ABSTRACT
The 12th Annual European CME Forum (#12ECF) was held 6–8 November 2019 at the Barnes Wallis building in the University of Manchester, Manchester, UK. An international group of attendees participated in highly interactive learning sessions, ranging from workshops to panel discussions to oral presentations by poster authors. Breakout session themes addressed continuing medical education (CME) from the perspective of the learner (micro-practice); collaborations, partnerships and interprofessional approaches (meso-practice); and consideration of compliance and regulatory issues (macro-practice). Topics covered included standards for accreditation, doctor-patient communication, a framework for CME educators’ professional development, capacity building and a futurist viewpoint of continuing professional development (CPD) from a global perspective. The high level of engagement by learners set a solid foundation for further collaboration among stakeholders in European CME.
12th Annual European CME Forum
The 12th edition of the Annual European CME Forum (#12ECF) continued its recent practice of using a venue with iconic connections, as described in the reports of the 2016 [Citation1], 2017 [Citation2] and 2018 meetings [Citation3]. Between 6–8 November 2019, attendees from Europe, Asia and the Americas convened in the Barnes Wallis building at the University of Manchester, UK. The building () was opened in 1967 by Sir Barnes Neville Wallis, 24 years after his most famous exploit – the development, testing and implementation of the “bouncing bomb” strikes of Operation Chastise used by the Royal Air Force to damage the strategically important Ruhr dams during World War Two. These events were famously depicted in the 1955 film The Dam Busters, with Sir Michael Redgrave playing the role of Barnes Wallis.
Development, testing and implementation strategies also featured in many of the presentations and workshops during the 3-day forum, which was centred around three key workshop themes:
Micro-practice: the perspective of the learner
Meso-practice: collaborations, partnerships and interprofessional approaches
Macro-practice: consideration of compliance and regulatory issues
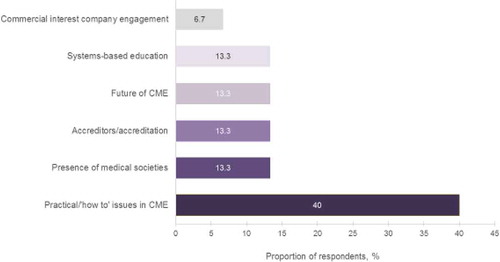
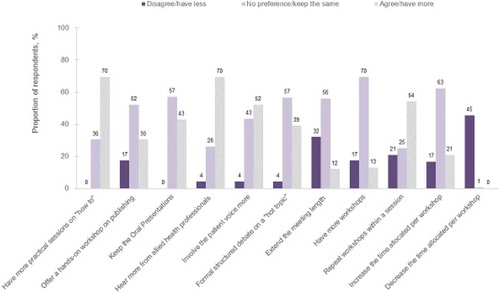
The meeting was planned and implemented using the best practice principle to include session topics based on results of the #11ECF post-meeting survey. Respondents’ top preferences were the inclusion of more practical “how to” sessions, more from allied health professionals and to repeat workshops within a session ( and ).
Day 1
The Good CME Practice group (gCMEp; www.gcmep.org) opened Day 1 with a pre-conference orientation session outlining the current roles and interactions among stakeholders in European continuing medical education (CME). In the opening address, Eugene Pozniak, the Programme Director for #12ECF, followed with a review of the main events in European CME during the previous year, as well as the potential effects of Brexit. Developments included the European Federation of Pharmaceutical Industries and Associations (EFPIA) Code update in August 2019 to include for the first time specific guidance on support of medical education in the new Article 16 [Citation4], the agreement of mutual recognition of CME credit between the American Medical Association (AMA) and the European Board for Accreditation in Cardiology (EBAC) [Citation5] in October 2019, as well as the reaffirmation by the Accreditation Council for Continuing Medical Education (ACCME) of substantial equivalency of the two accreditors [Citation6]. The focus on interaction during the forum was emphasised by Chris Elmitt of Crystal Interactive who acted as moderator for many of the sessions and provided live polling and feedback technology. Various opportunities for interaction during the meeting were also described within the programme ().
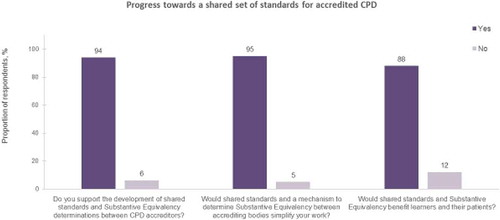
The opening session of the conference was presented by Kate Regnier, Executive Vice President of the ACCME, with colleagues Michel Smith of the Royal College of Physicians and Surgeons of Canada (RCPSC) and Jörg Stein of the European Cardiology Section Foundation (ECSF) [Citation7]. This session provided a report from the International Academy for CPD Accreditation on the progress towards a shared set of standards for accredited continuing professional development (CPD) (). The Academy accepted the task of identifying international CPD accreditation standards that reflect shared values and principles by which accreditation systems could be evaluated and determined to be substantively equivalent. The working group put forward a set of domains for consideration as follows:
Domain 1: Eligibility and administrative responsibilities of an accrediting body
Domain 2: Independence and transparency in accredited education
Domain 3: Needs assessment in the planning of accredited education
Domain 4: Content validity in accredited education
Domain 5: Quality of educational design in accredited education
Domain 6: Outcomes from accredited education
A common set of terms and a glossary have also been produced to support the proposed shared standards and these were provided to learners during table discussions to consider the positive and negative implications of the standards.
Figure 5. Proposals for shared standards for accredited CME/CPD [Citation7]
![Figure 5. Proposals for shared standards for accredited CME/CPD [Citation7]](/cms/asset/7a6f5cfd-c52d-46ca-a5fc-7f6e6f737333/zjec_a_1754121_f0005_oc.jpg)
The #12ECF learners indicated by polling with overwhelmingly positive responses that such standards would be well-received ().
Day 1 concluded with three concurrent “micro-practice” workshops:
Micro Workshop 1. Closing the Gap: Effective Communication between Patient and Doctor
Jeanette Andersen and Helga Ovens, patient representatives of Lupus Europe, moderated discussion on a series of cases that illustrated ongoing issues in doctor-patient communication [Citation8]. They presented a summary review by Ha and Longnecker [Citation9] and the contribution of the learners and facilitators led to the conclusion depicted in .
Figure 7. Benefits of effective doctor-patient communication [Citation8]
![Figure 7. Benefits of effective doctor-patient communication [Citation8]](/cms/asset/29c85adc-62ac-4d5c-ad78-076eb1d9b528/zjec_a_1754121_f0007_oc.jpg)
Micro Workshop 2. Professional Development of the Healthcare CPD Professional
Steven Kawczak of the Cleveland Clinic and past president of the Alliance for Continuing Education in the Health Professions (ACEhp) described a range of competencies deemed appropriate for healthcare educators at various stages in their careers [Citation10]. Competency areas and specific learning competencies within each area, developed by ACEhp, were described in detail and learners worked in teams to design and describe some strategies for competency development. The main benefits of using the competency model () were:
Incorporating adult learning principles
Providing a template for planning
Managing and leading a team
Staffing & recruiting
Providing benchmarks for career progression
Figure 8. Competencies for healthcare CPD professionals [Citation10]
![Figure 8. Competencies for healthcare CPD professionals [Citation10]](/cms/asset/1f4c31fd-19d9-4643-8678-e72f40628f8c/zjec_a_1754121_f0008_oc.jpg)
Micro Workshop 3. The Master Adaptive Learner
Don Moore of Vanderbilt University provided a comprehensive description of the master adaptive learner and elicited consideration of a role for such learners in clinical practice and CME/CPD [Citation11]. The concept of adaptability was introduced as the difference between routine and adaptive expertise. Don Moore highlighted the importance of preparing physicians for future learning as master adaptive learners whilst balancing innovation and efficiency in caring for patients, whether in routine or complex clinical situations. A similar approach could also be implemented in preparing CME/CPD professionals to become master adaptive learners.
The main aspects of Moore’s conceptual approach are summarised in .
Figure 9. Phases of adaptive learning mastery [Citation11]
![Figure 9. Phases of adaptive learning mastery [Citation11]](/cms/asset/c9d716ee-06f2-4f96-8687-b9337d47769b/zjec_a_1754121_f0009_oc.jpg)
Day 2
Day 2 began with a session moderated by Chris Elmitt during which the workshop leaders and learner scribes from the previous day’s micro workshops reflected on their shared experiences during each session. Discussion then led to the emergence of some common themes from each workshop. These included the need for educators to make logistical and skill changes and the need to value teamwork and move beyond perceived barriers such as “lack of time”, as exemplified by the typical doctor-patient interaction called the 7-minute encounter. Furthermore, it was concluded that an essential element to continuous improvement is the need for open collaboration with experts outside the CME/CPD community.
Oral Presentations
Two poster authors were invited to give oral presentations to the forum during separate sessions on Days 2 and 3.
The first of these, entitled “1 hr on-call”, was presented by junior clinical fellow Jyothis Manalayil of Blackpool Teaching Hospitals NHS Foundation Trust [Citation12]. Jyothis Manalayil described a simulation programme designed to let final-year medical students experience the pressures of being on-call, where positive feedback from each small cohort was reported ().
Figure 10. Simulation of the on-call experience for final year medical students [Citation12]
![Figure 10. Simulation of the on-call experience for final year medical students [Citation12]](/cms/asset/c2616c5b-bb2e-46e6-b016-eb11ab6bb476/zjec_a_1754121_f0010_oc.jpg)
“Meso-practice” workshops completed the morning of Day 2:
Meso Workshop 1. Creating a Learning Organisation
Having first discussed the characteristics of a learning organisation, Miriam Uhlmann, Manager of Faculty Development at the AO Education Institute, prompted learners to identify characteristics of their own workplace that could align people, processes and purposes to support the creation of a learning organisation [Citation13]. Her description of such an organisation was one that facilitates continuous learning of its members and continuously transforms. Some salient features of such an entity were listed as:
Maintaining levels of innovation and remaining competitive
Being better placed to respond to external pressures
Having the knowledge to link resources efficiently to customer needs
Improving the quality of outputs at all levels
Increasing the pace of change within the organisation
Creating a supportive learning environment
Having leadership that reinforces learning
Some attributes of a high performing learning system are outlined in .
Figure 11. Example of the alignment of attributes in a learning organisation [Citation13]
![Figure 11. Example of the alignment of attributes in a learning organisation [Citation13]](/cms/asset/a7d9ba40-9ff5-4e39-8758-286fc310aa2c/zjec_a_1754121_f0011_oc.jpg)
Meso Workshop 2. The Changing Life of the CME Provider in Europe: What’s New?
Members of the gCMEp conducted a workshop to discuss the current perception of the status of CME in Europe as seen by stakeholders as well as the public scrutiny from media and regulatory bodies [Citation14]. The structure of the workshop was based on the learning objectives shown in . The workshop elicited ideas on new formats such as micro-learning and considered the core principles to underpin effective, quality CME.
Figure 12. Learning plan to consider the changing face of CME in Europe [Citation14]
![Figure 12. Learning plan to consider the changing face of CME in Europe [Citation14]](/cms/asset/57b668b9-4229-4135-a0f6-0158e9d5eacd/zjec_a_1754121_f0012_oc.jpg)
Meso Workshop 3. Applying the Capacity Building Model to CPD: A Real-world Collaborative Example
After a theoretical introduction by Don Moore, Jann Balmer, Gretchen Keefer and Ian Harding provided details of a transatlantic project based on an adaptation of capacity development for healthcare improvement [Citation15].
Capacity development was defined as the process through which an organisation and its constituent parts identify, develop and maintain the capabilities to set and achieve their own goals and objectives over time. This approach identifies capacities as its starting point and then supports efforts to enhance and retain existing capacities and develop new capacities necessary for success. Such capacities are seen to exist at three levels analogous to the macro, meso and micro descriptors applied to the series of workshops conducted at #12ECF. These levels are:
The enabling environment: the broad social system within which people and organisations function, consisting of rules, laws, policies, power structures and social norms.
The organisational level: refers to internal hierarchy, policies and procedures that determine an organisation’s effectiveness. The potential for growing capacity is directly related to the resources available and degree of alignment of these elements.
The individual level: the skills, experience and knowledge from formal or informal education and training that allow each person to perform.
Within each level five separate steps can be identified ().
Figure 13. Steps involved in capacity development [Citation15]
![Figure 13. Steps involved in capacity development [Citation15]](/cms/asset/ef61c09f-8db0-4d19-a0e5-c25c6ff2b2c8/zjec_a_1754121_f0013_oc.jpg)
Details of a grant-funded initiative involving six institutions in the USA and UK that provide immunotherapy care to cancer patients were presented. It is hoped that after a pilot project these institutions will incorporate capacity building to improve other systems-based procedures. The goal of the pilot project is to help organisations to identify gaps in development or delivery of immunotherapy care protocols and to accelerate individual, team and organisational changes to improve immunotherapy care.
The desired outcome is to drive organisational and systems-based change at micro, meso and macro systems levels that are specific and responsive to the needs of the clinicians, teams, patients and programmes in each institution.
Lunch with the Learners
The “Lunch with the Learners” session has become increasingly popular among European CME Forum attendees. At the forum this year, two clinical fellows from local hospitals answered audience questions about their personal perspective on CME. Both learners indicated that the lifelong role of CME/CPD had not been clearly explained to them during their initial training. The learners indicated that they were only now becoming aware of the instructional design and outcomes-based approach utilised by CME providers. Both learners stated that while they would be open to follow-up to assess practice change as a result of CME initiatives, such engagement may not be the norm among their peers. Incentives for engagement were recommended as being important to consider in the planning and implementation of CME and collegial learning was put forward as an example of such an incentive. A typical reaction from the attendees was that it was a “great reality check on the learner perception of CPD”.
Meso Workshop Reflection
Once again there were linkages that emerged from the workshops. Microlearning may be a way forward and can contribute to a culture of learning as seen in learning organisations and can be supported by the capacity building model.
Day 2 concluded with a final set of concurrent workshops under the umbrella of Macro-practice.
Macro Workshop 1. The Evolving Role of the Specialist Societies in Europe
This workshop led by Julie-Lyn Nöel of Eurospine provided an opportunity for participants to consider the status of scientific medical societies in Europe ()[Citation16].
Figure 14. European medical societies’ workshop objectives [Citation16]
![Figure 14. European medical societies’ workshop objectives [Citation16]](/cms/asset/e62bb955-58db-4ffb-a8f2-4710f1361b97/zjec_a_1754121_f0014_oc.jpg)
Consensus emerged that medical societies, being varied in their organisational structure, need to have a unified system to allow discussion and advocacy. An umbrella organisation, such as the Biomedical Alliance in Europe, might be able to provide much-needed collaboration in responding to public health issues and navigating different healthcare systems in the diverse European situation. The importance of outcomes measures beyond attendance and satisfaction was emphasised and a call to action for more “professionalisation” of CME was agreed.
Macro Workshop 2. Preparing the Medical Education Community for the Healthcare Evolution and Its Impact on Medicine
Thomas Kellner (UCB) and Celeste Kolanko (Liberum IME), representing the Global Alliance for Medical Education (GAME), reported on the recent Futurist Forum organised by GAME [Citation17]. They presented highlights of the results from dialogue with futurist leaders. In line with output from other #12ECF workshops, the futurist view included greater emphasis on:
Collaboration among institutions
Patients taking more responsibility for their own healthcare
Simulation and the use of Artificial Intelligence in learning
Use of Big Data
More workplace-based learning
Some of these predictions link with issues such as the increased role of data scientists and behavioural scientists as well as patients in shared clinical decision making. A graphical representation of some of these changing roles is shown in .
Figure 15. Futurist predictions for healthcare professionals’ learning [Citation17]
![Figure 15. Futurist predictions for healthcare professionals’ learning [Citation17]](/cms/asset/5256b53b-bfea-4fb9-9146-009ba1ae5cb7/zjec_a_1754121_f0015_oc.jpg)
Macro Workshop 3. Round the CPD World in 90 Minutes
Lawrence Sherman (AMEE, Meducate Global) conducted an informal workshop that provided practical tips on how to succeed in different countries when designing and implementing CME/CPD activities. This highlighted that very different approaches to independent CME exist around the world and that challenges exist for providers in staying on top of local compliance requirements and language and cultural barriers. To that end, the importance of involving local medical professionals who understand the cultural nuances was emphasised. It was also important to note that accreditation of CME/CPD activities does not exist in all countries so that a yardstick for meeting needs may not be in place. Local contacts and use of available technology were also listed as important factors.
Day 3
Following reflections on the previous day’s Macro workshops, a second oral presentation from the poster authors, entitled “An ecological approach to improving Public health CME for GPs” was made by Thomas Roux of University College Dublin [Citation18]. Thomas Roux described his doctoral study involving the application of a theoretical framework to support the development of relevant and timely Public Health CME to ensure that GPs remain competent in the face of changing population and practice dynamics. Thomas Roux’s poster presentation of this mixed-method systematic review is shown in .
Figure 16. A theoretical framework for CME improvement [Citation18]
![Figure 16. A theoretical framework for CME improvement [Citation18]](/cms/asset/5e28e7d7-882f-42f2-a3f9-ddfa720bd7d4/zjec_a_1754121_f0016_oc.jpg)
Corridor Consult
A panel consisting of Margarita Velcheva of Kenes (provider), Thomas Kellner (pharmaceutical industry), Leonard Harvey of UEMS-EACCME (accreditor) and David Vodusek of BioMed Alliance (medical society), representing the spectrum of CME stakeholders, considered a series of scenarios with input from the attendees.
The scenarios and main responses included:
Satellite symposia should be accredited: The panel were mostly in accordance that these should not be accredited if produced by industry. However, it was pointed out that such activities may be educationally sound by adhering to independent medical education principles without any input from industry.
Promotion of a new drug in a CME event: This was regarded as being against the EFPIA code as well as being unacceptable as CME.
Funding for medical society guidelines update: Tools to evaluate guidelines and identify undue influence are available to mitigate promotion appearing in guidelines. The role of the Good Publishing Practice was also mentioned.
Use of tradenames: The panel noted that this should normally be resolved prior to a presentation but one attendee commented that the mere mention of products does not necessarily equate to their promotion, particularly when the benefits and limitations are discussed equally.
A futurist viewpoint: Use of big data is now a vital component of drug development and approval and will be more relevant to stakeholder collaboration and a patient-centric approach. More locally based education, particularly for GPs, will require adaptation by accreditors.
The CME Unsession
Lawrence Sherman conducted the now familiar “CME Unsession”, where attendees ask final questions or provide feedback. The main talking points that arose were:
Integration of the master adaptive learner concepts into instructional design
Case-based learning should challenge the learner to go beyond the edge of their expertise
Interprofessional education – learning within and across teams
The most valued format for CME is discussion based and learning together
Comparison of different accrediting bodies in Europe to determine alignment
Patient inclusion
Commitment to change
Alternative sources of needs data such as electronic health records
Conclusions
The unprecedented level of interaction during #12ECF was appreciated by learners, as evidenced by polling results obtained during the meeting. The majority of attendees found the workshop sessions to be relevant to their CME/CPD role and either identified ways to make practice changes or felt that their learning from the sessions reinforced their current practice. The final task for attendees was to submit a commitment to change as a result of attendance at #12ECF.
Presentations delivered at the 12th European CME Forum are available at the European CME Forum website (www.europeancmeforum.eu) and a Twitter stream is accessible at @eCMEf.
The 13th Annual European CME Forum (#13ECF) will take place 4–6 November 2020 at the NH Collection Barcelona Constanza Hotel, Barcelona, Catalonia, Spain. This highly interactive meeting is geared towards the key stakeholders of European CME as well as anyone with an interest in global CME/CPD.
Disclosure statement
No potential conflicts of interest were reported by the authors.
References
- Murray R. Report on proceedings of the Ninth Annual European CME Forum, Amsterdam, the Netherlands, November 2016. JECME. 2017;6(1):1302672.
- Murray R. Report on proceedings of the Tenth Annual European CME Forum, Dublin, Ireland, November 2017. JECME. 2018;7(1):1421376.
- Murray R. Report on proceedings of the Eleventh Annual European CME Forum, King’s Fund, London, November 2018. JECME. 2019;8(1):1613861.
- European Federation of Pharmaceutical Industries and Associations. EFPIA code of practice. Brussels: European Federation of Pharmaceutical Industries and Associations; 2019.
- American Medical Association. Agreement with European Board for Accreditation in Cardiology (EBAC). [cited 2020 Feb 27]. Available from: https://www.ama-assn.org/education/ama-pra-credit-system/agreement-european-board-accreditation-cardiology-ebac
- Accreditation Council for Continuing Medical Education. ACCME December 2019 Board of Directors Meeting Executive Summary. Chicago: Accreditation Council for Continuing Medical Education; 2020.
- Regnier K, Smith M, Stein J. Progress towards a shared set of standards for accredited CPD: a report from the International Academy for CPD Accreditation. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Anderson J, Ovens H. The voice of the patient in educating the healthcare team. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38–12.
- Kawczak S. Professional development of the CPD professional. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Moore D. The master adaptive learner. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Manalayil J. 1HR on-call. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Uhlmann M. Creating a learning organisation. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Wilson S, Neve M. The changing life of the CME provider in Europe: what’s new? 12th Annual European CME Forum; 2019 November 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Keefer G, Balmer J Applying the capacity building model to continuing professional development – a real world example. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Nöel J-L. The evolving role of specialist societies in Europe. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Kellner T, Kolanko C. Preparing the medical education community for the healthcare evolution and its impact on medicine. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/
- Roux T. Applying an ecological theoretical framework to CME research: a working example. 12th Annual European CME Forum; 2019 Nov 6–8; Manchester, UK. [cited 2020 Feb 27]. Available from: http://europeancmeforum.eu/12ecf/