ABSTRACT
Introduction: Parental support behaviors are established predictors of children's physical activity and healthy eating. However, little is known about predictors of these parental support behaviors. Identity (i.e. a component of the self-concept) has been hypothesized to be an influential construct that may be associated with a variety of behavioral antecedents and behavior itself. Specifically, research suggests healthy eating or physical activity parental support affective attitude may predict parental identity, and that identity may predict support behavior directly and indirectly through support self-regulation (e.g. planning). Thus, this study expands on past literature by exploring these antecedents and outcomes of parental identity in the context of parental support for physical activity and healthy eating among overweight and obese children.
Methods: Using a cross-sectional survey design, 83 parents (61.4% female) with at least one overweight or obese child completed measures assessing parental support affective attitude, parental identity, support self-regulation, and actual support behaviors. Path analysis was conducted to examine model fit and hypothesized relationships between variables for eating and physical activity separately.
Results: For both behavioral domains, the model fit was good. Parental support affective attitude predicted parental identity, parental identity predicted support self-regulation, and support self-regulation predicted support behavior. Further, for both behaviors, support self-regulation mediated the relationship between parental identity and support behavior. Finally, parental identity also directly predicted support behavior for physical activity but not eating.
Conclusions: The results demonstrate the importance of identity in parental support behaviors. These results also show that fostering enjoyable experiences for parents while supporting their children may strengthen their supportive identities.
Childhood obesity is one of the most common pediatric health problems and has been linked to multiple physiological and psychosocial problems such as high blood pressure and lower quality of life (Canning, Courage, & Frizzell, Citation2004; Maximova, Kuhle, Davidson, Fung, & Veugelers, Citation2013; Schwimmer, Burwinkle, & Varni, Citation2003). Without intervention, overweight children will likely continue to be overweight during adolescence and adulthood (Canning et al., Citation2004; Twig et al., Citation2016). If current trends continue, by 2040, up to 70% of adults aged 40 years will be either overweight or obese (Twig et al., Citation2016). Lifestyle behavioral interventions are the principal intervention approach for helping children maintain a healthy weight (Flynn et al., Citation2006; Kohl et al., Citation2012; Sacher et al., Citation2010; Tyson & Frank, Citation2018; Wang et al., Citation2013). Consistent moderate to vigorous physical activity (i.e. activity causing harder breathing and sweating; Godin & Shephard, Citation1985) and a diet composed of sufficient amounts of fruits and vegetables are important behaviors for preventing and managing childhood obesity and ensuring optimal health and development (Poitras et al., Citation2016; Morenga, & Montez, & M, Citation2017; Wang et al., Citation2014). Therefore, there is a need to study the determinants of these two health behaviors to provide some guidance regarding future intervention targets (Rothman, Citation2004).
Family-based lifestyle behavioral interventions may be more effective at helping children maintain a healthy weight if consistent parental support behaviors are present. Parental support behaviors for a healthy lifestyle are established key predictors of child physical activity and healthy eating (Scaglioni et al., Citation2018; Yao & Rhodes, Citation2015). Support has been conceptualized as responsiveness (i.e. giving encouragement) and providing structure (i.e. provide an optimal physical environment) and those parents that provide both to their children may be most likely to succeed at supporting healthy lifestyle behaviors (Davison, Li, Baskin, Cox, & Affuso, Citation2011). Thus, interventions increasing the regularity of these forms of parental support should in turn promote child health.
Knowledge regarding predictors of parental support behaviors in the physical activity and healthy eating domains (especially for overweight and obese children) is limited. However, in terms of physical activity, Rhodes et al. (Citation2019a) recently demonstrated that parental identity toward supporting one's child to do regular moderate to vigorous physical activity better predicted parental support than all of the other psychological variables tested (support affective attitude, instrumental attitude, perceived capability, perceived opportunity, planning, habit). Identity can be defined as a component of a hierarchically organized self-concept made up of various roles (Markus, Citation1977; Stryker & Burke, Citation2000). According to identity theory, identities act as personal standards that are compared to current behavior. Any discrepancies between the two should create negative affect which would then motivate action to close the gap between identity and the present situation (Burke, Citation2006). Thus, parents who hold a parental physical activity identity (i.e. ‘It is my duty to be physically active and to ensure my child is consistently active’) and a parental healthy eating identity (i.e. ‘It is my job to ensure our family is consistently eating fruits and vegetables’) should be more likely to provide support (e.g. take child to a place where they can be physically active, buy fruits and vegetables) when they recognize a discrepancy between current behavior (e.g. being sedentary together, eating unhealthy together) and the identities. In terms of healthy eating, Strachan and Brawley (Citation2009) demonstrated that strength of a healthy eater identity (i.e. ‘I am someone who eats healthy’) does predict healthy eating. Therefore, based on past literature, it is our belief that parental healthy eating or physical activity identity may be a potential target for interventions to increase parental support.
It is important to understand the antecedents of parental healthy eating or physical activity identity to know how to modify it. A review of identity in the physical activity domain found that commitment, self-efficacy, affective judgements, identified/integrated regulation (i.e. valuing the behavior and believing it is congruent with the self), and social activation (e.g. experiencing feelings of belonging) all reliably predicted identity (Rhodes, Kaushal, & Quinlan, Citation2016a). Affective judgements or attitude, which are emotional feelings about the behavior based on prior experiences and expectations (e.g. ‘The behaviour is pleasant’; Fishbein & Ajzen, Citation2010), may be particularly important. Affective attitude generally has a large-sized correlation with behavioral intentions, a medium-sized correlation with behavior (McEachan et al., Citation2016), and experimental studies in the physical activity domain show it is modifiable through intervention (Rhodes, Gray, & Husband, Citation2019b). The physical activity self-definition model (Kendzierski & Morganstein, Citation2009) also suggests that enjoyment predicts identity because enjoyment increases commitment to maintain the identity, and self-determination theory (Ryan & Deci, Citation2000) predicts that people will continue to do a behavior if they believe the behavior is enjoyable and congruent with the self. It therefore seems probable that affective attitude about parental support would predict parental identity for healthy eating or physical activity.
Identity may exert its effects on behavior both directly and indirectly (Caldwell et al., Citation2018; Kahneman, Citation2011; Rhodes, Citation2017). Direct effects may occur when the process is relatively automatic, reflexive, and beyond conscious awareness. There is empirical support for the idea that identity directly effects behavior for both healthy eating and physical activity (Carfora, Caso, & Conner, Citation2016; Rhodes et al., Citation2016a). A direct effect may occur when parental support behaviors occur immediately after the activation of the parental identity for healthy eating or physical activity. Regarding healthy eating, for example, a parent may be prompted to prepare a vegetable snack for one's child. Indirect effects may occur when the process is relatively slow, reflective, and within conscious awareness. Mediators of the relationship between parental identity and parental support behavior for healthy eating or physical activity are therefore important to identify because they explain how parental identity leads to parental support when we are consciously aware of what we are doing. Rhodes et al. (Citation2016a) found that identity has reliably predicted self-regulatory behaviors such as goal setting, planning, and self-monitoring regarding the progress one is making on the behavior. These parental support self-regulation processes may then be mediators and there is some evidence supporting this idea. For example, Strachan, Brawley, Spink, Sweet, and Perras (Citation2015) showed that self-regulation self-efficacy (i.e. confidence to self-regulate) was a mediator in the relationship between physical activity identity and exercise behavior, and Carraro and Gaudreau (Citation2010) found planning to be a mediator. Rhodes et al. (Citation2019a) and Rhodes et al. (Citation2016b) also both showed parental physical activity support self-regulation was correlated with support behavior. These empirical findings are also consistent with identity theory. That is, the discrepancies between current behavior and the identity should motivate self-regulatory action to close the gap between identity and behavior (Stryker & Burke, Citation2000). Parental identity (e.g. for physical activity) may then cause parents to employ self-regulation strategies (e.g. plan to drive one's child to a place to play a sport) to ensure they provide support (e.g. actually drive one's child to a place to play a sport) to their children.
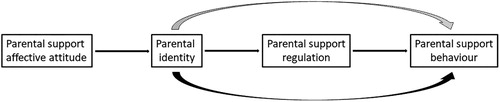
The purpose of this study was to examine the purported antecedents and outcomes of parental identity noted above in the context of parental support for physical activity and healthy eating among overweight and obese children. No research has yet examined these particular theoretical paths in one model for either behavior. It was hypothesized that affective attitude regarding parental support would predict parental identity, identity would predict parental self-regulation to support one's child, and self-regulation would then predict parental support for both child physical activity and healthy eating. Further, it was hypothesized that parental identity would also directly predict parental support, and support self-regulation would mediate the relationship between parental identity and parental support (see ).
Method
Design
This is a sub-study of a randomized waitlist-controlled trial (registered trial number: NCT03643341) that assessed the effectiveness of a 10-week interactive family-based lifestyle intervention for children 8–12 years of age (BMI ≥ 85th percentile of age and sex). Baseline data were analyzed in this study. Study participants were recruited from British Columbia, Canada. Participants completed the baseline survey from October 2018 to March 2019. Ethical clearance was formally provided by a university's human subject research ethics board for the trial and participants provided informed consent.
Participants
Eighty-three parents (61.4% female), representing 89 overweight or obese children (M age = 10.58, SD = 1.55), completed the measures using an online survey at the baseline phase of a family-oriented intervention to manage childhood obesity. All children recruited were 8–12 years of age with a BMI ≥ 85th percentile of age and sex. Please see for available demographic information.
Table 1. Available demographic information.
Measures
Affective attitude for healthy eating and physical activity support. Two items, adapted from Rhodes, Blanchard, and Matheson (Citation2006), measured parental support affective attitude for eating (α = .50) and physical activity (α = .80). This scale has shown adequate reliability and discriminant, construct, and predictive validity (Rhodes et al., Citation2006). The first item for each behavior was scored on a scale that ranged from 1 (extremely unenjoyable) to 7 (extremely enjoyable). The items were ‘For me, regularly supporting my child's (healthy eating [e.g. increasing fruit and vegetable consumption and decreasing intake of sugary beverages]/moderate-to-vigorous physical activity [e.g. driving to practice, scheduling activities]) over the next two weeks would be:’ The second item for each behavior was scored on a scale that ranged from 1 (extremely unpleasant) to 7 (extremely pleasant). The items were ‘For me, regularly supporting my child's (healthy eating/moderate-to-vigorous physical activity [e.g. driving to practice, scheduling activities]) over the next two weeks would be:’ Because reliability for eating affective attitude was poor, we included only the first item in subsequent eating analyses (see Appendix).
Self-regulation for healthy eating and physical activity support. Four items, adapted from previous research (Rhodes et al., Citation2016b; Rhodes et al., Citation2016b; Sniehotta, Schwarzer, Scholz, & Schüz, Citation2005), measured parental support self-regulation for eating (α = .86) and physical activity (α = .89). Areas of self-regulation targeted were based on evidence indicating which self-regulation behavior change techniques are most effective at influencing healthy eating and physical activity (Golley, Hendrie, Slater, & Corsini, Citation2011; Michie, Abraham, Whittington, McAteer, & Gupta, Citation2009). The items assessed goal setting (for the behavior; item 1), review of behavioral goals (item 2), problem solving/coping planning (item 3), and action planning (item 4). The items, scored on a scale that ranged from 1 (strongly disagree) to 5 (strongly agree), were ‘I set short-term (daily or weekly) goals for how I could support my child's (healthy eating/leisure-time physical activity) behaviors last month,’ ‘If I did not reach (my goal/one of my goals) for supporting my child's (healthy eating/physical activity) last month, I analyzed what went wrong,’ ‘I made plans regarding what to do if something made it difficult to support my child's (healthy eating/physical activity) last month,’ and ‘I made regular plans concerning “when”, “where”, “how”, and “what” kind of support I could provide for my child's (eating behaviors and food choices/physical activity) last month.’
Parental identity for healthy eating and physical activity. Three items, adapted from the role identity subscale of the Exercise Identity Scale (Anderson & Cychosz, Citation1994; Wilson & Muon, Citation2008), measured parental identity for eating (current study α = .82) and physical activity (current study α = .88). Wilson and Muon (Citation2008) found the scale had adequate reliability (α = .84) and construct, convergent, and predictive validity. The eating items were ‘I consider myself an individual who prepares healthy food and beverage choices,’ ‘When I describe myself to others, I usually include my commitment to eating healthy,’ and ‘Others see me as someone who regularly eats healthy.’ The physical activity items were ‘I consider myself an exerciser,’ ‘When I describe our family to others, I usually include something about our physical activities,’ and ‘Others see us as a family that is regularly active.’ Each item was scored on a scale that ranged from 1 (strongly disagree) to 5 (strongly agree).
Parental support for healthy eating and physical activity. Commensurate with the responsiveness and structure dimensions of parental support, participants were asked questions about encouragement and logistics support. Three items, adapted from previous research (Davison et al., Citation2011; Rhodes et al., Citation2016b), measured parental support for eating (α = .82) and physical activity (α = .80). Davison et al. (Citation2011) found the physical activity scale to be reliable (α = .72) and valid (construct and convergent validity tested). The healthy eating items were study created. The eating items began with the stem ‘During a typical week how often have you or another family member of your household:’ The items, scored on a scale that ranged from 1 (not at all) to 4 (every day), were ‘Encouraged your child to eat more fruit,’ ‘Encouraged your child to eat more vegetables,’ and ‘Bought fruit or vegetables you know your child likes.’ The physical activity items, scored on a scale that ranged from 1 (strongly disagree) to 5 (strongly agree), were ‘I watch my child play sports or participate in other activities such as martial arts or dance,’ ‘I enroll my child in sports teams and clubs such as soccer, basketball, and dance,’ and ‘I take my child to places where he/she can be active.’
Data analysis
Path analysis with a covariance matrix using robust maximum likelihood estimation was conducted to examine model fit and the relationships between variables for eating and physical activity separately (Schumacker & Lomax, Citation2010). Total (i.e. the independent variable predicting the dependent variable), direct (i.e. the independent variable predicting the dependent variable controlling for the intervening variable), and indirect (i.e. the total effect minus the direct effect) relationship effects were examined to test the study's hypotheses (Preacher & Hayes, Citation2004). For indirect effect tests for both healthy eating and physical activity, the independent variable is parental identity, the mediator is support self-regulation, and the dependent variable is parental support behavior. Analyses were conducted using LISREL version 10.10. Several criteria were used to judge model fit: (a) significance and direction of relationships between variables, (b) size of standardized residuals between variables (greater than 3.29 was considered unacceptable), and model fit indices. The following indices (accompanied with acceptable fit guidelines) were used to assess how well the model fit the data: χ2 (non-significant value), GFI (.90 or higher), SRMR (less than .05), RMSEA (.08 or lower), and NFI (.90 or higher; Schumacker & Lomax, Citation2010). Also, as per guidelines provided by Cohen (Citation1988), small, medium, and large effect sizes were interpreted when R2 was greater than or equal to .02, .13, and .26, respectively. Based on the planned analyses, using G*Power, we calculated needing a sample size of 77 participants to detect a medium effect size (ƒ2 = .15; Cohen, Citation1988) at 80% power with α = .05 (Faul, Erdfelder, Lang, & Buchner, Citation2007). Thus, the final sample size was slightly larger than this estimate.
Results
Data screening and preparation
Using SPSS version 24, the data were first examined for outliers at the univariate level (Tabachnick & Fidell, Citation2012). Univariate outliers were values more than three times greater or less than the middle 50% (25th to 75th percentiles) of the distribution (Pallant, Citation2011). No outliers were discovered. Next, patterns in missing data were examined for each behavior separately. The data were missing completely at random for eating (Little's MCAR test: chi-square = 18.68, DF = 29, p = .93) and physical activity variables (Little's MCAR test: chi-square = 32.04, DF = 24, p = .13). Imputation was then conducted through the expectation maximization procedure using LISREL version 10.10 for each behavior separately. Finally, multivariate outliers, participants with a Cook's distance greater than 1 (Tabachnick & Fidell, Citation2012), were investigated for each behavior separately; however, none were discovered.
Parental support for healthy eating
The fit indices for this model are as follows: χ2 = 1.07 (df = 2), p = .59, GFI = .99, SRMR = .04, RMSEA = .00, and NFI = .97. There were no large standardized residuals and nearly all of the relationships between variables were also significant and in the positive direction (see for the correlation matrix). Therefore, the available information suggest that this model fits the data well (see ). Parent support affective attitude had a small-sized association with parental identity (β = .30, p < .01, R2 = .09), parental identity had a small-sized association with support self-regulation (β = .31, p < .01, R2 = .09), and support self-regulation significantly predicted parental support (β = .40, p < .01). The direct effect between parental identity and parental support (i.e. controlling for support self-regulation) was not significant (β = .10, p = .38), and the variance explained in parental support from parental identity and support self-regulation was in the medium-sized range (R2 = .19). There was also a positive indirect effect between parental identity and parental support through support self-regulation (β = .12, p < .05; see for means and standard deviations).
Figure 2. Standardized regression coefficients (and measurement errors in ellipses) for the healthy eating model. The dotted curved arrow represents an indirect effect and the solid curved arrow represents a direct effect controlling for the mediator. Statistically significant effects have an asterisk. Unstandardized indirect effect = .096, CIs = .012, .180.
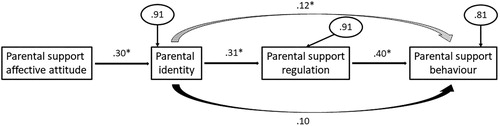
Table 2. Correlation matrices.
Table 3. Means and standard deviations.
Parental support for physical activity
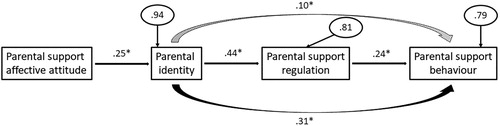
The fit indices for this model are as follows: χ2 = 2.12 (df = 2), p = .35, GFI = .99, SRMR = .04, RMSEA = .06, and NFI = .95. There were no large standardized residuals and all of the relationships between variables were also significant and in the positive direction (see for the correlation matrix). Therefore, the available information suggest that this model fits the data well (see ). Parental support affective attitude had a small-sized association with parental identity (β = .25, p = .02, R2 = .06), parental identity had a medium-sized association with support self-regulation (β = .44, p < .001, R2 = .19), and support self-regulation significantly predicted parental support (β = .24, p = .03). The direct effect between parental identity and parental support (i.e. controlling for support self-regulation) was significant (β = .31, p < .01), and the variance explained in parental support from parental identity and support self-regulation was in the medium-sized range (R2 = .21). There was also a positive indirect effect between parental identity and parental support through support self-regulation (β = .10, p < .05; see for means and standard deviations).
Figure 3. Standardized regression coefficients (and measurement errors in ellipses) for the physical activity model. The dotted curved arrow represents an indirect effect and the solid curved arrow represents a direct effect controlling for the mediator. Statistically significant effects have an asterisk. Unstandardized indirect effect = .124, CIs = .001, .247.
Discussion
The purpose of this study was to examine antecedents and outcomes of parental identity in terms of physical activity and healthy eating among overweight and obese children. We postulated that affective attitude regarding parental support would predict parental identity, identity would predict parental self-regulation to support one's child, and self-regulation would then predict parental support for both child physical activity and healthy eating. Further, we hypothesized that parental identity would also directly predict parental support, and support self-regulation would mediate the relationship between parental identity and parental support. To our knowledge, this is the first study to examine the relationships between these variables in a single model among parents of children who are overweight or obese. Nearly all of the hypotheses were supported for both behaviors. Our results have important research and clinical implications as they highlight key factors that may lead to improvements in parental support behavior for their child to engage in regular physical activity and eat a healthy diet.
First, from a theoretical perspective, this study advances knowledge of the identity construct regarding parental support in the physical activity and healthy eating domains. According to identity theory (Burke, Citation2006; Stryker & Burke, Citation2000), discrepancies between a current self and one's identity should produce distress and motivate self-regulation and subsequent behavior change to reduce any discrepancies. In the current study, for both behavioral domains, support self-regulation mediated the relationship between parental identity and parental support. Stated another way, viewing oneself as a healthy eater or physically active parent motivated support self-regulatory behaviors (i.e. goal setting, self-reflection, planning) which then, in turn, motivated parental support behaviors (i.e. encouragement and logistical support). Thus, these findings are consistent with identity theory. Also, the pattern of findings are consistent with behavioral theories that propose reflective (indirect, mediated) and reflexive (direct) paths to behavior stemming from identity (Caldwell et al., Citation2018; Kahneman, Citation2011; Rhodes, Citation2017). Evidence of the latter was also observed because there was indeed a direct effect from parental identity to parental support for physical activity. The direct effect suggests that identity can also affect behavior in a manner not associated with self-regulation in certain situations. The lack of a direct effect for healthy eating may indicate that eating parental support requires self-regulation such as planning meals for one's family.
The results also indicated that support affective attitude predicted parental identity for health eating and physical activity. This effect has been consistently demonstrated in the physical activity domain (Rhodes et al., Citation2016a). Also, the physical activity self-definition model (Kendzierski & Morganstein, Citation2009) would predict the same effect, and self-determination theory (Ryan & Deci, Citation2000) suggests that individuals need to enjoy the behavior and believe the behavior is congruent with the self in order for behavioral maintenance to occur. Therefore, support affective attitude predicting parental identity is consistent with related theories. However, this effect had not yet been demonstrated in the parental support literature. This finding suggests that parents may require some sort of enjoyment during parental support activities for healthy eating or physical activity in order for the identity to develop and strengthen over time. Practically, or from a clinical perspective, this knowledge also provides guidance for intervention. It suggests that parental support affective attitude be targeted in interventions.
Affective attitude is modifiable (Rhodes et al., Citation2019b), so future research should investigate whether an experiment can influence parental identity through support affective attitude change. There are no published identity interventions in the physical activity domain beyond one feasibility trial (i.e. Husband, Wharf Higgins, & Rhodes, Citation2018) and only a handful exist in the healthy eating domain (e.g. Brouwer & Mosack, Citation2015; Carfora, Caso, & Conner, Citation2017). Regarding potential intervention targets, self-determination theory (Ryan & Deci, Citation2000) would suggest enhancing parent autonomy, relatedness, and competence in terms of support, and hedonic theory (e.g. Zajonc, Citation1980) would suggest making support behaviors more pleasurable. In terms of enhancing the pleasure of the experience during the provision of support, we know that people tend to prefer immediate rewards compared to delayed ones (Metcalfe & Mischel, Citation1999). Thus, interventions would need parents to think that providing support is worth it in the short-term. Perhaps the implementation of a reward system or conditioning parents to think of support as being enjoyable (e.g. through Pavlovian or evaluative conditioning) would positively influence parental support affective attitude for healthy eating or physical activity (de Ridder, Kroese, Evers, Adriaanse, & Gillebaart, Citation2017; Mantzari et al., Citation2015; Rhodes & Kates, Citation2015). Certainly, more research is needed to learn how support affective attitude can be manipulated to encourage the development of strong parental identities for healthy eating and physical activity.
A strength of this study is the use of previously validated questionnaires to measure support affective attitude, identity, self-regulation, and parental support behaviors for physical activity and diet. Additionally, this study focused on examining the support behaviors for a healthy lifestyle in a critical population group, parents of children who are overweight or obese. Family-focused behavioral weight management interventions are the principal intervention approach for achieving long-term weight control in children (Flynn et al., Citation2006; Kohl et al., Citation2012; Sacher et al., Citation2010; Tyson & Frank, Citation2018; Wang et al., Citation2013). Thus, understanding the factors contributing to health eating and physical activity parental support behavior is important. A limitation of the present study was the small sample size. Also, our sample did not have a diverse ethnicity and social-economic status background. Furthermore, our healthy eating measures focused on evaluating fruit and vegetable intake. Other components such as dietary fat intake were not measured. These factors limit the generalizability of our findings. Another limitation was the lack of longitudinal data over a lengthy period. Longitudinal data can be used to build more complex multivariate models with the ability to better examine both mediation and moderation effects to help inform mechanisms of change. Future study in this area is warranted. Finally, our healthy eating support affective attitude measure contained only one item which limited our understanding of its reliability.
Conclusion
This study examined the predictors of parental support for physical activity and healthy eating among parents who have children who are overweight and obese. We found that that affective attitude about parental support predicts parental identity, identity predicts parental self-regulation to support their child, and self-regulation predicts parental support for both child eating and physical activity. Also, there were indirect and direct effects of parental identity to parental support. These results reinforce the importance of fostering enjoyable experiences for parents while supporting their children in order to strengthen their healthy eating and physical activity parental identities.
Supplemental Material
Download MS Word (17.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anderson, D. F., & Cychosz, C. M. (1994). Development of an exercise identity scale. Perceptual and Motor Skills, 78(3), 747–751. doi:10.2466/pms.1994.78.3.747 doi: 10.1177/003151259407800313
- Brouwer, A. M., & Mosack, K. E. (2015). Motivating healthy diet behaviors: The self-as-doer identity. Self and Identity, 14(6), 638–653. doi: 10.1080/15298868.2015.1043335
- Burke, P. J. (2006). Identity change. Social Psychology Quarterly, 69(1), 81–96. doi:10.1177/019027250606900106
- Caldwell, A. E., Masters, K. S., Peters, J. C., Bryan, A. D., Grigsby, J., Hooker, S. A., … Hill, J. O. (2018). Harnessing centred identity transformation to reduce executive function burden for maintenance of health behaviour change: The maintain IT model. Health Psychology Review, 12(3), 231–253. doi: 10.1080/17437199.2018.1437551
- Canning, P. M., Courage, M. L., & Frizzell, L. M. (2004). Prevalence of overweight and obesity in a provincial population of Canadian preschool children. Canadian Medical Association Journal, 171(3), 240–242. doi: 10.1503/cmaj.1040075
- Carfora, V., Caso, D., & Conner, M. (2016). The role of self-identity in predicting fruit and vegetable intake. Appetite, 106, 23–29. doi: 10.1016/j.appet.2015.12.020
- Carfora, V., Caso, D., & Conner, M. (2017). Correlational study and randomised controlled trial for understanding and changing red meat consumption: The role of eating identities. Social Science & Medicine, 175, 244–252. doi: 10.1016/j.socscimed.2017.01.005
- Carraro, N., & Gaudreau, P. (2010). The role of implementation planning in increasing physical activity identification. American Journal of Health Behavior, 34(3), 298–308. doi: 10.5993/AJHB.34.3.5
- Cohen, J. W. (1988). Statistical power analysis for the behavioral sciences (2nd ed). Hillsdale, NJ: Lawrence Erlbaum Associates.
- Davison, K. K., Li, K., Baskin, M. L., Cox, T., & Affuso, O. (2011). Measuring parental support for children’s physical activity in White and African American parents: The activity support scale for multiple Groups (ACTS-MG). Preventive Medicine, 52(1), 39–43. doi: 10.1016/j.ypmed.2010.11.008
- de Ridder, D., Kroese, F., Evers, C., Adriaanse, M., & Gillebaart, M. (2017). Healthy diet: Health impact, prevalence, correlates, and interventions. Psychology & Health, 32(8), 907–941. doi: 10.1080/08870446.2017.1316849
- Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. doi: 10.3758/BF03193146
- Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach. New York, NY: Psychology Press.
- Flynn, M. A. T., McNeil, D. A., Maloff, B., Mutasingwa, D., Wu, M., Ford, C., … Tough, S. C. (2006). Reducing obesity and related chronic disease risk in children and youth: A synthesis of evidence with ‘best practice’ recommendations. Obesity Reviews, 7(S1), 7–66. doi: 10.1111/j.1467-789X.2006.00242.x
- Godin, G., & Shephard, R. J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Science, 10(3), 141–146.
- Golley, R. K., Hendrie, G. A., Slater, A., & Corsini, N. (2011). Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns – what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obesity Reviews, 12(2), 114–130. doi: 10.1111/j.1467-789X.2010.00745.x
- Husband, C. J., Wharf Higgins, J., & Rhodes, R. E. (2018). A feasibility randomized trial of an identity-based physical activity intervention among university students. Health Psychology and Behavioral Medicine, 7(1), 128–146. doi: 10.1080/21642850.2019.1600407
- Kahneman, D. (2011). Thinking, fast and slow. New York, NY: Farrar, Straus and Giroux.
- Kendzierski, D., & Morganstein, M. S. (2009). Test, revision, and cross-validation of the physical activity self-definition model. Journal of Sport and Exercise Psychology, 31(4), 484–504. doi: 10.1123/jsep.31.4.484
- Kohl, H. W. 3rd, Craig, C. L., Lambert, E. V., Inoue, S., Alkandari, J. R., Leetongin, G., … Lancet Physical Activity Series Working Group (2012). The pandemic of physical inactivity: Global action for public health. The Lancet, 380(9838), 294–305. doi: 10.1016/S0140-6736(12)60898-8
- Mantzari, E., Vogt, F., Shemilt, I., Wei, Y., Higgins, J. P. T., & Marteau, T. M. (2015). Personal financial incentives for changing habitual health-related behaviors: A systematic review and meta-analysis. Preventive Medicine, 75, 75–85. doi: 10.1016/j.ypmed.2015.03.001
- Markus, H. (1977). Self-schemata and processing information about the self. Journal of Personality and Social Psychology, 35(2), 63–78. doi: 10.1037/0022-3514.35.2.63
- Maximova, K., Kuhle, S., Davidson, Z., Fung, C., & Veugelers, P. J. (2013). Cardiovascular risk-factor profiles of normal and overweight children and adolescents: Insights from the Canadian health measures survey. Canadian Journal of Cardiology, 29(8), 976–982. doi: 10.1016/j.cjca.2012.08.013
- McEachan, R., Taylor, N., Harrison, R., Lawton, R., Gardner, P., & Conner, M. (2016). Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine, 50(4), 592–612. doi: 10.1007/s12160-016-9798-4
- Metcalfe, J., & Mischel, W. (1999). A hot/cool-system analysis of delay of gratification: Dynamics of willpower. Psychological Review, 106(1), 3–19. doi: 10.1037/0033-295X.106.1.3
- Michie, S., Abraham, C., Whittington, C., McAteer, J., & Gupta, S. (2009). Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychology, 28(6), 690–701. doi: 10.1037/a0016136
- Morenga, T., & Montez, L., & M, J. (2017). Health effects of saturated and trans-fatty acid intake in children and adolescents: Systematic review and meta-analysis. PLoS One, 12(11), e0186672. doi: 10.1371/journal.pone.0186672
- Pallant, J. (2011). SPSS survival manual: A step by step guide to data analysis using SPSS (4th ed). Australia: Allen & Unwin.
- Poitras, V. J., Gray, C. E., Borghese, M. M., Carson, V., Chaput, J.-P., Janssen, I., … Tremblay, M. S. (2016). Systematic review of the relationship between objectively measured physical activity and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41, S197–S239. doi: 10.1139/apnm-2015-0663
- Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. doi: 10.3758/BF03206553
- Rhodes, R. E. (2017). The evolving understanding of physical activity behavior: A multi-process action control approach. In A. J. Elliot (Ed.), Advances in motivation science, Vol. 4 (pp. 171–205). Cambridge, MA: Elsevier Academic Press.
- Rhodes, R. E., Berry, T., Faulkner, G., Latimer-Cheung, A. E., O’Reilly, N., Tremblay, M. S., … Spence, J. C. (2019a). Application of the multi-process action control framework to understand parental support of child and youth physical activity, sleep, and screen time behaviours. Applied Psychology: Health and Well-Being, 11(2), 223–239. doi: 10.1111/aphw.12150
- Rhodes, R. E., Blanchard, C. M., & Matheson, D. H. (2006). A multicomponent model of the theory of planned behaviour. British Journal of Health Psychology, 11(1), 119–137. doi: 10.1348/135910705X52633
- Rhodes, R. E., Gray, S. M., & Husband, C. (2019b). Experimental manipulation of affective judgments about physical activity: A systematic review and meta-analysis of adults. Health Psychology Review, 13(1), 18–34. doi: 10.1080/17437199.2018.1530067
- Rhodes, R. E., & Kates, A. (2015). Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Annals of Behavioral Medicine, 49(5), 715–731. doi: 10.1007/s12160-015-9704-5
- Rhodes, R. E., Kaushal, N., & Quinlan, A. (2016a). Is physical activity a part of who I am? A review and meta-analysis of identity, schema and physical activity. Health Psychology Review, 10(2), 204–225. doi: 10.1080/17437199.2016.1143334
- Rhodes, R. E., Spence, J. C., Berry, T., Deshpande, S., Faulkner, G., Latimer-Cheung, A. E., … Tremblay, M. S. (2016b). Understanding action control of parental support behavior for child physical activity. Health Psychology, 35(2), 131–140. doi: 10.1037/hea0000233
- Rothman, A. J. (2004). Is there nothing more practical than a good theory?”: Why innovations and advances in health behavior change will arise if interventions are used to test and refine theory. International Journal of Behavioral Nutrition and Physical Activity, 1, 11. doi: 10.1186/1479-5868-1-11
- Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. doi: 10.1037/0003-066X.55.1.68
- Sacher, P. M., Kolotourou, M., Chadwick, P. M., Cole, T. J., Lawson, M. S., Lucas, A., … Singhal, A. (2010). Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity, 18(S1), S62–S68. doi: 10.1038/oby.2009.433
- Scaglioni, S., De Cosmi, V., Ciappolino, V., Parazzini, F., Brambilla, P., & Agostoni, C. (2018). Factors influencing children’s eating behaviours. Nutrients, 10, 706. doi: 10.3390/nu10060706
- Schumacker, R. E., & Lomax, R. G. (2010). A beginner’s guide to structural equation modeling (3rd ed). New York, NY: Routledge.
- Schwimmer, J. B., Burwinkle, T. M., & Varni, J. W. (2003). Health-related quality of life of severely obese children and adolescents. JAMA, 289(14), 1813–1819. doi: 10.1001/jama.289.14.1813
- Sniehotta, F. F., Schwarzer, R., Scholz, U., & Schüz, B. (2005). Action planning and coping planning for long-term lifestyle change: Theory and assessment. European Journal of Social Psychology, 35(4), 565–576. doi: 10.1002/ejsp.258
- Strachan, S. M., & Brawley, L. R. (2009). Healthy-eater identity and self-efficacy predict healthy eating behavior: A prospective view. Journal of Health Psychology, 14(5), 684–695. doi: 10.1177/1359105309104915
- Strachan, S. M., Brawley, L. R., Spink, K. S., Sweet, S. N., & Perras, M. G. M. (2015). Self-regulatory efficacy’s role in the relationship between exercise identity and perceptions of and actual exercise behaviour. Psychology of Sport and Exercise, 18, 53–59. doi: 10.1016/j.psychsport.2015.01.002
- Stryker, S., & Burke, P. J. (2000). The past, present, and future of an identity theory. Social Psychology Quarterly, 63(4), 284–297. doi: 10.2307/2695840
- Tabachnick, B. G., & Fidell, L. S. (2012). Using multivariate statistics (6th ed). Boston, MA: Pearson.
- Twig, G., Yaniv, G., Levine, H., Leiba, A., Goldberger, N., Derazne, E., … Kark, J. D. (2016). Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. New England Journal of Medicine, 374(25), 2430–2440. doi: 10.1056/NEJMoa1503840
- Tyson, N., & Frank, M. (2018). Childhood and adolescent obesity definitions as related to BMI, evaluation and management options. Best Practice & Research Clinical Obstetrics & Gynaecology, 48, 158–164. doi: 10.1016/j.bpobgyn.2017.06.003
- Wang, X., Ouyang, Y., Liu, J., Zhu, M., Zhao, G., Bao, W., & Hu, F. B. (2014). Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ, 349, g4490. doi: 10.1136/bmj.g4490
- Wang, Y., Wu, Y., Wilson, R. F., Bleich, S., Cheskin, L., Weston, C., … Segal, J. (2013). Childhood obesity prevention programs: Comparative effectiveness review and meta-analysis . Agency for Healthcare Research and Quality (US); Report No.: 13-EHC081-EF.
- Wilson, P. M., & Muon, S. (2008). Psychometric properties of the Exercise identity scale in a university sample. International Journal of Sport and Exercise Psychology, 6(2), 115–131. doi: 10.1080/1612197X.2008.9671857
- Yao, C. A., & Rhodes, R. E. (2015). Parental correlates in child and adolescent physical activity: A meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 12, 10. doi: 10.1186/s12966-015-0163-y
- Zajonc, R. B. (1980). Feeling and thinking: Preferences need no inferences. American Psychologist, 35(2), 151–175. doi: 10.1037/0003-066X.35.2.151
Appendix: Full Measures
Affective Attitude:
Healthy Eating:
For me, regularly supporting my child's healthy eating (e.g. increasing fruit and vegetable consumption and decreasing intake of sugary beverages) over the next two weeks would be:
For me, regularly supporting my child's healthy eating over the next two weeks would be:
Physical Activity:
For me, regularly supporting my child's moderate-to-vigorous physical activity (e.g. driving to practice, scheduling activities) over the next two weeks would be:
For me, regularly supporting my child's moderate-to-vigorous physical activity (e.g. driving to practice, scheduling activities) over the next two weeks would be:
Self-Regulation:
Healthy Eating:
I set short-term (daily or weekly) goals for how I could support my child's healthy eating behaviors last month.
If I did not reach my goal for supporting my child's healthy eating last month, I analyzed what went wrong.
I made plans regarding what to do if something made it difficult to support my child's healthy eating last month.
I made regular plans concerning ‘when,’ ‘where,’ ‘how,’ and ‘what’ kind of support I could provide for my child's eating behaviors and food choices last month.
Physical Activity:
I set short-term (daily or weekly) goals for how I could support my child's leisure-time physical activity last month.
I made regular plans concerning ‘when,’ ‘where,’ ‘how,’ and ‘what’ kind of support I could provide for my child's physical activity last month.
I made plans regarding what to do if something made it difficult to support my child's physical activity last month.
If I did not reach one of my goals for supporting my child's physical activity last month, I analyzed what went wrong.
Identity:
Healthy Eating:
I consider myself an individual who prepares healthy food and beverage choices.
When I describe myself to others, I usually include my commitment to eating healthy.
Others see me as someone who regularly eats healthy.
Physical Activity:
I consider myself an exerciser.
When I describe our family to others, I usually include something about our physical activities.
Others see us as a family that is regularly active.
Parental Support:
Healthy Eating:
During a typical week how often have you or another family member of your household:
Encouraged your child to eat more fruit.
Encouraged your child to eat more vegetables.
Bought fruit or vegetables you know your child likes.
Physical Activity:
I watch my child play sports or participate in other activities such as martial arts or dance.
I enroll my child in sports teams and clubs such as soccer, basketball, and dance.
I take my child to places where he/she can be active.