. While this change has only resulted in 13 cases (0.2%) in 2016 and has not had much impact at this time, careful monitoring of the trend may be required to assess its impact [Citation68].
Vaccination programs have also changed the serotype distribution. After the introduction of PCV7 and PCV13 into the national immunization program, the PCV13 serotype coverage in pediatric IPDs considerably declined. Similarly, after the introduction of PPV23 into the national immunization program, the PPV23 serotype coverage in IPDs in the elderly also decreased. However, when examined in detail, limited data showed that the serotype coverage of PPV23 serotypes not included in PCV13 steadily increased during the same time period. Herd immunity of the PCV13 vaccination in children may have contributed to this trend. A change in serotype distribution would have a huge impact on the overall efficacy and cost-effectiveness of a particular vaccination policy. Therefore, up-to-date data on serotype distribution would be crucial for decision makers around the National Immunization Program.
The present literature review did not identify any studies on HRQoL and only studies on patient reported outcomes were identified for the humanistic burden review. Nevertheless, when studies beyond the scope of this literature review are examined, studies could be found like Glick et al. that recently reported HRQoL outcomes in Japanese adults and elderly people with CAP [Citation16]. QALYs were collected using the Japanese version of the EuroQol-5D-5 L health-state classification instrument at days 0, 7, 15, 30, 90, 180 and 365 after a pneumonia diagnosis from participants enrolled between 2017 and 2018. The adjusted EuroQol-5D-5 L scores were 0.759 at day 30, 0.561 at diagnosis, 0.702 by day 180 and 0.689 by day 365. Pneumonia resulted in a mean adjusted loss of 0.13 QALYs at 365 days [Citation16]. In another study from Belgium, IPDs resulted in a loss in QALY over a year at 0.0203 in patients between the ages of 50 and 64 years and 0.1741 in patients ≥65 years of age [Citation69].
Limited data on the economic burden related to pneumococcal diseases suggest a high burden posed on patients, with direct costs ranging from 340,905 to 405,978 JPY (3,099–3,691 USD) and from 767,447 to 848,255 JPY (6,977–7,711 USD) for pneumococcal bacteremia and meningitis, respectively. Complications due to pneumococcal diseases, namely neurological sequelae and hearing loss, as well as death, have the highest economic burden, which lead to increased costs [Citation56,Citation58]. Regarding resource use among children, ALOS was estimated as 7.2 [Citation56]–11.5 days [Citation56] for pneumococcal bacteremia and 13.8 [Citation56]–31.9 days [Citation57] for pneumococcal meningitis. Among adults and the elderly, ALOS was estimated as 9.0 [Citation59]–16.4 days [Citation62] for pneumococcal pneumonia and CAP caused by S. pneumoniae combined and 28.7 days [Citation63] for pneumococcal bacteremia.
The limitation of the present review is the heterogeneity of the studies included in terms of population, studied diseases, geographical areas, time-periods, clinical settings, methods, and sample size, as well as limited data available in certain domains (e.g., on economic burden) resulting in a high degree of data variations, which might cause difficulties in providing conclusive evidence on the magnitude of the burden or the impact of vaccine programs (e.g., on serotype distribution). This is especially true for non-IPDs where a national surveillance system has not been established to date in Japan. A comprehensive national surveillance system may be needed including prevalence, not only for IPDs but also for non-IPDs. Furthermore, heterogeneity may lead to potential biases, posing challenges to the generalizability of the findings. Despite these limitations, our findings reveal important data on the burden of pneumococcal diseases, which may support the management of vaccination programs among different age groups in Japan. Currently, pneumococcal vaccines with greater serotype coverage are being developed worldwide for children and the elderly. Then, updated information such as serotype distributions and HRQoL data would be crucial for decision makers of the National Immunization Program.
Conclusions
The epidemiological burden of pneumococcal diseases remains high in Japan, especially among children and the elderly. Given the heavy burden of pneumococcal disease, especially CAP, prevention via vaccination is a crucial tool to control the outbreak of the disease. Coordinated effort to collect evidence on all types of PDs may greatly contribute to the assessment of the disease burden as well as overall efficacy and cost-effectiveness of vaccination programs. Continued discussions on the required data needs would be beneficial in making effective policy decisions. According to the trend of serotype distributions, a significant reduction in the PCV13 serotypes was observed, while it was unclear for non-PCV13 serotypes of PPV23. Although other sources indicate a substantial decrease in QALYs in the adult and elderly Japanese populations suffering from CAP, no evidence was found on the effect of pneumococcal diseases on HRQoL, which warrants further studies in a real-world setting. A high economic burden of pneumococcal diseases may exist despite only limited evidence being available.
Article highlights
The study investigates the burden of pneumococcal diseases on the Japanese population by age groups.
The review presents comprehensive data on epidemiology; humanistic and economic burden; treatment adherence and compliance; and serotype distribution associated with pneumococcal diseases in Japan.
The heterogeneity of the studies included may hamper the assessment of the magnitude of the burden and limit the generalizability of the findings.
Supplemental Material
Download MS Word (77.1 KB)Acknowledgments
Anna Jakubowska, a former employee of Creativ-Ceutical provided technical support. Medical writing support was provided by Małgorzata Biernikiewicz of Creativ-Ceutical.
Disclosure statement
Ataru Igarashi reports grants and other from Gilead Sciences KK., grants from Intuitive Surgical GK., grants from Boston Scientific Japan Inc., grants and personal fees from Pfizer Japan Inc., grants from Beckton Dickinson and Company, grants from Milliman Inc., personal fees and other from Terumo corporation, personal fees from Chugai Pharmaceuticals Inc., personal fees from Astellas Pharma Inc., other from Fuji film Inc., other from CSL Behring Japan Inc., personal fees from Sanofi Japan Inc., personal fees and other from Takeda Pharmaceutical Inc., personal fees from Nippon Boeringer Ingelheim Inc., personal fees from Ono pharmaceutical Inc., personal fees from Taiho pharmaceutical Co. Ltd., personal fees from Eisai Inc., personal fees from Abbvie GK, personal fees from Sumitomo Dainippon Pharma Inc., personal fees from Ayumi Pharmaceutical Inc., personal fees from Medilead Inc., personal fees from Novo Nordisk Japan Inc., personal fees from Novartis Pharma Inc., personal fees from GSK Inc., outside the submitted work. Maki Ueyama, Koki Idehara and Mariko Nomoto report grants from Pfizer Japan, during the conduct of the study.
Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
Notes
1 The cost estimates were taken from the additional file of Konomura et al. [Citation25]. While USD is used in the main text as the unit of the cost estimates, no unit was mentioned in the additional file. Therefore, we assume that the unit used in the additional file is in JPY.
References
- Matanock A, Lee G, Gierke R, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68(46):1–14.
- Committee for discussing Pneumococcal Vaccine Revaccination, National Institute of Infectious Diseases (NIID) Japan. [Guidelines on Pneumococcal Vaccine Revaccination]. 2009. [cited 2020 Dec 7]. Available from: http://www.kansensho.or.jp/uploads/files/guidelines/pneumococcus_vaccine.pdf
- World Health Organization. Pneumococcal disease [cited 2020 Mar 25]. Available from: https://www.who.int/ith/diseases/pneumococcal/en/
- Vital, Health and Social Statistics Office, Ministry of Health, Labour and Welfare. [Number of deaths, confirmed numbers, vital Statistics]. 2020. [updated 17 Sept 2020; cited 2020; cited 2020 Sept 2020; cited 2020 17 Dec 17 Sept 2020; cited 2020 17]. Available from: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450011&tstat=000001028897&cycle=7&year=20190&month=0&tclass1=000001053058&tclass2=000001053061&tclass3=000001053065&stat_infid=000031982756&result_back=1&result_page=1&tclass4val=0
- National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases, Centers for Disease Control and Prevention (CDC). About pneumococcal disease. [updated 21 Nov, 2019; cited 2019; cited 2020 Nov, 2019; cited 2020 25 Mar 21 Nov, 2019; cited 2020 25]. Available from: https://www.cdc.gov/pneumococcal/about/index.html
- Morimoto K, Suzuki M, Ishifuji T, et al. The burden and etiology of community-onset pneumonia in the aging Japanese population: a multicenter prospective study. PLoS One. 2015;10(3):e0122247.
- Health Service Bureau, Ministry of Health, Labour and Welfare. [Regarding the Enforcement, etc. of the Ministerial Order Partially Amending the Enforcement Regulation of the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases (the Infectious Diseases Control Law) (Enforcement Notice)]. (No. 0307-(1) dated 7 March 2013). 2013. [cited 2020 Oct 15]. Available from: https://www.mhlw.go.jp/web/t_doc?dataId=00tb9101&dataType=1&pageNo=1
- National Institute of Infectious Diseases (NIID) Japan. Pneumococcal infections in 2017, Japan. IASR2018. p. 107–108.
- Health Service Bureau and Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare. [Regarding the Emergency Project for the Promotion of Vaccination Against Cervical Cancer, etc.] (No. 1126-(10) dated 26 November 2010). 2010. [cited 2020 Oct 15]. Available from: https://www.mhlw.go.jp/bunya/kenkou/other/dl/101209i.pdf
- Health Service Bureau, Ministry of Health, Labour and Welfare. [Regarding the Enforcement, etc. of the Act Partially Amending the Immunization Act] (No. 0330-(1) dated 30 March 2013)0. 2013. [cited 2020 Oct 15]. Available from: https://www.mhlw.go.jp/topics/bcg/tp250330-2.html
- Health Service Bureau, Ministry of Health, Labour and Welfare. [Regarding the enforcement, etc. of the ministerial order partially amending the enforcement regulation of the immunization act and the immunization practice regulation] (no. 0911-(1) dated 11 september 2013). 2013. [cited 2020 Oct 15]. Available from: https://www.mhlw.go.jp/web/t_doc?dataId=00tb9595&dataType=1&pageNo=1
- National Institute of Infectious Diseases (NIID) Japan. [Fact sheet on 13-valent pneumococcal conjugate vaccine (for Adults)] [updated 28 Jul 2015; cited 2015; cited 2020 Jul 2015; cited 2020 31 Jul 28 Jul 2015; cited 2020 31]. Available from: https://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/0000093331.pdf
- Health Service Bureau, Ministry of Health, Labour and Welfare. [Regarding the enforcement of the cabinet order partially amending the order for enforcement of the immunization act, and the ministerial order partially amending the enforcement regulation of the immunization act and the immunization practice regulation] (No. 0716-(24) dated 16 July 2014). 2014. [cited 2020 Oct 15]. Available from: https://www.mhlw.go.jp/web/t_doc?dataId=00tc0252&dataType=1&pageNo=1
- National Institute of Infectious Diseases (NIID) Japan. [Fact sheet on 10-valent pneumococcal conjugate vaccine] [updated 2016; cited 2020 Jan 2016; cited 2020 1 Jul 28 Jan 2016; cited 2020 1]. Available from: https://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/02shiryo1betten.pdf
- Pharmaceuticals and Medical Devices Agency (PMDA) Japan. [Information on updates of package insert within one month (9 December 2017)]. [cited 2020 Dec 17]. Available from: https://www.info.pmda.go.jp/psearch/tenpulist.jsp?DATE=20171209
- Glick HA, Miyazaki T, Hirano K, et al. One-year quality of life post-pneumonia diagnosis in Japanese adults. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2020 May 24;ciaa595.
- National Institute of Informatics (NII) Japan. [Database of Grants-in-Aid Scientific Research (KAKEN)]. [cited 2020 Jun 2]. Available from: https://kaken.nii.ac.jp/
- National Institute of Infectious Diseases (NIID) Japan. National institute of infectious diseases. [cited 2020 Dec 11]. Available from: https://www.niid.go.jp/niid/en/
- Exchange rate for October 2021. Bank of Japan. 2021. [01 October 2021]. Available from: https://www.boj.or.jp/about/services/tame/tame_rate/kijun/kiju2110.htm
- National Institute of Infectious Diseases (NIID) Japan. Invasive Haemophilus influenzae and Streptococcus pneumoniae infections, as of August. 2014. IASR2014. p. 229–230.
- Suga S, Togashi T, Hosoya M, et al. [Current situation of invasive pneumococcal disease among children following the introduction of 13-valent pneumococcal conjugate vaccine]. IASR2018. p. 112–113.
- Suga S, Chang B, Asada K, et al. Nationwide population-based surveillance of invasive pneumococcal disease in Japanese children: effects of the seven-valent pneumococcal conjugate vaccine. Vaccine. 2015;33(45):6054–6060.
- Kamidani S, Shoji K, Ogawa E, et al. High rate of febrile seizures in Japanese children with occult bacteremia. Pediatr Emerg Care. 2017;36(4):e199–e203.
- Naito S, Tanaka J, Nagashima K, et al. The impact of heptavalent pneumococcal conjugate vaccine on the incidence of childhood community-acquired pneumonia and bacteriologically confirmed pneumococcal pneumonia in Japan. Epidemiol Infect. 2016;144(3):494–506.
- Ohtake S, Okada H, Hiramoto R. [The trend of invasive pneumococcal disease after introduction of pneumococcal conjugate vaccine]. Jpn J Pediatr. 2019. 06. 72(6):763–769.
- Konomura K, Nagai H, Akazawa M. Economic burden of community-acquired pneumonia among elderly patients: a Japanese perspective. Pneumonia. 2017;9(1):19.
- Chiba N, Morozumi M, Shouji M, et al. Rapid decrease of 7-valent conjugate vaccine coverage for invasive pneumococcal diseases in pediatric patients in Japan. Microb Drug Resist. 2013;19(4):308–315.
- Oishi T, Wada A, Chang B, et al. Serotyping and multilocus sequence typing of Streptococcus pneumoniae isolates from the blood and posterior nares of Japanese children prior to the introduction of 7-valent pneumococcal conjugate vaccine. Jpn J Infect Dis. 2011;64(4):341–344.
- Sakai F, Chiba N, Ono A, et al. Molecular epidemiologic characteristics of Streptococcus pneumoniae isolates from children with meningitis in Japan from 2007 through 2009 [原著論文]. [2007〜2009年の日本における髄膜炎小児からのStreptococcus pneumoniae分離株の分子疫学的特性]. J Infect Chemother. 2011 06; 17(3): 334–340.
- Sakata H. Invasive Streptococcus pneumoniae infections in children in Kamikawa and Soya subprefecture, Hokkaido, Japan, 2000-2010, before the introduction of the 7-valent pneumococcal conjugate vaccine [原著論文]. [北海道の上川地方と宗谷地方の小児における7価肺炎球菌共役ワクチン導入前の2000〜2010年の侵襲的肺炎連鎖球菌感染症]. J Infect Chemother. 2011 12;17(6):799–802.
- Nishimura T, Fukazawa M, Yoshida H, et al. [Clinical epidemiological study of occult pneumococcal bacteremia in a pediatric outpatient setting]. J Jpn Pediatr Soc. 2008 06;112(6):973–980.
- Hotomi M, Billal DS, Kamide Y, et al. Serotype distribution and penicillin resistance of Streptococcus pneumoniae isolates from middle ear fluids of pediatric patients with acute otitis media in Japan. J Clin Microbiol. 2008;46(11):3808–3810.
- Kamiya H, Kato T, Togashi T, et al. [Epidemiological survey of pneumococcus serotypes in pediatric patients with acute suppurative otitis media] [原著論文]. J Jpn Assoc Infect Dis. 2007 01; 81(1): 59–66.
- Nakanishi N, Yonezawa T, Tanaka S, et al. Assessment of the local clonal spread of Streptococcus pneumoniae serotype 12F caused invasive pneumococcal diseases among children and adults. J Infect Public Health. 2019;12(6):867–872.
- Kawahara R, Yamaguchi T, Katsukawa C, et al. [Serotype distribution of Streptococcus pneumoniae strains causing invasive pneumococcal disease in Osaka Prefecture, 2014-2017]. IASR2018. p. 110–111.
- Nakano S, Fujisawa T, Ito Y, et al. Nationwide surveillance of paediatric invasive and non-invasive pneumococcal disease in Japan after the introduction of the 13-valent conjugated vaccine, 2015-2017. Vaccine. 2020;38(7):1818–1824.
- Mokuno E, Morozumi M, Ubukata K, et al. [Epidemiology of acute otitis media in children after introduction of the 13-valent pneumococcal conjugate vaccine] [原著論文]. Nippon Jibiinkoka Gakkai Kaiho. 2018 07; 121(7): 887–898.
- Miyazaki H, Shibuya R, Midorikawa N, et al. Serotype distribution and antimicrobial susceptibility of Streptococcus pneumoniae strains isolated in Japan after introduction of the routine immunization program. J Infect Chemother. 2017;23(4):234–240.
- Tanaka J, Ishiwada N, Wada A, et al. Incidence of childhood pneumonia and serotype and sequence-type distribution in Streptococcus pneumoniae isolates in Japan. Epidemiol Infect. 2012;140(6):1111–1121.
- Miyahara H, Maruyama H, Kanazawa A, et al. Changes in the features of invasive pneumococcal disease after introduction of the seven-valent pneumococcal conjugate vaccine in a regional core hospital of Kochi, Japan. Acta Med Okayama. 2015;69(4):255–260.
- Okade H, Funatsu T, Eto M, et al. Impact of the pneumococcal conjugate vaccine on serotype distribution and susceptibility trends of pediatric non-invasive Streptococcus pneumoniae isolates in Tokai, Japan over a 5-year period. J Infect Chemother. 2014;20(7):423–428.
- Chiba N, Kobayashi R, Hasegawa K, et al. Antibiotic susceptibility according to genotype of penicillin-binding protein and macrolide resistance genes, and serotype of Streptococcus pneumoniae isolates from community-acquired pneumonia in children. J Antimicrob Chemother. 2005;56(4):756–760.
- Takemoto T, Matsubara K, Isome K, et al. [Invasive pneumococcal disease in children before and after the introduction of pneumococcal conjugate vaccine at a regional center in Kobe, Japan, 2002-2018] [原著論文]. J Jpn Assoc Infect Dis. 2019 07;93(4):485–492.
- Ubukata K, Takata M, Morozumi M, et al. Effects of pneumococcal conjugate vaccine on genotypic penicillin resistance and serotype changes, Japan, 2010-2017. Emerg Infect Dis. 2018;24(11):2010–2020.
- Takeuchi N, Naito S, Ohkusu M, et al. Epidemiology of hospitalised paediatric community-acquired pneumonia and bacterial pneumonia following the introduction of 13-valent pneumococcal conjugate vaccine in the national immunisation programme in Japan. Epidemiol Infect. 2020;148:e91.
- Kadota T, Nomura N, Mitsuyama J, et al. [Sensitivity surveillance of Streptococcus pneumoniae isolates for several antibacterial agents in the Chubu region in Japan (2015-2016)] [原著論文]. Jpn J Antibiot. 2019 06;72(2):123–141.
- Nariai A. [Impact of the spread of pneumococcal conjugate vaccination on macrolide resistance in Streptococcus pneumoniae obtained from the nasopharynx of infants and young children] [原著論文]. Jpn J Antibiot. 2018. 03. 71(Suppl.A):61–66.
- Yanai T, Nariai A, Kanetaka T, et al. [Epidemiology of serotypes and drug-susceptibility of Streptococcus pneumoniae colonizing the nasopharynx in children (author’s transl)] [原著論文]. Kyosai Med J. 2018 05;67(2):201–205.
- Uozumi Y, Ozaki T, Nishimura N, et al. [Capsular serotypes of pediatric isolates of Streptococcus pneumoniae during one year from August 2016: comparison with those obtained in the two previous surveys] [原著論文]. Jpn J Med Technol. 2019 10;68(4):731–736.
- Chiba N, Morozumi M, Sunaoshi K, et al. Serotype and antibiotic resistance of isolates from patients with invasive pneumococcal disease in Japan. Epidemiol Infect. 2010;138(1):61–68.
- Shimbashi R, Fukusumi M, Shimada T, et al. [Clinical features of invasive pneumococcal disease among adults and analysis of serotype distribution of the causative bacteria]. Tokyo: IASR: NIID; 2018. p. 115–117.
- Akata K, Chang B, Yatera K, et al. The distribution and annual changes in the Streptococcus pneumoniae serotypes in adult Japanese patients with pneumococcal pneumonia from 2011 to 2015 [原著論文]. [2011〜2015年における日本人成人肺炎球菌性肺炎患者の肺炎連鎖球菌血清型の分布と経年変化]. J Infect Chemother. 2017 06; 23(5–6): 301–306.
- Akuzawa N, Naito H. Nutritional parameters affecting severity of pneumonia and length of hospital stay in patients with pneumococcal pneumonia: a retrospective cross-sectional study. BMC Pulm Med. 2015;15(1):149.
- Akata K, Chang B, Yatera K, et al. Distribution and annual changes in Streptococcus pneumoniae serotypes in adult Japanese patients with pneumonia. J Infect Chemother. 2015;21(10):723–728.
- Sando E, Suzuki M, Furumoto A, et al. Impact of the pediatric 13-valent pneumococcal conjugate vaccine on serotype distribution and clinical characteristics of pneumococcal pneumonia in adults: the japan pneumococcal vaccine effectiveness study (J-PAVE). Vaccine. 2019;37(20):2687–2693.
- Shiragami M, Mizukami A, Leeuwenkamp O, et al. Cost-effectiveness evaluation of the 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugate vaccine and 13-valent pneumococcal vaccine in Japanese children. Infect Dis Ther. 2014;4(1):93–112.
- Iwata S, Ishiwada N, Sakata H, et al. [Burden of illness of bacterial meningitis and bacteremia caused by Streptococcus pneumoniae in children] [原著論文]. Jpn J Pediatr. 2008 11;61(11):2206–2220.
- Suaya JA, Ohno T, Hilton B, et al. [Cost-effectiveness analysis of 13-valent versus 10-valent pneumococcal conjugate Vaccines as part of routine infant pneumococcal vaccination program in Japan] [原著論文]. Jpn J Pediatr. 2015 06;68(6):1197–1217.
- Uryu K, Nishiura S, Yamamoto T, et al. [Changes in medical treatment fees for pneumococcal pneumonia in our hospital before and after the introduction of DPC] [原著論文]. J Jpn Soc Clin Pathway. 2012 06;14(2):113–121.
- Satou M, Mutou M, Aoki H. [An disease burden and life convalescence of pneumococcal pneumonia of the elderly person - retrospective examination of a hospital the past three years] [原著論文]. Health Inf Manage. 2016. 03. 27(4):58–62.
- Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare. [Report on the deliberation results]. 2009. [updated 8 Sept; cited 2020 Sept; cited 2020 17 Nov 8 Sept; cited 2020 17]. Available from: https://www.pmda.go.jp/drugs/2009/P200900053/53039600_22100AMX02255_A100_1.pdf
- Pharmaceutical Safety Committee of the Pharmaceutical Affairs and Food Sanitation Council, Ministry of Health, Labour and Welfare. [Pediatric pneumococcal vaccination status and concurrent vaccination (provided by Pfizer Inc.)]. 2011. [cited 2020 Nov 17]. Available from: https://www.mhlw.go.jp/stf/shingi/2r9852000001dn2t-att/2r9852000001dn5f.pdf
- Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare. [Report on the deliberation results]. 2015. [updated 2020 Mar; cited 2020 17 Nov 10 Mar; cited 2020 17]. Available from: https://www.pmda.go.jp/drugs/2015/P201500029/342275000_22700AMX00660_A100_1.pdf
- Pharmaceuticals and Medical Devices Agency (PMDA) Japan. [Drug interview form “prevenar 13® suspension liquid for injection”]. 2020. [updated Oct; cited 2020 Oct; cited 2020 17 Nov 17]. Available from: https://www.info.pmda.go.jp/go/interview/2/672212_631140EC1022_2_1F.pdf
- Pharmaceuticals and Medical Devices Agency (PMDA) Japan. [Drug Interview Form “PNEUMOVAX® NP”]. 2020. [updated Oct; cited 2020 Oct; cited 2020 17 Nov 17]. Available from: https://www.info.pmda.go.jp/go/interview/2/170050_6311400A1037_2_016_1F.pdf
- Number of people administered routine vaccinations. 1995-2019.: Ministry of health, labour and welfare. [2021 Jun 26]. Available from: https://www.mhlw.go.jp/topics/bcg/other/5.html
- Nakamura A, Kawakami K, Wakana A, et al. A Japanese nationwide survey of 23-valent pneumococcal capsular polysaccharide vaccine (PPSV23) revaccination coverage rate among elderly adults aged 65 and older and physician’s attitude. Hum Vaccin Immunother. 2020 Sep 1;16(9):2292–2299.
- Reported number of invasive pneumococcal infections based on the Infectious Diseases Control Law. 2013-2017. National Institute of Infectious Diseases. [cited 2021 Jun 26]. Available from: https://www.niid.go.jp/niid/ja/pneumococcal-m/pneumococcal-idwrs/8041-ipd-180517.html
- Blommaert A, Bilcke J, Willem L, et al. The cost-effectiveness of pneumococcal vaccination in healthy adults over 50: an exploration of influential factors for Belgium. Vaccine. 2016 April 19;34(18):2106–2112.
- Shinjoh M, Yamaguchi Y, Iwata S. Pediatric bacterial meningitis in Japan, 2013-2015-3-5 years after the wide use of Haemophilus influenzae type b and Streptococcus pneumoniae conjugated vaccines. J Infect Chemother. 2017;23(7):427–438.
- Fukazawa M. [Efficacy of Hib and 7-valent pneumococcal vaccine from bacteremia cases for 11 years in practicing pediatrics (author’s transl)] [原著論文]. Fukuoka-Ken-Ihou. 2017;04(1490):57–59.
- Tamura YB, Matsubara K, Matsubara C, et al. [Trend of invasive pneumococcal disease before and after the introduction of pneumococcal conjugate vaccine in Hiroshima city] [原著論文]. J Pediatric Infect Dis Immunol. 2017 10;29(3):241–248.
- Sakata H. Invasive pneumococcal diseases in children in Hokkaido, Japan from April 2000, to March 2015. J Infect Chemother. 2016;22(1):24–26.
- Ishiwada N, Hishiki H, Nagasawa K, et al. The incidence of pediatric invasive Haemophilus influenzae and pneumococcal disease in Chiba prefecture, Japan before and after the introduction of conjugate vaccines. Vaccine. 2014;32(42):5425–5431.
- Nakamura R, Togashi T. Population-based incidence of invasive haemophilus influenzae and pneumococcal diseases before the introduction of vaccines in Japan. Pediatr Infect Dis J. 2013;32(12):1394–1396.
- Togashi T, Sakata H, Tsutsumi H, et al. [Epidemiology of bacteria meningitis in childhood just before the introduction of conjugate vaccines in Hokkaido, the Northernmost Island of Japan] [原著論文]. J Jpn Pediatr Soc. 2010 03;114(3):473–478.
- Higashigawa M, Suzuki M, Omori Y, et al. [Clinical investigation of 26 cases of bacteremia in infants and children] [原著論文]. J Jpn Pediatr Soc. 2009 10;113(10):1557–1563.
- Ishiwada N, Kurosaki T, Terashima I, et al. The incidence of pediatric invasive pneumococcal disease in Chiba prefecture, Japan (2003-2005). J Infect. 2008;57(6):455–458.
- Ogita J, Ishiwada N, Kurosaki T, et al. [Incidence of community-acquired pneumonia and pneumococcal pneumonia, among children in Chiba City, Japan]. J Jpn Assoc Infect Dis. 2008;82(6):624–627.
- Sakata H. [Study of Streptococcus pneumoniae bacteremia in children] [原著論文]. J Jpn Assoc Infect Dis. 2005 01;79(1):1–6.
- Takaki M, Nakama T, Ishida M, et al. High incidence of community-acquired pneumonia among rapidly aging population in Japan: a prospective hospital-based surveillance. Jpn J Infect Dis. 2014;67(4):269–275.
- Kubota T, Ishida M, Tokaji A, et al. [Current status of invasive pneumococcal disease in Kochi] [原著論文]. J Kochi Med Assoc. 2019 03;24(1):171–178.
- Griffith MM, Fukusumi M, Kobayashi Y, et al. Epidemiology of vaccine-preventable diseases in Japan: considerations for pre-travel advice for the 2019 Rugby World Cup and 2020 Summer Olympic and Paralympic Games. Western Pac Surveill Response J. 2018;9(2):26–33.
- Obara H, Saitou J, Fukuda H. [Increased burden on medical resources of penicillin-resistant Streptococcus pneumoniae infections: estimmates using JANIS data] [原著論文]. Jpn J Environ Infect. 2015 05;30(3):165–173.
- Hishiki H, Ishiwada N, Fukasawa C, et al. Incidence of bacterial coinfection with respiratory syncytial virus bronchopulmonary infection in pediatric inpatients. J Infect Chemother. 2011;17(1):87–90.
- Ishiwada N, Niwa K, Tateno S, et al. Pneumococcal endocarditis in children: a nationwide survey in Japan. Int J Cardiol. 2008;123(3):298–301.
- Ariga S, Imataka G, Yoshida A, et al. Bacteriological study of 53 children with bacterial meningitis in our hospital (2000-2017) [原著論文]. [当院(2000〜2017年)における細菌性髄膜炎の患児53名の細菌学的研究]. Dokkyo J Med Sci. 2017 07;44(2):169–171.
- Haro K, Ogawa M, Hoshina T, et al. Difference between Japanese secondary and tertiary medical facilities regarding changes in the hospitalization of children for pneumonia after the introduction of the pneumococcal conjugate vaccine. Jpn J Infect Dis. 2017;70(3):270–274.
- Hoshino T, Takeuchi N, Fukasawa C, et al. Analysis of Streptococcus pneumoniae and Haemophilus influenzae isolated from middle ear fluid before and after the introduction of government subsidies for pneumococcal and H. influenzae type b vaccines in Japan. J Infect Chemother. 2017;23(2):85–89.
- Nariai A, Uchimura T, Kanetaka T, et al. [Effects of widely used of 7-valent pneumococcal conjugate vaccine on serotypes of colonized Streptococcus pneumoniae infants and young children with lower respiratory tract infections] [原著論文]. J Pediatric Infect Dis Immunol. 2014 07;26(2):213–219.
- Otsuka T, Kitami O, Kondo K, et al. Incidence survey of acute otitis media in children in Sado Island, Japan–Sado Otitis Media Study (SADOMS). PLoS One. 2013;8(7):e68711.
- Takano M, Ozaki K, Nitahara Y, et al. Streptococcus pneumoniae and Haemophilus influenzae at the initial stage of influenza. Pediatr Int. 2009;51(5):687–695.
- Ishida T, Tachibana H, Ito A, et al. Clinical characteristics of severe community-acquired pneumonia among younger patients: an analysis of 18 years at a community hospital. J Infect Chemother. 2014;20(8):471–476.
- Kimura M, Kataoka K, Kato K, et al. [Clinical study of adult community-acquired pneumonia with respiratory failure in our hospital (author’s transl)] [原著論文]. Med J Tosei General Hospital. 2008;10(24):1–6.
- Oda K, Yatera K, Fujino Y, et al. Respiratory comorbidities and risk of mortality in hospitalized patients with idiopathic pulmonary fibrosis. Respir Investig. 2018;56(1):64–71.
- Kurai D, Sasaki Y, Saraya T, et al. Pathogen profiles and molecular epidemiology of respiratory viruses in Japanese inpatients with community-acquired pneumonia. Respir Investig. 2016;54(4):255–263.
- Yoshii Y, Shimizu K, Morozumi M, et al. Identification of pathogens by comprehensive real-time PCR versus conventional methods in community-acquired pneumonia in Japanese adults. Infect Dis (Auckl). 2016 [2016 December 01];48(11–12):782–788.
- Ryu K, Takayanagi N, Ishiguro T, et al. Etiology and outcome of diffuse acute infectious bronchiolitis in adults. Ann Am Thorac Soc. 2015;12(12):1781–1787.
- Fukuyama H, Yamashiro S, Tamaki H, et al. A prospective comparison of nursing- and healthcare-associated pneumonia (NHCAP) with community-acquired pneumonia (CAP). J Infect Chemother. 2013;19(4):719–726.
- Abe T, Tokuda Y, Ishimatsu S, et al. Usefulness of initial blood cultures in patients admitted with pneumonia from an emergency department in Japan. J Infect Chemother. 2009;15(3):180–186.
- Kobashi Y, Yoshida K, Miyashita N, et al. Evaluating the use of a Streptococcus pneumoniae urinary antigen detection kit for the management of community-acquired pneumonia in Japan. Respiration. 2007;74(4):387–393.
- Miyashita N, Fukano H, Mouri K, et al. Community-acquired pneumonia in Japan: a prospective ambulatory and hospitalized patient study. J Med Microbiol. 2005;54(Pt 4):395–400.
- Suzuki M, Dhoubhadel BG, Ishifuji T, et al. Serotype-specific effectiveness of 23-valent pneumococcal polysaccharide vaccine against pneumococcal pneumonia in adults aged 65 years or older: a multicentre, prospective, test-negative design study. Lancet Infect Dis. 2017;17(3):313–321.
- Kumagai S, Ishida T, Tachibana H, et al. Polybacterial aetiology and outcomes in patients with community-acquired pneumonia. Int J Tuberc Lung Dis. 2016;20(1):129–135.
- Ichikawa T, Otsuka S, Iwasaki M, et al. [Study of pneumonia admissions in the Department of Respiratory Medicine at our hospital in 2016 (author’s transl)] [原著論文]. J Asahikawa City Hospital. 2019 12;51(1):1–6.
- Nariai A, Yanai T, Kanetaka T. [Epidemiology of pneumococci obtained from the nasopharynx of infants and young children before and after transition to 13-valent pneumococcal conjugate vaccine: change of serotypes] [原著論文]. J Jpn Pediatr Soc. 2016. 04. 120(4):744–751.
- Ozawa D, Yano H, Endo S, et al. Impact of the seven-valent pneumococcal conjugate vaccine on acute otitis media in Japanese children: emergence of serotype 15A multidrug-resistant Streptococcus pneumoniae in middle ear fluid isolates. Pediatr Infect Dis J. 2015;34(9):e217–21.
- Chiba N, Morozumi M, Shouji M, et al. Changes in capsule and drug resistance of Pneumococci after introduction of PCV7, Japan, 2010-2013. Emerg Infect Dis. 2014;20(7):1132–1139.
- Abe T, Furuno K, Bin C, et al. [Bacteriological analysis of pneumococcus detected from the sputum of hospitalized children] [原著論文]. J Jpn Assoc Infect Dis. 2017 03;91(2):137–144.
- Kawaguchiya M, Urushibara N, Aung MS, et al. Serotype distribution, antimicrobial resistance and prevalence of pilus islets in pneumococci following the use of conjugate vaccines. J Med Microbiol. 2017;66(5):643–650.
- Kawaguchiya M, Urushibara N, Aung MS, et al. Emerging non-PCV13 serotypes of noninvasive Streptococcus pneumoniae with macrolide resistance genes in northern Japan. New Microbes New Infect. 2016;9:66–72.
- Nakano S, Fujisawa T, Ito Y, et al. Serotypes, antimicrobial susceptibility, and molecular epidemiology of invasive and non-invasive Streptococcus pneumoniae isolates in paediatric patients after the introduction of 13-valent conjugate vaccine in a nationwide surveillance study conducted in Japan in 2012-2014. Vaccine. 2016;34(1):67–76.
- Uda K, Morikawa Y, Ito K, et al. [Serotype replacement of invasive pneumococcal disease after introduction of pneumococcal conjugated vaccine at children’s hospital in Japan] [原著論文]. J Pediatric Infect Dis Immunol. 2015 04;27(1):9–15.
- Kawaguchiya M, Urushibara N, Ghosh S, et al. Serotype distribution and susceptibility to penicillin and erythromycin among noninvasive or colonization isolates of Streptococcus pneumoniae in northern Japan: a cross-sectional study in the pre-PCV7 routine immunization period. Microb Drug Resist. 2014;20(5):456–465.
- Eto M, Mizunaga S, Fukuda Y, et al. [Sensitivity surveillance of Streptococcus pneumoniae isolates for several antibacterial agents in Gifu and Aichi prefecture (2010-2011)] [原著論文]. Jpn J Antibiot. 2013 10;66(5):265–282.
- Nariai A, Uchimura T, Kanetaka T, et al. [Epidemiology of pneumococcal strains obtained from the nasopharynx of infants and young children with lower respiratory tract infection before the distribution of 7-valent conjugate vaccine in 2010] [原著論文]. J Jpn Pediatr Soc. 2013 11;117(11):1759–1766.
- Fukusumi M, Chang B, Tanabe Y, et al. Invasive pneumococcal disease among adults in Japan, April 2013 to March 2015: disease characteristics and serotype distribution. BMC Infect Dis. 2017;17(1):2.
- Maeda Y, Akiba Y, Kajiwara Y, et al. [Study of adult invasive pneumococcal disease (IPD) in our hospital (author’s transl)] [原著論文]. J Chiba Assoc Med Technol. 2019;10(137):6–10.
- Furuya Y, Yamagishi Y, Okade H, et al. Impact of the pneumococcal conjugate vaccine on serotype distribution of adult non-invasive Streptococcus pneumoniae isolates in Tokai region, Japan, 2008-2016. J Infect Chemother. 2017;23(6):394–399.
- Shoji H, Maeda M, Takuma T, et al. Serotype distribution of Streptococcus pneumoniae isolated from adult respiratory tract infections in nationwide Japanese surveillances from 2006 to 2014. J Infect Chemother. 2017;23(8):538–544.
- Hosoya M, Inomata A, Kimura Y, et al. [Serotype distribution of Streptococcus pneumoniae isolates from invasive pneumococcal disease patients in Niigata prefecture] [原著論文]. Annual Report of Niigata Prefectural Institute of Public Health and Environmental Sciences. 2015 .10;30:62–66.
- Shoji H, Maeda M, Shirakura T, et al. Changes in the distribution of capsular serotypes of streptococcus pneumoniae isolated from adult respiratory specimens in Japan [原著論文]. [日本における成人呼吸器検体から分離された肺炎球菌の莢膜血清型の分布における変化]. Intern Med. 2015 06; 54(11): 1337–1341.
- Ubukata K, Chiba N, Hanada S, et al. Serotype changes and drug resistance in invasive pneumococcal diseases in adults after vaccinations in children, Japan, 2010-2013. Emerg Infect Dis. 2015;21(11):1956–1965.
- Noguchi S, Yatera K, Akata K, et al. Distribution and annual changes in the proportion of Streptococcus pneumoniae serotypes in Japanese adults with pneumococcal pneumonia from 2011 to 2017. J Infect Chemother. 2019;25(11):925–929.
- Toda H, Tanaka Y, Satoh K, et al. Epidemiological and molecular characterization of invasive Streptococcus pneumoniae isolated following introduction of 7-valent conjugate vaccine in Kinki region, Japan, 2008-2013. J Infect Chemother. 2020;26(5):451–458.
- Nakano S, Matsumura Y, Ito Y, et al. Development and evaluation of MALDI-TOF MS-based serotyping for Streptococcus pneumoniae. Eur J Clin Microbiol Infect Dis. 2015;34(11):2191–2198.
- Hotomi M, Togawa A, Kono M, et al. PspA family distribution, antimicrobial resistance and serotype of Streptococcus pneumoniae isolated from upper respiratory tract infections in Japan. PLoS One. 2013;8(3):e58124.
- Hotomi M, Nakajima K, Hiraoka M, et al. Molecular epidemiology of nonencapsulated Streptococcus pneumoniae among Japanese children with acute otitis media. J Infect Chemother. 2016;22(2):72–77.
- Yamagishi Y, Mikamo H, Sawamura H, et al. [Epidemiological analysis of Streptococcus pneumoniae in Gifu prefecture and the northern district of Aichi prefecture −2009-] [原著論文]. Jpn J Antibiot. 2012 02;65(1):27–47.
- Suzuki H, Tokuda Y, Shichi D, et al. Morbidity and mortality among newly hospitalized patients with community-acquired pneumococcal bacteremia: a retrospective cohort study in three teaching hospitals in Japan [原著論文]. [市中肺炎球菌性菌血症の新規入院患者における合併症および死亡率 日本の教育病院3施設における後向きコホート研究]. Geriat Gerontol Int. 2013 07; 13(3): 607–615.
- Ishiwada N, Iwata S, Sakata H, et al. [Burden of illness of pneumonia caused by Streptococcus pneumoniae in chilren] [原著論文]. Jpn J Pediatr. 2008 11;61(11):2194–2204.
- Uda A, Tokimatsu I, Koike C, et al. Antibiotic de-escalation therapy in patients with community-acquired nonbacteremic pneumococcal pneumonia. Int J Clin Pharm. 2019;41(6):1611–1617.
- Shinjoh M, Iwata S, Yagihashi T, et al. Recent trends in pediatric bacterial meningitis in Japan–a country where Haemophilus influenzae type b and Streptococcus pneumoniae conjugated vaccines have just been introduced. J Infect Chemother. 2014 Aug;20(8):477–483.
- Tanaka K, Matsui T, Tachibana T, et al. Factors associated with acute otitis media in children due to penicillin intermediately resistant Streptococcus pneumoniae. Int J Pediatr Otorhinolaryngol. 2009;73(10):1344–1347.
