ABSTRACT
INTRODUCTION: COVID-19 is associated with a risk of severe pneumonia and acute respiratory distress syndrome (ARDS), requiring treatment at an intensive care unit (ICU). Since clinical deterioration may occur rapidly, a simple, fast, bedside, non-invasive method for assessment of lung changes is warranted. The primary aim of this study was to investigate whether lung ultrasound (LUS) findings within 72 hours of admission were predictive of clinical deterioration in hospitalized patients with confirmed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).
METHODS: Patients admitted to a dedicated COVID-19 unit were subject to daily LUS examinations. Number of present consolidations and pleural effusions were registered and a Mongodi score was calculated. These findings were correlated with initial chest x-ray and clinical deterioration, defined as ICU-admission, ARDS diagnosis, death.
RESULTS: In total, 29 of 83 patients had LUS performed during admission, 18 within 72 h of admission. Of these, four patients died during admission, six were transferred to the ICU and 13 were diagnosed with ARDS.
Initial Mongodi-score did not differ significantly between patients with and without clinical deterioration (p = 0.95). Agreement between initial LUS and chest x-ray findings were fair with Cohen’s Kappa at 0.21.
CONCLUSION: LUS performed within 72 h in patients admitted to a dedicated COVID-19 unit could not predict ARDS, ICU admission or death. However, consecutive investigations may be of value, as sudden substantial changes may herald disease progression, enabling earlier supplementary diagnostics and treatment initiation.
Introduction
The coronavirus disease 2019 (COVID-19) outbreak, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a Public Health Emergency of International Concern by the World Health Organization on January 30, 2020[Citation1]. The virus is highly contagious and predominantly affects the respiratory organ, causing symptoms ranging from simple cough to severe pneumonia and acute respiratory distress syndrome (ARDS), requiring intensive care treatment [Citation2].
The radiological findings of SARS-CoV-2 pneumonia are variable, but most commonly include bilateral and multilobar parenchymal involvement. The most common findings on computed tomography (CT) of the chest are diffuse bilateral ground glass opacities, septal thickening, consolidations, and pleural effusions [Citation3].
Rapid clinical deterioration from limited symptoms to acute respiratory failure with ARDS development is a known complication to COVID-19. Consequently, close monitoring of these patients, to allow early detection of ARDS-development, is essential. However, this would require repeated thoracic imaging which is time-consuming and overall challenging in a COVID-19 setting, since chest CT and non-supine chest x-ray (CXR) often require temporary intrahospital patient transportation [Citation4] and hence risk of virus transmission [Citation5].
Lung ultrasound (LUS) is a fast, cheap and mobile imaging modality ideal for frequent repeated imaging, hence being a potential ideal monitoring tool in the COVID-19 pandemic [Citation6]. Additionally, small portable and handheld ultrasound machines are easy to clean and can be used as part of the clinical assessment of the patient. LUS can clearly visualize lung lesions adjacent to the pleura and is established as a reliable tool for the diagnosis and monitoring of ARDS as well as possible complications to COVID-19 (e.g. pleural effusion, consolidations associated with potential bacterial pneumonia, and pulmonary embolism) [Citation7,Citation8].
Furthermore, as LUS is able to detect dynamic changes in the lung parenchyma and pleura, which can be observed in relation to pulmonary oedema, ARDS or lung lavage, LUS should be considered a valued tool to detect and monitor rapid changes in relation to patients with COVID-19 [Citation9–11]. From a clinical perspective, this approach is highly relevant in dedicated COVID-19 wards where admitted patients are at risk of sudden clinical deterioration.
The primary aim of this study was to investigate whether LUS findings within 72 hours of admission were predictive of clinical deterioration in hospitalized patients with confirmed COVID-19. Secondary aims were the correlation between LUS and CXR findings, and whether serial LUS can predict ARDS-development.
Materials and methods
Design and setting
The study was conducted as a single-center prospective cohort study at Odense University Hospital (OUH), Denmark. The hospital serves as a community-hospital for approximately 0.25 million inhabitants and as a tertiary hospital for the the Region of Southern Denmark (approximately 1.2 million inhabitants) [Citation12]. In the beginning of the epidemic, all medically stable patients with COVID-19 in the Region of Southern Denmark were transferred to a dedicated COVID-19 unit at OUH for further therapy[Citation13].
Population
We included all patients who were 1) 18 years or older, 2) had a positive real time polymerase chain reaction (RT-PCR) analysis for SARS-CoV-2 performed on material from a pharyngeal swab or tracheal secretion, 3) were admitted or transferred to the COVID-19 unit at OUH between the 10th of March to 31st of May 2020 and 4) had LUS performed at least once during admission.
LUS
The LUS examination was performed using a 14-zone scanning protocol, previously validated for assessing patients with acute respiratory failure in an emergency department setting [Citation14,Citation15]. The protocol was supplemented with a LUS scoring system (Mongodi) based on a model previously validated for assessing patients with ARDS and severe pneumonia [Citation16]. The Mongodi score is based on LUS performed in the four anterior and four lateral zones, making it optimal for a COVID-19 setting, where patients are often restrained to a supine position. In each zone, between 1 and 4 points are given based on LUS-findings, resulting in a final score between 8 and 32 points (). Each point was defined according to the following:
1 point:<3 B-lines
2 points:≥3 B-lines occupying ≤50% of the pleural line
3 points: ≥3 B-lines occupying >50% of the pleural line
4 points: Lung consolidation present
Figure 1. LUS findings in COVID-19 and corresponding score.A: the pleuraline (PL) appears normal. No B-lines or consolidation is present corresponding to a score of 1.B: multiple B-lines (B) origninating from the pleural line (PL). The B-lines involve less than 50% of the pleuraline, corresponding to a score of 2.C: multiple confluent B-lines (CB) are present. More than 50% of the pleural line are involved corresponding to a score of 3.D: A small subpleural consolidation (C) is present just below the pleural line, corresponding to a score of 4
For the duration of admittance to the COVID-19 unit, LUS examination was performed on a daily basis presupposing availability of a physician skilled in LUS. The results of the LUS examinations were prospectively registered using a standardised reporting form. Portable, handheld ultrasound machines were used for the LUS examinations (SonoSite iViz machine with a high frequency linear transducer, GEV scan with dual probe).
Other imaging
CXR was performed routinely upon admission to the hospital and described by the attending radiologist who did not have access to the result of any LUS findings. If clinical deterioration with progressive respiratory failure was observed, patients were referred for high-resolution computed tomography (HRCT) or CT pulmonary angiography depending on primary presumptive diagnosis (e.g. ARDS and pulmonary embolism).
Standard of care at the COVID-19 unit
The COVID-19 management at the dedicated unit was based on local and national guidelines and consisted primarily of supportive therapy and use of dexamethasone for ARDS [Citation13]. Upon admission, each patient was evaluated by a senior consultant and an intensive care specialist to determine whether the patient was a candidate for intensive care unit (ICU) treatment based on a combination of age, comorbidities, and the patient’s own consideration along with potential for future rehabilitation. Based on this evaluation, patients who developed severe respiratory failure or multi-organ failure during admission were either transferred to the ICU or treated at the COVID-19 unit [Citation13].
Data collection
A review of the patients’ medical record was performed to obtain data on demography, comorbidities, as well as clinical and outcome data. All data were registered in a REDCap database by one investigator and subsequently validated by a second member of the study team. In case of discrepancy, a consensus was reached through discussion among team members. A complete codebook was predefined for all variables [Citation13].
Outcome definitions
Clinical deterioration was defined as death, admission to ICU or ARDS as defined by the Berlin criteria [Citation17].
Statistics
All statistical analyses were performed in GraphPad Prism 9.0.0.
For continuous numerical variables, Shapiro-Wilks test was used to assess normality.
Normally distributed data were presented as mean with standard deviation (SD). Non-normally distributed data were presented as medians with interquartile ranges (IQR). To identify whether LUS could predict clinical deterioration, we compared the median initial Mongodi score within 72 hours of admission between patients with or without clinical deterioration using the Mann-Whitney test. Mean or median Mongodi score and number of consolidations and effusion detected by LUS during admission was compared using a Mann–Whitney test or an unpaired t test. We also estimated the median maximum Mongodi score as well as the median time after admission to reach this score. To estimate the level of agreement between the radiologist CXR interpretation and the LUS findings, we used Cohen’s Kappa coefficient (Cκ).
Ethics
The study was approved as a quality study and registered on the Region of Southern Denmark’s record of data processing activities (journal number 20/16,169). Data were handled in accordance with the General Data Protection Regulation, the Danish Act on Data Protection, the Danish Act on Research Ethics Review of Health Research Projects and the Danish Health Act.
Results
Population
During the study period, 83 patients were admitted to the COVID-19 unit. Of these, a total of 29 patients were subject to at least one LUS investigation and were included in the study. Mean age was 63 years (± 17.3) with a male predominance (65.5%). Four patients (13.8%) died during admission. Six patients (20.7%) were admitted to the ICU and 13 patients (44.8%) were diagnosed with ARDS. An overview of the study population is presented in [].[])
Table 1. Baseline characteristics of patient population. BMI = Body mass index
LUS findings
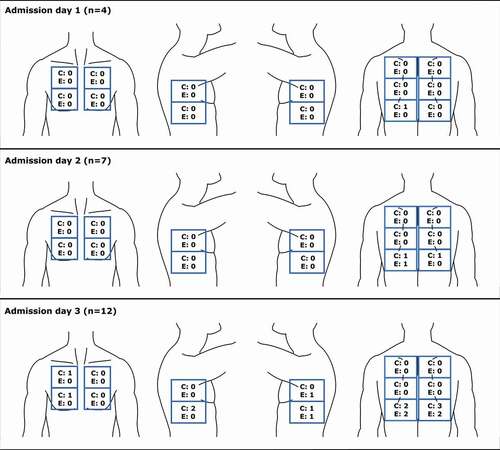
Eighteen patients (62.1%) had LUS performed within 72 h of admission. Number of visible consolidations and effusions on days 1–3 as well as the Mongodi score is presented in []. The initial Mongodi score did not differ significantly between the eight patients who developed the predefined outcome and the 10 patients who did not[Mongodi score: 11.5 (IQR: 8.0–16.8) and 11.3 ± 4.2, respectively (p = 0.95)]. The number of consolidations were significantly higher at day 3 than day 1 and 2 (p = 0.03 for both). There was no significant difference in the number of detected pleural effusions or Mongodi score on day 3 of admission compared to day 1 and 2 (pleural effusions p = 0.16 for both, Mongodi score, p = 0.15 for day 1, p = 0.18 for day 2).
Longitudinal Mongodi scores during the entire hospital stay
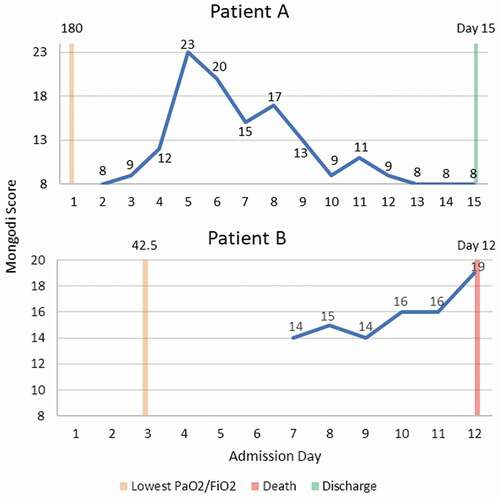
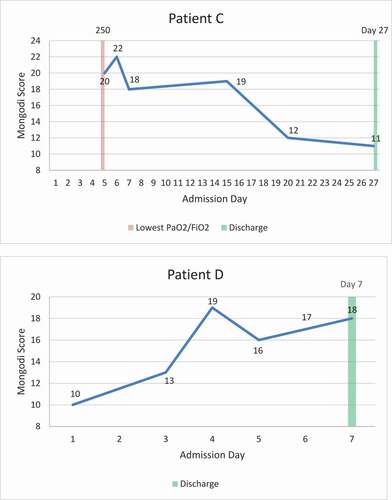
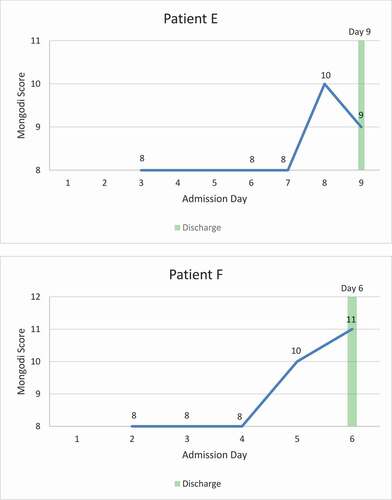
For the 29 included patients, the median number of registered Mongodi scores was 2 (IQR 1.0–3.0). The mean maximal Mongodi score for these 29 patients of 14.5 ± 6.0 was registered at median day 5.0 (IQR 2.5–8.0). This score did not differ significantly from median initial score of 10 (IQR 8–16.25) in the 18 patients who had LUS performed within 72 hours of admission (p = 0.16) or mean score of 9.5 ± 1.91 for the four patients who had LUS performed at day 1 of admission (p = 0.11). When comparing mean score at day 1 of admission with mean score of 14.6 ± 5.0 for the nine patients who had LUS performed at day 5, no significant difference was observed (p = 0.08). Six patients had five or more LUS performed during their admission. Longitudinal data including time points for ARDS diagnosis with lowest partial PaO2/FiO2, transferral to ICU and death or discharge is presented in [] and [APPENDIX].
CXR and LUS agreement
For the 18 patients who were investigated by LUS within 72 h of admission the agreement between CXR diagnosis of lung opacities and LUS with present consolidation was fair (Cκ 0.21) with an agreement of 58.8%. Agreement between CXR and LUS diagnosis of pleural effusion was calculated for 17 patients and was fair (Cκ 0.21) with an agreement of 76.5%. In ten patients, CXR findings compatible with pulmonary oedema and LUS with the presence of interstitial syndrome were compared, reaching a 90%’s agreement. Cohen’s Kappa could not be computed, as there were no cases presenting with both findings. The mean time between initial CXR and first LUS was 2.2 days ±0.8.
Discussion
The aim of this study was to clinically appraise the utility of initial (<72 h) and repeated LUS for predicting ARDS, transfer to ICU or death in COVID-19 patients, and to assess whether these findings correlated with findings on CXR.
Although we found no significant increase in pleural effusion or Mongodi score during the first 72 hours of admission, a significant increase in the number of lung consolidations was observed, which likely indicates progressive lung involvement as part of a pre-state to or manifest ARDS. While no significant increase in Mongodi score was observed within 72 hours, the median and mean score increased slightly, suggesting an increase in the extent of lung parenchymal involvement. Indeed, the maximal score was observed at median day 5 after admission. Thus, an initial scan following transfer to a COVID-19 unit seems to have limited prognostic value. However, an important aspect to consider is that LUS was performed at the COVID-19 unit following admission through an emergency department system. Included patients were therefore a selected population of COVID-19 patients in which admission was already deemed necessary based on clinical assessment and the results of other diagnostic tests (e.g. blood samples, CXR). As indicated by other studies, LUS may still have a potential diagnostic and prognostic role when used as an upfront imaging modality in an emergency department. This is exemplified by a recent study by Perrone et al. investigating if a single LUS examination on the day of admission was predictive of need for high-flow oxygen support, ICU admission and death within 30 days in 52 COVID-19 patients [Citation18,Citation19]. Their findings showed higher LUS scores were associated with clinical worsening during admission.
While the initial LUS findings in this study seem to be of limited prognostic value, our results suggest a possible role when used as part of a daily monitoring system. A rapid substantial increase in consecutive Mongodi scores may aid in decision making, exemplified by patient A in [] whose score increased from 12 to 23 between admission day four and five with no obvious concomitant clinical deterioration or change in oxygen saturation level. This increase led to a CT referral revealing a generalized lung involvement compatible with ARDS requiring anti-inflammatory treatment with dexamethasone. Indeed, daily LUS by the treating physician has recently been shown to be a reliable tool in predicting both abnormal CT chest scans and the need for oxygen requirements in patients with COVID-19 [Citation20].
We chose to use the Mongodi scoring system since it had been validated for monitoring development of ARDS and the findings could potentially be generalised to a COVID-19 population. Apart from being previously validated, the scoring system also has a low interrater variance, is simple to use and feasible for non-LUS experts. Additionally, as severely ill COVID-19 patients may be confined to a supine position challenging LUS investigation of the posterior zones, the Mongodi score is calculated solely based on findings in the anterior and lateral zones. In this study, we could scan the posterior zones in 15 out of 18 patients (83%) and found that the majority of consolidations and pleural effusions were observed in the basal posterior zones (R5 and L5 in []), implying that important findings are often missed. Thus, a separate scoring protocol for COVID-19 patients not restrained to a supine position is warranted. These findings are supported by other studies in which scoring systems use all 14 zones, thus, including posterior zones seems to be superior to a protocol limited to the anterior and lateral surface of the chest [Citation18,Citation19]. As highlighted by the recently published international expert consensus recommendation for multi-organ point-of-care ultrasound for COVID-19, LUS has a role as a monitoring tool in moderate-severe COVID-19, but still has limitations and further studies are still needed to establish the optimal protocol and clinical use [Citation21].
CXR
CXR is routinely used as the first line imaging option in patients presenting with respiratory symptoms. For COVID-19 patients, a portable CXR device is often used to decrease intra-hospital transport and risk of transmission, and only allows supine images leading to reduced interpretability. In our study, there was a fair agreement between CXR and LUS findings of pleural effusion and lung consolidations. However, for the latter, the inter-rater agreement was substantially lower at 58.8%. As parenchymal involvement in COVID-19 does not always involve the subpleural lung parenchyma in mild to moderate cases of the disease, parenchymal lung involvement can be present even though LUS findings are normal. This is also reflected by a study by Lu et al. in which the sensitivity of LUS to detect lung parenchymal involvement in COVID-19 was 68.8% and 77.8% when compared to chest CT in mild and moderate cases, respectively [Citation22]. Chest HRCT is considered the golden standard to detect lung involvement in COVID-19 and alternatives as CXR and LUS have clear diagnostic limitations. To what extent a composite measure involving CXR and LUS can improve the overall diagnostic accuracy when compared to chest CT remains to be determined.
Limitations
The major limitations were the single-center study set-up and the small sample size. Furthermore, as not all attending physicians in the beginning of the inclusion period had the required skill for performing LUS, it was only performed in a proportion of the COVID-19 patients admitted to the dedicated COVID-19 unit at our hospital. LUS was thus initially performed if the attending physician could perform the examination, even though the selection of attending physician for each specific admitted patient was not based on LUS qualifications, selection bias may have indirectly been introduced. As such, the results may affect the generalizability of our findings. Additionally, the physicians performing LUS were not limited to experts within the field, but also included physicians with LUS skills at a point-of-care level from a wide range of different specialities, leading to potential detection bias as consequence of different degree of LUS experience. Nevertheless, these findings represent the everyday clinical setup in a COVID-19 unit, manned by physicians able to perform LUS at a point-of-care level in a focused manner. The viability of LUS as a continuous monitoring tool needs to be validated in larger cohorts.
Conclusion
LUS is widely accessible and may be a valuable tool in continuous monitoring of patients admitted with COVID-19. Our findings suggest that initial LUS at admission to a dedicated COVID-19 unit is unlikely to predict ARDS, ICU admission or death, or replace a CXR within 72 hours. However, a rapid increase in Mongodi LUS scores may indicate lung parenchymal and pleural disease progression warranting initiation of supplementary diagnostics and treatment.
Data availability statement
Data can be requested from the corresponding author. The study guarantors (CF, NJ and CBL) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported and that no important aspects of the study have been omitted.
Disclosure statement
The author(s) report no conflict of interest.
Additional information
Funding
Notes on contributors
Casper Falster
Casper Falster MD is a PhD student at Odense Respiratory Research Unit (ODIN) at Odense University Hospital. He is co-founder of the influential scientific society Danish Innovative Collaboration on Knowledge of Pulmonary Interstitial and Cancerous Studies.
Niels Jacobsen
Niels Jacobsen MD is a PhD student at Odense Respiratory Research Unit (ODIN) at Odense University Hospital. He is co-founder of the influential scientific society Danish Innovative Collaboration on Knowledge of Pulmonary Interstitial and Cancerous Studies.
Lone Wulff Madsen
Lone Wulff Madsen MD is an infectious disease specialist and PhD student at the Department of Infectious Diseases, Odense University Hospital and at the Research Unit for Infectious Diseases, University of Southern Denmark, Odense, Denmark.
Line Dahlerup Rasmussen
Line Dahlerup Rasmussen MD, PhD, DMSc, is an associate professor at Faculty of Health Sciences at University of Southern Denmark. She is senior registrar at the Department of Infectious Diseases, Odense University Hospital, Odense Denmark.
Jesper Rømhild Davidsen
Jesper Rømhild Davidsen MD, PhD is an associate professor at Odense Respiratory Research Unit (ODIN), Department of Clinical Research, University of Southern Denmark, Odense, Denmark. He is further Head of South Danish Center for Interstitial Lung Diseases (SCILS) and Specialty Chief Consultant at Department of Respiratory Medicine, Odense University Hospital, Odense, Denmark.
Fredrikke Christie Knudtzen
Fredrikke Christie Knudtzen MD, DTM&H, is a PhD-student at the Clinical Center for Emerging and Vector-borne Infections, Department of Infectious Diseases, Odense University Hospital, Denmark.
Stig Lønberg Nielsen
Stig Lønberg Nielsen MD, PhD is a senior registrar at the Department of Infectious Diseases and a researcher at the Research Unit of Infectious Diseases, Clinical Institute, University of Southern Denmark.
Isik Somuncu Johansen
Isik Somuncu Johansen MD, DMSc., is a professor and head of research at the Department of Infectious Diseases, Odense University Hospital and University of Southern Denmark.
Christian B. Laursen
Christian Laursen MD, PhD, Prof, is consultant at the Department of Respiratory Medicine, Odense University Hospital. He is head of research at Odense Respiratory Research Unit (ODIN), Department of Clinical Research, University of Southern Denmark.
References
- Statement on the second meeting of the International Health Regulations (2005) Emergency committee regarding the outbreak of novel coronavirus (2019-nCoV). https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (cited 2020 Nov 26).
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–12.
- Lai CC, Shih TP, Ko WC, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062.
- Knight PH, Maheshwari N, Hussain J, et al. Complications during intrahospital transport of critically ill patients: focus on risk identification and prevention. Int J Crit Illn Inj Sci. 2015;5(4):256–264.
- Lichtenstein DA. BLUE-Protocol and FALLS-Protocol: two applications of lung ultrasound in the critically ill. Chest. 2015;147(6):1659–1670.
- Bai C, Chotirmall SH, Rello J, et al. Updated guidance on the management of COVID-19: from an american thoracic society/european respiratory society coordinated international task force (29 July 2020). Eur Respir Rev. 2020;29(157):1–15.
- Zhou Y, Fan Q, Cavus O, et al. Lung ultrasound: predictor of acute respiratory distress syndrome in intensive care unit patients. Saudi J Anaesth. 2018;12(3):457–461.
- Arbelot C, Ferrari F, Bouhemad B, et al. Lung ultrasound in acute respiratory distress syndrome and acute lung injury. Curr Opin Crit Care. 2008;14(1):70–74.
- Via G, Lichtenstein D, Mojoli F, et al. Whole lung lavage: a unique model for ultrasound assessment of lung aeration changes. Intensive Care Med. 2010;36(6):999–1007.
- Frasure SE, Matilsky DK, Siadecki SD, et al. Impact of patient positioning on lung ultrasound findings in acute heart failure. Eur Hear J Acute Cardiovasc Care. 2015;4(4):326–332.
- Folketal. Danmarks statistik. https://www.dst.dk/da/Statistik/emner/befolkning-og-valg/befolkning-og-befolkningsfremskrivning/folketal (cited 2020 Nov 28).
- Madsen LW, Lindvig SO, Rasmussen LD, et al. Low mortality of hospitalised patients with COVID-19 in a tertiary Danish hospital setting. Int J Infect Dis. 2021;102:212–219.
- Laursen CB, Sloth E, Lassen AT, et al. Point-of-care ultrasonography in patients admitted with respiratory symptoms: a single-blind, randomised controlled trial. Lancet Respir Med. 2014;2(8):638–646.
- Laursen CB, Sloth E, Lambrechtsen J, et al. Focused sonography of the heart, lungs, and deep veins identifies missed life-threatening conditions in admitted patients with acute respiratory symptoms. Chest. 2013;144(6):1868–1875.
- Mongodi S, Bouhemad B, Orlando A, et al. Modified lung ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med. 2017;38(5):530–537.
- Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. J Am Med Assoc. 2012;307:2526–2533.
- Perrone T, Soldati G, Padovini L, et al. A new lung ultrasound protocol able to predict worsening in patients affected by severe acute respiratory syndrome Coronavirus 2 pneumonia. J Ultrasound Med. 2020 Nov 6. published online. DOI:https://doi.org/10.1002/jum.15548.
- Soldati G, Smargiassi A, Inchingolo R, et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19. J Ultrasound Med. 2020;39(7):1413–1419.
- Falgarone G, Pamoukdjian F, Cailhol J, et al. Lung ultrasound is a reliable diagnostic technique to predict abnormal CT chest scan and to detect oxygen requirements in COVID-19 pneumonia. Aging (Albany NY). 2020;12(20):19945–19953.
- Hussain A, Via G, Melniker L, et al. Multi-organ point-of-care ultrasound for COVID-19 (PoCUS4COVID): international expert consensus. Crit Care. 2020;24(1):702.
- Lu W, Zhang S, Chen B, et al. A clinical study of noninvasive assessment of lung lesions in patients with coronavirus disease-19 (COVID-19) by bedside ultrasound. Ultraschall Med. 2020;41(3):300–307.
Appendix A1
Overview of consolidations, effusions, and Mongodi score through day one to three of admission by zone
Appendix A2
Longitudinal Mongodi scores in patients with five or more LUS performed during admission