ABSTRACT
Background
The coronavirus infection (COVID-19) pandemic has seen a progressive increase in childhood morbidity worldwide. Continuous mutation of the SARS-CoV-2 virus causes the wave-like course of the COVID-19 pandemic, which is characterized by an undulating course and the predominance of different variants of the SARS-CoV-2 virus. There are many reports that the clinical picture may vary depending on the circulating strain of the virus [7–11, 13–16]. Based on this, we decided to analyze and evaluate the presence of a pattern between the clinical and epidemic COVID-19 characteristics and the strain of the SARS-CoV-2 virus prevailing locally.
The aim of the work
To study the effects of various strains of SARS-CoV-2 on the clinical and epidemiological characteristics of pediatric patients; to determine the regularity between the severity of the disease and the circulating strain of SARS-CoV-2.
Materials and methods
A retrospective analysis of 945 case stories of COVID-19 disease in children who were hospitalized at the infectious diseases hospital (Kyiv, Ukraine) in the period from June 2020 to February 2022 (corresponding to a period of four waves of different SARS-CoV-2 strains). We investigated epidemiological and clinical features, as well as laboratory and instrumental parameters, comparing four waves of the disease.
Results and Conclusions
A regularity between the wave of COVID-19 and the severity of the disease was found. The third wave seemed to be the most severe, due to the increase in the frequency of complications, concomitant pathology, clinical symptoms and the level of mortality. The timing of this outbreak matched with the circulation of the SARS-CoV-2 delta-variant and correlated with an increase in hospitalization rates in Ukraine.
Introduction
More than two years have passed since the beginning of COVID-19, and the first case of COVID-19 in Ukraine was recorded from the beginning of March 2020. By April 2022 there were 5 million PCR-confirmed cases in Ukraine, of which more than 112,000 were fatal [Citation1]. The total number of cases worldwide reached more than 509 million, of which 6.22 million were fatal [Citation2]. According to UNICEF, among the deaths from COVID-19, 0.4% were children and adolescents under the age of 20. Among them, 58% were teenagers aged 10–19 years and 42% were children aged 0–9 years [Citation3]. The American Academy of Pediatrics reported about 13 million cases of COVID-19 in children, which is 19% of all cases in the USA. The total rate was 17,000 cases per 100,000 of the child population [Citation4]. According to the Ministry of Health of Ukraine, the morbidity rate of children at the beginning of February reached 6.2%.
For easy identification of COVID-19 variants, the WHO expert group suggested marking them with Greek letters – alpha, beta, gamma, delta, epsilon, zeta, eta, theta, iota, kappa, lambda, mu and omicron [Citation5].
The quick appearance of new variants of the SARS-COV-2 virus necessitated the differentiation of particularly dangerous strains and the introduction of such concepts as Variants of Concern (VOCs), which included delta and omicron [Citation6].
The epidemiological chronology of COVID-19 began with the ‘Wild’ L strain, which was identified in Wuhan, China, Hubei Province in December 2019, and was gradually replaced by other variants of the virus. In the first published studies, the clinical picture was characterized by general respiratory symptoms in 65% of patients, in 26% by mild disease, and in 9% by asymptomatic course. Severe or critical cases were not identified. The most common symptoms were fever (73.7%), cough (73.7%), shortness of breath (86.7%), and nausea and vomiting (40.0%) [Citation7–10].
The next global outbreak was caused by the alpha variant (B.1.1.7) – known as the British variant, which spread to 182 countries. Over a million confirmed cases have been registered. The presence of clinical symptoms was observed in confirmed cases of the alpha strain in children in 54.2%. These symptoms were characterized by fever, cough and rhinitis (according to the study conducted by German scientists). Among all cases, 71.2% were children from birth to 12 years old. There was no significant difference in the clinical picture between the alpha variant and the ‘Wild’ strain [Citation9,Citation11].
The beta and gamma variants spread with the next wave. The beta variant (B.1.351), first discovered in South Africa, has spread to 121 countries. The Brazilian version of gamma variant (P.1) spread to 108 countries. By September 2021, there were more than 22 million cases of COVID-19 recorded and more than 600,000 deaths in Brazil. A new variant of the P.1 virus was identified, based on genomic sequencing of samples from patients with COVID-19 in Manaus, Brazil, in January 2021. In children, the share of hypoxemia was higher (52.5% vs. 41.1%), as well as the frequency of hospitalization in the intensive care unit (28.3% vs. 24.9%) [Citation9].
The next variant was delta (B.1.617.2), which was characterized by a more severe course, a higher frequency of complications and deaths. The delta variant was registered in 178 countries and more than 3 million cases have been reported. According to the US Centers for Disease Control and Prevention (CDC) and published research (Sheng JF, et.al., 2021) [Citation10], this strain was more contagious than previous variants. In addition, the CDC reported a significant increase in the morbidity among children and an increase in the number of complicated cases [Citation12].
Since January 2022, a new disease outbreak has been registered in Ukraine, mostly caused by the omicron strain (B.1.1.529). This variant was first registered by the end of November 2021 in South Africa and spread to 170 countries. High infectivity, resistance to acquired immunity, and increased disease morbidity in vaccinated individuals contributed to the rapid spread of a worldwide disease burden within a few weeks [Citation13]. Omicron is also characterized by a shorter incubation period and shorter period of less severe clinical symptoms similar to previous outbreaks [Citation14,Citation15]. The reproduction number of omicron copies was approximately 3 times higher than that of the delta variant [Citation16], however the replication process was primarily located in the bronchi and not the lung tissue, which was the case for the delta variant [Citation14,Citation17,Citation18].
Based on numerous local reports, showing patterns of COVID-19 disease correlating to timing of various SARS-CoV-2 strain predominance, we decided to study these trends in children in Ukraine and analyze how the clinical picture changed in hospitalized patients during the different waves of the pandemic.
The purpose of the study was to investigate the effect of various predominant strains of SARS-CoV-2 on the clinical and epidemiological characteristics of pediatric patients with COVID-19; to determine a regularity between the severity of the disease and the circulating strain.
Materials and methods
We conducted a retrospective analysis of 945 case stories of children who were hospitalized to the Kyiv City Children’s Clinical Infectious Diseases Hospital (KCCCIDH) (Kyiv, Ukraine) with COVID-19 in the period from June 2020 to February 2022.
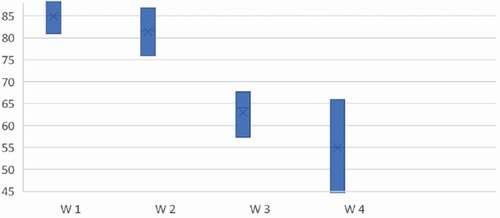
All patients were stratified by age () and periods of the COVID-19 pandemic () corresponding to the waves of the different SARS-CoV-2 strains to compare the characteristics of the clinical course, laboratory and epidemiological indicators.
Figure 1. The structure of the research: (1) – The age distribution of patients; (2) – The research timeline.
The analysis of the main clinical and laboratory indicators, data on anamnesis, results of objective and instrumental examination, methods of treatment was performed. A retrospective routine medical information analysis did not involve obtaining informed consent from patients. The bioethical commission of KCCCIDH approved the study.
Statistical analysis
To compare the most significant laboratory and instrumental indicators during all waves of morbidity, we used the biostatistical package Statistical software EZR v. 1.54 and carried out point, interval estimation of the distribution, multiple comparisons and used the D’Agostino-Pearson, Dunn, chi-square, Kruskal-Wallis and analysis of conjugation tables. As outcome variables, we used the notation W1 for the 1st wave, W2 – for the 2nd, W3 – for the 3rd, and W4 – for the 4th wave period. We also evaluated the level of leukocytes, procalcitonin, D-dimer, CRP and the frequency of abnormal radiological findings. The interquartile range (IQR, 1st – 3rd quartile) and median (M) were also determined in the study. The significance of the difference between nonparametric indicators was determined using the Chi-square test or Fisher’s exact test.
Results
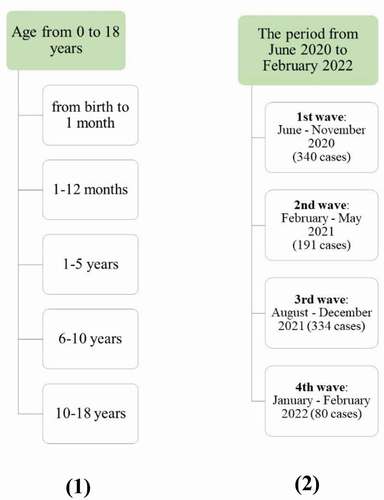
The distribution of patients with COVID-19 by age during the 4 waves ().
Figure 2. The distribution of patients admitted with COVID-19 divided by age groups during the 4 waves.
Compared with previous waves, the share of children aged 1–5 increased significantly – 44% during the 3rd wave against 26.2%, 41% and 27,5% of cases in previous waves, and the percentage of teenagers decreased (p = 0,00012). During the 4th wave, patients aged 1–12 months prevailed, accounting for 50% cases. Compared to the previous waves, the frequency of patients aged from 1 to 12 months increased (50% during the 4th wave against 25%; 21,6% and 21,8% of previous waves), p < 0,00001. No significant changes were found in the gender structure, though there was a slight predominance of boys over girls (p = 0,12).
Analyzing the results of epidemiological research, we found a gradual increase in the frequency of infection within children’s groups during the 4th wave, which was 8.7% of cases, compared to 7.3%, 5.3% and 1.0% of cases in previous outbreaks (p = 0.004). Number of illness days at the moment of hospitalization (median 2; IQR 1–3) and the number of bed-days (median 4; IQR 2–6) during the 4th wave decreased compared to previous outbreaks (p < 0.001). The detailed structure of the characteristics is shown in .
Table 1. The main characteristics of patients during the waves of COVID-19.
The highest frequency of concomitant disease was observed during the 3rd wave (16.3% vs. 5%; 14.7% vs. 8.8% of other outbreaks), p < 0.001. It was characterized by increasing number of neurological, oncological, and hematological diseases well as a prior affection of cardiovascular system, congenital malformations, prematurity and jaundice in newborns. There were also 13 cases of concomitant infectious diseases such as infectious mononucleosis, chickenpox, influenza and malaria (p = 0,003). Comparative characteristics of clinical symptoms during the waves of COVID-19 are shown in .
Table 2. Symptom characteristics of clinical symptoms during the waves of COVID-19.
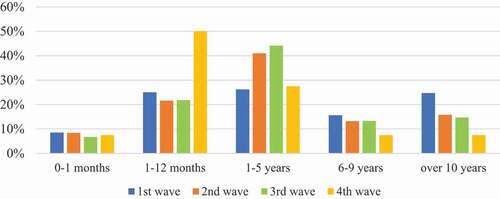
We observed a progressive increase of general intoxication symptoms during all the waves (): fever (100% during the 3rd and 4th waves against 91.2% and 97.9% of previous outbreaks (p < 0.001)); general weakness (98.8% during the 4th wave against 88.2%, 97.3% and 98.0% during the previous waves (p < 0.001)); decreased appetite (98.8% during the 4th wave against 73.8%, 97.3% and 98, 5% (p < 0.001)). The same was the case for symptoms of damage to the upper respiratory tract: rhinitis (79.0% and 78.8% during the 3rd and 4th waves against 40.9% and 73.2% of the previous waves (p < 0.001)) and cough (81.6% and 80.0% during the 3rd and 4th wave against 64.4% and 54.7% of previous outbreaks (p < 0.001)). An interval analysis of the changes is shown in .
Figure 3. Interval analysis of the frequency of clinical symptoms in children during the 4 waves: (1) – fever; (2) – weakness; (3) – decreased appetite; (4) – rhinitis; (5) – diarrhea; (6) – stomach ache; (7) – headache; (8) – cough; (9) – shortness of breath; (10) – sore throat.
The interval analysis of the frequency of symptoms such as fever (), weakness (), decreased appetite () and rhinitis () showed a statistically significant difference between the groups: W1-W2; W1-W3; and W1-W4. During the 1st wave, a significantly lower frequency of these symptoms was observed, compared to the following waves, p < 0.001.
Through the analyzed waves we observed an increase in the frequency of diarrhea, p = 0.013 () and stomach ache, p = 0.088. ().
The highest frequency of headache () was observed during the 2nd (16.8%) and 3rd (16.0%) waves. A statistically significant difference was found between the groups: W1-W2, p = 0.003 and W1-W3, p < 0.001.
Due to the interval analysis of cough frequency (), a statistically significant decrease was observed during W2 (54.7%) compared to W3 and W4, p < 0.001. During the 3rd wave there was an increase in the frequency of shortness of breath (), p=0.090, and sore throat (), p=0.027 compared to the other waves.
The 3rd wave of the disease prevailed (p < 0.001)) in terms of the number of complicated cases (). During the 3rd wave, we observed 75 (23.7%) complicated cases, against 4 (2.06%), 17 (9.9%) and 7 (11.3%) during the other waves. The majority of complicated cases was observed in children with existing medical conditions – obesity, congenital malformations, oncological diseases, cerebral palsy, Down’s syndrome and meningococcemia.
Table 3. Characteristics of complicated cases of COVID-19.
During the 2nd and 3rd waves, 4 deaths were registered – an 8-year-old child and three newborns. All these cases were accompanied by bilateral pneumonia, septic shock, acute respiratory distress syndrome, multiple organ failure syndrome, and cerebral edema. Two cases of spontaneous pneumothorax were also registered.
During all 4 waves of COVID-19, most of patients underwent general clinical, biochemical tests (alanine transaminase (ALAT), aspartate transaminase (ASAT), bilirubin), coagulation tests (International Normalized Ratio (INR), inflammation marker studies (C-reactive protein (CRP), procalcitonin), fibrinolysis marker (D-dimer) and X-ray examination of the thoracic cavity.
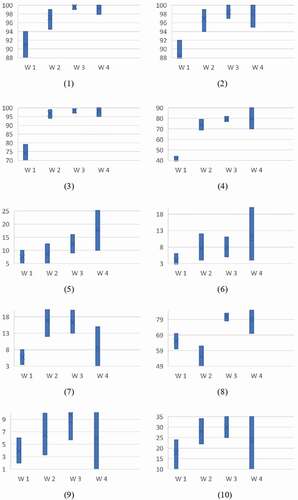
An increase in leukocytes level (>10*109/l) was observed in 12 (15.0%) patients of the 4th wave against 32.0%, 25.0% and 43.0% of the previous waves (). Correspondingly, we found a significant decrease in the average number of leukocytes () during the 4th wave (6.9*109/l (5.6–9.5) vs. 8.3*109/l (6–11.9), 7.7*109/l (5.5–10.3) and 8.9*109/l (5–12) during previous waves), p = 0.001 by interval analysis, and similarly we found a lower fraction of children with elevated CRP (> 6 mg/l) in W4; 55 patients (68.8%) vs. 76.0%, and 87.8% and 86.0% of the investigated cases during the previous waves corresponding to a lower CRP level () during the 2nd and 4th waves;30.4% (95%CI 24.1–37.1) for the 2nd wave and 35.0% (95%CI 24.8–45.9) for the 4th wave, compared to 38.2% (95%CI 33.1–43.5) and 39.8% (95%CI 34.6–45.1) for the 1st and 3rd respectively, p = 0.164. The fraction of children with an increased rate erythrocyte sedimentation rate (>10 mm/h) during the 4th wave was also lower comparing to the 3rd wave; 6 patients (7.5%) versus 67 patients (20.2%).
Table 4. Laboratory parameters.
Figure 4. Interval estimation of the average values of parameters during the waves: (1) – leukocytes; (2) – СRP; (3) – procalcitonin; (4) – D-dimer.
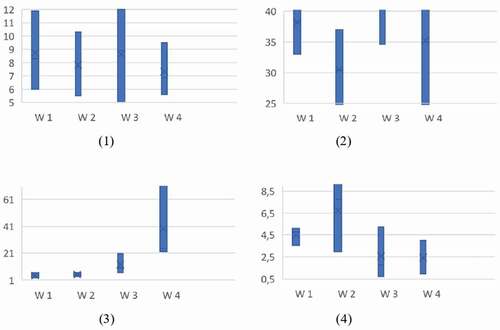
In contrast, Procalcitonin levels was highest during the 4th wave (0.242 ng/ml (0.22–0.721) vs. 0.041 ng/ml (0.027–0.064), 0.053 ng/ml (0.036–0.067) and 0.1 ng/ml (0.066–0.206)) comparing to previous waves, p < 0.001 () and correspondingly, there was a significantly higher fraction of children with elevated procalcitonin during the 4th wave (median 0.242; IQR 0.22–0.721) compared with the 3rd (median 0.1; IQR 0.066–0.206), 2nd (median 0.053; IQR 0.036–0.067) and 1st (median 0.041; IQR 0.027–0.064) waves and an increased fraction of the children had elevated platelet levels (>420*109/l) during W4; 6 cases (7.5%) compared to 8.2%, 16.3% and 7.9% during previous waves. We also found an increase in the fraction of children with elevated D-dimer (N < 0.5 mg/l) during the 4th wave (median 2.32; IQR 0.96–4) compared to during the 3rd wave (median 1.76; IQR 0.74–5.25), however, the level was lower during the first two waves (median 7.75; IQR 2.95–9.6 for the 2nd wave and median 4.77; IQR 3.55–5.13 for the 1st wave), but median D-dimer was highest during the 2nd wave; median 7.75 ng/ml and IQR 2.95–9.6, against the 1st, 3rd and 4th, p = 0.001 ().
X-Ray changes were found during W1 in 289 (85.0%) patients, W2 in 156 (81.7%), W3 in 209 (64.0%) and W4 in 44 (55.0%) (). The changes were interstitial lesions, peribronchial infiltration and lobular infiltrations. Interstitial changes were present during W1 in 81% of cases, W2 in 80.0%, W3 in 83.0% and during W4 in 80.0%. Peribronchial infiltration was found during W1 in 15% of cases, W2 in 18%, W3 in 13% and during W4 15%, lobular infiltrations in 4.0%, 2.0%, 4.0% and 5.0% of patients respectively.
Table 5. Interval analysis of the frequency of X-Ray changes during the four waves.
We found a tendency of decreasing of the frequency of parenchymal changes in radiography (), and an increase in the frequency of an uncomplicated course with a predominance of upper respiratory tract symptoms, p < 0.001.
Discussion
This research was conducted in KCCCIDH – a specialized children’s infectious disease hospital, which became a specialized hospital for children with COVID-19 in the capital city of Ukraine from the first days of the pandemic. Therefore, this work reports s characteristics of COVID-19 during various waves among the population of children in the largest city in Ukraine.
According to the results of our study, the period of the third disease outbreak seemed to be the most severe, in terms of the frequency of complicated cases, concomitant pathology, clinical symptoms and mortality rate. The timing of this outbreak matched with the circulation of the SARS-CoV-2 delta variant in Ukraine and it correlated with an increase in hospitalization rates across Ukraine [Citation1]. According to the CDC, the peak hospitalization rate was 1.8 per 100,000 population which was observed in September 2021 and corresponded to a period of predominance with the SARS-CoV-2 delta variant [Citation19]. Further, since January 2022 (W4), the rate of hospitalization of children with COVID-19 was 7.1 per 100,000 population and was accompanied by the spread of the omicron variant, with a predominance of hospitalizations in children in the ages from birth to four years old [Citation20]. According to the results of our study, the fourth wave of the disease was also associated with a significant increase in the number of younger pediatric patients. The greatest increase in the disease was observed in the group of children from 1 to 12 months and from 1 to 5 years (p < 0.00001).
A possible reason for the redistribution of the age association could be the introduction of adaptive quarantine, which provided the weakening of quarantine measures in the periods of the 3rd-4th waves and the opening of preschool children’s institutions [Citation21,Citation22]. This hypothesis correlates with the gradual increase in morbidity we observed in waves W1-W4, and with another study on the weakening of quarantine and the opening of children’s schools and preschools [Citation23].
It should be noticed that the increase in the frequency of severe cases was also associated with an increase of patients with concomitant pathology. As it is known from the previous studies, chronic pathology is one of the risk factors for severe and complicated course of COVID-19 in children [Citation24]. Numerous meta-analyses indicate a progressive increase in the number of hospitalizations among children with concomitant background pathology during recent outbreaks, comparing to the beginning of the epidemic [Citation25–27]. This tendency was also observed in our study, especially during the 3rd wave.
We observed an increase in general intoxication symptoms, symptoms of upper respiratory tract affection, and diarrhea. This correlates well with a previous study, in which the key symptoms of the omicron variant were symptoms of upper respiratory tract affection [Citation28], and a study reporting a predominance of fever and diarrhea symptoms in children hospitalized during the circulation of the omicron SARS-CoV-2 virus variant [Citation29].
Previous studies have found an increase in the level of C-reactive protein, D-dimer erythrocyte sedimentation rate, and procalcitonin levels [Citation30]. These results correlate with the majority of published works during all waves and are correlated with our obtained indicators.
We observed a tendency towards fewer radiological changes, which may correlate with a much slower rate of virus replication in the lungs [Citation17].
Our study had a number of limitations. The study was single-center and retrospective, and did not include outpatients or children who had out-of-hospital treatment.
In conclusion, the 3rd wave of COVID-19 corresponding to the surge of the SARS-CoV-2 virus delta variant was characterized by a more severe course and a higher frequency of complicated cases of COVID-19 in Ukrainian children. Among the hospitalized children, the proportion of patients with concomitant diseases has progressively increased. We found a regularity between the severity of the condition and the period of spread of the disease. Further studies of the clinical and epidemiological characteristics of COVID-19 are necessary for better understanding the trends of the epidemic process, and prediction of the course of the disease in the pediatric population with future variants.
Acknowledgments
The authors would like to thank all participants of this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Iryna Seriakova
Seriakova Iryna Department of Pediatric infectious diseases, Bogomolets National Medical University, Ukraine
Vitalii Yevtushenko
Yevtushenko Vitalii PhD, Associate Professor, Department of Pediatric infectious diseases, Bogomolets National Medical University, Ukraine
Sergiy Kramarov
Kramarov Sergiy MD, professor, Head of the Department of Pediatric infectious diseases, Bogomolets National Medical University, Ukraine
Liudmyla Palatna
Palatna Liudmyla PhD, Associate Professor, Department of Pediatric infectious diseases, Bogomolets National Medical University, Ukraine
Iryna Shpak
Shpak Iryna PhD, Associate Professor, Department of Pediatric infectious diseases, Bogomolets National Medical University, Ukraine
Tatiana Kaminska
Kaminska Tatiana MD, professor, Department of Pediatric infectious diseases, Bogomolets National Medical University, Head of Kyiv City Children’s Clinical Infectious Diseases Hospital, Ukraine
References
- Coronavirus Statistics – Worldometer. 2022. https://www.worldometers.info/coronavirus/country/ukraine/
- World Health Organisation (WHO) WHO coronavirus (COVID-19) dashboard. 2022. https://covid19.who.int/
- UNICEF data: Monitoring the situation of children and women. https://data.unicef.org/covid-19-and-children/
- American Academy of Pediatrics. Children and COVID-19: State-Level Data Report. 2022. https://www.aap.org/
- World Health Organization. Statement on Omicron sublineage BA.2. 2022. Accessed 22 02 2022. on Omicron sublineage BA.2. https://www.who.int/news/item/22-02-2022-statement-on-omicron-sublineage-ba.2
- European Centre for Disease Prevention and Control (ECDC) 2021. Weekly epidemiological update: omicron Variant of Concern (VOC) – week . https://www.ecdc.europa.eu/en/news-events/weekly-epidemiological-update-omicron-variant-concern-voc-week-50-data-19-december-2021
- Wang XF, Yuan J, Zheng YJ, et al. [Retracted: clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen]. Zhonghua Er Ke Za Zhi. 2020;58:E008.
- Chen ZM, Fu JF, Shu Q, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020;16(3):240–10.
- Oliveira EA, Simões Silva AC, Oliveira MC, et al. Comparison of the First and second waves of the coronavirus disease 2019 (COVID-19) pandemic in children and adolescents in a middle-income country: clinical impact associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) gamma lineage. J Pediatr, 244:P178–185 . DOI:10.1016/j.jpeds.2022.01.001. 01 05 2022. https://www.jpeds.com/article/S0022-3476(22)00001-4/fulltext
- Sheng JF, Shao L, Wang YL. Clinical features of children with coronavirus disease 2019 caused by delta variant infection. Zhongguo Dang Dai Er Ke Za Zhi = Chinese Journal of Contemporary Pediatrics. 2021 Dec 15;23(12):1267–1270.
- Meyer M, Holfter A, Ruebsteck E, et al. The Alpha Variant (B.1.1.7) of SARS-CoV-2 in children: first experience from 3544 nucleic acid amplification tests in a cohort of children in Germany. Viruses. 2021 Aug;13(8):1600.
- USA Centers for Disease Control and Prevention. Underlying medical conditions associated with high risk for severe COVID-19: information for healthcare providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html
- Rahmani S, Rezaei N. Omicron (B.1.1.529) variant: development, dissemination, and dominance. J Med Virol. 2021. 10.1002/JMV.27563
- Jansen L, Tegomoh B, Lange K, et al. Investigation of a SARS-CoV-2 B.1.1.529 (omicron) variant cluster - Nebraska, November-December 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1782–1784.
- Khandia R, Singhal S, Alqahtani T, et al. Emergence of SARS-CoV-2 Omicron (B.1.1.529) variant, salient features, high global health concerns and strategies to counter it amid ongoing COVID-19 pandemic. Environ Res. 2022 Jun[Published online 2022 Jan 29];209:112816.
- Ito K, Piantham C, Nishiura H. Relative instantaneous reproduction number of omicron SARS-CoV-2 variant with respect to the delta variant in Denmark. J Med Virol. 2021. DOI:10.1002/JMV.27560
- Chi-wai CM. 2021. HKUMed finds omicron SARS-CoV-2 can infect faster and better than delta in human bronchus but with less severe infection in lung.https://www.med.hku.hk/en/news/press/20211215-omicron-sars-cov-2-infection
- Dyer O. Covid-19: omicron is causing more infections but fewer hospital admissions than delta, South African data show. BMJ. 2021;375(3104). DOI:10.1136/BMJ.N3104
- COVID-NET. A weekly summary of US COVID-19 hospitalization data. Available at gis.cdc.gov/grasp/COVIDNet/COVID19_5.html
- Marks KJ, Whitaker M, Anglin O, et al. Hospitalizations of children and adolescents with laboratory-Confirmed COVID-19 - COVID-NET, 14 states. MMWR Morb Mortal Wkly Rep. 2022 July 2021-January 2022;71:271.
- Government portal of Ukraine. https://www.kmu.gov.ua/news/z-23-veresnya-v-usih-regionah-ukrayini-bude-vstanovleno-zhovtij-riven-epidnebezpeki-rishennya-derzhavnoyi-komisiyi-teb-ta-ns
- Wang XF, Yuan J, Zheng YJ, et al. Clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen. Zhonghua Er Ke Za Zhi. 2020;58:E008.
- Forbes H, Morton CE, Bacon S, et al. Association between living with children and outcomes from covid-19: openSAFELY cohort study of 12 million adults in England. BMJ. 2021;n628.Internet. DOI:10.1136/bmj.n628.
- Parsons S, Tran V. The Trilogy of SARS-CoV-2 in pediatrics (Part 1): acute COVID-19 in special populations. J Pediatr Pharmacol Ther. 2021;26(3):220–239.
- Irfan O, Muttalib F, Tang K, et al. Clinical characteristics, treatment and outcomes of paediatric COVID-19: a systematic review and meta-analysis. Arch Dis Child. 2021;
- Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus Disease 2019 Case Surveillance - USA. MMWR Morb Mortal Wkly Rep. 2020 January 22-May 30, 2020.;69:759.
- Kim L, Whitaker M, O’Halloran A, et al. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-Confirmed COVID-19 - COVID-NET, 14 states. MMWR Morb Mortal Wkly Rep. 2020 [March July 25,];69:1081.
- Mohiuddin M, Kasahara K. Investigating the aggressiveness of the COVID-19 Omicron variant and suggestions for possible treatment options. Respir Med. 2021;191:106716.
- Cloete J, Kruger, A., Masha, M., du Plessis, N. M., Mawela, D., Tshukudu, M., & Feucht, U. Paediatric hospitalisations due to COVID-19 during the first SARS-CoV-2 omicron (B.1.1.529) variant wave in South Africa: a multicentre observational study. Lancet Child Adolesc Health. 2022;6(5):294–302.
- Irfan O, Muttalib F, Tang K, et al. Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 - COVID-NET, 14 States, March 1-July 25, 2020. Arch Dis Child. 2021;106(5):440–448.