ABSTRACT
Background:
Acute cardiogenic pulmonary oedema is highly associated with poor in-hospital outcomes. This study aimed to determine the in-hospital outcome and its predictors among patients with acute cardiogenic pulmonary oedema at a tertiary hospital in Harar, Eastern Ethiopia, from May 1 to 20, 2023.
Methods:
A retrospective cohort study was employed among 204 patients with acute cardiogenic pulmonary oedema who were admitted between 1st May 2018 and 30th April 2023. The collected data were entered into Excel, and analysed using theSTATA software version 17. The hazard ratio with its 95% confidence interval was used and a P-value < 0.05 was considered a statistically significant association.
Results:
The overall mortality rate was 17.60 (95% CI: 11.59–26.72) per 1000 person-day observation with mean (±SD) time to death was 2.88 (±2.06) days. Age (AHR: 1.35; 95% CI: 1.04–1.74 for every 10 years), being smoker (AHR: 3.26; 95% CI: 1.05–10.10), having respiratory rate of ≥40 breaths per minute (AHR: 5.46; 95% CI: 1.71–17.45), and having anaemia (AHR: 4.35; 95% CI: 1.23–15.33) were significant predictors of in-hospital mortality.
Conclusion:
More than one in ten patients in this study died in the hospital. Therefore, special attention needs to be considered for patients with those predictors of in-hospital mortality.
Background
Acute cardiogenic pulmonary oedema is also called volume-overload pulmonary oedema. It is caused by rapid elevation in the hydrostatic pressure of the pulmonary capillaries and commonly occurs in patients having left ventricular systolic and diastolic function, valvular function, and rhythm disorders (Annette Esper et al., Citation2021; Figueras et al., Citation2016; Iqbal & Gupta, Citation2023; Malek & Soufi, Citation2023). It is a life-threatening medical emergency and patients with pulmonary oedema usually present to the emergency department with very severe breathlessness (Clark & Cleland, Citation2013). The prevalence of cardiogenic pulmonary oedema among patients having heart failure and low ejection fraction ranges from 75% to 85%. Being male and elderly increases the likelihood of having cardiogenic pulmonary oedema (Iqbal & Gupta, Citation2023).
Patients with cardiogenic pulmonary oedema have a poor treatment outcome, with a significant in-hospital mortality rate or death in hospitals ranging from 3.8% to 36.5%. Their prognosis mainly depends on several factors such as age, the severity of illness, presence of comorbidity or underlying medical conditions and difference in setting (Clark & Cleland, Citation2013; Cosentini et al., Citation2009; El-Khawas et al., Citation2021; Figueras et al., Citation2016; Militaru et al., Citation2017; Parissis et al., Citation2010; Schmickl et al., Citation2015; Sert et al., Citation2021; Tahilyani et al., Citation2018; Zanza et al., Citation2023). Despite the scarcity of data, different countries reported varying mortality rates of cardiogenic pulmonary oedema in the United Kingdom (26.2%) (Crane, Citation2002), Italy (11.4%) (Cosentini et al., Citation2009), the United States of America (36.3%) (Fedullo et al., Citation1991), France (15.6%) (Cohen & Grossi, Citation2000), Brazil (17.6%) (Wajner et al., Citation2017), and Israel (12%) (Roguin et al., Citation2000).
More than 75% of cardiovascular disease-related deaths worldwide take place in low- and middle-income countries (WHO, Citation2023). However, despite dealing with a large number of acute heart failure patients, evidence of in-hospital outcomes and predictors among patients with acute cardiogenic pulmonary oedema is sparse, particularly in our study setting. Therefore, this study aimed to assess the in-hospital outcome and its predictors among patients with acute cardiogenic pulmonary oedema among patients admitted to a tertiary hospital, in Harar, Eastern Ethiopia.
Method and material
Study setting, design, and period
An institution-based retrospective cohort study design was employed. This study was carried out at Hiwot Fana Comprehensive Specialized Hospital (HFCSH) located in Harar, Eastern Ethiopia. Harar is the capital city of Harari Regional State. The region is located in Eastern Ethiopia, at a distance of 526 km from Addis Ababa. Hiwot Fana Comprehensive Specialized Hospital is the only tertiary hospital in Harar, Eastern Ethiopia. It has a total of 235 beds. It serves as a referral hospital for Dire Dawa City Administration, Somali Region State, and the Eastern part of Oromia (Hiwot Fana Comprehensive Specialized Hospital, 2022). Data were collected from May 1 to 20, 2023.
Study population
All patients with acute cardiogenic pulmonary oedema admitted to HFCSH between 1st May 2018 and 30th April 2023 were considered for this study. Patients with acute cardiogenic pulmonary oedema but with unknown date of admission, discharge or death were excluded from the study.
Sample size and sampling techniques
All patients with acute cardiogenic pulmonary oedema admitted to HFCSH between 1st May 2018 and 30th April 2023 were considered as the sample size. Accordingly, a total of 204 patients’ medical records which fulfil the inclusion criteria were reviewed consecutively.
Study variables
The dependent variable for this study was the survival status. Sociodemographic, clinical and laboratory characteristics and the prescribed regimen were among the independent variables used in the present study.
Data collection methods
The medical records of patients with acute cardiogenic pulmonary oedema were retrospectively reviewed and data were collected using a data abstraction format. The data abstraction format was adapted from a previous study (Tirfe et al., Citation2020). Data were extracted and collected by two well-trained nurses. Patients were followed from the date of admission until discharge or death. Data on socio-demographic characteristics, clinical characteristics, in-hospital management and in-hospital outcomes were extracted using a data abstraction format.
Data quality control
Data collectors were trained before the commencement of data collection. The data abstraction format was pretested at Jugal General Hospital. The principal investigator supervised the data collection. Patients’ medical records were cross-checked with registration log books. All collected data were examined for completeness and consistency during data management, storage, and analysis.
Data entry and statistical analysis
After the data were checked for completeness and consistency, data were entered into Excel and the analysis was carried out by STATA software version 17. The descriptive variable analysis for categorical variables was performed and the results were expressed as frequency with percent. For continuous variables, the normality was tested by the Shapiro–Wilk test. Then, descriptive analysis was done and the results were presented as a median with an interquartile range (non-normal distribution).
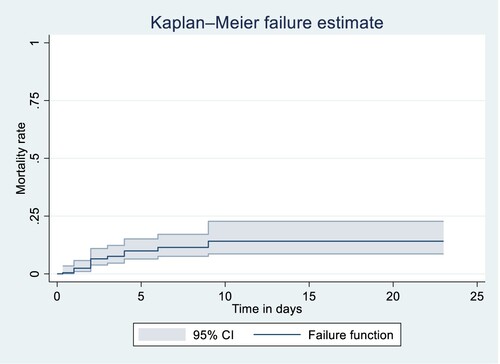
To identify the predictors of survival status, the Cox proportional hazards analysis model was computed. A bivariable Cox proportional hazards analysis model was performed to identify potential predictors of the survival status of patients with acute cardiogenic pulmonary oedema. Variables with p-value < 0.25 in bivariable Cox proportional hazards analysis were considered eligible for multivariable analysis. Associations were tested at a 95% confidence level and a p-value less than 0.05 was declared as a significant association between variables. Cox proportional hazard assumptions were tested by Schoenfeld residuals global test and log–log plot. The overall model adequacy was assessed by using the Cox-Snell residual graph. Kaplan-Meier failure curves and log-rank tests were used for the comparison of survival status between different groups of patients.
Measurement and operational definitions
The outcome of interest for this study was survival status. The verification of a survival status (death or recovery) was established by the physician’s approval of the final status of patients on their medical records. Once patients were diagnosed with acute cardiogenic pulmonary oedema, they immediately started follow-up. The independent variables were classified as socio-demographic variables (age, sex, residency, and smoking status), clinical characteristics, in-hospital management, length of hospital stay, and outcome.
Event: Death during treatment from any cause.
Censored: An individual was termed as censored if the patient was improved, self-discharged or referred to another hospital.
Pulmonary oedema: The final diagnosis of acute cardiogenic pulmonary oedema was taken from a physician’s diagnosis established according to different parameters: clinical examination, medical history, electrocardiogram, chest x-ray, echocardiographic examination, brain natriuretic peptide results, and response to therapy.
Ethical consideration
Ethical approval was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the Haramaya University College of Health and Medical Sciences with a reference number of IHRERC/196/2022. The college dean provided a letter of support to the hospital's chief clinical director for the study to be carried out. Informed, voluntary, written, and signed consent was obtained from the chief clinical director of Haramaya University Hiwot Fana Comprehensive Specialized Hospital. As this study is a retrospective medical record review, consent from patients was not needed.
Results
Socio-demographic and clinical characteristics
A total of 204 acute cardiogenic pulmonary oedema patients’ medical records were included in this study. The median age (IQR) of patients was 40 (35–54.5) years. More than half of the patients (53.43%) were males and more than two-thirds (70.59%) of them were from rural areas. Among study participants, about 37.75% were smokers, and 44.12% of the patients had at least one comorbidity. One-fifth of patients had reduced ejection fraction. Chronic rheumatic valvular heart disease (CRVHD) was the most common (44.12%) underlying illness. The median (IQR) of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were 107 (97–126) mmHg and 65 (56.5–74) mmHg, respectively. Almost half of the patients had a pulse rate of >100 beats per minute. Only 19 (9.31%) patients had a respiratory rate of ≥40 breaths per minute. A majority (84.80%) of patients were hypoxic at presentation and 82 (40.20%) patients had anaemia. The median (IQR) of serum creatinine, sodium, and potassium was 0.89 (0.68–1.19) mg/dl, 136 (132–138) mmol/L, and 4.15 (3.7–4.8) mmol/L, respectively ().
Table 1. Socio-demographic and clinical characteristics of patients with acute cardiogenic pulmonary oedema admitted to a tertiary hospital in Harar, Eastern Ethiopia from 1 May 2018 to 30 April 2023 (n = 204).
Prescribed cardiovascular drugs
Cardiovascular drugs administered during hospitalisation for patients with acute cardiogenic pulmonary oedema are presented in (). Furosemide was the most commonly (81.86%) used drug during hospitalisation of patients with acute cardiogenic pulmonary oedema followed by aspirin (36.27%).
Table 2. Cardiovascular drugs administered during hospitalisation for patients with acute cardiogenic pulmonary oedema admitted to a tertiary hospital in Harar, Eastern Ethiopia from 1 May 2018 to 30 April 2023 (n = 204).
In-hospital outcome
From 204 study participants, 22 (10.78% (95% CI: 6.88–15.87%)) of patients died. From 189 patients with censored observation; (147 (72.06%), 27 (13.24%), and 8 (3.92%) were improved, self-discharged, and referred to another hospital, respectively). The median (IQR) length of hospital stay for acute cardiogenic pulmonary oedema was 6 (4–8) days. The lowest length of follow-up was 8 h and the highest length of follow-up was 23 days. The total person-time risk was 1250.33 person-days. The overall mortality rate from acute cardiogenic pulmonary oedema was 17.60 (95% CI: 11.59–26.72) per 1000 person-day observation (). The mean (±SD) time to death was 2.88 (±2.06) days. The difference in the cumulative probability of death between patients having a respiratory rate of ≥40 breaths per minute and their counterparts was statistically significant (log-rank: p < 0.001).
Predictors of in-hospital mortality among patients with acute cardiogenic pulmonary oedema
Predictors that had an association at a p-value of <0.25 in bivariable Cox regression were included in multivariable Cox regression. Age, smoking status, SBP, DBP, RR, comorbidity, and anaemia were selected for multivariable Cox regression. In the final Cox regression model, age, smoking status, RR, and anaemia were predictors of mortality at a p-value of 0.05 level of significance (). The hazard of death was increased by 35% (AHR: 1.35; 95% CI: 1.04–1.74) per 10-year increment in patients age. Smoker patients would have more than three times (AHR: 3.26; 95% CI: 1.05–10.10) higher probability of death than those who did not smoke. The hazard of death among patients with a respiratory rate of ≥40 breaths per minute was more than five times (AHR: 5.46; 95% CI: 1.71–17.45) higher than patients with a respiratory rate of <40 breaths per minute. Compared to patients without anaemia, the probability of death was more than four fold higher (AHR: 4.35; 95% CI: 1.23–15.33) for patients with anaemia.
Table 3. Predictors of death among patients with acute cardiogenic pulmonary oedema admitted to a tertiary hospital in Harar, Eastern Ethiopia from 1 May 2018 to 30 April 2023 (n = 204).
Discussion
The aim of the current study was to assess in-hospital mortality and its predictor among patients with acute cardiogenic pulmonary oedema. Assessing in-hospital outcomes and its predictor among patients with acute cardiogenic pulmonary oedema can have great implications for healthcare professionals in planning effective and efficient inventions that help to improve the treatment outcomes of those patients. The present study showed that more than 10% of study participants with acute cardiogenic pulmonary oedema had died in the hospital and this in-hospital mortality is more likely among patients with advanced age, patients with a history of smoking, patients with elevated respiratory rate, and patients who had anaemia at admission.
In the present study, the overall in-hospital mortality from acute pulmonary oedema was 10.78% (95% CI: 6.88–15.87%). This finding is consistent with the result reported elsewhere 13.8% (Sert et al., Citation2021). However, the finding was lower than the study conducted at Austin Hospital, Australia 19.3% (El-Khawas et al., Citation2021), Tan Tock Seng Hospital, Singapore 21.06% (Tahilyani et al., Citation2018), and Barcelona, Spain 27.5% (Figueras et al., Citation2016), and higher than data reported from Acute Heart Failure Global Survey of Standard Treatment 7.4% (Parissis et al., Citation2010), Italy 3.8% (Cosentini et al., Citation2009), and 4.2% (Militaru et al., Citation2017). The possible explanation for this difference in hospital mortality from acute pulmonary oedema might be related to different factors including the age of the study participants, the study setting, and differences in treatment modalities. For instance, the median age of the participants in the current study is 40 years, which is considerably younger than the results of the previous study, where the mean age of the participants was over 60 (Tahilyani et al., Citation2018) and 70 years (Figueras et al., Citation2016). The fact that the participants in the current study were younger may have contributed to the reduced mortality rate. Another possible justification for this discrepancy might be due to the difference in the service/care provided for the patients with acute cardiogenic pulmonary oedema at each setting.
The results of the current study demonstrated that several variables, including patient age, smoking status, elevated respiratory rate, and anaemia, were independently linked with in-hospital mortality from acute pulmonary oedema. Accordingly, the risk of in-hospital mortality increased by 35% for every 10-year increment. This finding is in line with research done in Italy (Cosentini et al., Citation2009), Spain (Figueras et al., Citation2016), and Australia (El-Khawas et al., Citation2021), which found that older patients were more likely to die in hospitals from acute pulmonary oedema. Being a smoker is related to hospital mortality in the current study. As a result, people with a history of smoking had a more than threefold increased risk of dying in the hospital compared to non-smokers. Smoking may worsen the prognosis of individuals with acute pulmonary oedema by causing endothelial cell inflammation and death (Rounds & Lu, Citation2018).
Another finding from this study is that increased respiratory rate and anaemia were independent predictors of in-hospital mortality. Accordingly, patients with a respiratory rate of more than 40 breaths per minute were more than five times more likely to have in-hospital mortality from acute pulmonary oedema. Experimental evidence shows that an elevated respiratory rate may exacerbate pulmonary oedema which further progresses to impaired gas exchange, and respiratory failure and might contribute to in-hospital mortality from acute pulmonary oedema (Retamal et al., Citation2016). The likelihood of in-hospital death from acute pulmonary oedema was more than four times higher in patients with anaemia, and the finding is consistent with a report from Italy (Cosentini et al., Citation2009) where in-hospital mortality from acute pulmonary oedema was more among patients with anaemia.
Loop diuretics are the foundation of current acute heart failure treatment during hospitalisation (Felker et al., Citation2009). In the current study, furosemide was the most commonly used loop diuretic (four out of five patients) during the hospitalisation of patients with acute cardiogenic pulmonary oedema. This is because it is readily available, as well as the volume overload and congestion nature of acute cardiogenic pulmonary oedema clinical presentation.
The findings of this study should be interpreted with these limitations. This study may not accurately reflect national trends because it is based on data from a single hospital. Furthermore, because this study is based on a retrospective review of patient records, it may not display all variables that may predict variation in mortality rate.
Conclusion and recommendation
More than one in ten patients with acute pulmonary oedema had in-hospital mortality. Factors, such as the age of the patient (every 10-year increment), being a smoker, respiratory rate of more than 40 breaths/per minute, and being anaemic, were independent predictors of in-hospital mortality from acute cardiogenic pulmonary oedema. Therefore, healthcare provider needs to consider special attention while providing care for patients with advanced age, a history of smoking, elevated respiratory rate, and anaemia to reduce in-hospital mortality from acute cardiogenic pulmonary oedema. Because the mortality rate of acute cardiogenic pulmonary oedema in this study is significant, hospital managers and policy-makers must have an updated and revised protocol for managing acute cardiogenic pulmonary oedema. A multicentre prospective scale-up study is needed to find other predictors of in-hospital outcomes of cardiogenic pulmonary oedema.
Limitations of the study
The findings of this study should be interpreted with these limitations. This study may not accurately reflect national trends because it is based on data from a single hospital. Furthermore, because this study is based on a retrospective review of patient records, it may not display all variables that may predict variation in mortality rate.
Author contributions
All authors contributed to the conception, designation of the study, supervision of data collection, data analysis and interpretation, drafting or revising the article, agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Ethical approval and consent to participate
Ethical approval was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the Haramaya University College of Health and Medical Sciences with a reference number of IHRERC/196/2022. Informed, voluntary, written, and signed consent was obtained from each hospital head. Confidentiality was maintained, and the names and unique identifiers of the patients were not included in the data abstraction format. As this study is a retrospective medical record review, consent from patients was not needed.
Acknowledgements
The authors would like to thank Haramaya University, HFCSH, for the cooperation during protocol approval and data collection of the study. Also, their gratitude is extended to HFCSH administrators and card room staff members for their cooperation during data collection.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data will be available from the corresponding author upon request.
Additional information
Funding
Notes on contributors
Natanim Degefu
Natanim Degefu, an assistant professor of Pharmaceutics at School of Pharmacy College of Health and Medical Sciences, Haramaya University. Among her recent publications: ‘Emergency department overcrowding and its associated factors at HARME medical emergency center in Eastern Ethiopia', and ‘In-hospital mortality and length of stay of patients with hypertensive crisis treated at public hospitals in Harari Regional State, Eastern Ethiopia’.
Abera Jambo
Abera Jambo, a lecturer at School of Pharmacy College of Health and Medical Sciences, Haramaya University. Among his recent publications: ‘COVID-19 vaccine acceptance, use, and associated factors among health sciences students in Eastern Ethiopia', ‘Seizure Remission and Its Predictors Among Epileptic Patients on Follow-up at Public Hospitals in Eastern Ethiopia: A Retrospective Cohort Study', and ‘The Magnitude of Hypertension and Its Contributing Factors Among Patients Receiving Antiretroviral Therapy in Public Hospitals in Harar City, Eastern Ethiopia: A Cross-Sectional Study’.
Lemma Demissie Regassa
Lemma Demissie Regassa, an assistant professor at School of Public Health, College of Health and Medical Sciences Haramaya University. Currently, a PhD student at London School of Hygiene and tropical medicine in infectious disease epidemiology, with a primary focus on the epidemiology and policy of meningococcal disease. Among his recent publications: ‘The burdens, associated factors, and reasons for traditional uvulectomy in Ethiopia: A systematic review and meta-analysis', and ‘In-hospital mortality and length of stay of patients with hypertensive crisis treated at public hospitals in Harari Regional State, Eastern Ethiopia’.
Melaku Getachew
Melaku Getachew, an assistant professor of emergency and critical care medicine at School of Medicine, College of Health and Medical Sciences Haramaya University. Among his recent publications: ‘Emergency department overcrowding and its associated factors at HARME medical emergency center in Eastern Ethiopia', and ‘In-hospital mortality and length of stay of patients with hypertensive crisis treated at public hospitals in Harari Regional State, Eastern Ethiopia’.
References
- Clark, A. L., & Cleland, J. G. (2013). Causes and treatment of oedema in patients with heart failure. Nature Reviews Cardiology, 10(3), 156–170. https://doi.org/10.1038/nrcardio.2012.191
- Cohen, M., & Grossi, L. G. (2000). Prognostic factors in acute cardiogenic pulmonary edema. The American Journal of Emergency Medicine, 18(3), 342–343. https://doi.org/10.1016/s0735-6757(00)90137-2
- Cosentini, R., Aliberti, S., Bignamini, A., Piffer, F., & Brambilla, A. M. (2009). Mortality in acute cardiogenic pulmonary edema treated with continuous positive airway pressure. Intensive Care Medicine, 35(2), 299–305. https://doi.org/10.1007/s00134-008-1281-7
- Crane, S. D. (2002). Epidemiology: Treatment and outcome of acidotic, acute, cardiogenic pulmonary oedema presenting to an emergency department. European Journal of Emergency Medicine, 9(4), 320–324. https://doi.org/10.1097/00063110-200212000-00005
- El-Khawas, K., Richmond, D., Zwakman-Hessels, L., Cutuli, S. L., Belletti, A., Naorungroj, T., Abdelkarim, H., Yang, N., & Bellomo, R. (2021). Radiologically and clinically diagnosed acute pulmonary oedema in critically ill patients: Prevalence,: Patient characteristics, treatments and outcomes. Critical Care and Resuscitation, 23(2), 154–162. https://doi.org/10.51893/2021.2.oa2
- Esper, A., Martin, G. S., & Gerald, W. S. (2021). Pulmonary edema I: Cardiogenic pulmonary edema. Decker Medicine.
- Fedullo, A. J., Swinburne, A. J., Wahl, G. W., & Bixby, K. (1991). Acute cardiogenic pulmonary edema treated with mechanical ventilation. Factors determining in-hospital mortality. Chest, 99(5), 1220–1226. https://doi.org/10.1378/chest.99.5.1220
- Felker, G. M., O'Connor, C. M., & Braunwald, E. (2009). Loop diuretics in acute decompensated heart failure: Necessary? Evil? A necessary evil? Circulation: Heart Failure, 2(1), 56–62. https://doi.org/10.1161/circheartfailure.108.821785
- Figueras, J., Bañeras, J., Peña-Gil, C., Barrabés, J. A., Rodriguez Palomares, J., & Garcia Dorado, D. (2016). Hospital and 4-year mortality predictors in patients with acute pulmonary edema with and without coronary artery disease. Journal of the American Heart Association, 5(2), https://doi.org/10.1161/jaha.115.002581
- Iqbal, M. A., & Gupta, M. (2023). Cardiogenic pulmonary edema (StatPearls). StatPearls Publishing LLC.
- Malek, R., & Soufi, S. (2023). Pulmonary edema (StatPearls). StatPearls Publishing LLC.
- Militaru, C., Mărginean, C. M., Neagoe, C.-D., Deliu, R. C., Alexandru, D. O., Mănescu, M. D., Liliac, I. M., & Rogoveanu, I. (2017). In-hospital and short-term prognostic factors in acute pulmonary edema: Clinical and morphological features. Romanian Journal of Morphology and Embryology = Revue Roumaine de Morphologie et Embryologie, 58(4), 1347–1356.
- Parissis, J. T., Nikolaou, M., Mebazaa, A., Ikonomidis, I., Delgado, J., Vilas-Boas, F., Paraskevaidis, I., Mc Lean, A., Kremastinos, D., & Follath, F. (2010). Acute pulmonary oedema: Clinical characteristics: Prognostic factors, and in-hospital management. European Journal of Heart Failure, 12(11), 1193–1202. https://doi.org/10.1093/eurjhf/hfq138
- Retamal, J., Borges, J. B., Bruhn, A., Cao, X., Feinstein, R., Hedenstierna, G., Johansson, S., Suarez-Sipmann, F., & Larsson, A. (2016). High respiratory rate is associated with early reduction of lung edema clearance in an experimental model of ARDS. Acta Anaesthesiologica Scandinavica, 60(1), 79–92. https://doi.org/10.1111/aas.12596
- Roguin, A., Behar, D. M., Ami, H. B., Reisner, S. A., Edelstein, S., Linn, S., & Edoute, Y. (2000). Long-term prognosis of acute pulmonary oedema—An ominous outcome. European Journal of Heart Failure, 2(2), 137–144. https://doi.org/10.1016/S1388-9842(00)00069-6
- Rounds, S., & Lu, Q. (2018). Cigarette smoke alters lung vascular permeability and endothelial barrier function (2017 Grover Conference Series). Pulmonary Circulation, 8(3), 2045894018794000. https://doi.org/10.1177/2045894018794000
- Schmickl, C. N., Biehl, M., Wilson, G. A., & Gajic, O. (2015). Comparison of hospital mortality and long-term survival in patients with acute lung injury/ARDS vs cardiogenic pulmonary edema. Chest, 147(3), 618–625. https://doi.org/10.1378/chest.14-1371
- Sert, E. T., Kokulu, K., Murat, G., & Mutlu, H. (2021). Predictors of in-hospital mortality in patients admitted to the emergency department with cardiogenic pulmonary edema. Journal of Contemporary Medicine, 11(2), 203–207. https://doi.org/10.16899/jcm.853237
- Tahilyani, A., Watson, T., Low, R., Foo, H., & Woon, C. (2018). Clinical outcome and prognosis of patients with acute pulmonary oedema (COPP APO). Journal of Cardiovascular Disease Medicine, 1(1), 39–42.
- Tirfe, M., Nedi, T., Mekonnen, D., & Berha, A. B. (2020). Treatment outcome and its predictors among patients of acute heart failure at a tertiary care hospital in Ethiopia: A prospective observational study. BMC Cardiovascular Disorders, 20(1), 16. https://doi.org/10.1186/s12872-019-01318-x
- Wajner, A., Zuchinali, P., Olsen, V., Polanczyk, C. A., & Rohde, L. E. (2017). Causes and predictors of in-hospital mortality in patients admitted with or for heart failure at a tertiary hospital in Brazil. Arquivos Brasileiros de Cardiologia, 109(4), 321–330. https://doi.org/10.5935/abc.20170136
- WHO. (2023). Cardiovascular Diseases. Retrieved August 26 from https://www.afro.who.int/health-topics/cardiovascular-diseases.
- Zanza, C., Saglietti, F., Tesauro, M., Longhitano, Y., Savioli, G., Balzanelli, M. G., Romenskaya, T., Cofone, L., Pindinello, I., Racca, G., & Racca, F. (2023). Cardiogenic pulmonary edema in emergency medicine. Advances in Respiratory Medicine, 91(5), 445–463. https://doi.org/10.3390/arm91050034