?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
Tubal disease is the leading cause of female infertility in the West African sub-region and hysterosalpingography (HSG) is the first-line imaging technique in its assessment. HSG is an acutely painful procedure. Various studies on analgesia for HSG were inconclusive. We compared the efficacy of 10 mg lidocaine 10% spray and 50 mg oral diclofenac sodium for pain relief during HSG.
Methods
This randomized clinical trial was carried out at the Department of Obstetrics and Gynecology, Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC) Ile-Ife, Nigeria between December 2019 and December 2021, among one hundred and eight eligible women undergoing HSG as part of their infertility workup. Ethical clearance was obtained from the ethics committee of the hospital with Protocol number ERC/2019/01/14. They were randomized into two groups. One group of 54 patients received 10 mg of 10% lidocaine spray and an oral placebo, while the second group of 54 women had 50 mg of oral diclofenac sodium and normal saline spray. Pain scores were assessed using a 10 cm visual analog scale at cervical traction, instillation of contrast media, and thirty minutes after HSG. The mean pain scores, the need for additional analgesia, and the occurrence of adverse drug reactions were compared between the two groups.
Result
Those in the oral diclofenac group had significantly lower pain scores than the 10% Lidocaine group 30 minutes after HSG; 1.13 ± 1.06 Vs. 2.04 ± 1.26 (p < 0.001). The additional analgesic requirement also showed no statistically significant difference between the two groups.
Conclusion
This study showed that oral diclofenac sodium is comparable to lidocaine spray for pain relief during HSG. It also has the additional benefit of improved quality of life 30 mins after HSG as evidenced by effective pain relief. Consideration should be given to the use of oral diclofenac sodium for pain relief during and after HSG in well-selected patients.
1. Introduction
Infertility is defined as the inability of a couple to conceive within a certain period, usually one year despite adequate unprotected sexual intercourse [Citation1]. It affects more than 80 million people worldwide. The prevalence of infertility is particularly high in sub-Saharan Africa, varying from 20–46% in some parts of West Africa, where up to 65% of gynecological consultations are for infertility [Citation2].
In Africa infertility is considered a stigma and a major public health problem that can cause great family problems, marital instability, and suicidal tendencies [Citation3]. It also has devastating psychological consequences on the affected couples, especially in Africa. The childless couples suffer from the conflux of personal, interpersonal, social, and religious expectations thus bringing a sense of failure to them [Citation3].
Tubal disease following pelvic inflammatory disease (PID), usually due to Neisseria gonorrhea and Chlamydia trachomatis is the commonest cause of female infertility in sub-Saharan Africa [Citation4]. Hysterosalpingography is the primary investigation of choice in assessing the morphology of the cervix, uterus, and fallopian tubes in infertile women [Citation5]. Gynecologists rely heavily on the information provided by hysterosalpingography in the evaluation of infertility. This procedure falls within the domain of both the gynecologist and radiologist. In the United State, 55% of hysterosalpingograms are obtained by the radiologists and gynecologists working together [Citation6]. Either the balloon catheter or tenaculum cannula technique can be used. The major advantages of hysterosalpingography are its cost-effectiveness and outpatient nature.
The procedure of hysterosalpingography is associated with pain which is its major disadvantage. About 85% of patients who undergo this procedure reported pain, with half complaining of moderate to severe pain [Citation7]. The application of tenaculum and cervical traction is the most painful of the procedure [Citation7]. Jayeola et al, on the contrary, stated that the peak of the pain is at the instillation of contrast medium [Citation8]. The pain can hurt the patient’s ability to cooperate during the procedure as well as her willingness to undertake other diagnostic studies.
The pain from the cervix and lower portion of the uterus is carried by the pelvic splanchnic nerve (parasympathetic S2, S3, and S4) whereas pain from the fundus and the body of the uterus is conducted via the hypogastric nerves to the lower thoracic segment (T11 – T12) [Citation9].
The perception of pain varies from individual to individual and also varies at different times and parts for the same individual [Citation9]. Thus, pain perception is subjective and this led to various instruments to objectively measure pain perception. These include the Visual Analog Scale (VAS) [Citation10] Numerical Rating Scale (NRS), Simple Descriptive Scale (SDS), and Verbal Rating Scale (VRS) [Citation11].
The most commonly used scale is the visual analog scale. A change in the VAS score represents a relative change in the magnitude of pain sensation. Use of the vas in comparative analgesic trials can now meaningfully quantify differences in potency and efficacy [Citation10]. For this study, visual analog scale (vas) was used to assess the pain score because it is more objective, easy to understand, and administered.
A postal survey was conducted in the United Kingdom to evaluate the current clinical practice regarding the methods used to provide pain relief during hysterosalpingography [Citation12]. Respondents in the survey expressed different opinions with regards to the timing, and the nature of analgesia used, and interestingly 38% of respondents did not use analgesia at all [Citation12]. This variation in clinical practice may reflect the scarcity of evidence contained within the literature.
The various interventions that have been tried include paracetamol, Naproxen Sodium versus intrauterine lignocaine, topical analgesics, and paracervical block with local anesthetics [Citation7,Citation8] but the search for an ideal analgesic that provides adequate pain relief during hysterosalpingography continues.
Lidocaine hydrochloride spray has been used on oral mucosa in dental analgesia and found to be safe and effective. Karasahin et al have shown that lidocaine spray is a practical and effective analgesic for decreasing pain scores during hysterosalpingography [Citation13]. Theoretically, oral diclofenac sodium is expected to reduce pain perception at cervical instrumentation, uterine distention, and peritoneal irritation by contrast medium. Based on their mechanisms of action both the oral diclofenac sodium and lidocaine 10% spray would seem to be logical choices for analgesia during hysterosalpingography. Non-steroidal anti-inflammatory drugs have been used singly [Citation8] or in combination with topical analgesics (Xylocaine spray) as preoperative premedication for hysterosalpingography in a previous study [Citation12]. Analgesia is not routinely used for hysterosalpingography in this institution. There is a paucity of local studies on this subject matter in the literature as most of the pieces of evidence so far are from developed countries. The findings from this study may change the practice of analgesia usage during hysterosalpingography in our institutions. A woman being evaluated for infertility is already carrying a very heavy physical, mental, psychological, and emotional burden. Adequate pain relief during hysterosalpingography which is a first step in the infertility workup will be a welcome development.
2. Material and methods
2.1. Study location
This study was conducted at the Department of Obstetrics and Gynecology of the Obafemi Awolowo University Teaching Hospital Ile-Ife, Osun State. Nigeria between December 2019 and December 2021
2.2. Study design
A double-blind randomized controlled study.
2.3. Inclusion criteria
All women who presented for hysterosalpingography in these two hospital units as part of their infertility workup were counseled about this study and written informed consent was obtained from each willing participant.
2.4. Exclusion criteria
Women with any history of allergy to local anesthetics, radio-opaque dye, non-steroidal anti-inflammatory medications, acute pelvic inflammatory disease, vaginal discharge (known to exacerbate and flare-up following hysterosalpingography), cervical stenosis, chronic pelvic pain, patients are on any form of analgesic and those who refuse to participate were excluded from the study.
2.5. Research hypotheses (null hypotheses)
There is no significant difference in analgesic efficacy between lidocaine 10% spray and oral diclofenac sodium for pain relief during hysterosalpingography.
There is no significant difference in the tolerability of lidocaine 10% spray and oral diclofenac sodium for pain relief during hysterosalpingography.
2.6. The alternative hypotheses
There is a significant difference in analgesic efficacy between lidocaine 10% spray and oral diclofenac sodium for pain relief during hysterosalpingography.
There is a significant difference in the tolerability of lidocaine 10% spray and oral diclofenac sodium for pain relief during hysterosalpingography.
2.7. Sample size determination
The mean difference in the VAS pain score (µ1- µ0) from previous study [Citation14] was (4.9–3.3) = 1.6, with an α-error of 5% and the power of study set at 80%. The minimum sample size to detect any statistically significant difference was calculated using this formula
Where (µ1- µ0) = 1.6
u= Power of the study, 80% = 0.84
v= level of significance of 5% (two-sided tail) = 1.96
δ1= standard deviation for the first group = 2.7
δ2= standard deviation for the second group = 2.9
µ1-µ0= expected difference between the means which will be a VAS score of 1.6 for this study
Number of patient expected to drop out of the study
The minimum sample size was 54 patients for each group. A total of 108 patients were required for this study. Attrition rate of 10% was used making a total of 120 patients with 60 patients in each group.
2.8. Training
Before the commencement of this study, a training session was organized by the researcher for the resident doctors and other health personnel that was involved in this study in these two hospitals. A protocol detailing the aims and methodology of the study was discussed exhaustively and any ambiguity was clarified.
2.9. Study procedure
All the eligible patients were educated about the study and written informed consent was obtained. The patients were also educated about the use of a visual analog scale which was the tool for measurement of the primary outcome of interest in this study. All cannulation and injection of the contrast medium were done by the principal investigator in the course of this study. Positioning of the patients on fluoroscopy table and directive about the timing of the x-rays were done by a Senior Registrar from the Department of Radiology, Obafemi Awolowo University Teaching Hospital Complex Ile Ife. Two research assistants were employed for the enrollment of the patients and the measurement of the pain scores.
Randomization was done in the Pharmacy department using a computer-generated random number table developed by an independent statistician. The study solution contained lidocaine 10% spray manufactured by Astra Zeneca the United Kingdom Limited, 600 Capacity Green Luton, United Kingdom, or 0.9% sodium chloride spray (normal saline) which was prepared by the pharmacy as its placebo. The lidocaine 10% spray and its placebo (normal saline spray) were contained in identical bottles without labels. Each of the spray bottles comes with a nozzle. To prevent cross-infection, a nozzle was used for a patient in a day. All the nozzles were sterilized by soaking them in 2% glutaraldehyde solution for 10 hours before use. The 50 mg oral diclofenac sodium capsule was manufactured by Drugfield Pharmaceutical limited, Lynson Chemical Avenue Kilometre 38, Lagos Abeokuta expressway Sango Ota, Nigeria. The placebo for oral diclofenac sodium capsule was capsules of diclofenac sodium manufactured by Drugfield limited but emptied and filled with lactose (placebo) in the pharmacy. The interventions given were kept inside sealed opaque envelopes. One set of envelopes contained Lidocaine 10% spray with placebo oral capsules. The second set of envelopes contained 50 mg of oral diclofenac sodium capsule and normal saline spray as a placebo. The investigators, the patients, and the outcome determiners were blinded to the intervention each patient received. The envelopes were identified only by the study number and a sequential envelope was used for each subsequent patient.
A research assistant collected the demographic data of the patients and enrolled the patients into the study by opening the envelope. He/she administered the capsule in each envelope which was either 50 mg diclofenac sodium or its placebo about 2 hours before the hysterosalpingography to the patients. The administration of this capsule was done by directly observed therapy to ensure 100% compliance. Each patient was positioned on the radiology fluoroscopy table by a senior registrar in the radiology department. The Principal investigator then placed the patient in the lithotomy position. The perineum was cleaned with 1% chlorhexidine solution. A bimanual pelvic examination was carried out by the principal investigator to determine the size and position of the uterus.
A bivalve Cusco’s speculum was inserted into the vagina and it was opened to expose the cervix. The cervix was cleaned with 1% chlorhexidine solution and dried. The spray solution from the patient’s envelope was applied to the cervix. After waiting for 3 minutes, the patient was asked if she felt any of the symptoms that may be attributable to the side effect of the drugs used (oral diclofenac sodium was expected to have attained its peak plasma concentration and this time also coincided with the onset of action of 10% lidocaine spray). The occurrence of side effects in either group was taken as a measure of tolerability. The cervix was grasped with a tenaculum at 12 O’clock or 6 O’clock position for an anteverted or retroverted uterus respectively. A Rubin HSG cannula was inserted into the cervical canal via the external cervical os. The speculum was removed and cervical traction was applied.
A water-soluble contrast medium (Urografin 76%) was injected slowly through the Rubin cannula. The uterine and tubal filling phase was watched carefully. The injection of the contrast medium was done under fluoroscopy guidance and appropriate X-rays were taken under the direction of the Radiology Senior Registrar.
Each patient was adequately counseled before the procedure and asked to make a mental note of her level of pain during cervical traction and contrast medium injection; the two painful steps of the procedure [Citation7,Citation8]. The patient was asked retrospectively to mark the pain scores at these two steps on the visual analog scale immediately after the procedure. The patient’s vital signs were monitored after the procedure. The pain score for delayed pain was marked on the visual analog scale by the patient 30 minutes after the procedure. Thereafter, the pain scores were measured on the visual analog scale regarding the distance on the scale by a research assistant. The patient was asked again if she was experiencing any symptoms that may be suggestive of possible side effects of these two drugs. Patients in both groups who experienced unbearable pain were given 30 mg of intramuscular pentazocine injection. The number of patients that required additional analgesics in both groups was compared and included in the final analysis. Patients that had pentazocine injections who were in the minority group were monitored in the observation room until they are fully awake before discharge. All patients were discharged in stable condition and were contacted on the mobile phone 24 hours after for any further adverse drug reactions.
2.10. Statistical analysis
Information obtained at the end of this study was processed using the computer software package, SPSS Version 16. Continuous variables were compared using the student t-test or Wilcoxon rank-sum test. Categorical variables were analyzed using chi-square or Fisher exact test. The level of significance was set at p < 0.05.
2.11. Ethical consideration
Ethical clearance was obtained for this study from the ethics and research committee of the Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife with Protocol number ERC/2012/09/14. All participants were fully informed about the study and reserved the right to voluntarily withdraw for whatever reasons at any stage of the study without penalty.
3. Results
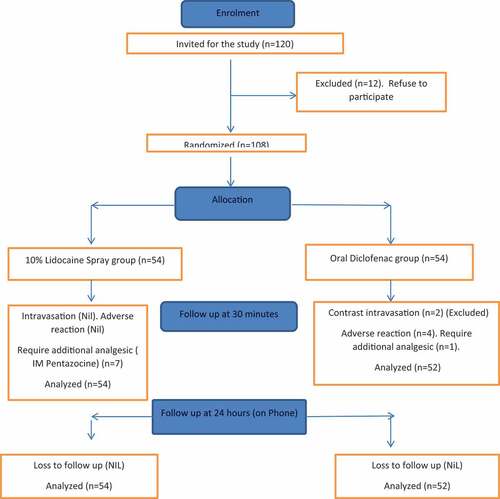
One hundred and twenty women undergoing the procedure of hysterosalpingography were recruited into the study. Twelve women were excluded because they refuse to participate in the study. One hundred and eight women were randomized into two groups (that is 54 women in each group) as shown in the flowchart in . Two women in the oral diclofenac sodium group had contrast intravasation thereby rendering their study inconclusive. They were excluded from the study leaving a total of 54 women in the Lidocaine 10% spray group and 52 women in the oral diclofenac group.
The age range in the Lidocaine group was 20–45 years with a mean of 34.43 ± 5.29 while that of Diclofenac was 19–44 years with a mean of 33.62 ± 5.91. This is not statistically significant (t = 0.744, p = 0.744). The mean parity of the Lidocaine group was 0.48 ± 0.81 while that of the Diclofenac was 0.65 ± 0.78 (t = 1.103; p = 0.459), which was not statistically significant.
Both groups were comparable in their sociodemographic characteristics. The majority of the study participants had tertiary education 50% and 53.8% in Lidocaine and Diclofenac groups respectively (p = 0.97)
Secondary infertility was commoner in the study groups, 72.2% and 80.8% in Lidocaine and Diclofenac groups respectively (p = 0.363) as shown in .
Table 1. Comparison of patients’ sociodemographic characteristics between the two study groups.
There was no statistically significant difference in both groups at cervical traction and instillation of contrast (p = 0.236 and 0.099 respectively). However, the pain score was significantly lower in the oral diclofenac than in the 10% Lidocaine group 30 minutes after HSG (<0.001).as shown in
Table 2. Comparison of pain scores between the two study groups.
The rate of adverse drug reaction (mainly gastrointestinal: nausea and vomiting) was more in the oral diclofenac group compared to the lidocaine group before the commencement of HSG 11.5% vs 0% (p-value = 0.012) but this was no longer statistically significant by 30 mins after HSG.
No incidence of adverse drug reaction was reported in both groups 24 hours after HSG as shown in .
Table 3. Comparison of adverse drug reactions between the study groups.
showed that there is significant difference in additional analgesic requirement (Intramuscular Pentazocine) between the two groups (13% in the Lidocaine group vs 1.9% in the Diclofenac group (exact = 0.060) 30 minutes after the procedure.
Table 4. Additional analgesic requirement per group (30 minutes after the PROCDURE).
4. Discussion
In Africa, infertility is considered a stigma and a major public health problem that can cause great family problems, marital instability, and suicidal tendencies [Citation2]. Hysterosalpingography (HSG) which is the first-line test of tubal patency can be painful and this may affect patient comfort and cooperation during the procedure. The use of analgesia during the procedure has been variously studied, but there is no consensus yet on its use and choice of an ideal agent [Citation7–10].
The majority of women regard a hysterosalpingogram as acutely painful because it involves placement of a cervical tenaculum, traction on the cervix, instillation of dye through a cervical cannula and tubal spilling [Citation10] The most painful step during HSG is when traction was applied to the cervix [Citation7,Citation15,Citation16]. In routine practice, four analgesic procedures are used to prevent pain perception during HSG. These are: use of oral nonsteroidal antiinflammatory drugs (NSAIDs) for systemic pain medication; paracervical block for the cervical pain mechanism; application of topical analgesic cream to the uterine cervix; and intrauterine analgesic instillation for the uterine-tubal pain mechanism. In addition, Erbil Karaman, in his randomized placebo controlled trial, established the efficacy of rectal indomethacin in HSG [Citation17].
In the present study, the mean pain score was comparable in both groups, though slightly lower in the Lidocaine 10% spray than in the oral Diclofenac group. This finding was similar to the findings of Korsuwan et al when EMLA 5% cream (25 mg Lidocaine+25 mg Prilocaine) was topically applied to the cervix [Citation13]. The pain score in the Lidocaine 10% spray arm of the study was similar to 2.80 reported by Kiridi et al at cervical traction when a paracervical block of 1% lidocaine was evaluated compared to a placebo [Citation17].
The perception of pain varies from individual to individual and also varies at different times and parts for the same individual [Citation10]. Thus, pain perception is subjective and this led to various instruments to objectively measure pain perception. These include the Visual Analogue Scale (VAS) [Citation11], Numerical Rating Scale (NRS), Simple Descriptive Scale (SDS), Verbal Rating Scale (VRS), and use of colors and faces for children. One of the most widely adopted instruments to measure pain level is the VAS, which has previously proven its validity and reliability as a pain categories tool [Citation11,Citation12]. Pain is a subjective experience, and therefore it may be difficult to measure in terms of physiologic response unless using complex and expensive materials [Citation12]. Hence, patient’s self-reported measures are valuable and frequently used in clinical and research settings.
There are some alternatives to VAS. The numeric rating scale (NRS) and the verbal rating scale (VRS) can be performed by phone and have demonstrated different levels of consistency and validity. The VAS showed the highest scores [Citation10–12]. Chiarotto et al [Citation12] concluded that NRS was strongly correlated with VAS in emergency patients, making NRS suitable for these patients. However, VRS and VAS are not interchangeable when measuring pain, whether chronic pain or chronic/idiopathic, nociceptive, and neuropathic pain. As a consequence, the measurement instrument used before, during, and after a procedure should be the same. The most commonly used scale is the visual analog scale. A change in the visual analog scale score represents a relative change in the magnitude of pain sensation. Use of the VAS in comparative analgesic trials can now meaningfully quantify differences in potency and efficacy [Citation10]. For the purpose of this study visual analog scale (vas) was used to assess the pain score because it is believed to be more objective, easy to understand and administered
The pain scores at contrast installation were not significantly different in both groups. There were however significantly lower pain scores in the oral diclofenac 30 minutes after the procedure of hysterosalpingography. The higher pain score in the 10% Lidocaine group may be because Lidocaine spray doesn’t have any effect on pain pathways arising from the uterus as a result of uterine distention with contrast medium and peritoneal irritation. This pain has been postulated to be due to prostaglandin synthesis [Citation9,Citation18,Citation19]. Lidocaine spray cannot, therefore, act on the pain receptors located in the uterus and peritoneum.
Oral diclofenac is more effective in relieving pain after HSG than Lidocaine spray as the number of patients that required additional analgesia (Pentazocine injection 30 minutes after the procedure) was lower in the Diclofenac group. This probably is a result of the anti-inflammatory effect of Diclofenac sodium mediated by blockade of the cyclooxygenase pathway thereby inhibiting prostaglandin synthesis in the uterus and the peritoneum. This may have a lot of clinical implications as it is likely to ensure patient comfort after the procedure. This fact has been corroborated by previous studies [Citation20–23].
From this study, the Lidocaine spray tolerability profile seems to be marginally better than oral Diclofenac sodium. This is not surprising as adverse drug reaction with the local anesthetic agent is very rare unless accidental injection into a blood vessel occurs, which may produce life-threatening cardiovascular or central nervous system side effects. This was however unlikely in this study as Lidocaine spray was topically applied, absorption was trans-mucosal and the risk of systemic absorption was very minimal. On the other hand, the oral diclofenac side effects were mainly mild gastrointestinal symptoms which are transient as they remained statistically insignificant by 30 minutes after hysterosalpingography.
5. Limitation of the study
The baseline pain score before the commencement of hysterosalpingography was not measured in this study. Also, the pain score was not assessed beyond 30 minutes after hysterosalpingography.
6. Conclusion
The 10% Lidocaine spray (10 mg) had comparable efficacy to 50 mg oral diclofenac sodium, especially during the tenaculum application and cervical traction which is the most painful step during hysterosalpingography. Oral diclofenac sodium, however, has the additional benefit of significant pain reduction 30 minutes after the procedure although it has a higher rate of side effects.
7. Recommendation
Based on the findings from this study, oral diclofenac sodium is comparable to lidocaine spray for pain relief during hysterosalpingography. It also has the additional benefit of improved quality of life 30 mins after hysterosalpingography as evidenced by effective pain relief. Consideration should be given to the use of oral diclofenac sodium for pain relief during and after hysterosalpingography in well-selected patients. However, in patients with known contraindication to the use of non-steroidal anti-inflammatory drugs, 10% lidocaine spray may be an option.
A larger randomized multicentre study is recommended to validate the result of this study. Future research should look into the evaluation of other non-steroidal analgesics with better side effect profiles than oral diclofenac sodium for analgesia during HSG.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Ayodeji Idowu
Ayodeji Idowu Dr. Ayodeji Idowu is a consultant Obstetrician Gynaecologist and the Chief Medical Director of the Stae Specialist Hospital, Ikare, Ondo State Nigeria
Akintunde O Fehintola
Dr. Fehintola Akintunde Olusegun is a Consultant Obstetrician and Gynaecologist and a senior lecturer at the Department of Obstetrics, Gynaecology, and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
Mopelola c Ashaleye
Dr. Mopelola C Ashaleye is a Consultant Radiologist and Associate Professor at the Department of Radiology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria.
Oluwole E Ayegbusi
Dr Oluwole E Ayegbusi is a consultant Obstetrician Gynaecologist and Lecturer at the Department of obstetrics, Gynaecology and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
Akinyosoye D Ajiboye
Dr. Akinyosoye D Ajiboye is a is consultant Obstetrician Gynaecologist and Lecturer at the Department of Obstetrics, Gynaecology and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
Olusegun O Badejoko
Olusegun O Badejoko Dr. Olusegun O Badejoko is a consultant Obstetrician Gynaecologist and Associate Professor at the Department of Obstetrics, Gynaecology and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
Kayode O Ajenifuja
Kayode O Ajenifuja Prof. Kayode O Ajenifuja is a consultant Obstetrician Gynaecologist and Professor at the Department of Obstetrics, Gynaecology and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
Morebise O Loto
Prof. Morebise O Loto is a consultant Obstetrician Gynaecologist and Professor at the Department of Obstetrics, Gynaecology and Perinatology, Obafemi Awolowo University, Ile-Ife, Osun State. Nigeria
References
- Akhondi MM, Ranjbar F, Shirzad M, et al. Practical difficulties in estimating the prevalence of primary infertility in Iran. Int J Fertil Steril. 2019 Jul;13(2):113.
- Giwa OM The impact of infertility diagnosis and subsequent treatment on couples’ relational dynamics in southwest Nigeria.
- Kyei JM, Manu A, Kotoh AM, et al. Beliefs about children and the psychosocial implications of infertility on individuals seeking assisted fertilization in Ghana. Reprod Biomed Online. 2021 Mar 1;12:88–95. DOI:10.1016/j.rbms.2021.02.003.
- Mbah CE, Jasani A, Aaron KJ, et al. Association between Chlamydia trachomatis, Neisseria gonorrhea, Mycoplasma genitalium, and Trichomonas vaginalis and Secondary Infertility in Cameroon: a case-control study. PLoS ONE. 2022 Feb 4;17(2):e0263186.
- Zafarani F, Ghaffari F, Ahmadi F, et al. Hysterosalpingography in the assessment of proximal tubal pathology: a review of congenital and acquired abnormalities.Br J Radiol. [2021 Jun 1] 1122 ;94(1122):20201386. DOI:10.1259/bjr.20201386.
- Oriji CP, Kiridi KE, Allagoa DO, et al. The use of NAAT-PCR to determine asymptomatic chlamydia and gonorrhea infections in infertile patients undergoing hysterosalpingogram at the federal medical center, Yenagoa, South-South Nigeria. Int J Reprod Contraception Obstetrics Gynecology. 2020;9(4):1508.
- Abu-Zaid A, Baradwan S, Abuzaid M, et al. I. EMLA (lidocaine-prilocaine) cream for pain relief during hysterosalpingography: a systematic review and meta-analysis of randomized placebo-controlled trials. Human Fertility. 2022 Feb;26:1–9.
- Jayeola DK, Bello TO, Oyedepo VO, et al. The efficacy of oral naproxen and cervical lidocaine spray on perceived pain during hysterosalpingography. Niger Postgrad Med J. 2021 Jul 1;28(3):193.
- Last RJ. Anatomy: regional and applied. 10th ed. New York: Churchill Livingstone; 1999. p. 295.
- Delgado DA, Lambert BS, Boutris N, et al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop. 2018 Mar;2(3):e088.
- Wiese AJ Canine & feline pain scales. online] cliniciansbrief. com. Available at: https://www.cliniciansbrief.com/article/canine-feline-pain-scales.html [Accessed 24 Nov. 2020]. 2018.
- Chiarotto A, Maxwell LJ, Ostelo RW, et al. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. 2019 Mar 1;20(3):245–263.
- Karasahin E, Alanbay I, Keskin U, et al. Lidocaine 10% spray reduces pain during hysterosalpingography: a randomized controlled trial. J Obstet Gynaecol Res. 2009;35(2):354–358.
- Kirkwood BR, Sterne JA. Calculating sample size. In: Kirkwood B Sterne J, editors. Essential medical statistics. Vol. 10. 2nd ed. Massachusettes: Blackwell; 2003. pp. 413–428.
- Aboshama RA, Shareef MA, AlAmodi AA, et al. The effect of hyoscine-N-butylbromide on pain perception during and after hysterosalpingography in infertile women: a systematic review and meta-analysis of randomised controlled trials. Human Fertility. 2020 Nov;2(3):1–8.
- Serrano González L, Pérez-Medina T, Bueno Olalla B, et al. Is hysterosalpingo-foam sonography (HyFosy) more tolerable in terms of pain and anxiety than hysterosalpingography (HSG)? A prospective real-world setting multicentre study. BMC Women’s Health. 2022 Dec;22(1):1–9.
- Karaman E, Çim N, İ A, et al. Rectal indomethacin use in pain relief during hysterosalpingography: a randomized placebo controlled trial. J Obstetrics Gynaecol Res. 2016 Feb;42(2):195–201.
- Khizroeva J, Nalli C, Bitsadze V, et al. Infertility in women with systemic autoimmune diseases. Best Pract Res Clin Endocrinol Metab. 2019 Dec 1;33(6):101369.
- Lozic M, Ludwig MO. InEncyclopedia of molecular pharmacology 2021 Jan 7. Cham: Springer International Publishing;pp. 1203–1209.
- Abbas AM, Wagdy WM, Salem MN, et al. Effect of oral diclofenac potassium plus cervical lidocaine cream on pain perception during hysterosalpingography: a randomized, double-blind, placebo-controlled trial. Middle East Fertil Soc J. 2018 Mar 1;23(1):52–56.
- Troia L, Darino I, Regini C, et al. Factors affecting pain perception in outpatient hysteroscopy. Eur J Obstet Gynecol Reprod. 2019;1(1):39–42.
- Tur-Kaspa I, Revelli A, Stadtmauer LA, et al. Sonohysterography (SHG) in reproductive medicine. In: Laurel, A. Stadtmauer, Ilan, Tur-Kaspa, editors. Ultrasound imaging in reproductive medicineCham: Springer; 2019. p. 199–210.
- Yuen MV, Gianturco SL, Pavlech LL, et al. Benzocaine: summary Report.