ABSTRACT
Purpose
Myalgic Encephalomyelitis (ME) is a chronic neurological illness also known as Chronic Fatigue Syndrome (CFS). Key symptoms are extreme fatigue, post-exertional malaise, cognitive problems and sleep disturbance. With reported higher levels of online activity for people with ME/CFS than other conditions, more knowledge of characteristics and experience of online use in everyday life is needed. This scoping review systematically identified, appraised and synthesised what is known on how people with ME/CFS use the internet.
Method
The following bibliographic databases were searched: Embase, Medline, PsychINFO, Cinahl, AMED, and ASSIA, plus Web of Science, ProQuest Dissertations & Theses Global, Scopus, and Google Scholar for grey literature. Two reviewers independently screened title-abstracts, and full text of studies against inclusion criteria. Remaining studies were quality-assessed using appropriate critical appraisal tools.
Results
Many people with ME/CFS go online daily to gain information and share experiences of their illness including difficulties with family, friends and doctors. Reciprocity of emotional and social support was found with a sense of in-group belonging and empowerment. Validation was sought online, and identity renegotiation took place. Some replacement of offline social support for online engagement was reported. Online lay expertise was seen to improve offline health professional relations but not replace them.
Conclusions
The internet is a valued source of support for people with ME/CFS in terms of sharing of experiences, legitimacy, empowerment, and integration into people’s everyday lives. The extent of interrelating of online and offline lives is not clear however and needs further investigation.
Introduction
Myalgic encephalomyelitis (ME) – meaning inflammation of the brain and spinal cord – is a long-term chronic neurological illness, often fluctuating in nature, that causes many symptoms affecting many bodily systems, most commonly the nervous and immune systems [Citation1]. Since 1988, the illness has also been known as Chronic Fatigue Syndrome (CFS). Many publications and researchers use both ME and CFS terms interchangeably and so we have operationalised both names as suitable for inclusion in this review. It is worth noting however, that debate exists in defining and classifying the two and there is evidence of distinct historical trajectories of ME and CFS, with distinguishing features of diagnosis and as such, including both names together could create additional issues surrounding the condition [Citation2]. Studies have reported however, that despite this debate, certain core symptoms of the illness do appear to be consistently present across both classifications, namely extreme fatigue, post-exertional malaise, neuro-cognitive difficulties and sleep disturbance [Citation3].
People with ME/CFS are significantly more impaired in both physical and social functioning than other long-term illnesses [Citation4–6]. The illness has a negative impact on people’s relationships and social networks, with suicide ideation endorsed more frequently in those experiencing unsupportive interactions and social distancing [Citation7, Citation8]. Due to the contested nature of the condition (no available biomarker; diagnosis is subjective), the legitimacy of the illness is often questioned in immediate social support networks, causing additional stress [Citation8, Citation9]. As Bowling states, lack of social support, participation and contact is associated with increased mortality risk and delayed recovery from disease [Citation10]. In a survey by Action for ME in 2019, 94% of participants had stopped or reduced social contact, and up to 97% of the 4038 participants said they felt socially isolated because of their condition [Citation11]. Patients describe feeling overwhelmed and let down when disbelieved. When seeking help was unsatisfactory, sufferers responded to this by taking more responsibility for their illness management via ‘self-help’ tactics such as seeking social support and greater lay knowledge [Citation12].
There are reported higher levels of online activity among people with ME than other patient groups [Citation13]. Online peer-to-peer support that connects to other sufferers in the form of interactive websites and social media, is now highly valued in chronic illness [Citation14, Citation15]. Transcending geographic boundaries, the internet is convenient to those with limited mobility [Citation16, Citation17]. Online communities provide support for people with long-term illness with a growing reliance on social media in patients experiencing social isolation and who fear marginalisation because of their illness [Citation18, Citation19]. It also offers support to people otherwise limited by disability or stigma when accessing support offline [Citation20].
Uncertainty surrounding illness appears to be a driving factor for internet use for those with persistent illness [Citation21] with internet itself being an increasingly public experience as people share personal information and interact in public spheres [Citation22]. As Beck, Gurion & Sheva state,
users of the world wide web are no longer passive audiences of data consumers … but are active participants controlling the content of the information. They shape the quality of the data … (facilitating) the expression of emotions (output) and the input of emotional messages, thus developing and reinforcing important social ties between users, forming a system of relationships similar to ties of family and friendship. (2 p. 46)
Receiving problem-focused and emotion-focused support from others aids coping and thus becomes a primary driver of willingness to offer such support to others [Citation23]. Online users describe ‘social overload’ however, where people feel they’re giving too much social support to others and experience online group exhaustion [Citation24].
So how does online usage interplay with the ‘real world’, particularly for ME patients who are often housebound due to the chronicity of their condition? In general, there is a ‘sharp distinction between concepts from the virtual world online and the “real world” offline’ but ‘technology enters and is gradually integrated into people’s daily lives’ (Lie & Sorensen 1996 cited in [Citation25]). By a process of ‘domestication’ people adapt new technologies and bring them into their home, transferring elements of the physical world into the virtual environment, merging the two worlds and creating a much broader definition of reality. Understanding how people with ME use the internet to aid their illness management and enhance their experience of daily life is crucial in gaining insight into how informational and social support is found and utilised online and offline. It will shed light on how people’s overall support networks are created and maintained, as well as identify the benefits of such illness behaviour.
Kingod et al studied how people with chronic conditions experience online peer-to-peer social support and its influence on everyday life, in a systematic review of 13 papers, but none of them covered the illness ME [Citation26]. They found four main themes: identity, social support and connectivity, experiential knowledge that both strengthened social ties and supported offline ties, and collective voice and mobilisation. Allen et al also looked at chronic illnesses which included ME in a primary study of 30 people across varying conditions. They found that online support was sought in response to deficits in offline support; it was used to assist offline ties as well as substitute offline support [Citation27].
Both Kingod et al and Allen et al stressed the need for further research into understanding the boundaries of online and offline social dimensions and relevance in daily life; how the role of online ties serves within personal networks [Citation26, Citation27]. Essentially how do people decide who to turn to now they have greater choice in who contributes to their everyday illness management and coping? Having further advancement of knowledge in this area will inform healthcare practice social support initiatives and aim to improve services to those housebound with ME/CFS. It will also gain knowledge into the lack of support present in the home life of people with ME/CFS.
Initial searches revealed a lack of studies conducted in this area that focused on ME/CFS. Studies on other chronic illnesses have an element of transferability of their findings to ME/CFS and several papers were found here highlighting a topic worthy of attention. Preference for online support over offline support was highlighted in cancer and diabetes patients [Citation28], with a lack of real-world social support predicting active participation in online groups [Citation29]. The benefits of using social media in health communication include interaction with others, the availability of shared knowledge, widened access to health information, social and emotional support, and empowerment in their healthcare process [Citation30, Citation31]. As much as 75% of a sample studied by Kummervold et al found it easier to discuss personal problems online than face-to-face [Citation32]. Virtual communities appear to play an important role in meeting patients’ social needs; sense of community is positively associated with cancer patients’ well-being in areas of personal relations and personal growth [Citation33].
Caplan found that depressed people may develop preference for online social interaction but this in turn leads to negative outcomes associated with internet use [Citation34], and Allen et al concluded that internet use may indicate an avoidance or absence of offline support [Citation27]. Moreover, Chung found those dissatisfied with their offline relationships were more likely to develop preference for online social interaction and this can become problematic when excessive reliance increases disengagement from offline interaction [Citation28]. Findings are largely positive in that using the internet appears to improve everyday life, however there are studies that highlight negative impacts. Given that ME/CFS is a contested illness with legitimacy issues and increased stigma, will data collected from the ME/CFS community produce similar or different themes to other conditions?
This scoping review aimed to explore the online usage characteristics of ME/CFS patients and inter-relatedness within everyday life of their online and offline worlds. To prevent unnecessary duplication, a preliminary search for existing scoping and systematic reviews on the subject was carried out in May 2022. To our knowledge, a comprehensive synthesis of related studies on ME/CFS in this field remained absent.
Methods
The broadest scope of literature on the topic of online usage in people with ME/CF was achieved by scoping review methodology. A scoping review is ideal for mapping out the scope or coverage of a body of literature on a given topic when the emerging evidence is still unclear and more specific questions cannot presently be posed [Citation35]. They give a clear indication of available literature, regardless of study design, and an overview of its focus, identifying characteristics of studies to provide an overall picture of current evidence [Citation36]. To map our field of study and examine the extent, range and nature of research activity to date, as well as identify any knowledge gaps in research, our process was developed using a framework set out by Arksey & O’Malley [Citation37]. We have also incorporated later improvements to this framework by the work of Levac and colleagues [Citation38], and the Joanna Briggs Institute [Citation39]. Guidance from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews checklist (PRISMA -ScR) has been consulted to yield greater transparency and reproducibility [Citation39].
Research question
We aimed to answer the following question: How do people with ME/CFS use the internet? This was achieved by addressing the following three objectives and sub-questions:
Examining the usage characteristics of people with ME/CFS utilising the internet. (What do they do online, when, and for how long?)
Examining people with ME/CFS’ experiences of online usage. (Why do they go online and what do they gain from going online?)
Examining people with ME/CFS’ online usage inter-relating with their offline lives. (e.g. how does using the internet fit in alongside their offline daily lives?)
Study eligibility
We found both published and grey literature studies. Loosely using a PCC (Population, Concept, Context) framework to develop our inclusion criteria, to align with our objectives and research questions, our population was adults identified as having ME/CFS. Our concept of interest was internet use. We defined ‘internet use’ as the computer network that allows users to connect with other users and content from all over the world [Citation40]. Online information, content and social support exist through many various technological avenues nowadays. Kaplan & Haenlein operationalised ‘social media’ usage in five main categories: collaborative projects, blogs, content communities, social networking sites and virtual worlds [Citation41]. Gaming is also an online social experience now as it is shared live with other users. The context is loosely any available knowledge that involves personal use of the internet and not organised institutionalised treatment agendas.
Search strategy
An initial literature search of Web of Science was conducted and from analysis of these results, key words and index terms were identified. A reference librarian was consulted in preparation, and a systematic search plan was formed with search terms incorporating medical subject headings (MeSH) as well as text words combining comprehensive terms for contemporary social media, and Boolean operators ‘AND’ and ‘OR’ ( shows an example search strategy of keywords for Web of Science. This was adapted to suit individual databases).
Table 1. Search strategy example for web of science.
Extensive electronic searches of the following bibliographic databases were conducted (in Aug to November 2022): EMBASE, Medline, Cinahl, PsychINFO, AMED. And ASSIA. Bramer et al found that optimal searching to ensure a minimum risk of missing studies, should use four key databases: Embase, Medline, Web of Science and Google Scholar [Citation42]. This produced a 98.3% recall of studies. Grey literature was also searched, namely Scopus, Web of Science, and ProQuest Dissertations & Theses Global taking place during November 2022. Web searching via Google Scholar was also conducted (first 200 entries) as well as citations and references of key papers searched by hand.
All eligible studies that met our inclusion criteria (adult participants over 18 years of age identified as having ME/CFS, focus on personal internet use, published in English language peer-reviewed primary studies) were saved on an Excel spreadsheet. Our exclusion criteria were studies focused on child participants (under 18 years of age), participant groups not identified as having ME/CFS, non-internet use studies, and not systematic reviews since their content is already secondary in nature, so analysis would further dilute and potentially bias findings.
Study selection
The primary researcher ran the initial searches, retrieved titles and abstracts, removed duplicates, and saved all files into a suitable data management storage. Two reviewers went through the title and abstract of each study and screened them to identify studies that met the inclusion criteria, and we documented all results in a ‘screening’ form. Reference lists of included studies were then examined by the lead reviewer to identify any eligible studies that met the inclusion criteria, and were then added to the database findings. Forward searching of papers, via Scopus, that have been cited, were also checked.
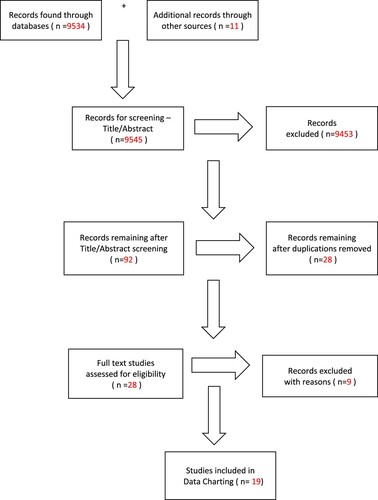
Two independent reviewers then read the full text of all provisionally included studies and assessed further against the inclusion and exclusion criteria. The devised extraction form was piloted to ensure it contained all relevant information needed. Studies were included or excluded against the pre-determined eligibility criteria. Any discrepancies were resolved within the research team. All reviewers agreed on the final list of included studies. A PRISMA-ScR flow diagram [Citation42] following the process of the scoping review was used to demonstrate the selection process ().
Critical appraisal
The original methodological framework set out by Arksey & O’Malley did not include appraisal but we chose to assess the remaining eligible studies for quality assessment [Citation36]. This took place after the data extraction of full-text studies. Pham et al reported only 22.38% of studies included an element of quality assessment [Citation43]. McColl et al argue that the emphasis of a scoping review is on comprehensive coverage and not standard of evidence [Citation44]. More recent refinements to guidelines however, support the use of some form of critical appraisal [Citation35, Citation38]. Brien et al believe a lack of quality assessment makes results more challenging to interpret and Grant & Booth believe it limits the uptake of findings into policy and practice [Citation45, Citation46]. Daudt considers quality assessment a necessary component of any scoping review and encourages the use of validated tools since the use of reporting checklists increases transparency of methods and allows the reader to use the research appropriately [Citation47]. Pham et al also recognises that some form of quality assessment would enable the identification of gaps in the evidence base rather than just where research is lacking [Citation43].
A quality assessment form was used to extract relevant data for appraisal. We chose the Critical Appraisal Skills Programme [Citation48] for qualitative studies. Any mixed methods studies found were appraised using the Mixed Methods Appraisal Tool [Citation49]. Any quantitative data found was appraised using the Checklist for Analytical Cross-Sectional Studies. No exclusion of eligible studies took place during appraisal since such studies can still contain rich and useful qualitative narratives. The qualitative checklist data can be found in full in supplement 1.
Results
Findings of individual studies were inputted into a data table to answer our research aim of how people with ME/CFS use the internet, as well as gain relevant information pertaining to demographics, recommendations and quality assessment. Please refer to .
Table 2. Study characteristics, quality assessment & results.
Demographics: Study dates ranged from 1997 to 2021, with the vast majority taking place in the last 10 years. Publication types for included studies were mixed: 11 were journal papers, 4 were book chapters, 1 was a magazine article, and 3 were PhD theses.
14 studies used samples of online social media content (including Facebook posts, blogs, forums and a virtual platform), 1 used an official website, and 4 interviewed online users directly (of which 3 compared ME/CFS users with other chronic conditions).
In terms of demographics, of the papers that stated a country of study, 8 of the 17 were conducted in the UK, followed by 4 in the USA and 4 in Norway. Australia and Spain also featured in studies. Of the 5 studies that recorded age, 2 had a mean age of 50, with 40–50s age group dominating all studies. Of the 8 papers that stipulated gender, all had a high majority of female participants (at least 75%). 2 studies stated the educational achievements of their participants and both were well above the 27% average of participants possessing a higher education degree (70–71%).
Areas of research focus varied. 36% (7 papers) were on the topic of identity and participation. 21% (4 papers) examined the experience of going online, and 1 investigated the effect of this online experience. 16% (3 papers) studied the notions of empowerment and online social movements. 3 papers discussed trust and privacy but were all linked by the same population sample. 2 papers obtained data on online behaviour and 1 paper looked at potential issues of online communication interaction.
Study design was heavily weighted (78.9% of papers) towards qualitative data collection and analysis. Only 2 of the 19 papers used quantitative means of collecting statistical information of online usage and sample demographics, with an additional 1 paper using mixed methods of both quantitative and open-ended qualitative questions.
Recommendations: Five papers suggested further investigation to obtain a greater understanding of online use as an empowering community and means of social change [Citation50–54]. Other papers suggested further study on health professionals' concerns over online support and acquisition of lay knowledge [Citation55, Citation56]. Three papers wanted to see research into the significance of the digital divide and technical issues of using the internet [Citation56–58]. Further suggestions were exploring the content and significance of the internet in society and the impact of this online support on quality of life, looking at how online support aids identity work and a sense of agency, and further investigation into the type and quality of available information on online forums [Citation13, Citation59–61].
Quality Assessment: There were 16 qualitative studies, two quantitative studies and one mixed methods study. Four of the 16 qualitative studies were written papers derived from data gathered in three included theses, which meant 12 individual studies of raw data. The overall quality of these papers, using the Critical Appraisal Skills Programme tool [Citation48], was good but lacking in certain areas of detail. All papers had clear aims and their use of qualitative data was appropriate for the research questions being asked. Research design was also suitable, given the research objectives, in all papers, but methodology was not detailed in three of the studies and in two of the studies the chosen methodology was not justified, therefore only meeting CASP criteria on the basic level. Sample recruitment was appropriate to the CASP form but was explained in varying levels of detail.
All but one of the studies failed to meet the CASP criteria for consideration of the relationship between researcher and participant. Little attention was given to the concept of researcher bias with 11 of the 16 studies making no mention of risk of bias at all. Ethical issues were not discussed in 5 of the studies. Justification for not gaining ethical approval was argued by referring to online data as public data and not private. Anonymity of participants was also mentioned. In terms of data collection, this was done sufficiently to meet CASP criteria in 14 of the 16 papers, but the degree of explanation varied, and some were implicit but not described in detail. Data analysis descriptions were poor or non-existent in a quarter of studies. Findings were however clearly described and discussed in all studies. Any contradictory data were not mentioned in any of the papers although surprising results were discussed in three of the studies. Papers stated how their research could not be transferred and generalised to the wider population due to sampling methodology used. Results were discussed however in relation to existing literature and previous research.
To summarise, whilst the methodology in most qualitative studies was of good or acceptable standard, the analysis process was not always written in sufficient detail and the lack of attention to potential biases was a worry.
The quality of the two additional studies of quantitative data was moderate to poor. The study by Knudsen et al. was not documented well and involved only basic research methodology [Citation60]. Confusion exists around the sample of participants as medical conditions were chosen that specifically affect young adults, yet the paper does not mention young adults anywhere else, only adults. Exposure and measurement details were unclear or missing and confounding variables were not mentioned. Reliability is likely to be poor due to only having one measurement point in time. Outcomes, whilst based on existing definitions of conditions, are troublesome since self-diagnosis or internet use by family members was not differentiated so over-reporting of figures is likely. The study by Tian et al has a better and more detailed methodological process but again analysis fails to rule out if traffic is new or returning visitors to the website so confounding factors could be of issue [Citation61]. These were not mentioned only in the limitations at write up. Outcome measures were standardised, but no detail given as to their reliability. One additional mixed methods study was of good overall quality [Citation62]. Quantitative data produced percentages of participants whilst qualitative data produced open-ended questions as narrative. Methodology was appropriate although it was not explicit how measures of central tendency and frequency distributions were used in analysis. No rationale for mixed methods design was given and qualitative findings were not discussed in any real detail. Any inconsistencies between quantitative and qualitative data were not mentioned.
How do people with ME use the internet? The studies that involved quantitative data revealed people with ME/CFS go online more than any other studied condition [Citation60, Citation63] The internet was used daily by half of a sample and weekly by 80% of a sample but only one study had researched this so these results cannot be generalised.
Several themes emerged within the studies overall. Common was the sharing of experiences of living day-to-day with the condition, revealing a sense of belonging in familiarity and commonality [Citation13, Citation51, Citation54, Citation56–58, Citation63, Citation64]. The experience of their struggles and difficulties with doctors and friends and family were often shared [Citation50–52, Citation56].
Reciprocity of emotional and social support through caring exchanges, via forum posts, provided moral support and encouragement [Citation13, Citation52, Citation54, Citation56, Citation63]. Users helped other members by sharing information and experience, which contributed to feeling good themselves, gaining a sense of purpose [Citation13, Citation56, Citation62, Citation63].
Following on from this, people with ME/CFS went online to gain information on the condition, on official sites as well as through knowledge sharing of forum users’ links and reading suggestions. There was scepticism over online content and a favoured leaning of the virtual community towards somatic approaches to treatments [Citation52, Citation56, Citation65, Citation66].
Being part of a virtual enabling community was welcomed, as a safe space away from family and friends, creating fellowship and belonging of an ‘in group’ with shared values and norms [Citation15, Citation52, Citation56, Citation59, Citation63].
Why do people with ME/CFS go online and what do they gain from going online for support? Several themes emerged from the studies. Social participation through the use of online social media provided an opportunity to go from being on the periphery of social life to full participation within a community of fellow sufferers, positioning themselves in social contexts again after the loss of ordinary contact with others. Through this participation came a voice and presence that negated isolation experienced by having ME/CFS [Citation13, Citation63, Citation64, Citation67].
Identity renegotiation was a strong theme in the studies with sufferers using online social support to transform life disruption (due to illness severity and loss of roles/relationships) into re-assertion and establishment of new selves over time, rethinking life plans and developing new identity not defined by loss. Empowering identity was formed through virtual connection in community participation; the inability to adopt a sick role (due to contested nature of the illness) and the resisting of health professional opinion leading to the establishment of patients as experts of their own illness, dealing with de-legitimisation by discrediting outsiders and constructing a more credible self-image [Citation50, Citation54, Citation59, Citation63, Citation64].
Online social support and connection with others gave opportunity for validation and legitimisation against the issues of contested illness experienced by people with ME/CFS. Their in-group narrative of descriptions of physical experiences, grounded in Western cultured medical discourse, was used against stigma and prejudice experienced in real life, asserting previously acceptable roles and distancing from the label of malingerer [Citation50, Citation54, Citation65].
Empowerment was another strong theme running through the studies. Following on from delegitimisation and stigma, posters on ME/CFS social media were united in working together to improve the social status of having ME/CFS. The groups’ norms, values, and goals guided the action of the community, sharing tips to cope with the medical system, promoting biochemical research and campaigning for change in public debate, plus seeking to address power balances between health professionals and patients [Citation13, Citation15, Citation52, Citation54, Citation56].
How does using the internet fit in alongside their offline daily lives? Results were less reported; only six studies researched this cross-over of online and offline worlds. Findings indicated that online identity was prioritised over the social identity of family/friends, and social support online replaced some of what was missing offline in terms of participation but that this was limited compared to the richness of face-to-face interaction [Citation13, Citation59, Citation67].
Online use enabled a ‘venting’ outlet away from their offline lives and anonymity was viewed as important, but both online and offline support were valued [Citation56, Citation57]. Online lay expertise was believed to improve offline engagement with health professionals, and support with daily living was found online that couldn’t be provided by health professionals, but this support was not seen to replace existing offline support but instead viewed as bridging the gap between services offered by medics and sufferers own day-to-day experiences [Citation51, Citation56, Citation58].
Discussion
This study used systematic scoping review methodology to investigate online user characteristics and experiences and their integration into everyday offline life. To our knowledge this is the first scoping review of its kind, taking a rigorous and transparent approach based on solid methodological framework, as well as being enhanced by a second reviewer for study selection and charting of results, and a quality assessment in accordance with study design.
All studies assessed reported high use of online support for sharing day-to-day struggles, reciprocity of emotional support and social participation in safe space virtual communities. Identity renegotiation, empowerment and establishment of patients as experts also emerged from the data, giving validation and legitimisation to the contested and stigmatised illness experience. Used as a venting outlet, social support online replaced some of what was missing offline, but not all, and lay experience was thought to improve offline engagement with health professionals.
Application of the inclusion criteria to the results of the searches identified 19 studies for inclusion in this review. Whilst ME/CFS is estimated to affect at least 7.6 million people in the world [Citation68], it is not surprising that so few papers were identified given the lack of serious interest in the illness historically. Piloting of the search strategy and supplementation of the results of the electronic searches with forwards and backwards citation searching and searching of reference lists of included papers allows confidence in the conclusion that all relevant research was included in this systematic scoping review and that conclusions arising from the review can be based on synthesis of all available evidence.
Overall, the methodological quality of included papers was good although often lacked in detail. Many of the studies were heavily weighted on female participants though, however ME/CFS does affect more women than men; women being at least three times more likely to develop the illness [Citation69, Citation70]. Having said this, women’s experience of the illness will be different from men so may give biased results. Murray, Day & Tobbell, found, in an analysis of English newspapers, portrayal of ME/CFS ‘differed meaningfully depending on gender’. An article of a woman suffering from the illness was highlighted with psychological and emotional elements foregrounded; a man however was given focus on physical elements with experience ‘accredited with greater legitimacy’ [Citation62]. As Bowling states, it’s a misconception that scientific research operates from an objective value-free neutrality. The reality is that scientists cannot remove themselves from the cultural, social, and political context they work from [Citation71].
Study authors raised the debate as to whether online social support via social media avenues should be classed as public or private data for the purposes of research and ethical approval. As Conrad, Bandini & Vasquez note, the internet is increasingly becoming a public experience as people share information and interact in public spheres [Citation22]. Should remote recruitment and data collection require similar data-sharing ethics procedures as ‘on-the-ground’ studies do? [Citation72]. There appears to be a general lack of clear guidance on conducting online research, with Arigo and colleagues highlighting challenges such as informed consent and maintaining anonymity and privacy [Citation73]. To always operate a ‘do no harm’ responsibility, ongoing consent may be more suitable than a one-off document that may not be read, but with third-party data, many are unaware of their contribution to research. Keeping participant confidentiality and anonymity in such cases may require no quoting verbatim to avoid posts being traced back to identify people [Citation74].
Data ownership implications remain problematic with 81% of participants of a microblog believing that researchers could not use their posts without consent [Citation75]. An ‘expectation of privacy’ in an essentially public environment remains controversial with many believing it is public, the poster bearing responsibility for choosing where and how privately to post. Anonymous forums are now also available to pool and share knowledge, providing social validation without risk of stigmatisation or being seen as inappropriate in other contexts [Citation76]. Privacy was rated as very important by 54% of patients when selecting a social media site to post about their health [Citation77]. This area of research ethics would benefit from stronger guidance.
Our review findings reported that people with ME go online up to 10-fold more often than other chronic conditions [Citation60]. Similar findings were also reported 25 years ago by Davison & Pennebaker who highlighted higher rates of participation than all other studied illness groups combined [Citation78]. We asked why do people with ME/CFS go online so much and what are they doing when online? Our results of, for example, reciprocal support, shared experience, information gathering, and sense of community were also found by Kingod and colleagues of other chronic illnesses [Citation26]. If all chronic illness yields similar internet use, why do people with ME in particular go online more often? As our introduction highlighted, 97% of participants of a large-scale survey of adults with ME, felt socially isolated because of their condition [Citation1], and lack of real-world social support predicted active participation in online groups [Citation29] with uncertainty surrounding illness also being a driving factor for internet use [Citation21]. Since ME is a contested illness with legitimacy being in question in immediate social support networks [Citation79], high levels of internet use were expected.
Patients with ME experience higher levels of stigma compared to other neurological illnesses [Citation80]. Davison, Pennebaker & Dickerson found support seeking to be highest in offline group participation for diseases viewed as stigmatising such as AIDS but in relation to online groups, people with CFS engaged in the highest level of support seeking [Citation51]. Allen and colleagues found online support was sought in response to deficits in offline support [Citation27] and Chung reported a preference for online support over offline support in cancer and diabetes patients [Citation7]. Our review found similar findings but only to a degree. Online identity was prioritised over social identity with friends and family [Citation59] and online support did replace what was missing in participation offline, but only in a limited capacity compared to face-to-face interaction [Citation13]; both online and offline support were valued [Citation56]. Outside of our review, offline support in the form of support groups for people with ME and Fibromyalgia found the most frequently endorsed benefits of membership were illness legitimisation, finding new information and feeling understood by others, but drop out reasons were inconvenience of location and time plus too sick to attend [Citation81] Internet use from one’s home has many advantages in terms of effort involved, making it more accessible for sufferers, something health professionals could utilise for management of the condition.
Other studies have found problems of reliance on online over offline support [Citation82], and online support can compromise efforts to seek offline support leading to depreciation of offline relationships [Citation83]. Those with diverse social networks were found to self-manage their illness better however [Citation84]. Apart from a study that indicated a third of participants experienced negative feelings because of online comments [Citation63], our review did not in general reveal any negative aspects to online usage, but data were limited on the interlinking of online and offline support. A study by Andreos and colleagues, on people with respiratory conditions, found that those with larger support networks communicated more openly and comfortably about their illness and shared its daily impact. The benefits of expanding their networks to include online peers were greater motivation and access to a supportive environment. Barriers however, included fear of being scammed and a preference for keeping illness-related problems to themselves and their immediate family [Citation85]. The study was on older adults though, which could explain such an opinion. Further, study into the integration of both online and offline support in a time–space dimension would aid in understanding of how the two constructs, reshapes, and constitutes daily life with ME/CFS.
Kummervold and colleagues found 75% of participants found it easier to discuss personal problems online than face-to-face [Citation32]. This fits in with findings for online use as an anonymous venting outlet away from offline lives [Citation57]. According to Bargh, McKenna & Fitzsimons, one’s true self is more likely to be active during internet interaction due to the anonymity of the online setting, but this can cause problems within established social circles and home life as feelings of closeness and intimacy can be hard to distinguish between what is the nature of internet use and what is genuinely due to the relationship itself [Citation86]. This could become troublesome if home life with significant others is under stress [Citation87–89]. Significant other relationships were only touched upon in our review [Citation56, Citation59] and further study into this area would be beneficial to understand the dynamics involved in patients’ daily lives; how much family members can help or hinder recovery.
Relationships with doctors and the emergence of lay expertise are something our review highlighted [Citation13, Citation15, Citation50, Citation52, Citation54, Citation56]. Being part of communities with a common cause to fight for biomedical recognition is something that up-skittles the traditional medical model’s view of doctor as expert. As Brooks, King & Wearden explain, patients, along with significant others, feel alarm when the knowledge and expertise they relied on are suddenly not able to provide definitive diagnosis or cure. Absence of adequate explanation from health professionals leads them to seek out answers for themselves [Citation90]. As they become more knowledgeable, their relationship with their doctor inevitably changes to one where they feel more equal to their physician. The relationship becomes challenged by this new form of educated empowered health consumer wanting to work in partnership [Citation18] and at times even knowing more than their medical service provider. This correction to the traditional asymmetry can result in negative doctor-patient encounters. In our review, lay expertise, achieved via online communities sharing successes and approaches to health professionals in a discourse of educating the ‘out group’, appeared to enhance the doctor-patient relationship rather than hinder it. Informed patients now bring with them the collective learning and advice of an extended health network of other patients and doctors [Citation90]. Going online to gain support with the psychological adjustment of living with illness also indirectly encourages approaches to management that doesn’t necessarily align with evidence-based recommendations [Citation91]. Tinkering with self-care offline can originate from Facebook support and exchanges of information creating person-centred knowledge about how to live with illness, that is situated to individual needs and unique daily living [Citation92].
It could be argued that medicine, in its attempts to be objective and removed from everyday contextualisation, has removed itself from the experiential meaning structure. Patients have quickly filled this gap by adopting online support groups, where their experience of illness is validated and welcomed as contributing to the general pool of knowledge of chronic long-term illness, something the medical model, with its ‘diagnosis, treatment and cure’ approach, has not delivered. This online support in our review [Citation13, Citation57] was not seen to replace existing offline help however, but instead merely complement it. Lian & Robson discuss medically unexplained symptoms and report that the main source of discontent of patients was not the lack of biomedical knowledge but doctors who fail to acknowledge the patients’ experience, describing how uncertainties in medical encounters are handled not in collaborative partnership but in a state of constant battle over the power to define their situation [Citation93]. The internet provides endless information which expands the range of narratives available, shifting the traditional doctor-patient relationship. Forums and blogs become sites of resistance as they provide space in which counter-narratives can be circulated [Citation54].
In online support communities, personal illness stories are validated and this fulfils a desperate need to feel connected and part of something bigger than ourselves. Our review highlighted empowerment and agency through online communities serving as social movements that contest medical power and generate a culture of shared norms and values. Such virtual symbolic communities foster co-operation, solidarity, support, and collective identity [Citation15, Citation52]. As a type of ‘self-help’, these groups allow individuals to assert responsibility for their illness and its management, acquiring social support and knowledge, key mediating factors in the emergence of control and acceptance [Citation12]. When patients have a voice, through mass media, they have an opening to change the social reality of the illness too, and this has been witnessed over the last decade especially with campaigns such as #MillionsMissing and ‘nothing about us, without us’ patient involvement in research. In the spirit of ‘small wins’, these social change efforts will continue to set about overturning mainstream opinion [Citation94].
Online communities play a big part in identity renegotiation of people with contested conditions in particular. In the absence of biomedical evidence, medical knowledge is instead constructed and developed through cultural meaning and historical interpretation. This shapes how society responds to a given illness which then affects the experience of that illness; the meaning of ME coming about through its interaction in social context [Citation95]. In our review, Cromby discusses this further with his concept of the ‘making up’ of people, where stereotypes of CFS patients may be accounted for because of people’s reasonable responses to their illness reinforced by the knowledge they’ve gained about its character, through online avenues [Citation65].
The inability to adopt a sick role in a contested illness such as ME, results in biographical disruption [Citation96]. In our review, online identity is prioritised over social identities of family or friends [Citation59]. Others’ denial of legitimacy of their situation means people with contested illness go through a chaotic period of rethinking and reconsidering all areas of their lives, juggling with restitution, chaos, and quest narratives [Citation97, Citation98], transitioning their identity to a reconstruction of self along with coping strategies [Citation99]. Our review revealed this transformation takes place largely through online social support channels where people’s illness experience is legitimised and accepted. Sites such as Facebook enabled a process of identity change, where supported individuals were able to move into full participation adapting to their renegotiated identities [Citation64]. As Sanchez points out, there are two dominant narratives operating in the larger cultural world; we either submit to medical authority and be cured (not possible for people with ME), or we remain chronically ill and discover greater meaning in life [Citation54]. The latter was present in our review as studies described this transformation of identity with the support of online communities. Individuals felt a sense of not belonging and being socially detached before gaining online support. They felt loss of their former self and even a legitimate place in society. Online interaction supported their process of transition to a new self which was valued more with no desire to return to their previous roles [Citation50, Citation59, Citation64]. They also find purpose and meaning in helping others on forums by offering experience and knowledge to those newly diagnosed [Citation63]. Groevelt highlighted that online social media use involved a ‘balanced positivity’ approach whereby illness was dealt with in a positive way with only occasional displays of hardship, a stark contrast perhaps to the stigma and disbelief of offline relationships [Citation100].
In previous research on people with ME/CFS, the invisible nature of the illness was of concern in studies [Citation101]. Other than through lack of belief and legitimacy of illness from immediate surrounding relationships, the illness as an invisible entity was not directly documented in our review. Could this be because, through campaigning and growing awareness of disabilities that are not visible, society is beginning to understand that illness can manifest in varying ways and many of which are not immediately obvious? In a recent study however, Khalafbeigi et al still found invisibility, as well as subjectivity of symptoms and fluctuation in severity to cause a lack of understanding leading to stigma [Citation102]. Further research into the impact of invisibility of ME/CFS on the acceptance of others would be useful here.
Only one paper in our search, by Morehouse 2021, yielded insight into the psychological impact of going online for social support, reporting that participation online appears to decrease depression and increase quality of life for people with ME [Citation63]. This is significant for not only helping those with ME/CFS but also their family members as studies show the negative impact on quality of life on those living with an ME patient [Citation103, Citation104]. Similar results to Morehouse et al have been found in other chronic illnesses, particularly those with stigmatised conditions. Yao, Zheng & Fan found the impact of online emotional support on psychological quality of life in people with Hepatitis B was most effective but also the influence of online support was dependent on the person’s perception of their level of social exclusion. Those with higher levels were more prone to seeking online support and therefore had greater benefit on quality of life [Citation105]. Brooks et al also found that the greater the subjective social support, the higher levels of self-compassion which in turn resulted in higher health-related quality of life [Citation106]. Further study on the impact of online social support on quality of life, and of those with stigmatised illness, is worthy of further investigation.
Conclusion
In conclusion, the use of the internet for information and social support is evident as a largely positive experience, benefiting those who use it by aiding the lived experience of ME/CFS. Gaining lay knowledge is empowering patients to play a greater role in their health care in addition to what is currently available. Online use supports identity renegotiation. In short, online communities are filling a gap in home self-care management and social participation. Studies on the impact of psychological use in everyday life have not been conducted enough to draw any confident conclusions. There is a need for greater understanding of the interplay between online and offline involvement in daily living, particularly in respect of significant others and family life, invisibility and stigma of contested illness. Promotion of self-management of long-term conditions is now a large feature of health care policy. Further insight into internet use of people with ME/CFS could provide online services for health professionals offering management plans to patients, helping and guiding available support in their homes.
Author contributions
Diane Shortland – responsible for all areas of the study from protocol design, screening, analysis, discussion, and writing up of study results.
Dr Qulsom Fazil, Dr Anna Lavis & Dr Nutmeg Hallett – contribution to the design of study, drafting and revising of work, final approval, and agreement.
Acknowledgement
Michelle Minns-Sykes has contributed to this paper by independently screening papers for the systematic review.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Open access. Study available by contacting lead author.
Additional information
Notes on contributors
Diane Shortland
Diane Shortland is a PhD student studying the social implications of long term illness, focusing on ME/CFS, at the Institute of Applied Health Research, University of Birmingham.
Qulsom Fazil
Qulsom Fazil is a lecturer in Disability Studies and Behavioural Science at the Institute of Applied Health Research, College of Medical and Dental Sciences, University of Birmingham.
Anna Lavis
Anna Lavis is an Associate Professor in Medical Anthropology across the Institute of Applied Health Research and Institute for Mental Health at the University of Birmingham, UK.
Nutmeg Hallett
Nutmeg Hallett is a registered Mental Health Nurse and Associate Professor in Nursing. Nutmeg teaches on a variety of undergraduate and post graduate mental health nursing and research modules at the Institute of Clinical Sciences, University of Birmingham.
References
- Action for ME. 2022. What is M.E.? See https://www.actionforme.org.uk/get-information/what-is-me/what-does-me-feel-like/.
- Grue J. A garden of forking paths: a discourse perspective on ‘Myalgic Encephalomyelitis’ and ‘Chronic Fatigue Syndrome’. Crit Discourse Stud. 2014;11:35–48. doi:10.1080/17405904.2013.829114
- Jason LA K, Sunnquist B, et al M. Chronic fatigue syndrome and myalgic encephalomyelitis: towards an empirical case definition. Health Psychol Behav Med. 2015;3(1):82–93. doi:10.1080/21642850.2015.1014489
- Kingod C, Bowman E, Curran H, et al. Functional status and well-being in people with myalgic encephalomyelitis/chronic fatigue syndrome compared with people with multiple sclerosis and healthy controls. PharmacoEconomics - Open. 2018;2:381–392. doi:10.1007/s41669-018-0071-6
- Hvidberg F, Brinth M, Schouborg L, et al. The health-related quality of life for patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). PLoS One. 2015;10(7):e0132421.
- Pendergrast T, Brown A, Sunnquist M, et al. Housebound versus nonhousebound patients with myalgic encephalomyelitis and chronic fatigue syndrome. Chronic Illn. 2016;12(4):292–307. doi:10.1177/1742395316644770
- Clarke J, James S. The radicalized self: the impact on the self of the contested nature of the diagnosis of chronic fatigue syndrome. Soc Sci Med. 2003;57:1387–1395. doi:10.1016/S0277-9536(02)00515-4
- McManimen S, McClellan D, Stoothoff J, et al. Effects of unsupportive social interactions, stigma, and symptoms on patients with myalgic encephalomyelitis and chronic fatigue syndrome. J Community Psychol. 2018;46(8):959–971. doi:10.1002/jcop.21984
- Harris K, Band R, Cooper H, et al. Distress in significant others of patients with chronic fatigue syndrome: a systematic review of the literature. Br J Health Psychol. 2016;21:881–893. doi:10.1111/bjhp.12202
- Bowling A. Measuring health: a review of quality of life measurement scales. Maidenhead: Open University Press; 2005.
- Action for ME.: Five year Big Survey. 2019. Available from: http://actionforme.org.uk/research-and-campaign/five-year-big-survey/ [Accessed 9th August 2022].
- Edwards CR, Thompson AR, Blair A. An ‘overwhelming illness: women’s experiences of learning to live with chronic fatigue syndrome/myalgic encephalomyelitis’. J Health Psychol. 2007;12(2):203–214. doi:10.1177/1359105307071747
- Ytre-Arne B. The social media experiences of long-term patients: illness, identity, and participation. Nordicom Review. 2016;37(1):57–70. doi:10.1515/nor-2016-0002
- Van der Eijk M, Faber M, Aarts J, et al. Using online health communities to deliver patient-centered care to people with chronic conditions. J Med Internet Res. 2013;15(6):e115. doi:10.2196/jmir.2476
- Lian O, Nettleton S. United we stand: framing myalgic encephalomyelitis in a virtual symbolic community. Qual Health Res. 2015;25(10):1383–1394. doi:10.1177/1049732314562893
- Lasker JN, Sogolow ED, Sharim RR. The role of an online community for people with a rare disease: content analysis of messages posted on a primary biliary cirrhosis mailing list. J Med Internet Res. 2005;7(1):e10. doi:10.2196/jmir.7.1.e10
- Eichhorn K. Soliciting and providing social support over the internet: an investigation of online eating disorder support groups. J Comput Mediat Commun. 2008;14(1):67–78. doi:10.1111/j.1083-6101.2008.01431.x
- Loane S, D’Alessandro S. Empowered and knowledgeable health consumers: the impact of online support groups on the doctor-patient relationship. Australas Mark J. 2014;22:238–245. doi:10.1016/j.ausmj.2014.08.007
- Perkins V, Coulson NS, Davies EB. Using online support communities for tourette syndrome and TIC disorders: online survey of user’s experiences. J Med Internet Res. 2020;22(11):e18099. doi:10.2196/18099
- Drentea P, Moren-Cross J. Social capital and social support on the web: the case of an internet mother site. Sociol Health Illn. 2005;27:920–943. doi:10.1111/j.1467-9566.2005.00464.x
- Conrad P, Stults C, et al. The internet and the experience of illness. In: Bird CE, Conrad P, Fremont AM, editors. Handbook of medical sociology. 6th ed. Nashville: Vanderbilt University Press; 2010. p. 179.
- Conrad P, Bandini J, Vasquez A. Illness and the internet: from private to public experience. Health. 2016;20(1):22–32. doi:10.1177/1363459315611941
- Lin TC, Hsu JSC, Cheng HL, et al. Exploring the relationship between receiving and offering online social support: a dual social support model. Inf Manag. 2015;52(3):371–383. doi:10.1016/j.im.2015.01.003
- Maier C, Laumer S, Eckhardt A, et al. Giving too much social support: social overload on social networking sites. Eur J Inf Syst. 2015;24(5):447–464. doi:10.1057/ejis.2014.3
- Beck LS, Gurion B, Sheva B. Internet ethnography: online and offline. Int J Qual Methods. 2004;3(2):45–51. doi:10.1177/160940690400300204
- Kingod N, Cleal B, Wahlberg A, et al. Online peer-to-peer communities in the daily lives of people with chronic illness: a qualitative systematic review. Qual Health Res. 2017;27(1):89–99. doi:10.1177/1049732316680203
- Allen C, Vassilev I, Kennedy A, et al. The work and relatedness of ties mediated online in supporting long-term condition self-management. Sociol Health Illn. 2020;42(3):579–595. doi:10.1111/1467-9566.13042
- Chung J. Social interaction in online support groups: preference for online social interaction over offline social interaction. Comput Human Behav. 2013;29:1408–1414. doi:10.1016/j.chb.2013.01.019
- Cummings J, Sproul L, Kiesler S. Beyond hearing: where the real-world and online support meet. Group Dyn. 2002;6(1):78–88. doi:10.1037/1089-2699.6.1.78
- Moorhea S, Hazlett D, Harrison L, et al. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):e85. doi:10.2196/jmir.1933
- Huan K, Chengalur-Smith I, Ran W. Not just for support: companionship activities in healthcare virtual support communities. Commun Assoc Inf Syst. 2014;34(1):561–594.
- Kummervold P, Gammon D, Bergvik S, et al. Social support in a wired world: use of online mental health forums in Norway. Nord J Psychiatry. 2002;56(1):59–65. doi:10.1080/08039480252803945
- Liemeister J, Schwiezer K, Leimester S, et al. Do virtual communities matter for the social support of patients? Antecedents and effects of virtual relationships in online communities. Inf Technol People. 2008;21(4):350–374. doi:10.1108/09593840810919671
- Caplan SE. Preference for online social interaction: a theory of problematic internet use and psychological well-being. Communic Res. 2003;30(6):625–648. doi:10.1177/0093650203257842
- Peters MDJ, Godfrey C, McInerney P, et al. Scoping reviews. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. 2020. Available from: https://synthesismanual.jbi.global.
- Munn Z, Peters M, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi:10.1186/s12874-018-0611-x
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi:10.1186/1748-5908-5-69
- Joanna Briggs Institute. Critical Appraisal Tools. Available from: https://jbi.global/critical-appraisal-tools. [Accessed 20th June 2023].
- Collins. 2022. Internet. Available from: www.collinsdictionary.com/dictionary/english/internet.
- Kaplan AM, Haenlein M. Users of the world, unite! The challenges and opportunities of social media. Bus Horiz. 2010;53:59–68. doi:10.1016/j.bushor.2009.09.003
- Tricco AC, Lillie E, Zarin E, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850
- Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2007;6(245).
- McColl MA, Shortt S, Godwin M, et al. Models for integrating rehabilitation and primary care: a scoping study. Arch Phys Med Rehabil. 2009;90(9):1523–1531. doi:10.1016/j.apmr.2009.03.017
- Brien SE, Lorenzetti DL, Lewis S, et al. Overview of a formal scoping review on health system report cards. Implement Sci. 2010;5(1):2. doi:10.1186/1748-5908-5-2
- Grant M, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(920):91–108. doi:10.1111/j.1471-1842.2009.00848.x
- Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48. doi:10.1186/1471-2288-13-48
- Critical Appraisal Skills Programme. CASP Qualitative Checklist. 2018. Available from: https://casp-uk.b-cdn.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf. [Accessed 9th August 2022].
- Mixed Methods Appraisal Tool. MMAT Mixed Methods Checklist. 2018. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/page/24607821/FrontPage. [Accessed 20th June 2023].
- Bates C. Performing the self in illness narratives. The role of evidentiality. In: Bates, Nebot, editors. Perspectives on evidentiality in Spanish: exploration across genres. John Benjamins; 2018. p. 73–106.
- Davison K, Pennebaker J, Dickerson S. Who talks? The ocial psychology of illness support groups. Am Psychol. 2000;55(2):205–217. doi:10.1037/0003-066X.55.2.205
- Lian O, Grue J. Generating a social movement online community through an online discourse: the case of myalgic encephalomyelitis. J Med Humanit. 2017;38:173–189. doi:10.1007/s10912-016-9390-8
- Murray R, Turner L. Living with chronic fatigue syndrome during lockdown and a global pandemic. Fatigue: Biomed Health Behav. 2021;8(3):144–155.
- Sanchez M. Sick and tired: narratives of contested illness in chronic fatigue syndrome blogs. In: Green S, Loseke D, editors. New narratives of disability: constructions, clashes, and controversies. Bingley: Emerald; 2019. p. 245–260.
- Best K, Butler S. The necessity of control for computer and internet users with myalgic encephalomyelitis/chronic fatigue syndrome. Inf Commun Soc. 2013;16(7):1042–1060.
- Brady B. 2015. Trust, empowerment, and identity online: a qualitative exploration of the use of Internet forums by individuals with long term conditions. The University of Manchester (UK).
- Brady E, Segar J, Sanders C. “I always vet things”: navigating privacy and the presentation of self on health discussion boards among individuals with long-term conditions. J Med Internet Res. 2016a;18(10):e274. doi:10.2196/jmir.6019
- Brady E, Segar J, Sanders C. “You get to know the people and whether they’re talking sense or not”: negotiating trust on health-related forums. Soc Sci Med. 2016b;162:151–157. doi:10.1016/j.socscimed.2016.06.029
- Kennedy A. 2014. Exploring the online social identities of people with chronic fatigue syndrome/myaligc encephalomyelitis (CFS/ME): a discourse analysis approach. University of Exeter (UK).
- Knudsen AK, Lervik LV, Harvey SB, et al. Comparison of chronic fatigue syndrome/myalgic encephalomyelitis with other disorders: an observational study. J R Soc Med Short Rep. 2012;3:32.
- Tian H, Brimmer D, Lin JM, et al. Web usage data as a means of evaluating public health messaging and outreach. J Med Internet Res. 2009;11(4):e52. doi:10.2196/jmir.1278
- Murray R, Day K, Tobbell J. Duvet woman versus action man: the gendered aetiology of chronic fatigue syndrome according to English newspapers. Fem Media Stud. 2019;19(2):890–905. doi:10.1080/14680777.2019.1595694
- Morehouse S, Schaible K, Williams O, et al. Impacts of online support groups on quality of life, and perceived anxiety and depression in those with ME/CFS: a survey. Fatigue: Biomed Health Behav. 2021;9(2):113–122.
- Murray R, Turner L. Using communities of practice theory to understand the crisis of identity in chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). Chronic Illn. 2021;19(1):1–9.
- Cromby J. The public meanings of CFS/ME: making up people. In: Ward C, editor. Meanings of ME: interpersonal and social dimensions of chronic fatigue. Basingstoke: Palgrave Macmillan; 2015. 129-151.
- Floyd J. Internet plugged in. Accent on Living. 2000;44(4):28–28.
- Brewer G, Stratton K. Living with chronic fatigue syndrome during lockdown and a global pandemic. Fatigue: Biomed Health Behav. 2020;8(3):144–155.
- International Alliance for ME. Recognition, research and respect: an agenda for change in ME. 2018. Available from: https://www.actionforme.org.uk/uploads/images/2019/01/IAFME-recognition-research-respect-041218.pdf [Accessed 29th August 2023].
- Capelli E, Lorusso L, Ghitti, M., Venturini, L , Cusa, C, Ricevuti, G. Chronic fatigue syndrome: features of a population of patients from Northern Italy. Int J Immunopathol Pharmacol. 2015;28(1):53–59. doi:10.1177/0394632015572074
- Faro M, Saez-Franca N, Castro-Marrero J, et al. Gender differences in chronic fatigue syndrome. Reumatología Clínica. 2016;12(2):72–77. doi:10.1016/j.reuma.2015.05.007
- Bowling A. Research methods in health: investigating health and health services. Fourth Edition Berkshire: Open University Press; 2014.
- Bamdad S, Finaughty D, Johns S. ‘Grey areas’: ethical challenges posed by social media-enabled recruitment and online data collection in cross-border, social science research. Res Ethics. 2022;18(1):24–38. doi:10.1177/17470161211045557
- Arigo D, Pagoto S, Carter-Harris L, et al. Using social media for health research: methodological and ethical considerations for recruitment and intervention delivery. Digital Health. 2018;4:205520761877175–15. doi:10.1177/2055207618771757
- Quinton S, Reynolds N. The changing roles of researchers and participants in digital social media research: ethics challenges and forward directions. In: Woodfield K, editor. The ethics of online research. Leeds: Emerald; 2017. p. 53–78.
- Chen Y, Chen C. Determining factors of participants’ attitudes toward the ethics of social media data research. Online Inf Rev. 2022;46(1):164–181. doi:10.1108/OIR-11-2020-0514
- Woodfield K, Iphofen R. Introduction to volume 2: the ethics of online research. In: Woodfield K, editor. The ethics of online research. Leeds: Emerald; 2017. p. 1–12.
- Colbert J, Yuan N, Agarwal P, et al. The promise of social media for health: a nationwide survey of primary care patients on usage patterns and attitudes. J Gen Intern Med. 2015;30:279–280.
- Davison K, Pennebaker J. Virtual narratives: illness representations in online support groups. In: Petrie K, Weinman J, editors. Perceptions of health & illness. London: Harwood Academic Publishers; 1997. p. 463–486.
- Anderson V, Jason L, Hlavaty L, et al. A review and meta-anaylsis of qualitative studies on myalgic encephalomylelitis/chronic fatigue. Patient Educ Couns; 2012;86:147–155.
- Baken D, Harvey S, Bimler D, et al. Stigma in myalgic encephalomyelitis and its association with functioning. Fatigue: Biomed Health Behav. 2018;6(1):30–40. doi:10.1080/21641846.2018.1419553
- Friedberg F, Leung D, Quick J. Do support groups help people with chronic fatigue syndrome and fibromyalgia? A comparison of active and inactive members. J Rheumatol. 2005;32:12.
- Hwang K, Ottenbacker A, Lucke J, et al. Measuring social support for weight loss in an internet weight loss community. J Health Commun. 2011;16(2):198–211. doi:10.1080/10810730.2010.535106
- Crabtree J, Haslam S, Postmes T, et al. Mental health support groups, stigma, and self-esteem: positive and negative implications of group identification. J Soc Sci. 2010;66(3):553–569.
- Reeves D, Blickem C, Vassilev I, et al. The contribution of social networks to the health and self-management of patients with long-term conditions: a longitudinal study. PLoS One. 2014;9(6). doi:10.1371/journal.pone.0098340
- Andreas A, Dhand A, Vassilev I, et al. Understanding online and offline social networks in illness management of older patients with asthma and chronic obstructive pulmonary disease: mixed methods study using quantitative social network assessment and qualitative analysis. JMIR Form Res. 2022;6(5):1.
- Barg J, McKenna K, Fitzsimons G. Can You See the Real Me? Activation and Expression of the ‘True Self’ on the internet. J Soc Issues. 2002;58(1):33–48. doi:10.1111/1540-4560.00247
- Ban R, Barrowclough C, Emsle R, et al. Significant other behavioural responses and patient chronic fatigue symptom fluctuations in the context of daily life: an experience sampling study. Br J Health Psychol. 2015;21:499–514.
- Brooks B, Kanuika A, Kelliher Rabon J, et al. Social support and subjective health in fibromyalgia: self-compassion as a mediator. J Clin Psychol Med Settings. 2022;29:375–383. doi:10.1007/s10880-021-09832-x
- Versaandonk J, Cenders M, Bleijenberg G, et al. The role of the partner and relationship satisfaction on treatment outcome in patients with chronic fatigue syndrome. Psychol Med. 2015;45:2345–2352. doi:10.1017/S0033291715000288
- Brooks J, Daglish J, Wearden A. Attributions, distress and behavioural responses in the significant others of people with chronic fatigue syndrome. J Health Psychol. 2013;18(10):1288–1295. doi:10.1177/1359105312464670
- Crump L, LaChapelle D. “My Fibro Family!” A qualitative analysis of Facebook Fibromyalgia support groups’ discussion content’. Canad J Pain. 2022;6(1):95–111. doi:10.1080/24740527.2022.2078183
- Kingod N. The tinkering m-patient: co-constructing knowledge on how to live with type 1 diabetes through Facebook searching and sharing and offline tinkering with self-care. Health. 2020;24(2):152–168. doi:10.1177/1363459318800140
- Lian O, Robson C. “It’s incredible how much I’ve had to fight”: negotiating medical uncertainty in clinical encounters. Int J Qual Stud Health Well-Being. 2017;12(1):1392219. doi:10.1080/17482631.2017.1392219
- Jason L. Small wins matter in advocacy movements: giving voice to patients. Leonard Am J Community Psychol. 2011;49(3):307–316.
- Conrad B, Barker K. The social construction of illness: key insights and policy implications. J Health Soc Behav. 2010;51(1):S67–S79. doi:10.1177/0022146510383495
- Bury M. The sociology of chronic illness: a review of research and prospects. Sociol Health Illn. 1991;13(4):451–468. doi:10.1111/j.1467-9566.1991.tb00522.x
- Gilberg C. A troubling truth: chronic illness, participation and learning for change. The Centre for Welfare Reform. 2016. Available from: http://www.cenrteforwelfarereform.org/uplaods/attachment/509/a-troubling-truth.pdf [Accessed 19/9/23].
- Frank A. The wounded storyteller: body, illness and ethics. Chicago (IL): The University of Chicago Press; 1995.
- Whitehead L. Toward a trajectory of identity reconstruction in chronic fatigue syndrome/myalgic encephalomyelitis: a longitudinal qualitative study. Int J Nurs Stud. 2006;43:1023–1031. doi:10.1016/j.ijnurstu.2006.01.003
- Groevelt I. “It’s not all nice and fun”: narrating contested illness on YouTube and Instagram. Health. 2022;26(5):589–604. doi:10.1177/13634593211017187
- Stein J. From activist to ‘passivist’: where is the mass movement? In: Munson P, editor. Stricken voices from the hidden epidemic. Oxfordshire: Routledge; 2000. p. 163–172.
- Khalafbeigi M, Yazdani F, Genis F, et al. Invisibility and diagnosis stigma: disabling factors for female adults with mylagic encephalomyelitis (ME/chronic fatigue syndrome (CFS) in a small-scale qualitative study in England. Ir J Occup Ther. 2023;51(2):52–59.
- Vya J, Muirhead N, Sing R, et al. Impacts of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) on the quality of life of people with ME/CFS and their partners and family members: an online cross-sectional survey. BMJ Open. 2022;12:e058128.
- Brittain E, Muirhead N, Finlay A, et al. Myalgic encephaloymyelitis/chronic fatigue syndrome (ME/CFS): major impact on lives of both patients and family members. 2021;57:43.
- Yao T, Zheng Q, Fan X. The impact of online social support on patients’ quality of life and the moderating role of social exclusion. J Serv Res. 2015;18(3):369–383. doi:10.1177/1094670515583271
- Brooks J, King N, Wearden A. Couple’s experiences of interacting with outside others in chronic fatigue syndrome: a qualitative study. Chronic Illn. 2014;10(1):5–17. doi:10.1177/1742395312474478