ABSTRACT
Objectives
Coronary artery thrombus burden (TB) is one of the risk factors for major adverse cardiovascular events (MACE) in patients with acute ST segment elevation myocardial infarction (STEMI). It was discovered that there is a strong relationship between epicardial adipose tissue (EAT) thickness and the incidence of coronary atherosclerosis. The aim of our study is to evaluate the relationship between EAT thickness and coronary TB in patients with STEMI treated with primary percutaneous coronary interventions (PPCI).
Methods
The study included 80 patients presented with acute STEMI and treated by PPCI; their mean age was 54.35 ± 8.80 years, and 70 (87.5%) were males. Patients were divided into 2 groups according to the degree of TB: group I (25 patients) with low TB and group II (55 patients) with high TB. The EAT thickness was measured by 2D-echocardiography in all patients.
Results
We found that EAT thickness was significantly higher in group II compared to group I (p < 0.001), and theROC curve cutoff point value of EAT thickness equal to or greater than 2.48 mm could predict high TB in patients with STEMI (p < 0.001), and by multivariate analysis, EAT thickness was the most significant predictor of high TB.
Conclusions
In STEMI patients undergoing primary PCI, the increased EAT thickness measured by 2D echocardiography is significantly associated with a high coronary artery thrombus burden.
1. Introduction
Coronary thrombus burden (TB) is one of the risk factors for major adverse cardiovascular events (MACE) in patients with acute coronary syndromes (ACS) [Citation1,Citation2]. Thrombus burden has an effect on the procedural success of primary percutaneous coronary intervention (PPCI) in patients with acute ST segment elevation myocardial infarction (STEMI). [Citation3] Therefore, identifying the variables that predict coronary TB is crucial for selecting the best course of action to avoid PCI failure and complications.
Epicardial adipose tissue (EAT) is the adipose tissue that covers the free wall of the right ventricle, the apex of the left ventricle (LV), and the atria. It starts at the atrioventricular and interventricular grooves and extends to the apex between the myocardium and visceral pericardium. The epicardial fat is vascularized by coronary artery branches [Citation4]. Under physiological conditions, this anatomically distinct fat compartment accounts for roughly 20% of the heart’s overall volume and almost 80% of its surface area. [Citation5] EAT is the source of a number of bioactive atherogenic and pro-inflammatory compounds such as adiponectin, tumor necrosis factor-alpha (TNF-alpha), Interleukin 1 (IL1), interleukin 6 (IL6), and monocyte chemoattractant protein-1 (MCP-1), which may have a significant effect on myocardial microvascular dysfunction and thrombus formation [Citation6–8]. The volume of the EAT remained a very accurate predictor of coronary atherosclerosis [Citation9]. The aim of our study is to evaluate the relationship between the EAT thickness as measured by 2D-echocardiography and the coronary artery TB in patients presented with STEMI and treated by PPCI.
2. Materials and methods
Our study is a prospective cohort one, conducted at the cardiology department at Alexandria University Hospital, from March 2021 to August 2022. The study was approved by our Faculty of Medicine ethical committee and included 80 patients with acute STEMI undergoing PPCI within 12 hours after the onset of ischemic symptoms, excluding those who received thrombolytic therapy, patients with left bundle branch block, cardiogenic shock on admission, established systemic inflammatory disorders, liver disease, and renal failure. All patients were subjected to the following:
All patients underwent the following:
An informed written consent was obtained from all patients with explanations of all steps of the research before the start of the study.
Detailed history and clinical examinations, including age, gender, risk factor for coronary artery disease (CAD), pain to first medical contact (FMC), assessment of pulse, blood pressure, and Killip class.
Standard 12-lead electrocardiogram (ECG) for the diagnosis of STEMI.
Laboratory investigations include hemoglobin level, serum urea, creatinine, serum total cholesterol (Ch), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, serum triglyceride (TG), glycated hemoglobin (HbA1c), high-sensitivity cardiac troponin, and creatine kinase-MB (CK-MB).
Coronary angiogram and PPCI with stent placement within 12 hours of symptoms were done to all STEMI patients included in the study, and before stent placement, the thrombus burden was graded (G) according to the Angiographic Thrombolysis in Myocardial Infarction (TIMI) thrombus scale as G0 = no thrombus, G1 = possible thrombus, G2 = small [greatest dimension ≤ 1/2 vessel diameter (VD)], G3 = moderate (>1/2 but < 2VD), G4 = large (≥2VD), and G5 = complete thrombotic occlusion of the vessel [Citation10]. And we classified our patients into two groups according to TB: Group I with a low TB grade (1–3), and Group II with a high TB grade (4–5).
Echocardiography: routine transthoracic echocardiography was done to all patients during their hospital stay post-PPCI and within 24 hours of admission using a Philips (iE33 xMATRIX) echo system, and the following parameters were measured:
Measurement of left ventricular end diastolic volume (LVEDV), left ventricular end systolic volume (LVESV), and estimation of LV ejection fraction (LVEF) using the biplane Simpson method [Citation11].
E/e’ of the left ventricle is the ratio between early mitral inflow velocity (E) and early diastolic mitral annulus velocity (e’) [Citation12].
Left atrial volume index (LAVI) [Citation12].
Wall motion score index (WMSI) [Citation11].
Assessment of mitral valve regurgiation severity [Citation11].
EAT: epicardial adipose tissue thickness was measured as an echo-free space between the myocardium and visceral epicardial and was measured perpendicular to the free wall of the right ventricle in parasternal long-axis view and parasternal short-axis view [Citation13].
3. Statistical analysis
Data were analyzed using IBM SPSS software package version 20.0 (Armonk, NY: IBM Corp.). Categorical variables were described using numbers and percents and compared using the chi-square test, while continuous variables were described using mean and standard deviation and compared using the Mann–Whitney test. The receiver operator characteristic (ROC) curve, univariate, and multivariate logistic regression tests were also used. The p value of <0.05 was considered statistically significant.
4. Results
4.1. Demographic, ECG, and laboratory data are shown in
The study included 80 patients, their mean age 54.35 ± 8.80 years, and 70(87.5%) were males. Our patients were divided into two groups according to TB: Group I with low TB grade 25 patients (30.3%), and group II with high TB grade 55 patients (68.6%). There was no significant difference between the 2 groups regarding age, gender, presence of previous cardiovascular diseases, cardiovascular risk factors, site of infarction, and Killipe class, however there was a significant increase in BMI, troponin, and CK-MB in group II.
Table 1. Comparison between the two studied groups according to demographic, clinical, and laboratory characteristics.
4.2. Coronary angiogram and PPCI details are shown in
There was no statistically significant difference between both groups regarding procedural characteristics except for balloon predilation which was higher in group II (p = 0.006).
Table 2. Comparison between the two studied groups according to the angiographic results.
4.3. Echocardiographic results are shown in
• There was no significant difference between the 2 groups as regards the LVEDV, LVESV, LVEF, E/e’ ratio, WMSI, or mitral valve regurgitation severity. However, LAVI (p = 0.002) and EAT (p < 0.001) were significantly higher in group II ().
Figure 1. Shows EAT thickness of 3.07 mm in one STEMI patients with angiographically high thrombus burden.

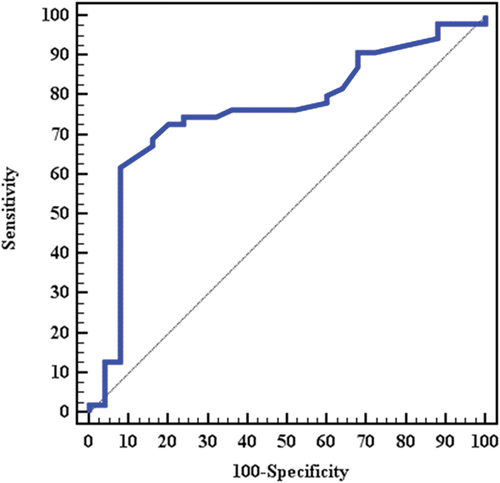
• The ROC curve analysis was performed to determine the cutoff value of EAT thickness that predicts the presence of high TB, and it was equal to or greater than 2.48 mm (74.55% sensitivity and 72.0% specificity, AUC: 0.75795% confidence intervals: 0.641–0.874; p < 0.001) ().
Figure 2. ROC curve that predict EAT thickness cutoff value of 2.48 mm to predict high thrombus burden in STEMI patient.
• Univariate logistic regression was done as seen in , and among all clinical, laboratory, angiographic, and echocardiographic variables, the BMI (odds ratio: 1.144, 95% CI: 1.029–272; p = 0.013) and EAT thickness (odds ratio: 1.898, 95% CI: 1.217–2.961; p = 0.005) were statistically significant univariate predictors of high TB. And by multivariate regression analysis, EAT thickness was found to be the most significant predictor of high thrombus burden (odds ratio: 2.573, 95% CI: (1.381–4.794); p = 0.003).
Table 3. Comparison between the two studied groups according to echocardiographic results.
Table 4. Univariate logistic regression of different parameters to predict the thrombus burden in STEMI patients undergoing PPCI.
5. Discussion
Coronary thrombus burden affects how successfully an ACS patient may respond to PCI. Therefore, determining the factors in the prediction of intracoronary thrombus burden has great importance in forecasting adverse cardiovascular events as well as determining the most appropriate treatment strategy to prevent any failure in PCI [Citation14,Citation15]. It was discovered that there is a strong relationship between EAT volume and the incidence of coronary atherosclerosis. Under the visceral pericardium, EAT is a real visceral fat store. It has now been established that the EAT is a metabolically active organ that generates proinflammatory cytokines. Increased EAT was linked to the metabolic syndrome, coronary artery disease, coronary no-reflow, and hypertension [Citation16]. Given that EAT may have paracrine effects, the distance between the epicardial coronaries and cardiac interstitium may have a significant role in the onset of myocardial microvascular dysfunction and the generation of thrombi [Citation17]. Measurement of EAT by transthoracic echocardiography has many advantages due to its affordability, accessibility, high reproducibility, and good correlation with EAT measured by magnetic resonance imaging [Citation13]. The EAT thickness measured by echocardiography is considered a marker of visceral adiposity, and EAT thickness ranging from 1 mm to 25 mm reflects the variation in intra-abdominal fat accumulation [Citation18].
Our present research results showed that the mean EAT thickness was statistically significantly lower in the low compared to high thrombus burden group (p < 0.001), and our results are in agreement with Uslu A et al., who studied 51 individuals with low TB and 105 with high TB, the EAT thickness measured by 2 D-echocardiography, and they found that there were no differences between the two groups as regard the LVEF, the different major risk factors for CAD; however, the EAT thickness was identified in multivariate logistic regression analysis as an independent predictor of high TB (p = 0.001) [Citation19]. Also, Wang, Q. et al. In total, 21 studies included 4975 subjects, of whom 2377 were assigned to the CAD group, while the remaining 2598 were assigned to the non-CAD group. The EAT thickness was measured by 2D echocardiography, and they found that patients with CAD have a greater thickness of EAT than patients without CAD. This suggests that an abnormally expanded EAT may contribute to the development of CAD and function as a useful predictor and potential therapeutic target for the disease condition [Citation20]. In our study, we found that the EAT thickness that predicts the presence of high TB was equal to 2.48 mm; this value was lower than that reported by Uslu A et al., who studied prospectively. 156 STEMI patients treated by PPCI, and EAT thickness was measured in all patients using tranthoracic echocardiography within 24 hours of admission, as we did in our study, and they found that EAT thickness of 5.3 mm with 86.7% sensitivity and 82.4% specificity can predict high TB, but they agree with us that EAT thickness was found to be an independent predictor of high TB (p < 0.001) [Citation19]. Also Mahfouz et al. Included 100 patients who were ungergoing coronary angiography, all patient had an echocardiogram with measurment of EAT thickness, they reported that EAT thickness is significantly associated with presence of CAD, and the ROC curve cutoff point value of ≥4.5 mm of EAT thickness predicts CAD, with a specificity and a sensitivity of 63.6% and 69.2%, respectively [Citation21].
6. Conclusions
In STEMI patients undergoing primary PCI, the increased EAT thickness measured by 2 D- echocardiography is significantly associated with high coronary artery thrombus burden.
Author contributions
GM did the acquisition and interpretation of echocardiography data, wrote and revised the article, DZ performed data collection and analyzed the data, and MH performed the final data analysis. All authors had read and revised the article critically for important intellectual content and final approval of the version to be published.
Ethics approval, and consent to participate
The Ethics Committee of the Faculty of Medicine at Alexandria University had approved the study, and informed consent was obtained from all participants included in the study.
Study limitations
Our study has several limitations, including the relatively small sample size for the total sample group; larger studies are needed to validate these results. Another important limitation of our study is that measurement of EAT or performing echocardiography in general is not recommended in STEMI patients before reperfusion strategy, and we already performed our echocardiography post-PPCI and within 24 hours from admission (and this was mentioned in the methodology). But in our study, we needed to prove the relationship between EAT and TB grade, and we found that EAT thickness was significantly higher in patients with a high TB grade. Accordingly, we recommend the measurement of EAT in all elective cases of chronic coronary syndromes, and those with increased EAT thickness should be advised to take more aggressive preventive measures.
Acknowledgments
The authors acknowledge the staff of the cardiology department at Alexandria University Hospital for their unlimited support during the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Gehan Magdy
Dr. Gehan Magdy, MD: Assistant professor in Cardiology and Angiology department, Faculty of Medicine, Alexandria university, Egypt.
Aly Alsaid Zidan
Dr. Aly Alsaid Zidan, MD: Lecturer in Cardiology and Angiology department, Faculty of Medicine, Alexandria university, Egypt
Diaa Aldin Taha Ramadan Zahran
Dr. Diaa Aldin Taha Ramadan Zahran, MS :Specialist of cardiology, Faculty of Medicine, Alexandria university, Egypt
Mahmoud Hassanein
Prof. dr. Mahmoud Hassanein, MD : Professor in Cardiology and Angiology department, Faculty of Medicine, Alexandria university, Egypt.
References
- Kumar R, Shah JA, Solangi BA, et al. The burden of short-term major adverse cardiac events and its determinants after emergency percutaneous coronary revascularization: a prospective follow-up study. J Saudi Heart Assoc. 2022 Jun 11;34(2):100–109. doi: 10.37616/2212-5043.1302
- Köktürk U, Somuncu MU, Begüm U, et al. Prognostic significance of thrombus burden on short- and long-term clinical outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2022;33(7):559–565. doi: 10.1097/MCA.0000000000001178
- Vecchio S, Varani E, Chechi T, et al. Coronary thrombus in patients undergoing primary PCI for STEMI: prognostic significance and management. World J Cardiol. 2014 Jun 26;6(6):381–392. doi: 10.4330/wjc.v6.i6.381
- Gaborit B, Sengenes C, Ancel P, et al. Role of epicardial adipose tissue in health and disease: a matter of fat? Compr Physiol. 2017;7:1051–1082.
- Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005;2(10):536–543. doi: 10.1038/ncpcardio0319
- Corradi D, Maestri R, Callegari S, et al. The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovasc Pathol. 2004;13(6):313–316. doi: 10.1016/j.carpath.2004.08.005
- Iacobellis G, Barbaro G. The double role of epicardial adipose tissue as pro- and anti-inflammatory organ. Horm Metab Res = Horm Und Stoffwechselforsch = Horm Metab. 2008;40(7):442–445. doi: 10.1055/s-2008-1062724
- Hirata Y, Kurobe H, Akaike M, et al. Enhanced inflammation in epicardial fat in patients with coronary artery disease. Int Heart J. 2011;52(3):139–142. doi: 10.1536/ihj.52.139
- Djaberi R, Schuijf JD, van Werkhoven JM, et al. Relation of epicardial adipose tissue to coronary atherosclerosis. Am J Cardiol. 2008;102(12):1602–1607. doi: 10.1016/j.amjcard.2008.08.010
- Sianos G, Papafaklis MI, Serruys PW. Angiographic thrombus burden classification in patients with ST-segment elevation myocardial infarction treated with percutaneous coronary intervention. J Invasive Cardiol. 2010;22(10 Suppl B):6B–14B.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiography. 2015;28(1):1)1–39. doi: 10.1016/j.echo.2014.10.003
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016 Apr;29(4):277–314.
- Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009;22(12):1311–1319. doi: 10.1016/j.echo.2009.10.013
- Köktürk U, Somuncu MU, Uygur B, et al. Prognostic significance of thrombus burden on short- and long-term clinical outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2022;33(7):559–565. doi: 10.1097/MCA.0000000000001178
- Satılmış S, Durmuş G. Predictive accuracy of CHA(2)DS(2)-VASc score in determining the high thrombus burden in patients with non-ST-elevation myocardial infarction. Acta Cardiol. 2021;76(2):140–146. doi: 10.1080/00015385.2019.1707934
- Konwerski M, Gąsecka A, Opolski G, et al. Role of epicardial adipose tissue in cardiovascular diseases: a review. Biology. 2022;11(3):355. doi: 10.3390/biology11030355
- Weber T, Lang I, Zweiker R, et al. Hypertension and coronary artery disease: epidemiology, physiology, effects of treatment, and recommendations: a joint scientific statement from the Austrian Society of Cardiology and the Austrian Society of hypertension. Wien Klin Wochenschr. 2016;128(13–14):467–479. doi: 10.1007/s00508-016-0998-5
- Nelson AJ, Worthley MI, Psaltis PJ, et al. Validation of cardiovascular magnetic resonance assessment of pericardial adipose tissue volume. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2009;11(1):15. doi: 10.1186/1532-429X-11-15
- Uslu A, Kup A, Dogan C, et al. Relationship between epicardial adipose tissue thickness and coronary thrombus burden in patients with ST-elevation myocardial infarction. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2020 Jun;164(2):141–146.
- Wang Q, Chi J, Wang C, et al. Epicardial adipose tissue in patients with coronary artery disease: a meta-analysis. J Cardiovasc Dev Dis. 2022;9(8):253. doi: 10.3390/jcdd9080253
- Mahfouz AM, Ibrahim KI, El-Gendy EA, et al. The relationship between epicardial adipose tissue thickness and coronary artery disease. Med J Cairo Univ. 2019;87(March):209–214. doi: 10.21608/mjcu.2019.52342
