ABSTRACT
Objective
To evaluate the learning curve and the success rate of the biplanar (0–90°) puncture technique in the flank-free modified supine position in comparison to the monoplanar puncture technique.
Methods
Randomized controlled study included 68 patients more than 18 years with renal stones more than 2 cm from August 2021 to August 2022 were randomly classified by closed envelope method into group A (34 patients) scheduled for monoplanar renal puncture technique in flank-free modified supine PCN. Meanwhile, group B (34 patients) was scheduled for the 0–90° simplified fluoroscopic puncture technique. Morbid obese patients and patients with contraindications for PNL were omitted from the study.
Results
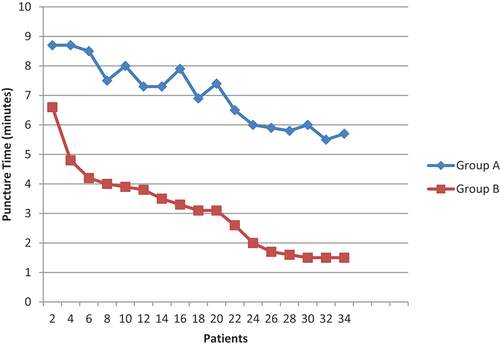
There was no significant difference between both groups regarding stone distribution and patients’ demographic data. There was a significant difference between both groups regarding puncture attempts. In 88.2% of patients in group B (Biplanar group), the success of renal puncture occurred from the 1st puncture attempt while in 11.2% of patients in group A (monoplanar group). There was a statistically significant difference between both groups in fluoroscopy time and total operation time (p-value <0.001 & p-value: 0.001), respectively. The stone-free rate was 85.2% vs. 88.2% in both groups, respectively, without significant difference. In this study puncture, attempt trials and puncture time were used as indicators for the easiness and rapid educability of the biplanar (0–90°) fluoroscopic guided renal puncture technique. In the biplanar (0–90°) group after 24 cases, the learning curve had reached the plateau.
Conclusion
Biplanar (0–90°) puncture technique in flank-free modified supine position allows an easy puncture technique with an easy learning curve without affecting the success rate or complication rate.
Introduction
The treatment of choice for renal stones more than 2 cm is percutaneous nephrolithotomy (PNL) [Citation1]. It is also an optional treatment for renal stones less than 2 cm, e.g. lower calyx stones. The main profession of urologists was surgical competence in PNL being mainly in renal access puncture [Citation2]. There are many ways to do renal puncture like fluoroscopy, ultrasound, and computed tomography (CT) guidance. However, most urologists prefer to do fluoroscopy-guided PNL [Citation3]. Other technology assistance may be used such as augmented reality, the ANT-X (Automated needle targeting with X-ray), or robot-assisted fluoroscopy [Citation4,Citation5]. The fluoroscopy-guided renal puncture can be done in one imaging plane or two imaging planes. In supine PNL, monoplanar technique is frequently used, but it may take many trials to reach the target. However, the biplanar technique resolves the problem of renal calyx depth calculation. So the urologist can easily determine the depth of the puncture and also the direction of the desired calyx [Citation6]. The ideal renal puncture is a cornerstone step for successful PNL with minimal complications. The increase in the number of puncture attempts is always associated with an increased risk of bleeding and sepsis. Therefore, precise puncture site identification means lower complication incidence [Citation7]. The 0–90° simplified fluoroscopic puncture technique allows easy renal puncture with low fluoroscopic screening time [Citation8], so we do this study to compare this biplanar technique with the conventional monoplanar technique in flank-free modified supine PCNL regarding success rate and complications as primary end point. The learning curve for bi-planar technique was evaluated also as secondary end point.
Patient and methods
Study design
This prospective randomized controlled study was done from August 2021 to August 2022 in Zagazig university Urology Department
Inclusion criteria
Patients ≥18 years old with renal stones ≥2 cm and Guys score grade 1–2 by non-contrast CT abdomen and pelvis scheduled for PNL. Exclusion criteria: Patients with contraindications for PNL like bleeding disorders, active UTI, and skeletal deformities were excluded. Morbid obese patients were excluded from the study.
Sample size
The sample size was calculated providing that the effect size is 0.5 with an error protection of 0.05 and 80% power of the study. After adding 10% for possible drop out or loss during follow-up, the sample size was at least 34 patients in each group. After Institutional Review Board (IRB) approval and written informed consent from all patients was obtained
Randomization
Patients were randomized into two groups by closed envelope method. Each group includes 34 patients.
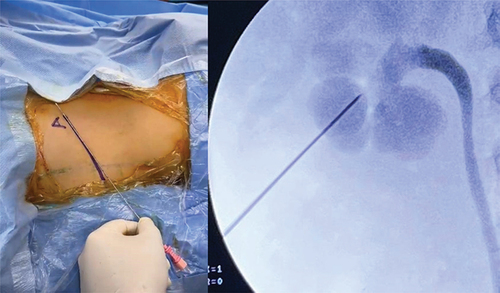
Operative techniques
Group A scheduled for monoplanar renal puncture technique in flank-free modified supine PCNL [Citation9,Citation10], while group B is scheduled for the 0–90° simplified fluoroscopic puncture technique in flank-free modified supine PCNL [Citation8,Citation10]. In this technique, we first use the C arm at 0° to determine the craniocaudal direction and the media-lateral direction of the puncture (line A) (. The C arm then rotated to 90° to determine the depth (anteroposterior level) which represents a horizontal line B . The puncture point will be the meeting of two lines. The needle will be horizontal in the same plane as line B. But it will be advanced in the direction of line A . Perioperative workup: All patients were assessed preoperatively by thorough history taking, preoperative laboratory requirements, and non-contrast pelvic-abdominal CT. All patients of both groups were assessed within the 1st 24 hours’ post-operative by CBC and pelvi-abdominal ultrasound to determine complications like bleeding and hematoma. Non-contrast CT was performed 1-month post-operative to determine stone clearance. All patients were operated on by the same surgeon (senior resident monitored by experienced PNL surgeon). We compared both groups regarding operative time from starting cystoscopy and retrograde ureteric catheter insertion to insertion of a nephrostomy tube. The number of puncture trials, fluoroscopy time in minutes, perioperative bleeding that needed a blood transfusion, post-operative complication grades according to Modified Clavien system [Citation11], and the need for ancillary procedures were determined. The learning curve was anticipated for each technique. The primary end point was success rate and complications. The secondary end point was learning curve.
Figure 1. C arm at zero position and line a represent the cranio-caudal and medio-lateral direction for target calyx.
Statistical methods
Data analysis was done using IBM SPSS 23.0 for windows (SPSS Inc., Chicago, IL, USA) and NCSS 11 for windows (NCSS LCC., Kaysville, UT, USA). According to the type of data, qualitative represented as number and percentage, quantitative continuous represented by mean and standard deviation, the following tests were used to test differences for significance; difference and association of qualitative variable by Chi-square test (X2). Differences between quantitative independent groups were by t-test or Mann–Whitney and repeated measures ANOVA for comparison of multiple means. p value was set at <0.05 for significant results &<0.001 for high significant result.
Results
Seventy patients were enrolled in this study. Sixty-eight patients fulfilled the inclusion and exclusion criteria and were accepted to participate (34 patients in each group). The patient flow chart in the study is shown in .
Demographic data
The mean age of patients in both groups was 50.63 ± 9.36 and 51.36 ± 10.61 years, respectively. The rest of the patient’s demographics and stone characteristics are shown in with no significant difference between both groups.
Table 1. Patient demographics and stone characteristics.
Renal puncture
In 88.2% of patients in group B (Biplanar group), the success of renal puncture occurred from the first puncture attempt, while in 11.2% of patients in group A (monoplanar group), 5 trials were needed to access the kidney and 3 times in 50% of patients (p-value: 0.001) (). There was a significant difference in the mean number of puncture attempts between both groups (3.273 ± 0.904 & 1.182 ± 0.404), respectively (p-value: 0.001) (). There was a significant difference in the mean of puncture time between both groups (7.11 ± 0.46 & 3.3 ± 0.68), respectively (p-value: 0.001) ().
Table 2. Operative data and clinical outcomes.
Learning curve
The mean puncture time in the biplanar group decreased with the increased number of patients in the study and looked stable in the last 10 cases in the study, while in group A, the learning curve still not reached the plateau at 34 cases ().
Procedure time
There was a statistically significant difference between both groups in fluoroscopy time and total operation time (p-value <0.001 & p-value: 0.001), respectively.
Success rate and complications: The stone-free rate was 85.2% vs. 88.2% in both groups, respectively, without significant difference. The residual stones in both groups were managed by one session of ESWL. Even radiolucent stones in two cases were managed by ultrasound guided ESWL. The overall complication rate was 17.6% vs. 11.7, and it was comparable between both groups (). Only one patient in group A needed blood transfusion. Transient fever was treated conservatively, while active infection was treated by empirical antibiotics till culture results obtained. Urinoma and urinary leak were managed by fixation of urinary catheter and bladder sedations, and no patients need ureteric stent reposition. Delayed hematuria in group A were reported in two patients and managed by angio-embolisation.
Table 3. Patients intra-operative & early post-operative complications.
Discussion
Multiple renal puncture techniques for PNL were present. Fluoroscopy, ultrasound (US), and computerized tomography (CT) guidance were used for most of them. Fluoroscopy is the most common technique for performing percutaneous renal puncture by endo-urologists worldwide using many monoplanar or biplanar fluoroscopic techniques [Citation3]. Usually, biplanar techniques provide better and perfect information about the depth and direction of the pelvicalyceal collecting system than monoplanar methods [Citation6]. A perfect puncture is a crucial point to achieve competence in the operation and avoid post-PNL complications, especially bleeding and sepsis. Therefore, when the puncture site is precisely calculated, it could mean fewer complication rates [Citation7]. Urologists remained for some time searching for a precise, reproducible, easily educable, and worldwide available puncture technique with fewer radiation hazards and less costly instruments [Citation5]. The biplanar (0–90°) fluoroscopic guided renal puncture technique for PNL is a simple maneuver with less radiation exposure that even could be done under pulsed fluoroscopy guidance [Citation8]. In our study, we depended on many factors as indicators for the easiness and rapid educability of the biplanar (0–90°) fluoroscopic guided renal puncture technique. The first of them was the number of renal puncture attempts. In the biplanar (0–90°) fluoroscopic guided renal puncture technique, the success of renal puncture occurred from the 1st puncture attempt in more than 88% of patients. This was significantly lower than the monoplanar group as 3 attempts were needed in 50% of group A patients in our study. This was in agreement with the study of Manzo and colleagues [Citation8], and even better than studies that use ultrasound-guided renal puncture [Citation12]. The 2nd indicator was the puncture time. There was a significant difference in the mean of puncture time between the biplanar and monoplanar groups. These results were comparable to or even better than studies comparing the monoplanar with biplanar puncture techniques [Citation6,Citation8,Citation13–16]. Moreover, not only the mean puncture time in the biplanar group is lower than that in the monoplanar group, but also it decreased with time and the number of cases reached its lower value and became stable in a plateau curve after 24 cases. B. Manzo et al. 2021 stated that the biplanar (0–90°) puncture technique is easy to learn as ten cases are sufficient to reach the plateau [Citation2]. while in group A the learning curve still not reached the plateau even with 34 case this was in agree with Negrete-Pulido et al. 2010 who stated that 50 cases were needed to reach the learning curve plateau. Also Tanriverdi et al. 2007 defined 60 cases as lower limit for learning PNL puncture [Citation12,Citation13] We used also the total operative time as an indicator for the easiness of the biplanar (0–90°) fluoroscopic guided renal puncture technique, especially since all the operations have been done by the same surgical team. The operative time (72.6±3.52) was significantly lower in the biplanar technique group. It was also lower compared to many studies [Citation16–18]. Regarding fluoroscopy time, the biplanar group was significantly lower than monoplanar group. Fluoroscopy time (2.41±0.19) in group B was even lower than reported in many studies [Citation6,Citation19]. There was no significant difference between both groups in stone complexity. Both groups showed non-significant difference regarding success rate and complications. The limitations of our study were 1st the sample size, as a larger sample size is needed for further evaluation of the bi-planar technique. The 2nd limitation is in manipulating the c-arm for 90 degrees we need a well-experienced c-arm technician. In 90 degrees the image quality is affected by 2 important factors, the 1st is the c-arm quality to give a good resolution image while the 2nd factor is the patient weight as in moderately obese patients will make the c-arm image in low quality. Finally, in the bi-planar technique, the entry point is the meeting of two lines (line A and line B). This point may be in an area outside the safety zone either anterior to the posterior axillary line or on the bony iliac crest. In the supine position, always we found the horizontal B line posterior to the posterior axillary line, while in only one case, line A met the B line on the bony iliac crest. This was managed by a slight adjustment of line A to meet the B line just above the iliac crest.
Conclusion
Biplanar (0–90°) puncture technique in flank-free modified supine position allows easy puncture technique with an easy learning curve without affecting the success rate or complication rate.
Authors contributions
Mohamed S Elderey: Study design, conception, protocol development, data analysis, manuscript writing, and manuscript editing.
Maged M. Ali: Data analysis, manuscript writing, and manuscript editing.
Lofty Elbendary: Data collection, manuscript writing and editing.
Esam A. Zaed: Manuscript writing and manuscript editing.
Esam Desoky: Manuscript editing and protocol development.
Ibrahim M. Ibrahim: Data collection and manuscript editing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Hughes T, Ho HC, Pietropaolo A, et al. Guideline of guidelines for kidney and bladder stones. Turk J Urol. 2020;46(Suppl 1):S104. doi: 10.5152/tud.2020.20315
- Manzo B, Torres J, Cabrera J, et al. Simplified biplanar (0–90°) fluoroscopic puncture technique for percutaneous nephrolithotomy: the learning curve. World J Urol. 2021;39(9):1–7. doi: 10.1007/s00345-021-03669-7
- Wei C, Zhang Y, Pokhrel G, et al. Research progress of percutaneous nephrolithotomy. Int Urol Nephrol. 2018;50(5):807–817. doi: 10.1007/s11255-018-1847-4
- Oo MM, Gandhi HR, Chong KT, et al. Automated needle targeting with X-ray (ANT-X)-robot-assisted device for percutaneous nephrolithotomy (PCNL) with its first successful use in human. J Endourol. 2021;35(6):e919–e. doi: 10.1089/end.2018.0003
- Rassweiler-Seyfried M-C, Rassweiler J, Weiss C, et al. iPad-assisted percutaneous nephrolithotomy (PCNL): a matched pair analysis compared to standard PCNL. World J Urol. 2020;38(2):447–453. doi: 10.1007/s00345-019-02801-y
- Dede O, Bas O, Sancaktutar AA, et al. Comparison of monoplanar and biplanar access techniques for percutaneous nephrolithotomy. J Endourol. 2015;29(9):993–7. doi: 10.1089/end.2015.0166
- Ganpule AP, Shah DH, Desai MR. Postpercutaneous nephrolithotomy bleeding: aetiology and management. Curr Opin Urol. 2014;24(2):189–94. doi: 10.1097/MOU.0000000000000025
- Manzo BO, Gómez F, Figueroa A, et al. A new simplified biplanar (0-90°) fluoroscopic puncture technique for percutaneous nephrolithotomy. Reducing fluoroscopy without ultrasound. Initial experience and outcomes. Urology. 2020;140:165–170. doi: 10.1016/j.urology.2020.03.002
- Salah MA. Monoplanar acces for Percutaneous Nephrolithotomy. J Urol Nephrol. 2016;1(1):000104. doi: 10.23880/OAJUN-16000104
- Desoky EA, Allam MN, Ammar MK, et al. Flank free modified supine position: a new modification for supine percutaneous nephrolithotomy. Arab J Urol. 2012;10(2):143–148. doi: 10.1016/j.aju.2011.12.008
- Kadlec AO, Greco KA, Fridirici ZC, et al. Comparison of complication rates for unilateral and bilateral percutaneous nephrolithotomy (PCNL) using a modified clavien grading system. BJU Int. 2013;111(4b):E243–E8. doi: 10.1111/j.1464-410X.2012.11589.x
- Agarwal M, Agrawal MS, Jaiswal A, et al. Safety and efficacy of ultrasonography as an adjunct to fluoroscopy for renal access in percutaneous nephrolithotomy (PCNL). BJU Int. 2011;108(8):1346–9. doi: 10.1111/j.1464-410X.2010.10002.x
- Negrete-Pulido O, Molina-Torres M, Castaño-Tostado E, et al. Percutaneous renal access: the learning curve of a simplified approach. J Endourol. 2010;24(3):457–60. doi: 10.1089/end.2009.0210
- Tanriverdi O, Boylu U, Kendirci M, et al. The learning curve in the training of percutaneous nephrolithotomy. Eur Urol. 2007;52(1):206–12. doi: 10.1016/j.eururo.2007.01.001
- Budak S, Yucel C, Kisa E, et al. Comparison of two different renal access techniques in one-stage percutaneous nephrolithotomy: triangulation versus “eye of the needle”. Ann Saudi Med. 2018;38(3):189–93. doi: 10.5144/0256-4947.2018.189
- Majidpour HS. Risk of radiation exposure during PCNL. Urol J. 2010;7(2):87–89.
- Falahatkar S, Allahkhah A, Soltanipour S. Supine percutaneous nephrolithotomy: pro. Urol J. 2011;8(4):257–264.
- Vicentini FC, Torricelli FC, Mazzucchi E, et al. Modified complete supine percutaneous nephrolithotomy: solving some problems. J Endourol. 2013;27(7):845–849. doi: 10.1089/end.2012.0725
- Barut O, Resim S. Comparison of access tecniques in treatment of renal stones with percutaneous nephrolithotomy. Annals of Med Res. 2019;26(12):2881. doi: 10.5455/annalsmedres.2019.09.572