ABSTRACT
Introduction: Dyspepsia is a symptom complex with varied underlying etiologies. The underlying etiology determines the precise treatment and prognosis though Helicobacter pylori infection plays a central role. The aim of this study was to describe the spectrum and pattern of distribution of findings in patients with dyspepsia undergoing oesophago-gastro-duodenoscopy at the University College Hospital, Ibadan.
Methods: A retrospective analysis of computerized database patients with dyspepsia who underwent oesophago-gastro–duodenoscopy from 2015 to 2019.
Results: A total of 1,373 procedures were done and dyspepsia was the indication in 736 (53.2%) comprising 317 (43.1%) male and 405 (55%) female (P< .001). The age ranged from 18 to 100 with a mean of 50 ± 15 years. The age group 40–59 years had the highest representation (P = .00). The esophageal mucosa was normal in 592 (80.4%) while 45 (6.1%) and 36 (4.9%) patients had esophagitis and esophageal candidiasis, respectively. In the stomach, 230 (31%) patients had normal mucosa while 433 (57.5%) and 40 (5.4%) patients had gastritis and gastric ulcers, respectively. Antrum was the most commonly involved site by the gastritis and ulcers in 236 (55.8%) and 24 (60%) patients, respectively. The mean age of those with non-ulcer dyspepsia was 49.8 ± 15 while that of those with organic dyspepsia was 55.7 ± 13.7 years (P= .01). Furthermore, there was a significant correlation between the age group and organic dyspepsia (P = .00). The first part of the duodenum was normal in 594 (80.7%) while bulbar duodenitis was seen in 106 (14.4%).
Conclusion: In our practice, OGD in patients with dyspepsia is either normal or yielded few abnormalities. The most common abnormalities were gastritis, duodenitis, esophagitis and gastric ulcers. Gastritis and ulcers were antral predominant and gastric ulcers were more common than duodenal ulcers. There was a significant relationship between increasing age and organic dyspepsia.
1. Introduction
Dyspepsia was originally defined as any symptom referable to the upper gastrointestinal tract (UGIT) [Citation1]. Heart burns and regurgitation were later removed from the constellation of symptoms of dyspepsia because they were thought to be specific for gastroesophageal reflux disease (GERD) [Citation2]. American College of Gastroenterology defines dyspepsia as persistent epigastric pain lasting for at least a month with or without other symptoms of UGIT [Citation3]. Thus, dyspepsia is now considered as a constellation of persistent symptoms referable to the gastro-duodenal region and these constellation may include epigastric pain, indigestion, bloating, epigastric discomfort, early satiation, epigastric burning among other subjective descriptions [Citation4,Citation5].
Dyspepsia is a common reason for patients to visit the general practitioners, family physicians and Gastroenterologists worldwide. The global prevalence of dyspepsia was found to be 20% in a meta-analysis [Citation6]. A community survey of dyspepsia in Plateau state, North central, Nigeria reported a prevalence of 45% [Citation7]. Another study among the students of a tertiary institution in Lagos, Nigeria reported a prevalence of 64% [Citation8]. Delayed meals, cigarette smoking, use of NSAID and consumption of garlic were found to be associated with dyspepsia in the study. A community-based survey of dyspepsia in North eastern Nigeria reported prevalence of 26% and 6% among adults and teenagers, respectively, [Citation9]. This study also found intake of alcohol and kola to be associated with dyspepsia. The wide difference in the prevalence of dyspepsia in these studies is not surprising because of their different definitions of dyspepsia which reflect the heterogeneity of the syndrome itself. Apart from the medical complications of the specific etiology, if any, it has been reported that dyspepsia reduces the quality of life and increases both direct and indirect health cost [Citation10].
The spectrum of etiology of dyspepsia is wide and this includes functional dyspepsia, gastritis, gastric ulcer, gastric cancer, duodenitis, duodenal ulcer, duodenal cancer, gastro-duodenal polyps etc. Although Helicobacter (H) pylori infection has a central role in the etiology of dyspepsia to a large extent, it is the specific treatment and prognosis depend on the specific etiology. Oesophago-gastro-duodenoscopy (OGD) though may not be cost effective in all patients with dyspepsia, it is the most accurate modality of determining the precise cause (s) of dyspepsia.
The aim of this study was to describe the spectrum and pattern of distribution of findings in patients with dyspepsia undergoing OGD at the University College Hospital (UCH), Ibadan, Nigeria.
2. Patients and methods
Study design: A 5-year retrospective analysis of computerized data of patients with dyspepsia who had OGD between January 1, 2015 and December 31, 2019.
Study site: The study was carried out at the endoscopy suite of UCH, Ibadan, Nigeria. UCH, Ibadan is the Nigerian Premier University Hospital established 62 years ago with 1000 in patients’ beds. The endoscopy suite has two functioning procedure rooms equipped with EVIS EXERA 111 Olympus video-endoscopy system since 2012. Scheduled OGD were done 3 days in a week for both outpatients and in patients while emergencies are done every day. Patients were referred for OGD from different clinics within and outside UCH. Referrals for endoscopy are also received from neighboring states of Ogun, Ondo and Osun states. The Endoscopy unit had Seven Consultant Medical and Surgical Gastroenterologists who have experience in gastrointestinal endoscopy spanning between 5 and 31 years. A pre-endoscopy assessment was done for all the patients to ascertain the indication for the procedure, ensure there was no contraindication(s) and obtain an informed written consent. The usual premedication was 10% xylocaine pharyngeal spray with or without intravenous midazolam depending on the preference of the Endoscopist and the patients’ comorbidities. Occasionally, ketamine and/or propofol was used for patients with history of allergy to xylocaine, very anxious patients, or those who preferred deep sedation despite adequate counseling that the procedure is usually done with conscious sedation. Each patient’s report was generated after the procedure and an electronic copy was stored in the desktop computer in each of the procedure room.
2.1. Data collection
The OGD reports of all the patients aged 18 years and above carried out from January 1, 2015 to December 31, 2019 were retrieved from the computer database. The investigators went through all the reports one after the other. Age, sex, indication, year of the procedure and the Consultant who performed the procedure were retrieved from the report. The following indications were taken as dyspepsia: Dyspepsia, epigastric pain, upper abdominal pain, indigestion, upper abdominal bloating. The findings in each report were classified into esophageal, gastric and duodenal. The findings in the esophagus and duodenum were further classified into normal and abnormal findings and those of the stomach into non-ulcer dyspepsia (normal findings and gastritis) and organic dyspepsia (other gastric findings). Patients that had multiple procedures for whatever reason (s) were analyzed just once.
The study was done in strict compliance to the Helsinki’s declaration of 2008 (11). Identifiers like name and address of the patients were not retrieved from their reports to ensure confidentiality.
2.2. Statistics
The data were analyzed with SPSS version 23. Categorical data were summarized using frequency tables while age was summarized with mean, median and mode. Chi square and student t test were used to test for significance among the categorical and continuous variables, respectively. variables. Multivariate correlation was done for age and significant endoscopic findings. Value of p < 0.05 was considered significant.
3. Results
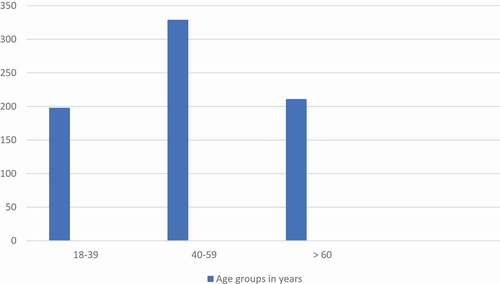
A total of 1,373 patients aged 18 to 100 years had OGD in the specified period. Dyspepsia was the indication in 736 (53.2%) patients. Twenty-one (2.9%) of the patients had a second indication out of which 11 (1.5%) were esophageal related symptoms of heartburns, regurgitation, dysphagia, odynophagia and globus pharygeus. Of those 736 patients, 317 (43.1%) were male while 405 (55%) were female (P < .001), gender of 14 (1.9%) patients were missing. The mean age was 50 ± 15 years while median and mode were 50 and 39 years, respectively. shows the distribution of the patients into different age groups. In 592 (80.4%) of the patients, esophageal mucosa was normal while 45 (6.1%) patients and 36 (4.9%) patients had esophagitis and esophageal candidiasis, respectively ().
Table 1. Spectrum and frequencies of findings among patients with dyspepsia who underwent oesophago-gastro-duodenoscopy
Figure 1. Age group distribution of patients with dyspepsia who underwent oesophago-gastro-duodenoscopy
In the stomach, 230 (31%) of the patients had normal mucosa while 433 (57.5%), 40 (5.4%), 16 (2.2%) of the patients had gastritis, gastric ulcer and gastric polyps, respectively. Only 9 (1.2%) had gastric mass suspected to be malignant. Classifying the gastric findings into two, 663 (88.5%) had non-ulcer dyspepsia (normal findings and gastritis) while 73 (11.5%) had organic dyspepsia. The mean age of those with non-ulcer dyspepsia was 49.8 ± 15 years while that of those with organic dyspepsia was 55.7 ± 13.7 years (P= .01). Also, 38 (22.5%) patients among those that were 60 years and above had organic dyspepsia as against 9 (5.1%) patient among those that were aged between 18 and 39 years (P = .00). There was a significant correlation between the age groups and organic dyspepsia (P = .00). Considering the gender, 46 (6.5%) females and 36 (5.1%) males had organic dyspepsia (P= 0.87) ()
Table 2. Relationship between the demographic parameters of the patients and the findings in the different parts of the upper gastrointestinal tracts
In patients with gastritis, antrum was involved in 236 (55.8%), while the body, fundus and cardia were involved in 211 (49.9%), 169 (40%) and 143 (33.8%) respectively. In patients with gastric ulcers, antrum was involved in 24 (60%) patients while the body, cardia, fundus and incisura were involved in 17 (42.5%), 5 (12.5%), 3 (7.5%) and 1 (2.5%) respectively. In the duodenum, the first part was normal in 594 (80.7%) while the second part was normal in 715 (97.1%) patients. Duodenitis was seen in 106 (14.4%) patients involving the first part and in 11 (1.5%) involving the second part of the duodenum ().
4. Discussion
The most common indication for OGD in Ibadan was dyspepsia, similar to findings of studies from other parts of Nigeria and the world [Citation11–13]. There were significantly more females with dyspepsia than male. A meta-analysis of 100 studies involving 312, 415 subjects concluded that un-investigated dyspepsia was more common in women [Citation6]. Functional gastrointestinal disorders including functional dyspepsia are also more common in women [Citation14]. Moreover, the health seeking behavior in women is better than men despite that they have lesser economic power [Citation15–17]. The peak age of patients with dyspepsia in this study was 40– 59 years, similar to 40–54 and 50–59 years found in studies among patients with dyspepsia in Canada and Japan, respectively, [Citation18,Citation19].
It is not surprising that majority of the patients had normal finding in the esophagus. Rome 111 criteria for functional bowel disorders have separated predominately reflux symptoms of heartburns and regurgitation from dyspepsia [Citation2]. However, about 20% of the patients had findings in the esophagus and the major finding was esophagitis. This is not surprising as patients may have overlap of dyspepsia and reflux symptoms. About 1.5% of our patients had esophageal related symptoms as the second indications for the OGD. Moreover, epigastric pain which is part of the dyspepsia complex has also been found to be a symptom of GERD [Citation20]. It is also possible that these esophageal findings were either asymptomatic or not bothersome to the patients. About 37% of patients with erosive esophagitis on OGD had no symptom of GERD in a study [Citation21]. In another study among the Brazilians, 18% of the patients with dyspepsia had features suggestive of GERD on OGD [Citation22]. Two Studies from United States of America and Nigeria reported that 5.4% and 8.1% of patients with dyspepsia had esophagitis on OGD, respectively, [Citation23,Citation24].
The most common finding in the stomach was gastritis followed by normal gastric mucosa. This finding is similar to that of Faintuch et al. [Citation22] who found gastritis and normal gastric mucosa in 46% and 20%, respectively, of their patients with dyspepsia in a south American tertiary hospital like ours. It is also similar to the report from Benin, Nigeria where gastritis and normal gastric mucosa accounted for 46% and 15% respectively [Citation25]. However, a study in the US, reported normal gastric mucosa in 51% while gastritis was seen only in 30% [Citation23]. The difference between a normal gastric mucosa and mild gastritis could be subtle, subjective and may depend on the resolution of the gastroscopy used. Furthermore, both normal gastric findings and gastritis are classified as non-ulcer dyspepsia since there is a poor correlation between gastritis and symptoms of dyspepsia [Citation26]. A study among healthy volunteers reported histological gastritis in 36% of the asymptomatic patients [Citation27]. There was a significant relationship between age of the patients and finding of organic dyspepsia. Similar studies in the US and Egypt also found increasing age to be associated with significant endoscopic finding in patients with dyspepsia [Citation23,Citation28]. Chronic illnesses like liver cirrhosis, chronic kidney diseases and others that are risk factors for peptic ulcer disease tend to occur with increasing age. Moreover, many elderly people may have to be on ulcer prone medications like non-steroidal anti-inflammatory drugs, alendronates for various reasons including arthritis, osteoporosis and anti-platelet activities.
Both gastritis and gastric ulcers involved the antrum more than any other parts of the stomach. Ndububa et al. [Citation26] reported a similar pattern among Nigerian patients with dyspepsia. It is also similar to the pattern found among American patients with non-ulcer dyspepsia with H. pylori infection [Citation29]. The pattern and degree of inflammation of the gastric mucosa by H. pylori determines the type of biochemical and clinical outcome of the gastroduodenal disease. H. pylori associated gastritis tends to be more pronounced in the antrum than the corpus which is relatively resistant to the infection [Citation30]. Antral predominant gastritis is associated with hypergastrinemia, increased gastric acidity, distal gastric cancer and duodenal ulcer [Citation31]. Many studies have shown the preponderance of H. pylori infection in our population generally and among our patients with dyspepsia in particular [Citation24,Citation32,Citation33].
However, gastric ulcers occurred more than duodenal ulcers among our cohort despite the antral predominance of the gastritis. A study in Atlanta, Georgia also found gastric ulcers more than duodenal ulcers among their patients with dyspepsia [Citation29]. Similarly, Jemilohun et al. [Citation24] in Ibadan, Odeghe et al. [Citation34], in Lagos, Ugiagbe et al. [Citation25], in Benin, all in Nigeria and Agyei-Nkansah et al. [Citation11], in Ghana found gastric ulcers to be more common in patients with dyspepsia though these studies did not look at the pattern of the gastritis in their cohorts. However, other studies in Nigeria and Brazil reported duodenal ulcers to be more common than gastric ulcers [Citation22,Citation26,Citation35]. In a study at Ife in 2016, Ndububa et el [Citation26] noted that even though duodenal ulcer was more common than gastric ulcer, there was a 50% reduction in the prevalence of duodenal ulcer when compared with a study done at the same center a decade earlier [Citation26]. Similarly, in Cameroon, West Africa the frequency of pyloro-duodenal ulcer among patients undergoing OGD reduced from 32.8% in 1990 to 12.9% in 2015 while that of gastric ulcer increased from 1.5% to 10.5% over the same period [Citation36]. A similar story was told in Zambia [Citation37]. In fact, most of the studies which reported predominance of duodenal ulcers were earlier in date than those that reported the reverse. A possible explanation for this transition is the widespread availability and use of H. pylori eradication regimens which patients take on their own sometimes even before presenting in the hospital, since they are widely available over the counter in our environment. Additionally, the ubiquitous use of non-steroidal anti-inflammatory drugs and anti-platelets could be responsible for the relative rise in gastric ulcers.
The frequency of gastric masses suspected to be malignant and indeed significant endoscopic lesions was low even in the elderly in this study, despite the frequency of H. pylori infection in the population. Many other studies in Nigeria and overseas have reported similar findings [Citation22,Citation24,Citation25,Citation34]. We know, however, that the outcome of H. pylori infection is an interaction of the virulence of the organism which is determined by its strains, host susceptibility and environmental factors [Citation38]. This shows that test and treat approach for dyspepsia should be encouraged in our population more so that the insurance coverage is poor and most patients pay out-of-pocket for the procedure. This will ensure judicious use of the patients’ resource and prevent unnecessary burden on the endoscopy facilities which are still largely restricted to the tertiary hospitals in Nigeria.
This study is not without limitations. Firstly, being a retrospective study, we did not take into account whether or not the OGD was done when the patient was still symptomatic. The practice in our unit is to scheduled endoscopy except in emergencies. Some lesions might have healed at the time of the endoscopy especially if patients were on medications which was the case, most times. This might have affected our results, though to a little extent, in our opinion since ours is not a high-volume center and most appointments are within a week. Furthermore, there was no information on the medical, medication, social history and Helicobacter pylori status of the patients which could also affect the spectrum of findings in dyspeptic patients, at least to some extent. Lastly, our data reflected only those whose were either on health insurance that reimbursed the cost of the endoscopy or were able to pay out-of-pockets meaning that some cases with dyspepsia who could not afford the cost of the procedure and were not on health insurance would have been left out of our data though we considered this would not have changed the data considerably.
In conclusion, among patients with dyspepsia who underwent OGD in Ibadan, majority had normal esophageal and duodenal mucosa while about a third had normal gastric mucosa. Among those with abnormal findings, the most common lesions are esophagitis, gastritis and duodenitis in the esophagus, stomach and duodenum, respectively. Furthermore, duodenal ulcers were more common than gastric ulcers. Gastritis and gastric ulcers were found more commonly in the antrum than other parts of the stomach. A significant relationship was found between increasing age and organic dyspepsia.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Kolawole Oluseyi Akande
Kolawole Oluseyi Akande is a Senior Lecturer in the Department of Medicine, College of Medicine, University of Ibadan. Kolawole’s research interest is in Hepatitis and its effects on the liver especially hepatocellular carcinoma.
Temitope Olufemi Oke
Temitope Olufemi Oke is a Consultant Physician in the Department of Medicine, University College Hospital, Ibadan. Tope has research interest in gastrointestinal oncology.
Oludolapo Afuwape
Oludolape Afuwape is a Senior Lecturer in the Department of Surgery. His research interest is in surgical gastroenterology especially rectal diseases.
Tinuola Abiodun Adigun
Tinuola Abiodun Adigun is a Senior Lecturer in Anaesthesia and has reserch interest in anaesthesia in GI procedures especially diagnostic and therapeutic digestive endoscopy.
Adegboyega Akere
Adegboyega Akere is a Senior Lecturer in Medicine with clinical and research interest in digestive endoscopy.
Ajibola Aje
Ajibola Aje is a special grade I consultant Physician in the Department of Medicine, University College Hospital with clinical and research interest in GI emergencies.
Samuel Olawale Ola
Samuel Olawale Ola is a Professor of Medicine in the College of Medicine, University of Ibadan with research interest in hepatitis.
Jesse Abiodun Otegbayo
Jesse Abiodun Otegbayo is a professor of Medicine in the College of Medicine, University of Ibadan and has research interest in GI and hepatic malignancies especially tumour markers for liver cancers.
References
- Colin-Jones DG, Bloom B, Bodemar G, et al. Management of dyspepsia: report of a working party. Lancet. 1988 Mar 12;331(8585):576–579.
- Klauser AG, Schindlbeck NE, Müller-Ler SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990 Jan 27;335(8683):205–208.
- Moayyedi PM, Lacy BE, Andrews CN, et al. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol. 2017 Jul;112(7):988–1013.
- Stanghellini V, Chan FKL, Hasler WL, et al. Gastroduodenal disorders. Gastroenterology 2016 May;150(6):1380–1392.
- Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006 Apr;130(5):1466–1479.
- Ford AC, Marwaha A, Sood R, et al. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut 2015 Jul;64(7):1049–1057.
- Ihezue CH, Oluwole FS, Onuminya JE, et al. Dyspepsias among the highlanders of Nigeria: an epidemiological survey. Afr J Med Med Sci. 1996 Mar 1;25(1):23–29.
- Omar J, Sholeye O. Prevalence and risk factors for dyspepsia among undergraduate students of a tertiary institution in Lagos, Nigeria. Adv Nutr. 2017 Jan 1;8(1): 21–21.
- Holcombe C, Omotara BA, Padonu MK, et al. The prevalence of symptoms of dyspepsia in north eastern Nigeria. A random community based survey. Trop Geogr Med. 1991 Apr;43(1–2):209–214.
- Nyrén O, Lindberg G, Lindström E, et al. Economic costs of functional dyspepsia. Pharmacoeconomics. 1992 May 1;1(5):312–324.
- Agyei-Nkansah A, Duah A, Alfonso M. Indications and findings of upper gastrointestinal endoscopy in patients presenting to a District Hospital, Ghana. Pan Afr Med J [Internet]. 2019 Nov;34(82).
- Aljebreen AM, Alswat K, Almadi MA. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy system. Saudi J Gastroenterol. 2013 Sep 1;19(5):219.
- Ismaila BO, Misauno MA. Gastrointestinal endoscopy in Nigeria - a prospective two year audit. Pan Afr Med J. 2013 Jan 15. DOI:https://doi.org/10.11604/pamj.2013.14.22.1865.
- Koloski NA, Talley NJ, Boyce PM. Epidemiology and health care seeking in the functional GI disorders: a population-based study. Am J Gastroenterol. 2002 Sep;97(9):2290–2299.
- Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016 Mar 31;17(1):38.
- Tenenbaum A, Nordeman L, Sunnerhagen KS, et al. Gender differences in care-seeking behavior and healthcare consumption immediately after whiplash trauma. PLoS One [Internet]. 2017 Apr 25;12(4). doi:https://doi.org/10.1371/journal.pone.0176328.
- Ortiz-Ospina E, Roser M Economic inequality by gender. Our World in Data [Internet]. 2018 Mar 21 [cited 2020 Mar 26]; Available from: https://ourworldindata.org/economic-inequality-by-gender
- Tougas G, Chen Y, Hwang P, et al. Prevalence and impact of upper gastrointestinal symptoms in the Canadian population: findings from the DIGEST study. Domestic/international gastroenterology surveillance study. Am J Gastroenterol. 1999 Oct;94(10):2845–2854.
- Hirakawa K, Adachi K, Amano K, et al. Prevalence of non-ulcer dyspepsia in the Japanese population. J Gastroenterol Hepatol. 1999 Nov;14(11):1083–1087.
- Vakil N, Van Zanten SV, Kahrilas P, et al., Global Consensus Group.The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006 Aug;101(8):1900–1920. quiz 1943..
- Ronkainen J, Aro P, Storskrubb T, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005 Feb 1;40(3):275–285.
- Faintuch JJ, Silva FM, Navarro-Rodriguez T, et al. Endoscopic findings in uninvestigated dyspepsia. BMC Gastroenterol. 2014 Feb 6;14(1):19.
- Abdeljawad K, Wehbeh A, Qayed E. Low prevalence of clinically significant endoscopic findings in outpatients with dyspepsia [Internet]. Vol. 2017. Hindawi: Gastroenterology Research and Practice; 2017.
- Jemilohun AC, Otegbayo JA, Ola SO, et al. Prevalence of Helicobacter pylori among Nigerian patients with dyspepsia in Ibadan. Pan Afr Med J [Internet]. 2010;6(1).
- Ugiagbe RA, Omuemu CE. Non-ulcer dyspepsia: an endoscopic review. Afr J Med Health Sci. 2013;12(1):6–9.
- Ndububa DA, Adekanle O, Omonisi AE. et al. Pattern of gastritis and Helicobacter pylori colonization of the stomach in Nigerian patients with dyspepsia. Niger J Gastroenterol Hepatol. 2016;8(2):81–88.
- Kreuning J, Bosman FT, Kuiper G, et al. Gastric and duodenal mucosa in “healthy” individuals. An endoscopic and histopathological study of 50 volunteers. J Clin Pathol. 1978 Jan;31(1):69–77.
- Gado A, Ebeid B, Abdelmohsen A, et al. Endoscopic evaluation of patients with dyspepsia in a secondary referral hospital in Egypt. Alexandria J Med. 2015 Sep 1;51(3):179–184.
- Vakil N, Talley NJ, Stolte M, et al. Patterns of gastritis and the effect of eradicating Helicobacter pylori on gastro-oesophageal reflux disease in Western patients with non-ulcer dyspepsia. Aliment Pharmacol Ther. 2006;24(1):55–63.
- Dixon MF. Pathology of gastritis and peptic ulceration. In: Mobley HL, Mendz GL, Hazell SL, editors. Helicobacter pylori: physiology and genetics [Internet]. Washington (DC): ASM Press; 2001.
- El-omar EM, Penman ID, Ardill JE, et al. Helicobacter pylori infection and abnormalities of acid secretion in patients with duodenal ulcer disease. Gastroenterology. 1995 Sep;109(3):681–691.
- Olokoba A, Gashau W, Bwala S, et al. Helicobacter pylori infection in Nigerians with dyspepsia. Ghana Med J. 2013 Jun;47(2):79–81.
- Bello AK, Umar AB, Borodo MM. Prevalence and risk factors for helicobacter pylori infection in gastroduodenal diseases in Kano, Nigeria. Afr J Med Health Sci. 2018;17(1):41–46.
- Odeghe EA, Adeniyi OF, Oyeleke GK, et al. Use of alarm features in predicting significant endoscopic findings in Nigerian patients with dyspepsia. Pan Afr Med J [Internet]. 2019 Feb;34(66). doi: https://doi.org/10.11604/pamj.2019.34.66.18848.
- Misauno MA, Lsmaila BO, Usman BD, et al. Spectrum of endoscopically diagnosed upper gastrointestinal diseases in Jos. Sahel Med J. 2011 Apr 1;14(2):63.
- Kamdem J, Palmer D, Barrier C, et al. Diagnostic yield of gastrointestinal endoscopy in North West Region Cameroon and trends in diagnosis over time. Pan Afr Med J [Internet]. 2018 Mar 27;29. doi:https://doi.org/10.11604/pamj.2018.29.178.10785.
- Kayamba V, Sinkala E, Mwanamakondo S, et al. Trends in upper gastrointestinal diagnosis over four decades in Lusaka, Zambia: a retrospective analysis of endoscopic findings. BMC Gastroenterol. 2015 Oct 6;15(1):127.
- Atherton JC. The clinical relevance of strain types of Helicobacter pylori. Gut 1997 Jun;40(6):701–703.
