Abstract
Background: While international experience suggests that well-trained primary care physicians improve the quality and cost effectiveness of health care, family medicine (FM) as the discipline of the specialist primary care physician appears to not be an attractive career for medical graduates in South Africa (SA). The aim of this study was to establish final-year medical students’ knowledge about FM and its relevance to the healthcare system, explore their perceptions of the discipline’s relevance, and identify their specialty preference.
Methods: This was a descriptive study conducted amongst final-year medical students at the University of KwaZulu-Natal (UKZN) in 2017 at the conclusion of their seven-week FM module. Data were collected using a self-administered questionnaire and results were analysed descriptively.
Results: The response rate of completed questionnaires was 80.2% (157/196). Students reported limited exposure to FM in their early undergraduate years and low levels of awareness about essential public health programmes. Students showed good awareness of the six roles of family physicians (FPs), but FM was only the sixth most popular choice for specialisation.
Conclusions: In general, students had favourable views concerning FM and its role in the future of healthcare delivery in SA, although their knowledge of essential health programmes was poor. The majority of students had limited interest in pursuing a career in FM. A key recommendation to address these issues is to introduce FM into the curriculum earlier, to cover the key roles of the FP, and provide teaching that highlights the relevance of FM to health system programmes.
Introduction
A 2007 review of the American literature by the late Barbara Starfield showed that an increase in the number of primary care physicians in the health sector was associated with improved health outcomes, including all-cause cancer, heart disease, stroke, infant mortality, low birthweight, life expectancy and self-rated health.Citation1 Although the South African context, with its quadruple burden of disease, is very different from the US experiences, recent work by von Pressentin suggests that the family physician (FP), as a well-trained specialist primary care physician, can have a significant impact on healthcare delivery with better indicators of performance and processes at district hospitals that had FPs than at district hospitals that did not have FPs.Citation2 The WHO report ‘Primary Health Care—Now More Than Ever’ noted that a better balance amongst specialised curative care, first contact care and health promotion contributed to significant improvements in health outcomes.Citation3 They identified excessive specialisation of healthcare providers and the narrow focus of many disease programmes as contributing to the fragmentation of healthcare services and poor health outcomes. In 2009, a resolution on primary health care (PHC) at the 62nd World Health Assembly highlighted the need to train and retain adequate numbers of health workers with an appropriate skills mix, including primary health care nurses, midwives, allied health professionals and primary care physicians, in order to ensure universal access to primary health care.Citation4
In South Africa (SA), most primary care is provided by a mixture of private general practitioners (GPs), family physicians as specialist primary care physicians, nurses at PHC clinics, and hospital-based FM departments. The role of the FP has been defined in a consensus document, and includes that of expert care provider, consultant and multi-skilled generalist, as well as a leader in clinical governance, community-orientated primary care (COPC), supervision and capacity building, along with other members of the PHC team.Citation5
The White Paper on National Health Insurance (NHI), Department of Health (DOH) Strategic Plan 2015 and the Government Gazette of August 12, 2011 all speak to the important role of primary care physicians in healthcare delivery in SA.Citation6–8 In addition the Ideal Clinical Realisation and Maintenance Program (ICRM) has recognised the role of family physicians as part of the specialist support team in the mentoring of PHC nurses, clinical audit and training to improve the quality of PHC.Citation9
In 2011, the Human Resources for Health 2030 (HRH 2030), a human resources planning document for the National Department of Health (NDOH), identified a shortage of 888 FPs in South Africa, this figure being based on the aim of having 0.2 FPs per 10 000 population.Citation8 This would allow one FP to be placed at every district hospital and community health centre (CHC), and to be part of the District Clinical Specialist team in each District, where they would be responsible for improving clinical outcomes at primary care facilities. Other expert bodies have suggested that there should be one to three FPs per 10 000 population, or one FP available to every family in a community, with the lowest of these targets requiring almost 5 000 more FPs to be available in the country.Citation10 In response to the HRH 2030 document, the eight university departments of family medicine in SA and the national Department of Health (DOH) established targets for training FPs, with each department aiming to have an annual intake of 13 new registrars and an output of at least 10 each year following the four years of specialist training. Assuming an attrition rate of 25%, these targets were meant to reduce the shortage of FPs from 888 to 593 by 2016.Citation8 However, since 2012, only 18–20 FPs have qualified nationally per year from the eight universities training FPs.Citation11
In 2008, the training platform at the University of KwaZulu-Natal (UKZN) was extended to include FM registrars in response to the needs of the health system. The purpose of the FM registrar programme is to train multi-skilled ‘expert’/specialist generalists who are able to cope with the majority of the conditions seen at district hospitals.Citation12 In addition to the clinical role, the FM training prepares postgraduate students to provide expertise in clinical governance, community-orientated primary care (COPC), supervision and capacity building.Citation5 These subjects are taught regularly or as discreet long rotations within the registrar programme, highlighting their importance to FM and the health system.
By December 2017, only 13 FPs had graduated from the UKZN registrar training programme, equating to only two graduates per year over the last six years. There are a number of hypotheses (based on the personal observations of the first author) for this poor throughput, some of which may also be relevant to undergraduates’ specialty choices. These include:
FM is a relatively new specialty and is not an established option for local graduates.
The career pathway for graduating FPs in SA is not clear, with a number of graduates filling clinical manager posts rather than specialist FP posts, as FP posts have not been available.
The KwaZulu-Natal Department of Health (KZN DOH) froze FM training posts at district hospitals from 2013 to 2016 due to financial constraints limiting the number of FPs who could be trained.
Since 2017, the KZN DOH has only allocated four registrar posts annually to FM, which is substantially lower than the number envisioned.
Since the start of the registrar training programme at UKZN in 2009, there has been a high attrition rate, with only 13 of the 22 registrars selected between 2009 and 2016 having achieved the full FP qualification due to personal reasons, or poor preparation for the programme.
Thus, despite the apparent recognition of the importance of the specialist generalist, the output of FPs at UKZN has been low, with potential health gains and cost-saving opportunities having been missed.
In the undergraduate MBChB programme at UKZN the Department of Family Medicine is responsible for 4–5 didactic lectures in each of years 1–3. These lectures focus predominantly on aspects of health promotion, prevention, ethics and health systems. In addition FPs facilitate in the Making a Difference module where first-year students participate in five ‘HIV and me’ workshops and do 16 hours of voluntary work at community centres. The selective 01, 02 and 03 modules run in years 2, 3 and 4 are coordinated by the Family Medicine and Public Health Medicine Departments and focus on the link between patients presenting in the consultation rooms and upstream factors that contribute to ill health. In years 4, 5 and 6 the Family Medicine department is responsible for 6- or 7-week block attachments, which are based at a PHC clinic (fourth year), district hospital outpatient department (fifth year) and rural district hospital (sixth year). Students have exposure to general practice during the selective programme and a four-day GP attachment in the fifth year. Family physicians are involved in all levels of teaching.
The aim of the undergraduate training is to expose students to the field of FM, ensure that they become skilled in the comprehensive management of undifferentiated problems at a district hospital, function without the support of specialists on site and are able to apply national health policies and engage with communities. Little is known about the career intentions and knowledge of final-year medical students regarding FM at UKZN. The aim of this study was to provide a baseline of students’ knowledge about FM and primary care programmes, their perceptions of the discipline’s relevance and their specialty preference (if any).
Methods
This was a descriptive study using a comprehensive self-administered 25-point questionnaire that covered the aims of the research project. The questionnaire was distributed to all 196 final-year students at the conclusion of their Integrated Primary Health Care (IPC3) module. The initial version of the questionnaire was piloted amongst a sample of 10 interns, medical officers and consultants at Wentworth Hospital to ensure that the questions were clear and unambiguous, with minor changes being made to the questionnaire based on the responses. There were no exclusion criteria, as all final-year students were invited to participate in the research.
Data collection took place in 2017, at the last contact session one week before the final examination at the end of each FM module. The module coordinator provided a printed informed consent form and questionnaire to complete and return on the same day, to ensure that completing the questionnaire did not interfere with student study time and to allow for students to decline participation. Close-ended questions and Likert scales were used to assess the level of exposure to FM during the undergraduate years, the role of FPs in the health system, and the students’ level of awareness of National Health Insurance (NHI), PHC re-engineering, District Clinical Specialist Teams (DCSTs), Ward Based Outreach Teams (WBOTs) and School Health Teams. The quantitative data were tabulated using SPSS® (IBM Corp, Armonk, NY, USA) and analysed descriptively.
Three open-ended questions (questions 12, 13 and a comments space at question 25), were included in the questionnaires to allow students to give their opinions on generalist training and the role of family medicine in this training. These questions were analysed separately, coded and generated first-level themes. Ethical permission for this study was given by the Biomedical Research and Ethics Committee of the University of KwaZulu-Natal (BE055/17), the UKZN registrar and the Head of Department of Family Medicine. An information sheet was given to each participant and consent was obtained prior to their completing the questionnaire.
Results
A total of 157 students completed the questionnaire (response rate 80.2%; 157/196), of whom 62% (97/ 157) were female. In terms of race, 67% (92/137) were Black, 24% (33/137) were Indian, 6% (10/137) were Coloured, 2% (2/137) were White, while 20/157 (13%) participants did not indicate their race. One-third (52/155, 33%) had attended schools in rural areas, 45% (70/155) in urban areas, 21% (33/155) in peri-urban areas, while two participants did not indicate where they attended school. Most of the students attended public schools, with 28/157 (18%) of students matriculating from private schools (8 Black, 1 White, 2 Coloured and 13 Indian participants; 4 did not indicate their race). Although the question on school quintile status piloted well with interns, it was only answered by 80 students (51%) and was not analysed due to the large amount of missing data.
Regarding the students’ knowledge about FM as a specialty, most were not aware that it would be a rotation when they applied to medical school (118/157, 75%). The majority reported that their main exposure to FM occurred during years 4–6 (112/157, 71%) as opposed to years 1–3 (29/157, 19%). Most students were aware that FM is a registered specialty with the HPCSA (137/157, 87%). Students had varying levels of awareness that a FM registrar programme was offered at UKZN (143/157, 91%), UCT (106/157, 68%), Witwatersrand (78/157, 50%), Stellenbosch (74/157, 47%), Pretoria (64/157, 41%), Free State (51/157, 33%), Sefako Makgatho University (58/157, 37%) and Walter Sisulu University (41/157, 26%).
Students reported a steady increase in exposure to FM from the first to last years of study. Utilising Likert scales, they agreed/strongly agreed that they were exposed to FM in Making a Difference (70/157, 45%) and Becoming a Professional (75/157, 48%) (both first-year modules), Selective 01 (89/157, 57%) (second-year module), Selective 02 (93/157, 59%) (third-year module), Selective 03 (93/157, 59%) and Integrated Primary Care (IPC) 1 (106/157, 68%) (both fourth-year modules), IPC2 (112/157, 71%) (fifth-year module) and IPC3 (123/157, 78%) (sixth-year module).
Student views on the main roles of a FP varied from specialist (35/157, 22%), to general hospital doctor (45/157, 29%) to GP (65/157, 41%). Most students were aware of and agreed with the six roles of an FP as identified in the national consensus document (see student responses in ).
Table 1: Students’ awareness of the roles of the family physician (n = 157)
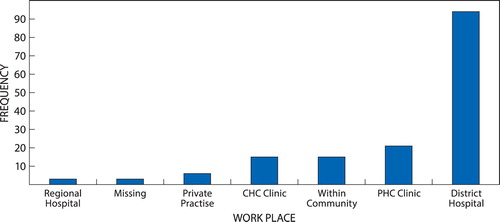
In all, 102 (65%) reported that FPs can effectively manage more than 75% of patients’ total healthcare needs in a PHC setting or at a district hospital. Over 85% (133/157) indicated that FPs should focus on individuals, families and communities rather than on only one of these groups and most indicated that the FP should be based at PHC sites (see ). Most respondents (133/157, 87%) also reported that they agreed/strongly agreed that FPs can reduce the cost of care and improve overall healthcare delivery.
Figure 1: Students’ perceptions of the main workplace for family physicians. PHC: Primary Health Care, CHC: Community Health Centre.
Less than 50% of students reported good awareness or excellent knowledge of national health insurance (NHI), PHC Re-engineering, District Clinical Specialist Teams (DCSTs), Ward Based Outreach Teams (WBOTs) and School Health Teams (SHT) (). However, despite reporting a poor understanding of NHI and PHC Re-engineering, 74% either agreed (79/157) or strongly agreed (38/157) that FPs will play a critical role in these areas.
Table 2: Likert scale of the awareness of primary care programmes (n = 157)
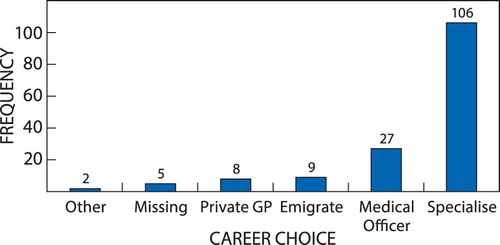
The majority of students agreed or strongly agreed they would remain in the public sector (106/157, 68%) with a smaller number indicating a decision to emigrate (9; 6%) or go directly into private GP practice (8; 5%)—see .
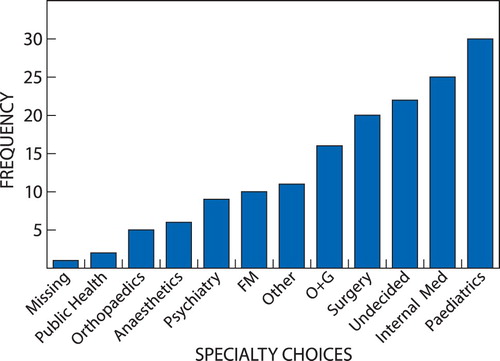
Although only 106 students had definite intentions to specialise, 156 gave an answer on potential specialty choice. Paediatrics was the most popular specialisation choice (30/157, 19%), whereas FM (10/157, 6%) was sixth on the list, with 22 respondents still undecided (). Of the 157 students, 85% (134) made their choices based on personal interest or passion, 24% (38/157) reported that they did not choose FM because they felt that it was too demanding, while 31% (49/157) had no interest in it. Of the 10 students who intend to specialise in family medicine, eight were Black, with no other demographic variable being associated with this specialisation intention.
First-level themes have been grouped into positive and negative perceptions of final-year students concerning family medicine and are presented in .
Table 3: Positive and negative perceptions of final year medical students concerning family medicine
Discussion
In this study, 58% (92/157) of the sample were Black students. A 2012 study of this cohort as first-year medical students at UKZN reported that the class was 73% Black students.Citation13 It is possible that many Black students declined to participate in this study, resulting in the gap. Alternatively, the possible attrition of Black students between first and final year is of concern. Although this is an incidental finding for this study, it is an important issue in the context of transformation of higher education in South Africa and needs further investigation and appropriate intervention if the results are confirmed.
Just over 30% of students indicated that they were of rural origin, which is similar to the 27% found at South African medical schools between 1999 and 2002, with 43% of the population living in rural areas at the time.Citation14 As a number of studies have shown that rural students are more likely to work in rural areas, South African medical schools have been encouraged to review their admission criteria to ensure that they train sufficient graduates willing to service rural populations.Citation10,Citation15,Citation16 In 2017 a new admission policy for health science courses, based on quotas for each of the 11 districts in KwaZulu-Natal (KZN) was introduced at UKZN to ensure the equitable admission of students from rural areas.Citation17 It is hoped that this new intake policy will go some way to ensuring that there are an adequate number of graduates who will be willing to work in rural areas.
Although 62% of the sample was female, there was no gender preference for FM. In contrast, a 2014 study among first- to fourth-year students at the University of the Free State showed a female preference for FM as a specialty.Citation18 The low number of women choosing a career in FM has been noted by the Academy of Family Medicine, which issued a consensus statement that advocated for the long-term role of women in FM as role models, in leadership and in gender-based research.Citation5
The majority of students in this study were unaware that FM was a specialty before they started their studies. Fewer than 60% reported exposure to FM in their early years, which is of concern, as FPs are involved in teaching in first, second and third year modules. A study in Turkey during the development of FM in that country reported that medical students began to cement their career choices while still in their preclinical year, and that as FM was not a well-known specialty choice at the time, it did not prompt enquiry among students.Citation19 In a Nepalese study of 1 112 medical students and graduates, only four chose general practice initially, while 569 (51%) respondents already had a specialty choice early on in medical school.Citation20 A 2018 appraisal of global evidence suggests that undergraduate primary care exposure can influence students towards a primary care career.Citation21 These findings suggest that if a career in FM is to be promoted, exposure to the role and scope of FM practice should be incorporated early into the curriculum to improve students’ perceptions, dispelling any negative stereotypes and providing them with a more accurate portrayal of the nature of the specialty. It is hoped that the greater emphasis on training generalist doctors, introduced into the UKZN curriculum in 2016, will encourage more graduates to consider a career in family medicine.
Final-year students thought that the main clinical role of an FP was that of a GP (41%), and were not aware of the distinction between a GP and a specialist family physician. They were aware that FM is a registered specialty with the HPCSA (87%), but it is not clear whether they understood the implications of this registration as a specialist in terms of alternate career options and medical aid billing, and whether this information would have impacted on their specialty choice. Most were aware that FM training is offered at UKZN (91%) but were not as aware of this option at the other seven universities (range 26%–68%). This low level of awareness could be in keeping with a general low level of prominence of FM amongst other specialties.
There was a steady increase in exposure to FM from the first (45%) to the last (78%) years of training, and good understanding of the wider roles of the FP in teaching, support of other clinicians, clinical governance and outreach in support of the re-engineering of PHC. It is important that students understand the wider roles of the FP as District Health Managers in SA have identified clinical care and governance as key competencies of FP.Citation22 In addition, co-workers of FPs perceived them to have a high impact as a care provider, consultant, clinical trainer, leader of clinical governance and champion of COPC.Citation23
Students in general had suboptimal knowledge about NHI, PHC Re-engineering, WBOTs, DCSTs and SHTs. This was despite spending six weeks working in a rural district hospital during their IPC3 rotation, where they practise according to PHC re-engineering principles and were expected to do a home visit with the community caregiver (CCGs). The WBOTs, SHTs and CCGs are an integral aspect of re-engineering of PHC. Although doctors are not often active members of these teams, it is important that they understand and are supportive of the role that these teams play in health promotion and disease prevention. This finding is disappointing as in 2015, 83% of those who participated in the UKZN selective modules evaluation reported an improved understanding of a population perspective on health, and having gained public health knowledge and skills.Citation24 The difference in findings suggests that learning during the Selectives modules (years 2–4) is not reinforced in later years, and highlights a critical gap in the training at UKZN. It is essential that graduates have a clear understanding of these PHC initiatives and the important move from curative to preventative-based services. In light of these results, the curriculum at UKZN needs to be interrogated to determine whether or not these principles are being appropriately taught and, if not currently embedded in the curriculum, where they could be included to enable the students to understand how the healthcare system works, regardless of their ultimate career choices.
Despite their poor understanding of NHI and re-engineering of PHC, most students believed that FM can play a critical role in NHI and PHC re-engineering, and that FPs can effectively manage the majority of patients presenting at PHC facilities, as well as reduce the cost of care and improve overall healthcare delivery. This perception is encouraging, and is consistent with the findings of Starfield and recent research in the South African context by von Pressentin, who reported that FPs have a higher perceived role impact than other doctors in the same facility, regardless of location (rural vs. urban), type of facility or FM training model.Citation1,Citation23 This data should be used to advocate for creating family physician posts and to encourage students to consider a career in FM.
Despite the recognition of the important role of FM, students did not appear to be interested in pursuing a career in this area of medicine, with only 10 indicating an interest in specialising in FM. This is in contrast to a survey of this same cohort in 2012 where 39% of respondents indicated that they were very likely to go into FM.Citation13
The low number of students who intended pursuing a career in primary care may indicate a negative perception of their role in future systems, e.g. NHI, earning potential or social status—this needs further research. In keeping with other studies, most students plan to specialise (68%) with many choosing a career in paediatrics, medicine or surgery, specialties that dominate the curriculum at most medical schools.Citation20 Although there is limited research in this area in Africa, a study in Ghana reported that FM was the least preferred medical specialty for postgraduate training.Citation25
These student responses also point to a disjunction between intentions and reality, and highlight the poor preparation of students for working life, with the 2009 statistics from the College of Medicine of South Africa and HPCSA indicating that 65% of doctors currently working in South Africa are practising as generalists (21 079 generalists vs. 10 229 specialists).Citation26 In the light of these statistics, it is of concern that 68% of students plan to specialise while medical schools should be preparing this proportion of graduates to work as generalists. These results also highlight the mismatch between student intentions and the human resource needs as documented in the HRH 2030 targets.Citation8
The open-ended questions (concerning undergraduate training, the role of FM and reasons for specialty choices) drew varied and thoughtful responses. Most students were positive about the role of FM in PHC and rural practice, and thought that FM could contribute to greater cost-effectiveness and integration. However, a number of students felt that FM was not a real specialty and not relevant in urban areas. There were conflicting thoughts about depth and breadth of knowledge required for FM, with some students finding it boring, while others found it too challenging. A qualitative study in Mozambique shows that compared with the traditional curriculum, an innovative or problem-based learning curriculum can empower students with skills, attitudes and competencies to better cope with the tensions that characterise FM.Citation27
Limitations
The study population was limited to the final-year class of 2017 at UKZN, and the results may not be generalisable to other classes or universities. In addition, piloting of the questionnaire was done amongst interns rather than final-year students, who might have a different perspective on the relevance of the questions from final-year students. As there was only an 80% response rate at one university, larger studies involving the other medical schools are needed to assess final-year students’ knowledge of FM and their career choices. In addition, students were asked to fill in the questionnaire at the end of their FM block and to remember their exposure to FM over the preceding six years, which could have resulted in significant recall and information bias. The study was conducted by FM department members and, despite being anonymous, some responses may have been influenced by both performance and social desirability bias, especially so regarding the role of FPs in practice, although in the section on career choices the majority chose specialties other than FM. A similar study could be conducted by another UKZN department to reduce this type of bias.
Conclusions and recommendations
Although the final-year class of 2017 at UKZN perceived FM to have an important role to play in healthcare delivery, only 10 students (7%) indicated an interest in pursuing it as a specialisation. Most students had poor knowledge of primary care programmes, which are essential to FM. If students are to be encouraged to consider a career in FM, thought needs to be given to introducing FM into the curriculum earlier, covering the key roles of the FP, as well as teaching that highlights the relevance of FM to health system programmes, such as the re-engineering of PHC. The FM fraternity also needs to highlight the benefits of becoming an FP, as this could attract more students to the specialty.
In order to meet the challenges of healthcare delivery in SA there is clearly a need for scaling up of FPs in KZN and throughout the country, starting with improved undergraduate training. To achieve this objective, in addition to curriculum initiatives, thought needs to be given to the selection of appropriate undergraduate students who would be willing to serve the future needs of the health system.
Disclosure statement
No conflict of interest was reported by the authors.
ORCID
R Omed Ali http://orcid.org/0000-0001-7764-5075
References
- Macinko J, Starfield B, Shi L. Quantifying the health benefits of primary care physician supply in the United States. Int J Heal Serv Plann Admin Eval. 2007;37(1):111–26. doi: 10.2190/3431-G6T7-37M8-P224
- von Pressentin KB, Mash RJ, Baldwin-Ragaven L, et al. The influence of family physicians within the South African district health system: a cross-sectional study. Ann Fam Med. 2018;16:28–36. doi: 10.1370/afm.2133
- WHO. The world health report 2008: Primary health care now more than ever. Geneva: WHO; 2008.
- WHO, editor. Primary health care, including health system strengthening. Sixty second world health assembly; 2009. . Geneva: WHO; 2009.
- Mash R, Reid S. Statement of consensus on Family Medicine in Africa. Afr J Prm Health Care Fam Med. 2010;2(1):Art. #1518.
- Department of Health. National health insurance for South Africa, Towards universal health coverage. In National Health Act, 2003. Amended 28/6/2017.
- Department of Health. Strategic Plan 2015/16—2019/20. nDOH; 2015.
- Human Resources for Health for South Africa 2030. South African National Department of Health 2011. [Online], Available from https://www.gov.za/sites/www.gov.za/files/hrh_strategy_0.pdf
- Department of Health. Ideal Clinic South Africa. nDOH; 2013.
- Mash R, Ogunbanjo G, Naidoo S, Hellenberg D. The contribution of family physicians to district health services: a national position paper for South Africa 2015. S Afr Fam Pract. 2015;57(3):54–61.
- Mash R, Von Pressentin K. Family medicine in South Africa: exploring future scenarios. S Afr Fam Pract. 2017;59(6):224–7. doi: 10.1080/20786190.2016.1272231
- Colleges of Medicine SA, Regulations: For Admission To The Fellowship Of The College Of Family Physicians of South Africa FCFP(SA), 2016.
- Azu O. Choice of speciality amongst first-year medical students in the Nelson R. Mandela School of Medicine, University of KwaZulu-Natal. 2013;1–7.
- Tumbo JM, Couper ID, Hugo JFM. Rural-origin health science students at South African universities. SAMJ S Afr Med J. 2009;99:54–6.
- de Vries E, Reid S. Do South African medical students of rural origin return to rural practice? S Afr Med J. 2003;93(10):789–93.
- Wilson N, Couper I, De Vries E, Reid S, Fish T, Marais B. A critical review of Interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas 2008. 1060.
- Botha SJ, Sturm WA. Community Based Training in a Primary Health Care Model (CBTPHCM) Five year Plan, Kwazulu-natal provincial department of health/University of Kwazulu-natal college of health sciences, n.d, Available Online http://www.chs.ukzn.ac.za/CBTPHCM/FiveYearPlan.aspx
- Hagemeister DT, Pal A, Naidoo N, Kristen U, Mokgosana N, Joubert G. Undergraduate medical students’ interest in specialising in Family Medicine at the University of the Free State, 2014. S Afr Fam Pract. 2017;59(5):166–71. doi: 10.1080/20786190.2017.1317977
- Ozcakir A, Yaphe J, Ercan I. Perceptions of family medicine and career choice among first year medical students: a cross-sectional survey in a Turkish medical school. Collegium Antropol. 2007;31:595–600.
- Hayes BW, Shakya R. Career choices and what influences Nepali medical students and young doctors: a cross-sectional study. Hum Resour Health. 2013;11(1):1083. doi: 10.1186/1478-4491-11-5
- Amin M, Chande S, Park S, Rosenthal J, Jones M. Do primary care placements influence career choice: what is the evidence? Education for primary care: an official publication of the association of course organisers, national association of GP Tutors. World Organ Fam Doct. 2018;29(2):64–7.
- Von Pressentin KB, Mash RJ, Baldwin-Ragaven L, Botha RPG, Govender I, Steinberg WJ. The bird’s-eye perspective: how do district health managers experience the impact of family physicians within the South African district health system? A qualitative study. S Afr Fam Pract. 2018;60(1):13–20. doi: 10.1080/20786190.2017.1348047
- von Pressentin KB, Mash RJ, Baldwin-Ragaven L, Botha RPG, Govender I, Steinberg WJ, et al. The perceived impact of family physicians on the district health system in South Africa: a cross-sectional survey. BMC Fam Pract. 2018;19(1):24. doi: 10.1186/s12875-018-0710-0
- Knight ES, Ross JA, Mahomed O. Developing primary health care and public health competencies in undergraduate medical students. S Afr Fam Pract. 2017;59(3):103–9. doi: 10.1080/20786190.2016.1272229
- Essuman A, Anthony-Krueger C, Ndanu TA. Perceptions of medical students about family medicine in Ghana. Ghana Med J. 2013;47(4):178–84.
- Strachan B, Zabow T, van der Spuy ZM. More doctors and dentists are needed in South Africa. S Afr Med J. 2011;101:523–528.
- Frambach JM, Manuel BAF, Fumo AMT, Van der Vleuten CPM, Driessen EW. Students’ and junior doctors’ preparedness for the reality of practice in sub-Saharan Africa. Med Teach. 2015 Jan;37(1):64–73. doi: 10.3109/0142159X.2014.920490