?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Introduction
Chronic kidney disease (CKD) is a major public health concern in Saudi Arabia. it is pertinent to mention that in the Southwestern region of Saudi Arabia. Hypertension and diabetes mellites are considered the major drivers of CKD. Research has documented worldwide the inappropriate dose adjustments in patients, ranging from 25% to 77%, of drugs requiring dose modifications. Pharmacists are pivotal members of the healthcare team, tasked with addressing issues pertaining to medications. This study aims to unveil pharmacist perspectives on renal dose adjustment in Saudi Arabia an important step in gauging their involvement in promoting healthy behaviours.
Method
A cross-sectional study design was conducted from December 2023 to January 2024 among pharmacists working in diverse healthcare settings, including clinical and hospital pharmacies, retail, and community pharmacies who had direct encounters with patients diagnosed with CKD. A validated questionnaire, the Renal Dose Adjustment-13 (RDQ-13) was used for this study. For comparing the knowledge, attitude, and perception scores of pharmacists statistical tests like One-Way ANOVA, and independent t-test; while for factors influencing the knowledge, attitude, and perception scores a multivariate linear regression was performed. The statistical significance level was set at 0.05.
Results
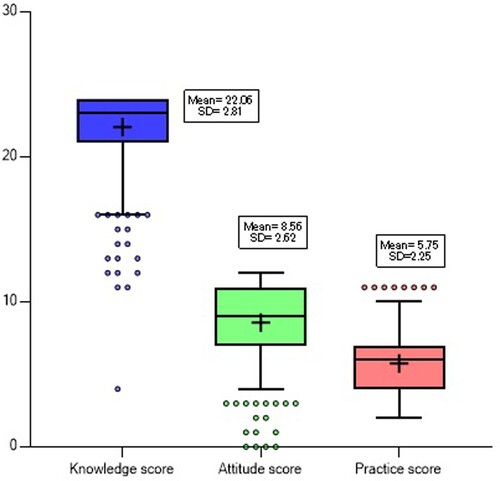
A total of 379 pharmacists completed the questionnaire, the knowledge score of pharmacists was 22.06 ± 2.81, while the attitude score was 8.56 ± 2.62 and the practice score was 5.75 ± 2.25. The findings of multivariate linear regression analysis indicated a statistically significant positive association between knowledge score and pharmacist’s age while for practice score the findings revealed a statistically negative association between working setting and designation of pharmacists.
Conclusion
The pharmacist in Saudi Arabia exhibited a proficient knowledge score of drug dosage adjustment pertinent to renal function while the attitude and practice score was less as compared to the knowledge score.
Introduction
Worldwide Chronic kidney disease (CKD) is a major public health concern affecting 10–15% of and contributes to morbidity and mortality in a considerable number of patients (Alemu et al., Citation2020). The statistics of different studies conducted worldwide indicate a significant rise (87%) in the prevalence of CKD from 1990 to 2016, particularly among individuals with chronic illnesses and older adults (Bikbov et al., Citation2020; Xie et al., Citation2018). Likewise, between 1990 and 2017, there was a 41.5% increase in the global mortality rate associated with CKD cases (Bikbov et al., Citation2020).
In recent decades, CKD has become a major public health concern in Saudi Arabia, driven by the increasing incidence and prevalence of end-stage renal disease (Almutary et al., Citation2013). According to recent statistics in Saudi Arabia, over 20,000 patients are receiving hemodialysis treatment (Alzahrani et al., Citation2023). According to findings of Global Burden of Diseases (GBD) in the year 2017, Saudi Arabia experienced a 25.1% increase in the number of CKD cases, with approximately two million reported cases and 3,818 deaths alone in 2017 (Tyrovolas et al., Citation2020). The increase in the number of cases and mortality resulting from CKD is attributed to an increase in the number of cases of hypertension, diabetes, and obesity (Ben Salah et al., Citation2023). Moreover, it is pertinent to mention that in the Southwestern region of Saudi Arabia, the prevalence of CKD is 2–4 times higher among the immediate family members (first or second-degree relatives) of individuals already diagnosed with CKD (Alsuwaida et al., Citation2010; Mousa et al., Citation2021). This increase in CKD is likely linked to the growing incidence of hypertension, diabetes mellitus, and obesity in Saudi Arabia (Ahmed et al., Citation2018; Albujays et al., Citation2018; Alobaidi, Citation2021; Hassanien et al., Citation2012; Mahmoud et al., Citation2023).
The prevalence of CKD is considered to be high among the elderly, females, and individuals with more co-morbid illnesses especially those with hypertension and diabetes mellitus, consequently heightening disease progression because of polypharmacy as reported by a study in Spain (Santos-Díaz et al., Citation2020). Literature has established known causes for elevation in the new cases of CKD resulting from hypertension and diabetes mellites and they act as major drivers of new cases of CKD (Banerjee et al., Citation2022; Kohagura, Citation2023; Webster et al., Citation2017), a study reporting the impact of hypertension and diabetes on the onset of CKD among the Japanese population revealed that both conditions contribute to CKD development, with hypertension exerting more contribution as compared to diabetes (Kaneyama et al., Citation2023). Similarly, literature has shown that diabetes is also a significant factor in CKD development, accounting for 33% of CKD cases among adults, and diabetic nephropathy in 20-40% of patients (Ginawi et al., Citation2014).
In developed countries, it is anticipated that the prevalence of hypertension and diabetes will increase by 60% and 69% by the year 2025 and 2030, respectively (Kearney et al., Citation2005; Shaw et al., Citation2010). Likewise, studies assessing the collective prevalence of hypertension (22.66%), and diabetes mellitus (10.1%) have revealed an upward trend in both conditions in Saudi Arabia. This upward surge in hypertension and diabetes cases across Saudi Arabia poses a subsequent heightened risk for the development of CKD cases (Alqahtani et al., Citation2023; Alshammari et al., Citation2023).
Apart from exposure to multiple drugs due to various co-morbid illnesses (Santos-Díaz et al., Citation2020), CKD has a substantial impact on the pharmacokinetics and pharmacodynamics of drugs that are primarily excreted by kidneys. Consequently, this leads to elevated plasma drug concentrations and increased risk of drug toxicity, and associated adverse events due to reduced drug excretion in case the drug requires renal dose adjustment (Saleem et al., Citation2017; Yang et al., Citation2016). Furthermore, the inadequate adjustment of drug doses increases both treatment expenses and hospitalisation costs, placing an additional economic strain on both patients and the healthcare system (Z. Hassan et al., Citation2021). Research has documented inappropriate dose adjustments in a notable number of patients, ranging from 25% to 77%, of drugs requiring dose modifications (Drenth-van Maanen et al., Citation2015; Fink & Chertow, Citation2009; Teh & Lee, Citation2019; Zafar, Rehman, Shah, Goh, et al., Citation2023).
Owing to the medication complexity associated with multiple co-morbidities in CKD patients, effective management requires a multidisciplinary healthcare team including a pharmacist (Joy et al., Citation2005; Wang et al., Citation2015). Literature supports the role of the pharmacist in improving the healthcare team's ability to promote safe, effective, and economical drugs (Al Raiisi et al., Citation2019; Joy et al., Citation2005; Wang et al., Citation2015). Pharmacists, given their clinical training, play an important role in addressing drug-related problems and excel in ensuring patient safety by delivering pharmaceutical services (Inoue et al., Citation2016). Similarly, studies have also reported the valuable contributions of pharmacists while managing patients with CKD and end-stage renal disease, leading to improved clinical outcomes and enhanced patient care (Gheewala et al., Citation2014; Y. Hassan et al., Citation2009; Inoue et al., Citation2016).
Considering the existing literature, it appears that medications necessitating dose adjustments are often not appropriately tailored for patients with CKD, a practice observed in both developed and developing nations. However, this matter has not been thoroughly explored in Saudi Arabia. Pharmacists play a crucial role in managing medication-related concerns within the healthcare framework. Thus, uncovering their viewpoints on renal dose adjustment in Saudi Arabia is vital for assessing their contribution to fostering positive health practices. Therefore, this study aimed to address this gap in the current body of research.
Methodology
Study design
A cross-sectional study was carried out to evaluate the knowledge, attitudes, and practices of pharmacists practicing in Saudi Arabia regarding renal dose adjustment. The study was conducted from December 2023 to January 2024. The study was performed in Riyadh, the capital city of Saudi Arabia. Pharmacists working in various healthcare settings, such as clinical and hospital pharmacies, as well as retail and community pharmacies, were included if they had direct interactions with patients diagnosed with CKD.
Inclusion/exclusion criteria
The study included pharmacists who had a minimum of one year of professional experience, possessed an undergraduate degree in pharmacy, and worked in clinical pharmacy, hospital pharmacy, or retail/community pharmacy environments. They were actively involved in the care of CKD patients, either directly or indirectly through roles involving medication reception and dispensing in community/retail pharmacies towards the CKD patients. However, pharmacists who did not meet the above-mentioned inclusion criteria were excluded from participation in this study.
Study tool
A validated questionnaire, the Renal Dose Adjustment-13 (RDQ-13), sourced from the literature (Zafar, Rehman, Shah, Ali, et al., Citation2023), was utilised in this study. The RDQ-13 questionnaire comprised various sections: demographic characteristics including gender, age, educational status, work experience, pharmacist's working environment, and designation. The knowledge segment is composed of six domains, each comprising four questions offering binary response options. Each correctly answered question was scored 1 point, resulting in a total knowledge score of 24. The attitude section consisted of four questions measured on a Likert scale ranging from 0 to 3, yielding a cumulative attitude score of 12. The practice section comprised three questions rated on a Likert scale with scoring ranges of 1–4 for two questions and 0–3 for the last question, yielding a total practice score of 11.
Study procedure
The study's objective was communicated to the pharmacists, emphasising the importance of assessing pharmacists’ knowledge, attitudes, and practices concerning CKD patients. Pharmacists who expressed interest in participating provided informed written consent before enrollment. The RDQ-13, a self-administered questionnaire, was provided to each pharmacist, allowing them 10–15 minutes to complete it based on their expertise and understanding.
Ethics approval
The study was approved by the Institutional Review Board (IRB) of the respective hospital and all the study procedures were compliant with the standard of IRB and with the Helsinki Declaration of 1975.
Sample size calculation
In this study, the sample size was calculated using a recommended formula (Daniel, Citation1978) using an anticipated prevalence (p = 0.57) of 5.7% of CKD in KSA (Alsuwaida et al., Citation2010) with a 95% confidence interval and 5% precision (d = 0.05). The sample size arrived at a total of n = 377 patients using the following assumptions: p = 0.57, d = 0.05, and Z (Z-statistics, 1.96) in the below-mentioned sample size formula.
Statistical analysis
The collected data was entered into Excel and transferred to Statistical Package for the Social Sciences (SPSS) version-24®. Data quality is crucial for the reliability of the study findings. Therefore, the entered data was assessed for accuracy twice to identify and rectify any potential errors or inconsistencies.
Data analysis was performed using SPSS version 24®. The frequency, percentages, and continuous variables including mean with standard deviation (SD) were reported by using descriptive statistics. To ascertain the factors influencing the knowledge, attitude, and practice scores, a multivariate linear regression analysis was performed, wherein the outcome score was considered as the dependent variable and the demographic characteristics of pharmacists served as independent variables. Initially, univariate linear regression was employed to identify factors, whereby those factors exhibiting a p-value <0.25 were selected for inclusion in the multivariate linear regression analysis. Subsequently, comparisons of knowledge, attitude, and practice scores among pharmacists concerning demographic characteristics were conducted using independent t-tests and One-way ANOVA. Statistical significance was determined at a p-value <0.05.
Results
Out of the total sample of 420 pharmacists approached, 379 pharmacists completed the questionnaire, resulting in a response rate of 90.24%. The majority of respondents were female (64.1%), aged between 20 and 30 years (75.7%), and had less than 5 years of experience (71.0%). The predominant educational background was Pharm D holders (79.4%), while the most common work settings were clinical pharmacy (44.6%) and hospital pharmacy (31.1%). In terms of designation, most participants were staff pharmacists (40.4%), followed by trainee pharmacists (32.2%). Access to drug reference materials was widespread, with 34.0% reporting ‘Others’ as the most common source for drug information, followed by 18.7% citing Lexicomp [details as shown in ].
Table 1. Demographic characteristics of the study participants (n = 379).
To evaluate pharmacists’ understanding of renal dose adjustment, the RDQ-13 questionnaire consisted of six domains, each comprising four questions. The data offers insights into pharmacists’ familiarity with renal dose adjustment for patients with CKD. Across these domains, respondents exhibit a notable awareness of renal considerations in medication management, [Details in Supplementary Table 1]. The mean scores ± standard deviations for each domain, indicative of knowledge assessment 3.32 ± 0.92, 3.85 ± 0.52, 3.60 ± 0.75, 3.78 ± 0.59, 3.72 ± 0.68, and 3.80 ± 0.58, respectively [Details in Supplementary Table 1]. However, the overall knowledge score among pharmacists concerning renal dose adjustment (mean ± SD) is 22.06 ± 2.81 [shown in ].
The attitude score of the pharmacist was assessed on four questions using the Likert scale. Regarding the question ‘How important is dose adjustment of medications for patients’ 82.1% of the pharmacists considered it very important. However, 34.8% reported as moderately confident to ‘How confident are you in calculating the appropriate dose for a patient’. Concerning the pharmacist’s willingness to question ‘Are you willing to consult the specialist regarding medication dose adjustment’ 42.2% responded with very willing and 47.2% reported being very receptive to the question ‘How receptive are you on feedback regarding your prescribing practices for patients’ [as shown in Supplementary Table 2]. The overall attitude score of pharmacists toward renal dose adjustment was (mean ± SD) of 8.56 ± 2.62 [shown in ].
For the assessment of the practice score of pharmacists, 35.1% of pharmacists reported encountering renal-impaired patients rarely in their practice. Additionally, 30.9% reported frequently adjusting the dose adjustment of prescribed medication for the patients. Moreover, 43.3% affirmed that renally impaired patients receive appropriate medication management [shown in Supplementary Table 3]. The overall practice score among pharmacists (mean ± SD) is 5.75 ± 2.25 [shown in ].
For comparison of knowledge, attitude, and practice scores, the knowledge score did not differ significantly among gender and professional experience. However, the age of pharmacists, education status differs significantly; pharmacists within the age group of 41–50 years had higher knowledge scores (23.50 ± 1.08) with a p-value = 0.007, while pharmacists holding a higher qualification had better knowledge scores (22.59 ± 2.87) as compared to others with a p-value = <0.001. Similarly, the knowledge scores of pharmacists working in different settings and designations also differ significantly, pharmacists working in clinical pharmacy had higher knowledge scores (22.96 ± 2.57) with p-value = <0.001, and assistant manager pharmacy had a higher score (23.62 ± 0.93) with p-value = 0.024 [as shown in ]. Regarding the comparison of the attitude score did not differ significantly among age, gender, education level, working setting, professional experience, and designation of pharmacists [as shown in ]. Furthermore, regarding the comparison of practice scores the score did not differ significantly among gender, age, professional experience, and education; however, the score differs significantly between the working setting and designation of pharmacist. The pharmacists working in a hospital pharmacy setting had a higher score (6.69 ± 2.19) as compared to other working setting having p-value = <0.001 and trainee pharmacists had a higher score (6.65 ± 2.14) as compared to other designated pharmacists with p-value = 0.001 [as shown in ].
Table 2. Scores of knowledge, attitude, and practice in relation to participants’ demographic characteristics.
We conducted a univariate linear regression analysis to pinpoint factors that were independently linked with pharmacists’ knowledge, attitude, and practice scores concerning dosage adjustment in CKD patients. The selection of potential factors relied on statistical significance, with a threshold of p-value < 0.25 for subsequent multivariate analysis. The findings from the multivariate linear regression analysis indicated a statistically significant positive association between pharmacists’ knowledge score and pharmacist’s age. This suggests that as increase in age of pharmacists, their knowledge scores tend to rise (β = 0.512; 95% CI = 0.025; 0.999; p-value = 0.040) [as shown in ]. Similarly, the findings revealed that there was a statistically negative association between working setting and the designation of pharmacists, the pharmacists working in other settings as compared to hospital pharmacy tend to have lower practice scores (β = – 0.824; 95% CI = −1.095;−0.554; p-value = <0.001) and designation of a pharmacist have a statistically significant negative association with practice score, other designation of pharmacist as compared to trainee pharmacist tend to have lower practice score (β = – 0.211; 95% CI = −0.362;−0.060; p-value = 0.006) [details in ].
Table 3. Factors affecting knowledge, attitude and practice scores of pharmacists on RDQ-13 scale regarding renal dose adjustment
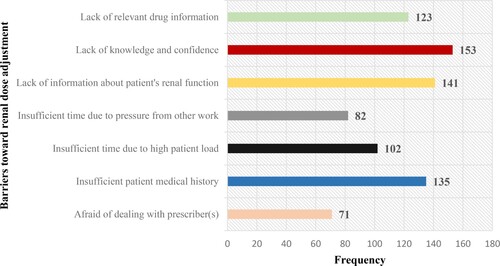
Pharmacists identified notable barriers hindering renal dose adjustment practice, including ‘lack of knowledge and confidence, lack of information about patient’s renal function and insufficient patients medical history’, as depicted in . Among pharmacists surveyed, the majority (52.5%) expressed a preference for online training as part of CME sessions, followed by in person with face to face sessions (34.0%), workshops (8.7%), and other modes, if available (4.8%)
Discussion
The renal function of individuals with CKD is already compromised, and the standard doses of medications recommended for managing various comorbidities and therapeutic outcomes in healthy patients may pose a risk of toxicity for these renal-compromised individuals. Due to factors such as self-medication for co-morbid conditions and overburden on healthcare facilities, the need for adjusting doses of medications is often overlooked among CKD patients. This oversight contributes to the deterioration of kidney health, leading to complications. With the consistent increase in the number of CKD cases, it is crucial to evaluate the knowledge of pharmacists, who play a pivotal role in dose adjustment.
The practice of pharmacy is rapidly evolving in Saudi Arabia and presenting the advanced and best practice in the region (Al-Abdelmuhsin et al., Citation2021). Given the vital role of pharmacists in the healthcare system in Saudi Arabia, this study is of high significance among pharmacists working in various settings in Saudi Arabia. Given the rising prevalence of CKD cases, it is imperative to evaluate and improve the comprehension and practices of healthcare professionals, with a special emphasis on pharmacists, concerning precise medication doses and a rational treatment approach for CKD management. Pharmacists play a crucial role as essential members of interdisciplinary healthcare teams, particularly in addressing drug-related issues through the application of clinical expertise. They demonstrate proficiency in enhancing patient safety through diverse activities such as screening, dispensing, monitoring, counselling, and delivering pharmaceutical services to inpatient populations (Basey et al., Citation2013; Inoue et al., Citation2016). Numerous studies emphasise the beneficial impact of pharmacists in the management of CKD and end-stage renal disease, ultimately improving outcomes and refining the overall quality of patient care (Al-Abdelmuhsin et al., Citation2020; Gheewala et al., Citation2014; Y. Hassan et al., Citation2009; Inoue et al., Citation2016). The increase in cases of CKD in Saudi Arabia is likely linked to the growing incidence of hypertension, diabetes mellitus, and obesity in Saudi Arabia (Ahmed et al., Citation2018; Albujays et al., Citation2018; Alobaidi, Citation2021; Hassanien et al., Citation2012; Mahmoud et al., Citation2023). As these underlying conditions continue to increase, it is foreseeable that the demand for renal dose adjustment will also rise. Consequently, there is an urgent need to consistently evaluate and improve the competency of healthcare professionals, particularly pharmacists, in ensuring accurate dosing and rational treatment for CKD.
Due to limited literature available on this subject, we were unable to compare our findings with the majority of published research. Nevertheless, we made comparisons wherever possible. The findings of our study revealed that pharmacists working in hospital pharmacy setups have statistically significant higher knowledge and practice score as compared to other pharmacists working in setups other than hospital pharmacy. However, research conducted in Pakistan (Zafar, Rehman, Shah, Ali, et al., Citation2023) and Malaysia (Teh & Lee, Citation2019) suggests that pharmacists in clinical pharmacy settings tend to have higher knowledge and practice scores regarding renal dose adjustment. Regarding the attitude score, the chief pharmacist in our study demonstrated a higher score as compared to pharmacists working on other designations. Our study findings strengthen the claim that the attitude score of pharmacist working on higher designated position were higher like a study in Pakistan reported the attitude score of chief pharmacists was significantly higher compared to other pharmacists (Zafar, Rehman, Shah, Ali, et al., Citation2023). This higher score of the attitude of the chief pharmacist can be attributed to the higher professional experience. Furthermore, chief pharmacists occupying and working in higher positions often undergo various trainings and receive clinical support from experts, which tend to enhance their decision-making ability and emphasise the importance of renal dose adjustment in CKD patients (Boussadi et al., Citation2013; Teh & Lee, Citation2019). However, the practice score decreases with an increase in designation of pharmacist in our study.
Our study findings revealed that there was a statistically significant association between trainee pharmacists with the practice score, with an increase in the designation of pharmacists the practice score decreases as evident from our study findings. Our study findings are aligned with the findings of another study that reported the practice score was significantly higher among resident pharmacists compared to others (Zafar, Rehman, Shah, Ali, et al., Citation2023). The possible reasons for this may be that trainee pharmacists are recent graduates and their knowledge is fresh and tend to follow the standards and guidelines that contributed toward their higher practice score. Furthermore, the continuation of trainee pharmacist jobs is linked to performance-driven, so this motivation keeps them stuck to the standard guidelines and results in higher practice score as compared to others. Similarly, our study revealed that with an increase in the age of pharmacists, their knowledge score increases as evident by our findings, and a similar pattern is observed with professional experience. Our study findings are aligned with findings of a similar nature performed in Pakistan and Malaysia reported pharmacists aged 41–50 years had higher knowledge, attitude, and practice scores than other pharmacists (Zafar, Rehman, Shah, Ali, et al., Citation2023). However, a Malaysian study found that participants under the age of 30 years had greater knowledge scores, while those participants with 11–20 years of experience had higher scores (Teh & Lee, Citation2019).
The primary barriers identified by pharmacists in this study regarding renal dose adjustment of medications were ‘lack of knowledge and confidence, lack of information about patient’s renal function and insufficient patients medical history’. A similar study among pharmacists reported insufficient time due to high patient load, lack of information about patient's renal function, and insufficient patient medical history (Zafar, Rehman, Shah, Ali, et al., Citation2023). Similar findings were reported by a study in which pharmacists faced difficulty in obtaining the medical history of the patients and renal function (Teh & Lee, Citation2019). Yet another study identified obstacles, including challenges in accessing information about a patient's renal function, and a lack of proficiency among pharmacists in pertinent pharmaceutical knowledge (Kondo et al., Citation2014). In our study the most common source of information used by pharmacists was ‘Others (Medscape, Renal Dosing Handbook, mobile applications, etc.)’ by (34.0%), followed by Lexicomp (18.7%). In another study conducted in Saudi Arabia among pharmacists dealing with CKD patients, Micromedex was used by 88.9% and Up-to-date (95.6%) of pharmacists as a source of drug information source in outdoor patients (Al-Abdelmuhsin et al., Citation2021). Among hospital pharmacists, the most common source of drug information as reported by the study is Up-to-date as community pharmacists do not have access to up-to-date (Wallace et al., Citation2014).
In our study, pharmacists exhibited commendable knowledge and attitude scores regarding renal dose adjustment. With the increasing prevalence of CKD and diabetes mellitus cases in Saudi Arabia, pharmacists play a pivotal role as members of the healthcare team, collaborating closely with physicians and nephrologists to mitigate drug-related issues, including medication dosing adjustments. Given that CKD patients often present with comorbidities and require multiple medications, the need for medication adjustments is frequent and complex. Therefore, pharmacists should undergo continuous medical education and refresher courses to stay updated with evolving guidelines aimed at slowing CKD progression. Moreover, it is crucial to prioritise the awareness of the general public regarding the associated risks of CKD. Our recommendations are aligned with a study conducted in Saudi Arabia; Training programmes tailored for healthcare professionals, including pharmacists, have the potential to notably decrease instances of inappropriate dosage prescriptions (Al-Abdelmuhsin et al., Citation2021).
Strengths and limitations
This study presents a noteworthy achievement by being the first study assessing the knowledge, attitude, and practice of pharmacists in Saudi Arabia concerning renal dose adjustment among CKD patients. Furthermore, this study serves as a significant contribution by laying a solid framework for health regulatory and decision-making bodies of the country to actively engage pharmacists in raising awareness among the general public regarding CKD. Limitations of the study include the following; some participants in the study could have provided exaggerated responses to some questions in the questionnaire or hesitated to provide truthful answers for upholding self-esteem and reputation. Similarly, these findings cannot be generalised to the entire pharmacist community of Saudi Arabia. Future studies involving pharmacists working in different regions of Saudi Arabia should be performed to generalise the findings.
Conclusion
Considering the elevated prevalence of CKD in Saudi Arabia, the pharmacist, as an integral part of the healthcare team, exhibited a proficient understanding of drug dosage adjustment pertinent to renal function. Nevertheless, there is room for enhancement in attitude and practice scores. The Ministry of Health and higher education authorities must prioritise the formulation of actionable strategies aimed at raising awareness of this concern and implementing effective measures to ensure the well-being of CKD patients across Saudi Arabia.
Competing interests
The authors declare that they have no competing interests.
Ethics and consent
The study was approved by the Institutional Review Board (IRB) of King Fahad Medical City Hospital. IRB Log Number: 24-020 (dated: 17th January 2024) and all the study procedures were compliant with the standard of IRB and with the Helsinki Declaration of 1975.
Supplemental Material
Download MS Word (21.9 KB)Acknowledgements
The authors would like to thank the Research Centre at King Fahad Medical City, Riyadh Second Health Cluster, for the valuable technical support provided for the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ahmed, I. A. B., Alharbi, S. H., Alateeq, F. A., Aloriney, A. M., Alharbi, A. A. H., AlSogair, A. R. A., Almansour, A. D. M., Albalawi, A. M. A., & Ahmed, H. G. (2018). Knowledge and awareness towards chronic kidney disease risk factors in Saudi Arabia. International Journal of Clinical Medicine, 09(11), 799–808. https://doi.org/10.4236/ijcm.2018.911066
- Al-Abdelmuhsin, L., Al-Ammari, M., Babelghaith, S. D., Wajid, S., Alwhaibi, A., Alghadeer, S. M., Al Arifi, M. N., & Alrabiah, Z. (2021). Assessment of pharmacists’ knowledge and practices towards prescribed medications for dialysis patients at a tertiary hospital in Riyadh Saudi Arabia. Healthcare, 9 (9), 1098.
- Al-Abdelmuhsin, L., Al-Ammari, M., D Babelghaith, S., Wajid, S., Asiri, Y. A., Almetawazi, M. S., Alghadeer, S. M., & Al-Arifi, M. N. (2020). Pharmacist-led medication counseling for patients undergoing hemodialysis: A path to better adherence. International Journal of Environmental Research and Public Health, 17(7), 2399. https://doi.org/10.3390/ijerph17072399
- Albujays, D. S., El-barbary, H. S., Althafar, A. K., Almulla, A. H., Hussain, M. A. A.-S., & Ali, S. I. (2018). Study of the level of awareness of chronic kidney diseases among diabetic patients in Al-Ahsa governorate, Kingdom of Saudi Arabia (cross-sectional study). International Journal of Scientific Study, 5(12), 88–91.
- Alemu, H., Hailu, W., & Adane, A. (2020). Prevalence of chronic kidney disease and associated factors among patients with diabetes in northwest Ethiopia: A hospital-based cross-sectional study. Current Therapeutic Research, 92, 100578. https://doi.org/10.1016/j.curtheres.2020.100578
- Almutary, H. H., Bonner, A., & Douglas, C. (2013). Chronic kidney disease in Saudi Arabia: A nursing perspective. Middle East Journal of Nursing, 101(900), 1–9.
- Alobaidi, S. (2021). Knowledge of chronic kidney disease among the population of Saudi Arabia evaluated using a validated questionnaire: A cross-sectional study. Patient Preference and Adherence, 15, 1281–1288. https://doi.org/10.2147/PPA.S315369
- Alqahtani, B., Elnaggar, R. K., Alshehri, M. M., Khunti, K., & Alenazi, A. (2023). National and regional prevalence rates of diabetes in Saudi Arabia: Analysis of national survey data. International Journal of Diabetes in Developing Countries, 43(3), 392–397. https://doi.org/10.1007/s13410-022-01092-1
- Al Raiisi, F., Stewart, D., Fernandez-Llimos, F., Salgado, T. M., Mohamed, M. F., & Cunningham, S. (2019). Clinical pharmacy practice in the care of Chronic Kidney Disease patients: A systematic review. International Journal of Clinical Pharmacy, 41(3), 630-666. https://doi.org/10.1007/s11096-019-00816-4
- Alshammari, S. A., Alshammari, A. S., Alshammari, H. S., & Ahamed, S. S. (2023). Overview of hypertension in Saudi Arabia: A systematic review and meta-analysis. Saudi Medical Journal, 44(10), 951–964. https://doi.org/10.15537/smj.2023.44.10.20230178
- Alsuwaida, A. O., Farag, Y. M., Al Sayyari, A. A., Mousa, D., Alhejaili, F., Al-Harbi, A., Housawi, A., Mittal, B. V., & Singh, A. K. (2010). Epidemiology of chronic kidney disease in the Kingdom of Saudi Arabia (SEEK-Saudi investigators)-a pilot study. Saudi Journal of Kidney Diseases and Transplantation, 21(6), 1066–1072.
- Alzahrani, N. S., Almarwani, A. M., Alhowaymel, F., & Alharbi, H. F. (2023). The lived experience of middle-aged Saudi patients With End-stage chronic renal disease on hemodialysis treatment. Journal of Transcultural Nursing, 34(4), 263–269. https://doi.org/10.1177/10436596231166041
- Banerjee, D., Winocour, P., Chowdhury, T. A., De, P., Wahba, M., Montero, R., Fogarty, D., Frankel, A. H., Karalliedde, J., Mark, P. B., Patel, D. C., Pokrajac, A., Sharif, A., Zac-Varghese, S., Bain, S., Dasgupta, I., On behalf of the Association of British Clinical, D., & The Renal, A. (2022). Management of hypertension and renin-angiotensin-aldosterone system blockade in adults with diabetic kidney disease: Association of British Clinical Diabetologists and the Renal Association UK guideline update 2021. BMC Nephrology, 23(1), 9. https://doi.org/10.1186/s12882-021-02587-5
- Basey, A. J., Krska, J., Kennedy, T. D., & Mackridge, A. J. (2013). Prescribing errors on admission to hospital and their potential impact: A mixed-methods study. BMJ Quality & Safety, 23(1), 17–25.
- Ben Salah, G., Farooqui, M., Salem Alshammari, M., Elghazali, A., Kassem, L., Ibrahim, N., Ben Abdelmalek, I., & Rasheed, M. K. (2023). Prevalence, types and disclosure of complementary and alternative medicine (CAM) use among chronic kidney disease (CKD) patients in Saudi Arabia. Journal of Pharmaceutical Policy and Practice, 16(1), 89. https://doi.org/10.1186/s40545-023-00589-2
- Bikbov, B., Purcell, C. A., Levey, A. S., Smith, M., Abdoli, A., Abebe, M., Adebayo, O. M., Afarideh, M., Agarwal, S. K., & Agudelo-Botero, M. (2020). Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 395(10225), 709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
- Boussadi, A., Caruba, T., Karras, A., Berdot, S., Degoulet, P., Durieux, P., & Sabatier, B. (2013). Validity of a clinical decision rule-based alert system for drug dose adjustment in patients with renal failure intended to improve pharmacists’ analysis of medication orders in hospitals. International Journal of Medical Informatics, 82(10), 964–972. https://doi.org/10.1016/j.ijmedinf.2013.06.006
- Daniel, W. W. (1978). Biostatistics: A foundation for analysis in the health sciences. Wiley.
- Drenth-van Maanen, A. C., van Marum, R. J., Jansen, P. A. F., Zwart, J. E. F., van Solinge, W. W., & Egberts, T. C. G. (2015). Adherence with dosing guideline in patients with impaired renal function at hospital discharge. PLoS One, 10(6), e0128237. https://doi.org/10.1371/journal.pone.0128237
- Fink, J. C., & Chertow, G. M. (2009). Medication errors in chronic kidney disease: One piece in the patient safety puzzle. Kidney International, 76(11), 1123–1125. https://doi.org/10.1038/ki.2009.315
- Gheewala, P. A., Peterson, G. M., Curtain, C. M., Nishtala, P. S., Hannan, P. J., & Castelino, R. L. (2014). Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs & Aging, 31(11), 825–835. https://doi.org/10.1007/s40266-014-0208-y
- Ginawi, I. A., Ahmed, H. G., & Al-Hazimi, A. M. (2014). Assessment of risk factors for chronic kidney disease in Saudi Arabia. International Journal of Science and Research, 3, 446–450.
- Hassan, Y., Al-Ramahi, R. J., Aziz, N. A., & Ghazali, R. (2009). Impact of a renal drug dosing service on dose adjustment in hospitalized patients with chronic kidney disease. Annals of Pharmacotherapy, 43(10), 1598–1605. https://doi.org/10.1345/aph.1M187
- Hassan, Z., Ali, I., Ullah, A. R., Ahmed, R., Zar, A., Ullah, I., Rehman, S., Khan, A. U., Ullah, R., & Hanif, M. (2021). Assessment of medication dosage adjustment in hospitalized patients With chronic kidney disease. Cureus, 13(2), e13449. https://doi.org/10.7759/cureus.13449
- Hassanien, A. A., Al-Shaikh, F., Vamos, E. P., Yadegarfar, G., & Majeed, A. (2012). Epidemiology of end-stage renal disease in the countries of the Gulf Cooperation Council: A systematic review. JRSM Short Reports, 3(6), 1–21. https://doi.org/10.1258/shorts.2012.011150
- Inoue, Y., Takikawa, M., Morita, Y., Takao, K., Kanamoto, I., & Sugibayashi, K. (2016). A comparison of pharmacists’ role functions across various nations: The importance of screening. Research in Social and Administrative Pharmacy, 12(2), 347–354. https://doi.org/10.1016/j.sapharm.2015.05.005
- Joy, M. S., DeHart, R. M., Gilmartin, C., Hachey, D. M., Hudson, J. Q., Pruchnicki, M., Dumo, P., Grabe, D. W., Saseen, J., & Zillich, A. J. (2005). Clinical pharmacists as multidisciplinary health care providers in the management of CKD: A joint opinion by the nephrology and ambulatory care practice and research networks of the American college of clinical pharmacy. American Journal of Kidney Diseases, 45(6), 1105–1118. https://doi.org/10.1053/j.ajkd.2005.02.027
- Kaneyama, A., Hirata, A., Hirata, T., Imai, Y., Kuwabara, K., Funamoto, M., Sugiyama, D., & Okamura, T. (2023). Impact of hypertension and diabetes on the onset of chronic kidney disease in a general Japanese population. Hypertension Research, 46(2), 311–320. https://doi.org/10.1038/s41440-022-01041-9
- Kearney, P. M., Whelton, M., Reynolds, K., Muntner, P., Whelton, P. K., & He, J. (2005). Global burden of hypertension: Analysis of worldwide data. The Lancet, 365(9455), 217–223. https://doi.org/10.1016/S0140-6736(05)17741-1
- Kohagura, K. (2023). The public health impact of hypertension and diabetes: A powerful tag team for the development of chronic kidney disease. Hypertension Research, 46(2), 339–340. https://doi.org/10.1038/s41440-022-01114-9
- Kondo, Y., Ishitsuka, Y., Shigemori, E., Irikura, M., Kadowaki, D., Hirata, S., Maemura, T., & Irie, T. (2014). Awareness and current implementation of drug dosage adjustment by pharmacists in patients with chronic kidney disease in Japan: A web-based survey. BMC Health Services Research, 14(1), 1–8. https://doi.org/10.1186/s12913-014-0615-0
- Mahmoud, M. A., Ibrahim, A., Fadil, H. A., Alalawi, A. M., Alnezary, F. S., Alahmadi, Y., Alolayan, S. O., Althaqfan, S. S., Omer, S., & Goresh, H. K. (2023). Assessment of public knowledge about chronic kidney disease and factors influencing knowledge levels: A cross-sectional study. Medicina, 59(12)), 2072.
- Mousa, D., Alharbi, A., Helal, I., Al-Homrany, M., Alhujaili, F., Alhweish, A., Marie, M. A., & Al Sayyari, A. (2021). Prevalence and associated factors of chronic kidney disease among relatives of hemodialysis patients in Saudi Arabia. Kidney International Reports, 6(3), 817–820. https://doi.org/10.1016/j.ekir.2020.12.029
- Saleem, A., Masood, I., & Khan, T. M. (2017). Clinical relevancy and determinants of potential drug-drug interactions in chronic kidney disease patients: Results from a retrospective analysis. Integrated Pharmacy Research & Practice, 6, 71–77. https://doi.org/10.2147/IPRP.S128816
- Santos-Díaz, G., Pérez-Pico, A. M., Suárez-Santisteban, MÁ, García-Bernalt, V., Mayordomo, R., & Dorado, P. (2020). Prevalence of potential drug–drug interaction risk among chronic kidney disease patients in a Spanish hospital. Pharmaceutics, 12(8), 713. https://doi.org/10.3390/pharmaceutics12080713
- Shaw, J. E., Sicree, R. A., & Zimmet, P. Z. (2010). Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice, 87(1), 4–14. https://doi.org/10.1016/j.diabres.2009.10.007
- Teh, X. R., & Lee, S. W. H. (2019). Pharmacists’ attitude, self-reported knowledge and practice of dosage adjustment among chronic kidney disease patients in Malaysia. Journal of Pharmacy Practice and Research, 49(2), 179–185. https://doi.org/10.1002/jppr.1450
- Tyrovolas, S., El Bcheraoui, C., Alghnam, S. A., Alhabib, K. F., Almadi, M. A. H., Al-Raddadi, R. M., Bedi, N., El Tantawi, M., Krish, V. S., & Memish, Z. A. (2020). The burden of disease in Saudi arabia 1990–2017: Results from the global burden of disease study 2017. The Lancet Planetary Health, 4(5), e195–e208. https://doi.org/10.1016/S2542-5196(20)30075-9
- Wallace, K. L., Beckett, R. D., & Sheehan, A. H. (2014). Pharmacist perception and use of UpToDate®. Journal of the Medical Library Association : JMLA, 102(4), 296–300. https://doi.org/10.3163/1536-5050.102.4.012
- Wang, S.-M., Hsiao, L.-C., Ting, I.-W., Yu, T.-M., Liang, C.-C., Kuo, H.-L., Chang, C.-T., Liu, J.-H., Chou, C.-Y., & Huang, C.-C. (2015). Multidisciplinary care in patients with chronic kidney disease: A systematic review and meta-analysis. European Journal of Internal Medicine, 26(8), 640–645. https://doi.org/10.1016/j.ejim.2015.07.002
- Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney disease. The Lancet, 389(10075), 1238–1252. https://doi.org/10.1016/S0140-6736(16)32064-5
- Xie, Y., Bowe, B., Mokdad, A. H., Xian, H., Yan, Y., Li, T., Maddukuri, G., Tsai, C.-Y., Floyd, T., & Al-Aly, Z. (2018). Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney International, 94(3), 567–581. https://doi.org/10.1016/j.kint.2018.04.011
- Yang, P., Chen, N., Wang, R. R., Li, L., & Jiang, S. P. (2016). Inappropriateness of medication prescriptions about chronic kidney disease patients without dialysis therapy in a Chinese tertiary teaching hospital. Therapeutics and Clinical Risk Management, 12, 1517–1524. https://doi.org/10.2147/TCRM.S116789
- Zafar, R., Rehman, I. U., Shah, Y., Ali, Z., Ming, L. C., & Khan, T. M. (2023). Knowledge, attitude and perceptions of pharmacists regarding renal dose adjustment among chronic kidney disease patients in Pakistan. Journal of Pharmaceutical Policy and Practice, 16(1), 102. https://doi.org/10.1186/s40545-023-00606-4
- Zafar, R., Rehman, I. U., Shah, Y., Goh, K. W., & Ming, L. C. (2023). Assessment of inappropriate dose adjustment of antimicrobials and other medicines Among chronic kidney disease patients: A multicenter observational study. Progress In Microbes & Molecular Biology, 6(1). doi:10.36877/pmmb.a0000348