ABSTRACT
Background: Research suggests dyadic interventions can increase physical activity; such interventions are untested within postpartum parent couples.
Methods: A three-armed pilot randomized trial addressed this gap and tested which type of dyadic intervention is most effective. Inactive postpartum mothers and a significant other were recruited in Australia (n = 143 assessed for eligibility) and randomised in a single-blinded fashion (i.e. participants were blinded) to 1 of 3 dyadic conditions involving a single face-to-face session with access to web-based group support: a minimal treatment control (n = 34), collaborative planning group (n = 38), or collaborative planning + need supportive communication group (n = 30). Participants were asked to wear their accelerometers for 8 days and completed self-report measures at baseline, end of intervention (week 4), and follow-up (week 12). We expected dyads in the collaborative planning + need supportive communication group would have the greatest increases in Physical Activity (PA), autonomous motivation, and partners’ need supportive behaviours; and decreases in controlled motivation and controlling partner behaviours.
Results: Results from 51 dyads using Bayesian actor-partner interdependence models provided some evidence for a small positive effect on total PA at follow-up for postpartum mothers in the collaborative planning group and for partners in the collaborative planning + need supportive communication group. Furthermore, partners in the collaborative planning + need supportive communication group were more likely to engage in some vigorous PA. At follow-up, postpartum mothers in the collaborative planning + need supportive communication group scored lower on personal autonomous reasons.
Conclusions: The impact of prior specification mean intervention effects need to be interpreted with caution. Progression to a full trial is warranted.
Regular physical activity (PA) is associated with increased quality of life and health, and reduced risks of heart and breathing problems, high blood pressure, obesity and type 2 diabetes (Marques, Santos, Martins, Matos, & Valeiro, Citation2018). The current Australian PA guidelines suggest engaging in 150 minutes/week of moderate-intensity PA (e.g. walking briskly), 75 minutes/week of vigorous-intensity PA (e.g. jogging), or an equivalent combination of the two (Department of Health, Citation2019). One population group prone to inactivity is new parents. Research indicates that first-time mothers decrease their moderate to vigorous PA (MVPA) more than women without children across the first 12-months of child-rearing (Rhodes et al., Citation2014). Further, women who have a child living at home are significantly less likely to meet PA guidelines compared to women with no dependent children (Carson, Adamo, & Rhodes, Citation2018). A study of health care provider advice in the U.S.A. found that nearly four out of five women do not receive any advice on PA during the first 3-months of the postpartum period (Ferrari et al., Citation2010). Despite these concerns, parents with very young children have received limited attention in the PA literature and the studies conducted tend to focus on mothers only, use cross-sectional designs, and rely exclusively on self-reports to assess PA (Bellows-Riecken & Rhodes, Citation2008).
Strategies to improve the PA of mothers
Fathers’ role in supporting mothers’ PA is often neglected in current PA intervention programs. This omission is important because social support for PA seems to be a stronger predictor of PA for women than men (Leslie et al., Citation1999; Molloy, Dixon, Hamer, & Sniehotta, Citation2010; Phongsavan, McLean, & Bauman, Citation2007) and mothers with young children face challenges attending sessions designed to increase their PA (Fjeldsoe, Miller, & Marshall, Citation2013). The most prevalent reason as to why mothers find it difficult to prioritize their own PA is because they tend to put the needs of the family first (Lewis & Ridge, Citation2005). Hence, having family members providing support for the mother’s PA may help negate these barriers. In challenging situations, such as having a new child, people often turn to their romantic partners for support (Berli, Bolger, Shrout, Stadler, & Scholz, Citation2018) and such support could be leveraged to help mothers find time for PA. Furthermore, any health behaviour change in mothers may have a ripple effect on their partner’s health behaviour: if one partner adopts a new healthier behaviour, their spouse may be more likely to follow suit (Jackson, Steptoe, & Wardle, Citation2015). However, ripple effects may not always emerge; Hagobian et al. (Citation2016) reported that an intervention aimed to prevent excessive gestational weight gain, did not lead to untreated partners losing a significant amount of weight. Thus, further consideration of potential ripple effects is warranted along with ways to engage partners more in the intervention to potentially increase the likelihood of such ripple effects emerging.
One way to incorporate partners is to actively involve them in strategies designed to promote PA in the target individual. Parents have reduced opportunities to be active due to caring for young children (Hamilton & White, Citation2010a) and hence they need to plan how to incorporate PA into their daily schedules. Implementation intention plans involve an individual making a specific plan with the format: if I encounter situation X then I will do Y (e.g. IF it’s Tuesday night at 8pm THEN I will go to my aerobics class). Experimental research supports the use of implementation intentions to increase engagement in exercise when used alongside other techniques designed to foster motivation or further support (e.g. Milne, Orbell, & Sheeran, Citation2002; Prestwich, Lawton, & Conner, Citation2003; Prestwich, Perugini, & Hurling, Citation2009, Citation2010). Such plans can be adapted to permit input from partners.
Collaborative implementation intentions
Collaborative implementation intentions (Prestwich et al., Citation2005), involve pairs of individuals jointly planning when and where they will perform a target behaviour together. Co-participation in PA is an important way in which partners can provide support to each other. For instance, there is evidence that participants engage in more PA on days when their romantic partner joins them (Berli et al., Citation2018). Moreover, there is some evidence to support the use of collaborative implementation intentions to promote PA (Prestwich et al., Citation2012). This approach may provide a useful cue to action as well as increasing enjoyment of the target behaviour (Prestwich et al., Citation2005). However, in the context of promoting PA in new parents, the stipulation via collaborative implementation intentions that couples should engage in the target behaviour together may lead to practical difficulties unless mothers and fathers can keep their children with them during the activity or they are able to enlist childcare.
Dyadic plans
An alternative approach is dyadic planning which refers to target persons forming plans for their own PA together with their partner but enacting the target behaviour individually (Knoll et al., Citation2017). Knoll et al. (Citation2017) suggest dyadic planning can be useful when the medical need to increase PA only applies to one partner (e.g. promoting pelvic floor exercise for those with prostate cancer, Burkert, Scholz, Gralla, Roigas, & Knoll, Citation2011; promoting breast self-examination, Benyamini, Ashery, & Shiloh, Citation2011) or when there are strong barriers to performing PA together or insufficient opportunities to do so. If one person engages in PA, this frees their partner to perform other tasks (e.g. looking after the children). However, in some cases, mothers may experience a lack of opportunity for reciprocity (e.g. supporting their partner to exercise but no opportunity for them to do the same) (Hamilton & White, Citation2010b) – as such, providing opportunities for both parents to be physically active remains important. Further, relationship quality may influence the success of dyadic plans. Knoll et al. required romantic couples to make PA dyadic plans for either themselves or their partner over a 6-week period. The findings showed no direct effects of dyadic planning on the target person’s PA although their partners did initially increase their vigorous PA (these changes were not maintained at 6 weeks post-intervention). However, among couples that reported lower relationship quality, activity of the target person decreased for those who planned with a partner how they would engage in PA, when compared to those who planned their PA on their own.
While there is evidence that dyadic plans (Knoll et al., Citation2017) and partner-based interventions (Prestwich et al., Citation2014) have been found to have positive impacts on social support, given the advantages and disadvantages of collaborative implementation intentions and dyadic planning, a potentially better solution may be for parents to choose which of these two approaches is best for them. Moreover, to optimize both approaches, it is likely important to ensure that partners communicate in a motivationally supportive way about PA and their goals (e.g. using non-pressuring language). Consequently, there is a need to explore how supportive or undermining behaviours and communication from the immediate family influence PA levels in dyadic interventions. It is important to foster good quality communication if spouses or other family members plan to exercise together. According to Ryan and Deci (Citation2017), individuals will be more autonomously motivated when their significant other communicates with them in ways that support three basic psychological needs: autonomy (having choice), competence (feeling behaviour is enacted effectively) and relatedness (feeling connected to each other). In turn this can promote engagement in and enjoyment of PA (Ntoumanis, Quested, Reeve, & Cheon, Citation2018). Autonomous motivation refers to behavioural engagement due to intrinsic interests or personal value of the behaviour. In contrast, controlled motivation refers to behavioural engagement due to internal (e.g. feelings of guilt) or external pressures (e.g. from a spouse or a clinician), and is negatively associated with sustained PA engagement. These theoretical predictions have been supported by meta-analytic evidence (see Ntoumanis et al., Citationin press). This need supportive communication includes behaviours such as provision of choice, perspective taking, positive feedback, and unconditional regard (Lim & Wang, Citation2009). There is evidence to suggest that creating a need supportive environment enhances self- and other-efficacy beliefs to engage in PA (e.g. Jackson, Whipp, Chua, Dimmock, & Hagger, Citation2013).
As well as benefiting behaviour directly, autonomy support can strengthen the effect of planning-based interventions on behaviour. For instance, Koestner, Otis, Powers, Pelletier, and Gagnon (Citation2008) showed that delivering planning-based interventions in an autonomy-supportive way is more effective than delivering the same intervention in a more controlling manner. This literature, however, has focused on personal autonomy (i.e. ‘how much I enjoy PA’) rather than relational autonomy (i.e. ‘how PA is important to my relationship with others’; Gore, Bowman, Grosse, & Justice, Citation2016). People may engage in PA because this would benefit their loved ones (relationally autonomous reasons), because of their own interest and values (personally autonomous reasons), or because they are demanded or expected to by someone else (relationally controlled reasons), or due to external pressures, rewards or punishments (personally controlled reasons). It is currently unknown how such diverse personal and controlled reasons for PA engagement might affect PA levels in dyadic interventions.
The present research
To examine the role of collaborative planning (an approach which offers participants the choice between collaborative implementation intentions or dyadic planning) and need supportive communication in helping mothers and a significant other of their choice to increase PA levels, we designed and tested the Postnatal Exercise Partners Study (PEEPS). PEEPS is a 12-week pilot randomized controlled trial of a dyadic PA program, with participants assigned to one of three conditions: a minimal treatment control (i.e. dyads with no planning or need supportive communication training), collaborative planning, or collaborative planning with need supportive communication training. We examined whether mothers with young children, randomized to one of the 3 conditions, increased their PA via exercising with a significant other (e.g. the father of their child, a family member, a friend).
It was predicted that mothers and their partners assigned to a collaborative planning or a collaborative planning + need supportive communication condition would increase PA more so than a control group (H1), and that mothers and their partners in the collaborative planning + need supportive communication condition would increase PA over-and-above collaborative planning alone (H2). It was also expected that mothers and their partners in the collaborative planning + need supportive communication condition would report increases in need supportive partner behaviours (H3a), personal and relational autonomous motivation (H4a), and reductions in controlling behaviours (H3b) and personal and relational controlled motivation (H4b); we did not expect any changes in these variables in the other two conditions. Lastly, we hypothesized that confidence in the partner to exercise and to provide support would be greater for mothers and their partners in the two intervention groups than in the control (H5).
Method
Participants
Women were eligible if they had a child between the ages of 3 months to 2 years. Prior to the main trial, twelve postpartum parents (six dyads) participated in semi-structured interviews to discuss the barriers to exercise and the feasibility of collaborative planning and need supportive communication training in promoting mothers and fathers’ PA. The parents disclosed that mothers and fathers cannot always exercise together due to difficulties during childbirth, or differences in fitness within the couple. Based on these discussions, the postpartum mothers could self-select any significant other to take part with them, not just the father of their child. Mothers self-selected a significant other (e.g. their romantic partner) to participate in the study; hereafter we refer to the significant others as the ‘partner’. There were 43 romantic partner dyads, 3 friend dyads, and 5 family member dyads (see ). Both had to be over the age of 18 years, and somewhat active or not active (i.e. less than 24 units on the LSI index of an adapted version of Godin’s (Citation2011) PA Questionnaire). We originally excluded mothers who were pregnant or planning to become pregnant in the next 5 months. Due to the possible health benefits of exercising when pregnant and difficulties with recruiting the sample we changed this restriction. However, mothers who were pregnant or dyads who had health problems, as identified by the PA Readiness Questionnaire (PAR-Q; Canadian Society for Exercise Physiology, Citation2002), had to seek medical permission prior to participation in the study. Participants were recruited via flyers, Facebook posts, and face-to-face from family and parenting centres in Perth, Western Australia. A Monte Carlo simulation study (Muthén & Muthén, Citation2002) using Mplus version 8.2 showed that with a sample size of 51 dyads, studies that included informative priors (as described in the Statistical Analysis section) showed that only prior specifications representing higher degree of certainty on the variance parameters yielded around 80% power (range 78-83%) to detect a medium effect of the intervention on total PA. We had 25-26% power to detect a medium effect of the intervention on total PA when using noninformative priors. A medium effect size was defined as an unstandardized regression coefficient of 30.00, which corresponds to a difference of 30.00 minutes of total PA after the intervention between the intervention and control groups. This estimation is based on the expectation that the participants would meet the PA guidelines by the Australian Department of Health (Citation2019). We had up to 8 months available to recruit. Fifty-one mothers (mean age = 34.57 years + SD = 4.31 years), and 51 partners (mean age = 38.84 years + SD = 9.30 years) received a workshop (in person n = 18, or via Skype n = 10) or were sent a video recording of the relevant workshop (n = 74, see ). Most partners were spouses (n = 43).
Figure 1. Flow diagram to show participant numbers throughout the study.
Note. This list is not exhaustive; it includes the main reason for exclusion of each participant, but multiple criteria may have applied to one participant. Reasons for exclusion can apply to the participant, their partner or both. Numbers are based on the self-report data, as this was the minimum for participants to continue the study
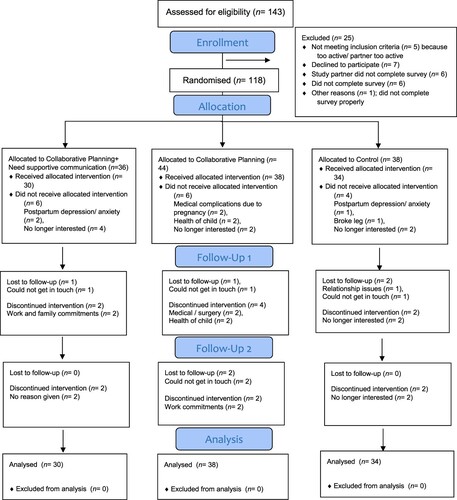
Table 1. Characteristics of the study sample at screening.
Measures
At screening, both dyad members reported their age, postcode, and the number of children they had living at home. Postpartum parents were asked if they had social support networks for childcare and if they breastfed, as such factors can influence PA levels (Evenson, Aytur, & Borodulin, Citation2009; Pereira et al., Citation2007). The following outcome measures were completed at baseline (week 0), post-intervention (week 4), and follow-up (week 12):
Primary outcome. PA, measured via GENEActiv accelerometers (Version 4.08a), based on recordings starting at 12:00md on the first day at 60 Hz for 8 days, at each time point. The data were converted to 60s epoch periods for analysis. Participants needed a minimum of 10 hours of wear time on 4 days for their data to be included in the analyses. Esliger et al.’s (Citation2011) criteria determined classifications into sedentary, light, moderate, and vigorous PA. Total PA was our primary outcome of interest.
Secondary outcomes. Specific PA categories (i.e. light, moderate, vigorous, total moderate and vigorous PA (MVPA), and sedentary time), as assessed by the GENEActiv accelerometers, were secondary outcomes. The Reasons for Health Scale by Gore et al. (Citation2016) was used to assess different motivations for PA. This scale makes a distinction between 4 types of motivation/reasons as to why people engage in PA. Following the stem ‘when I exercise I do so because’. participants rated how much they agreed with different statements (e.g. ‘the other people make it enjoyable’ (relationally autonomous reason), ‘of the fun and enjoyment it provides me’ (personally autonomous reason), ‘it is only important to someone close to me’ (relationally controlled reason), ‘I would feel guilty, ashamed, or anxious if I did not’ (personally controlled reason)) on a 1–5 (strongly disagree – strongly-agree) scale.
Need support provided by the partner was measured using an adapted version of the Williams, Grow, Freedman, Ryan, and Deci (Citation1996) scale. This measure requires participants to rate their degree of agreement (strongly disagree (1) – strongly agree (7)) with various statements (e.g. ‘I feel understood by my significant other’). Controlling partner behaviours were measured with an adapted version of the Bartholomew, Ntoumanis, and Thøgersen-Ntoumani (Citation2010) scale. Participants rated their degree of agreement (strongly disagree (1) – strongly agree (7)) with statements such as ‘my important other embarrasses me if I do not stick to my exercise regime’. An adapted version of the Shields and Brawley (Citation2006) self-efficacy for exercise questionnaire was used to assess relation-inferred self-efficacy (e.g. ‘how confident your study partner is in your ability to develop effective solutions to cope with potential barriers that can interfere with your exercise?’), confidence in the partner to exercise (e.g. ‘how confident are you that your study partner can schedule exercise sessions into his/her weekly routine so that s/he gets at least 30 min of exercise a day, 5 times per week?’) and confidence in the partner to provide support (‘how confident are you that your study partner can support you to set realistic, weekly exercise goals (e.g. ‘exercising 5 days/week?’)), along a 5-point scale (No confidence at all (1) – Complete confidence (5)). Internal consistency estimates for all scales are presented in Table S1. The personal controlled reasons for exercise measure is not presented in the Results due to low internal consistency (i.e. Cronbach’s alphas between −0.60 and 0.50). Control variables i.e. accelerometer wear-time, age, socioeconomic index, number of children, social support and breastfeeding were also measured.
Design and procedure
This three-armed RCT was approved by the ethics board at Curtin University, Western Australia, approval number HRE2017-0045-04. An un-blinded investigator was responsible for recruitment and data collection. Participants were provided a link to an online consent form and a screening survey. When screening participants, we found some had difficulty completing the Godin (Citation2011) survey online (e.g. reporting minutes performing the activities instead of the number of times), so this data was collected via email/phone instead. Participants were provided an information sheet. A website link to complete the measures was sent to the participants at each time point. Participants could also attend the university and be fitted with the accelerometer by the lead author or receive it by post (posting it back after 8 days of wear). Dyads were provided the following written instructions: wear the accelerometers on your non-dominant hand continuously for 8 days, with the numbers on the accelerometer facing upright. The dyads were randomized when at least one member of the dyad completed the baseline survey; both members of the dyad were required to complete the survey to receive the workshop (see ). Dyads were randomized by the lead author in equal proportions to one of the three groups using a computerized random number generator. In week 1, dyads attended a face-to-face workshop at a local University or a family and parenting centre in Western Australia. Not all participants were recruited at the same time, so there were several workshops and assessment sessions over a period of 6 months. The recording for the control group lasted 25 minutes, the collaborative planning condition 32 minutes, and the collaborative planning + need supportive communication condition 40 minutes. Participants were classed as receiving the allocated intervention when they watched the workshop video online or attended in person. They were required to email the researcher with the date they watched the workshop video online. Participants were told their group number but were unaware whether they were in the control or one of the two intervention conditions. Participants were offered a A$30 supermarket gift card ($60 per dyad) if they completed questionnaires at all 3 time points.
Control condition
In the workshop, the control group received general information about PA, current recommendations, and discussed the opportunities and barriers to being physically active. The dyads spent 5–10 minutes thinking about whether to exercise together or separately and setting a goal for the desired activity (e.g. ‘I will play tennis twice a week’). They were encouraged to discuss with their partner what they wanted to do. The aim was to reach the Australian PA guidelines (Department of Health, Citation2019) (i.e. engaging in 150 minutes/week of moderate-intensity PA, 75 minutes/week of vigorous-intensity PA), but they did not receive any targeted strategies beyond this information. Six participants received the workshop face-to-face; the majority received the workshop online (n = 28).
Intervention conditions
Collaborative planning condition. Participants received an expanded version of the control group’s workshop. Six participants received the workshop face-to-face; the majority received the workshop online (n = 32). Collaborative implementation intentions require two people to identify and plan the specific target behaviour (e.g. PA) they will do together in specific situations. For this study, to enable greater planning flexibility, participants were not required necessarily to perform PA together. Consequently, we deviated slightly from prior collaborative implementation intention research (e.g. Prestwich et al., Citation2012), and thus we refer to our plans as ‘collaborative plans’. Mothers and their partners discussed together when and where they would go about increasing PA and the types of PA, they would find enjoyable and convenient to do. Specifically, mothers and their partners were required to both make their own collaborative plans to work towards meeting the Australian PA guidelines (Department of Health, Citation2019) but could do this either in the format ‘if it is situation (X) then WE will do (Y)’ (a collaborative implementation intention) or in the format ‘if it is situation (X) then I will do (Y) and my study partner will do (Z)’ (a variant of a dyadic plan). For example, if it is Monday, Wednesday, or Friday when my husband is home from work, then I will go for a walk in the park and my study partner will care for our baby.
Collaborative planning + Need supportive communication condition. Participants received an expanded version of the collaborative planning condition’s workshop, and a general introduction on need supportive communication based on Self-Determination Theory (SDT) (Ryan & Deci, Citation2017). Six participants received the workshop face-to-face; the majority received the workshop online (n = 24). The dyads received a list of need supportive (see examples below) and controlling strategies (e.g. ‘discouraging questions or alternative opinions from your partner’ or ‘uttering your demands without explanations’). They were asked to write what they will say to each other, and what they would avoid saying to each other. They were presented with fictitious scenarios of dyads encountering difficulties when exercising and discussed what each person could say to make their partner feel supported in terms of their needs for autonomy, competence, and relatedness. Examples included (a) ‘Encourage a sense of choice for your partner when planning physical activities’ (autonomy support), (b) ‘Give positive, accurate and meaningful feedback’ (competence support), (c) ‘Give empathetic responses, acknowledge difficulties and negative feelings’ (relatedness support) (adapted from Hancox, Ntoumanis, Thøgersen-Ntoumani, & Quested, Citation2015).
E-social support
After the workshop the dyads were invited to join a password-protected Facebook group, one for each condition, to share their experiences and discuss materials. The Facebook group for the control condition involved sharing exercise tips or websites, the collaborative planning condition Facebook group shared their success and failures in pursuing their plans, and the collaborative planning + need supportive communication Facebook group shared tips on need supportive communication. Dyads were also provided access to a website, customized for each group. On that website, they could view the current PA guidelines (all groups), a planning flowchart detailing the steps to take in forming plans to exercise either together or separately, and some example plans (collaborative planning and collaborative planning + need supportive communication), and communication tips using appropriate scenarios (collaborative planning + need supportive communication). In weeks 2-4, weekly text messages were sent to the dyads in the two intervention conditions to elicit feedback on their use of the plans (collaborative planning; collaborative planning + need supportive communication) and their communication styles (collaborative planning + need supportive communication). In week 4, dyads were invited by the researcher to discuss via phone or email the materials and to make new plans and, if in the collaborative planning + need supportive communication group, to also discuss their communication strategies.
Statistical analysis
Mplus version 8.2 (Muthén & Muthén, Citation1998–2018) was used for all analyses. To examine the effects of the intervention, we used Bayesian actor-partner interdependence models (APIM; Kenny & Ledermann, Citation2010). The APIM takes into account the interdependency within dyads both within and across time points. Separate models were estimated for the effects at post-intervention (i.e. after 4 weeks) and follow-up (i.e. after 12 weeks); we controlled for baseline scores in all models (cf. Vickers & Altman, Citation2001). To assess within-group differences over time we compared baseline vs. post-intervention, baseline vs. follow-up, and post-intervention vs. follow-up, using Hedges’ gav as effect size estimate (Lakens, Citation2013). Effect size magnitudes of 0.20, 0.50, and 0.80 were used to indicate small, medium, and large effect sizes (Cohen, Citation1988). Means and standard deviations (presented in and ) were based on estimated sample statistics using the full-information maximum likelihood estimator (Enders, Citation2010) that included the control variables.
Table 2. Within-group estimates of actors’ total physical activity, sedentary time, and psychosocial outcomes, at baseline, post-intervention, and follow-up.
Table 3. Within-group estimates of partners’ total physical activity, sedentary time, and psychosocial outcomes at baseline, post-intervention, and follow-up.
In a first set of analyses two dummy coded variables representing the collaborative planning group and the need supportive communication-collaborative planning group, respectively, were included as predictors to assess the main effects of the intervention (i.e. the control group was used as comparison group). In a second set of analyses we used a contrast coding that compared the effect of the two intervention groups (i.e. need supportive communication-collaborative planning group vs. collaborative planning group). We also included a number of control variables in the analyses (described in the measures section of this report). To account for the skewed data of vigorous PA (i.e. some participants had zero minutes) we estimated a two-part regression model (Baldwin, Fellingham, & Baldwin, Citation2016). The two-part regression model has a binary part describing the probability of a non-zero value in vigorous PA, and a continuous part for the rest of the distribution (Muthén, Muthén, & Asparouhov, Citation2017; Olsen & Schafer, Citation2001). Parameter estimates were evaluated using the 95% credibility intervals. If the interval did not include zero, a parameter was considered as a credible and statistically significant estimate (Zyphur & Oswald, Citation2015). Missing data were handled by including all available information in the analyses, similar to full-information maximum likelihood estimation (Asparouhov & Muthén, Citation2010; Enders, Citation2010).
The Bayesian APIMs were estimated using four Markov chain Monte Carlo chains and 100,000 iterations. The first 50,000 iterations were discarded as burn-in and the remaining 50,000 iterations were used to estimate the posterior distribution of the parameters. Chain convergence was assessed using the potential scale reduction factor (PSFR; Brooks & Gelman, Citation1998), with a low (e.g. <1.05) and stable PSFR being considered as evidence of chain convergence. Model fit was evaluated using the posterior predictive p (PPP) value and its accompanying 95% confidence interval. PPP values around 0.50 with a 95% CI centering on zero were considered as evidence of a well-fitting model, whereas a low PPP value and a 95% confidence interval with a positive lower limit were used as evidence of a poor fitting model (Asparouhov & Muthén, Citation2010). The deviance information criterion (DIC) was used to compare models with different prior specifications; a lower DIC value indicates better model fit (Zyphur & Oswald, Citation2015). A DIC difference of 1–2 indicate that both models deserve consideration, whereas a difference of 3–7 (or more) between two competing models is considered evidence that the model with lower DIC has considerably more support (Spiegelhalter, Best, Carlin, & Van Der Linde, Citation2002).
We attempted to find previous studies from which we could derive priors for the main outcome total PA, but we were unable to locate prior information (i.e. point estimates) that could be directly applied to our analyses. For example, Carr et al.’s (Citation2019) meta-analysis found a small positive effect (i.e. g = 0.20) of dyad interventions on PA of any type, however, translating this effect size to minutes of total PA is challenging, and no straightforward guidelines are available for such translation. Prestwich et al. (Citation2012) used a similar design as the one in our study but assessed PA using self-report measures, not accelerometers, which makes the metric of the PA variables in the two studies incompatible. However, Prestwich et al. reported effect size estimates for the comparisons between groups and found small to medium effects of the dyad intervention, with Cohen’s ds ranging from approximately −0.15 to 0.60, depending on comparison group, PA measure, and measurement point.
Despite the lack of directly compatible sources to derive prior information, we hypothesized that the dyad intervention would have a positive effect on the participants’ total level of PA, hence, we specified informative mean and variance priors on the regression coefficients of the intervention effects, based on effect size estimates in Carr et al. (Citation2019) and Prestwich et al. (Citation2012). Based on Carr et al. (Citation2019), we specified a prior mean of 15 to reflect a small effect of the intervention, which represents a difference of 15 minutes of total PA per day between the intervention group and control group at post-intervention and follow-up. Two different variance priors were examined, representing higher (SD = 7.5) and lower (SD = 15) degree of certainty in the prior mean. Based on Prestwich et al. we specified a prior mean of 30 to reflect a medium effect of the intervention, which represents a difference of 30 minutes per day between the intervention and control groups. Two different variance priors were examined, representing higher (SD = 15) and lower (SD = 30) degree of certainty in the prior mean. The same prior specification was used for the comparisons between the two intervention groups (i.e. need supportive communication-collaborative planning group vs. collaborative planning group). For the remaining parameters and the rest of the analyses, we relied on the default noninformative prior specification in Mplus (see Muthén & Muthén, Citation1998–2018, p. 775, for a description of the default priors when Bayesian estimation is used).
To understand the impact of the informative priors on the results we compared estimates from models with noninformative priors and informative priors by computing a percent relative deviation [(parameter estimate with informative priors) – (parameter estimate with noninformative priors)/(parameter estimate with informative priors)]*100 (Depaoli & Van de Schoot, Citation2017). If the size of the discrepancy is small (e.g. <1%) or moderate (e.g. 1–10%) and the substantive conclusions remain the same, the subjectivity of the prior has no impact or a small to moderate impact on the results. If, however, the discrepancy is moderate (e.g. 1–10%) or large (e.g. >10%), and the substantive results differ, the subjectivity of the prior has had a large impact on the results.
Results
Descriptive statistics and within-group differences over time
Characteristics of the sample at screening are presented in . Descriptive statistics for actors’ and partners’ total PA, sedentary time, wear time and number of valid days, and psychosocial outcomes at baseline, post-intervention, and follow-up are presented in and , respectively. For actors, most effect sizes were in the small to medium range, and few consistent within-group effects were observed. For partners, most of the effect sizes were small (i.e. below 0.20). Descriptive statistics and effect size estimates of the within-group differences over time for light, moderate, vigorous, and MVPA are presented in the supplemental material Tables S2–S3. All the analyses were pre-specified and based on the 51 mothers (actors) and 51 partners in their originally assigned groups.
Between-group differences at post-intervention and follow-up
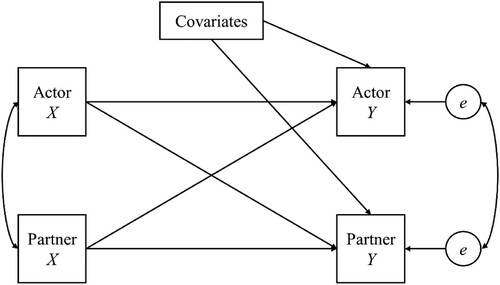
The APIM is graphically depicted in . All effects within and between dyad members were freely estimated. We tested separate models for each outcome variable and for the effects at post-intervention and follow-up.
Figure 2. The actor-partner interdependence model. X and Y indicate measured variables and e denotes residual variance.
Primary outcome: Total PA. The results from the APIMs evaluating the intervention effects at post-intervention on total PA are presented in . Based on the DIC, Model E1 received less support than Models B1 and C1 (i.e. DIC difference of 3). The DIC difference was 2 or less between Models B1, C1, and D1, hence, all of these models deserve consideration. Whereas Models B1 (prior mean = 15, SD = 15), and D1 (prior mean = 30, prior, SD = 30) indicated that the intervention effects were not credible (i.e. the 95% CIs included zero), the results from Model C1 (prior mean = 15, prior, SD = 7.5) indicated a credible effect for actors in the collaborative planning group (B = 15.54, 95% CI [1.55, 29.54]) and partners in the collaborative planning + need supportive communication group (B = 15.37, 95% CI [0.98, 29.65]). It is also noticeable that the percent relative deviation was large for all estimated intervention effects (i.e. > 100%), indicating a large impact of the prior specification in the results. Taken together, based on Model C1 with informative priors, we can infer that the intervention had a small positive effect on actors in the collaborative planning group and partners in the collaborative planning + need supportive communication group at post-intervention.
Table 4. Intervention effects at post-test on total physical activity for actors and partners.
Comparisons between the two intervention groups at post-test indicated that Models A2 and E2 received less support than Models B2, C2, and D2. These latter three models all deserve consideration due to a DIC difference of 1 or less (). Whereas Model B2 (prior mean = 15, SD = 15) and D2 (prior mean = 30, SD = 30) indicated that the effect of the intervention was not credible, Model C2 (prior mean = 15, SD = 7.5) indicated a credible effect for partners (but not for actors) in the need supportive communication-collaborative planning group over and above partners in the collaborative planning group (B = 15.67, 95% CI [1.27, 30.13]). Based on these results from Model C2 we can tentatively conclude that the intervention had a stronger effect for partners (but not for actors) in the need supportive communication-collaborative planning group compared to partners in the collaborative planning group. However, the percent relative deviation was large also for these analyses, indicating a large impact of the prior specification on the results. Similar results were observed at follow-up (see ). Model J1 (prior mean = 30, SD = 15) received considerably less support then Model G1 (prior mean = 15, SD = 15), indicated by a DIC difference of 3. The DIC difference between Models G1, H1, and I1 was 2 or less, indicating that they all deserve consideration. Whereas Models G1 (prior mean = 15, SD = 15) and I1 (prior mean = 30, SD = 30) indicated that the intervention effects were not credible, the results from Model H1 (prior mean = 15, prior SD = 7.5) indicated a credible effect for actors in the collaborative planning group (B = 17.15, 95% CI [2.86, 31.40]) and partners in the collaborative planning + need supportive communication group (B = 16.39, 95% CI [2.12, 30.62]). The percent relative deviation for actors in the collaborative planning group in Model H1 was 65.78%, whereas the percent relative deviation for the effect on partners in the collaborative planning + need supportive communication group was 34.36%. The percent relative deviation for the remaining effects with priors in Model H1 was large (i.e. >100%). The discrepancy between the parameter estimates with noninformative priors and informative priors indicate that the prior specification had a large impact on the results. Taken together, based on Model H1 with informative priors, the intervention had a small positive effect on actors in the planning group and partners in the collaborative planning + need supportive communication group at follow-up.
Table 5. Effect of collaborative planning + need supportive communication vs. collaborative planning at post-test on total physical activity for actors and partners.
Table 6. Intervention effects at follow-up on total physical activity for actors and partners.
Comparisons between the two intervention groups at follow-up indicated that Model J2 received less support than Models G2 and I2 (DIC difference of 3). Models F2, G2, H2, and I2 were all deserve consideration due to a DIC difference of 1 or less (). Whereas Models F2 (noninformative priors), G2 (prior mean = 15, SD = 15), and I2 (prior mean = 30, SD = 30) indicated that the effect of the intervention was not credible, Model H2 (prior mean = 15, SD = 7.5) indicated a credible effect for partners (but not for actors) in the need supportive communication-collaborative planning group over and above partners in the collaborative planning group (B = 16.84, 95% CI [2.47, 31.17]). Based on these results from Model H2 we can tentatively conclude that the intervention had a stronger effect for partners (but not for actors) in the need supportive communication-collaborative planning group compared to partners in the collaborative planning group. However, the percent relative deviation was large for these analyses, indicating a large impact of the prior specification on the results.
Table 7. Effect of collaborative planning + need supportive communication vs. collaborative planning at follow-up on total physical activity for actors and partners.
To summarize, based on models with informative priors on the means (M = 15) and SDs (SD = 7.5) of the intervention effects we tentatively conclude that the intervention had a small positive effect on actors in the collaborative planning group and partners in the collaborative planning + need supportive communication group at post-intervention and follow-up. We also observed a small positive effect for partners in the collaborative planning + need supportive communication group over and above partners in the collaborative planning group. However, due to the large impact of the prior specification on the results and similar model fit observed for models not indicating a credible effect, these findings need to be interpreted with caution.
Secondary outcomes: PA categories and self-reports. The intervention effects on the secondary outcome variables are presented in Tables S4–S29 in the supplemental material. Partners in the collaborative planning + need supportive communication group were 3.68 (95% CI [1.45, 6.82]) times more likely to have non-zero minutes of vigorous PA at follow-up, compared to the control group (Table S7). Actors in the collaborative planning + need supportive communication group scored lower on personal autonomous reasons (B = −0.51, 95% CI [−0.86, -.015]), and partners in the collaborative planning + need supportive communication group scored lower on confidence in their partner’s support (B = −0.82, 95% CI [−1.37, −0.27]) at follow-up, compared to the corresponding values in the control group (see Tables S9 and S14). No other credible intervention effects were observed on the secondary outcome variables.
Comparisons between the two intervention groups showed that actors in the collaborative planning + need supportive communication group had more sedentary time than actors in the collaborative planning group at post-test (B = 59.72, 95% CI [2.91, 116.95]) and follow-up (B = 65.52, 95% CI [8.96, 122.23]; see Table S17). Actors in the collaborative planning + need supportive communication group also engaged in less light PA at follow-up (B = −55.86, 95% CI [−110.09, 1.693]) than actors in the collaborative planning group (Table S18). Partners in the collaborative planning + need supportive communication group were 3.11 (95% CI [0.64, 6.15]) times more likely to have non-zero minutes of vigorous PA at follow-up, compared to partners in the collaborative planning group (Table S20). No other credible differences were observed between the two intervention groups.
It is also noticeable that the partners’ sedentary time had credible and positive effects on the actors’ sedentary time at post-intervention (B = 0.35, 95% CI [0.10, 0.60]) and follow-up (B = 0.27, 95% CI [0.38, 1.06]; see Table S4). Partners’ levels of moderate PA also had credible and positive effects on actors’ levels of moderate PA at post-intervention (B = 0.24, 95% CI [0.04, 0.43]) and follow-up (B = 0.43, 95% CI [0.21, 0.64]; see Table S6). Partners’ levels of total MVPA also had credible and positive effects on actors’ levels of total MVPA at post-intervention (B = 0.25, 95% CI [0.05, 0.44]) and follow-up (B = 0.43, 95% CI [0.20, 0.64]; see Table S8). Hence, partners’ sedentary time, moderate PA, and total MVPA appear to be associated with actors’ sedentary time, moderate PA, and total MVPA over time. We also noted that actors’ personal autonomous reasons at baseline had a credible and positive effect on partners personal autonomous reasons at follow-up (B = 0.31, 95% CI [0.05, 0.56]). Hence, actors’ personal autonomous reasons seem to have a long-term association with partners’ personal autonomous reasons (see Table S9).
Engagement
Engagement with the Facebook groups was poor. In the collaborative planning + need supportive condition 1 participant posted twice on their page; in the control condition 2 participants posted once on their page; no participants posted on the collaborative planning condition’s page. As this is a pilot study, we also explored the types of plans set. We do not have this information for some participants, primarily because although we offered to provide advice on the participants’ plans, only a minority of participants shared them. Based on the available data from 29 individuals, 21 individuals planned to engage in PA both together and separately; 8 individuals planned to only exercise separately; 0 individuals planned to exercise together all the time.
Discussion
In this 3-group RCT we examined the role planning and need supportive communication might play in helping mothers and a significant other of their choice to increase PA levels and improve their motivation and confidence for PA. We compared changes at post-intervention and follow-up across groups. Analysis of dyadic data differs from traditional analyses, as it is the study of non-independence of observations from the two dyad members (Kenny, Kashy, & Cook, Citation2006). Statistical analyses tend to assume that participants are sampled from the general population: dyadic analysis violates this assumption (Fitzpatrick, Gareau, Lafontaine, & Gaudreau, Citation2016). Given we recruited dyads purposely, so we could study the influence one dyad member may have on the other, we focus mainly on the actor-partner interdependence model results. The results showed a positive effect of the intervention on changes in total PA for actors in the collaborative planning group, and for partners in the collaborative planning + need supportive communication group at post-intervention and follow-up, compared to the control condition. These effects were small, but in line with the meta-analysis by Carr et al. (Citation2019) on dyadic interventions to promote PA. We found partial support for H1, as the differences in PA between the control group and the two experimental groups were not equivalent for actors and partners.
Actors had greater total PA in the collaborative planning condition compared to the control condition at the follow-up. This effect was mainly driven by increases in light activity (see Table S2). It could be that light activity is more manageable in this population, as first-time mothers attend to the daily workload of infant care and thus shift from sedentary behaviour to light activity (Rhodes et al., Citation2014). During our feasibility interviews in the development phase, mothers alluded to difficult births and how child-birth complications hindered their intentions to undertake MVPA, thus light PA is easier to participate in. Further, there are many time-consuming responsibilities that are linked to infant care, such as household chores and returning to work (Connolly, Feltz, & Pivarnik, Citation2014), with many of these responsibilities involving light PA. Need supportive communication training may be less important for light PA and possibly counterproductive as light PA can be accumulated through partaking in chores and childcare tasks.
In partial support of H2 (which predicted that mothers and their partners in the collaborative planning + need supportive communication condition would have higher PA compared to participants in the collaborative planning only condition), a credible effect was found for partners but not actors. Partners (84% of whom were spouses) in the need supportive communication + collaborative planning group increased their total PA over and above partners in the collaborative planning group. Based on these results we can tentatively conclude that the intervention had a stronger effect for partners (but not for actors) in the need supportive communication-collaborative planning group compared to partners in the collaborative planning group. Partners in the collaborative planning + need supportive were also more likely to engage in some vigorous activity at follow-up compared to partners in the collaborative planning condition. Given that planning was a focus in both conditions, partners might have benefitted more from the motivational support available in the collaborative planning + need supportive communication condition. Such support might be less important for light PA which is easier to carry out and more incidental (Merom et al., Citation2014). Nevertheless, this explanation is tentative, given that there were no differences across conditions in perceptions of need supportive behaviours.
It is important to note that the priors did have a large impact on the results related to total PA (i.e. as indicated by the percent relative deviation). For some intervention effects (mostly at the post-intervention) there were relatively large differences in the magnitude, sign, and interpretation of the effects between models with informative and noninformative priors (Van de Schoot & Depaoli, Citation2014), which needs to be taken into consideration when interpreting the findings. The differences between models with informative and noninformative priors at post-intervention potentially reflect that parents need more time to implement their plans and motivation strategies than the time frame of our study. Parents may feel they have limited time to reflect on the strategies or they may take longer to start using them after the workshop, due to their childcare commitments. Thus, more time for reflection and practice could be useful. However, the large impact of the prior specification on the results and the similar model fit observed for models not indicating a credible effect, suggests that these findings need to be interpreted with caution.
Motivation and confidence
We found no support for Hypotheses 3-5. Contrary to H3a, H3b, and H4b, there were no group differences in need supportive behaviours, controlling behaviours, or controlled motivation. Previous research has shown that need supportive training of 1–3 hours in duration, produces greater effect sizes than longer or shorter durations of the same training (Su & Reeve, Citation2011). As our collaborative planning + need supportive communication video was 40 minutes in duration, this might have been too short to produce increases in need support. Our training was relatively brief because mothers had limited time for the intervention and asking them to engage in a 3-hour workshop would not be feasible.
The findings for H4a and H5 were surprising. At the follow-up, compared to the control condition, actors in the collaborative planning + need supportive communication group scored lower on personal autonomous reasons (counteracting hypothesis H4a), and partners scored lower on confidence in the mothers’ ability to support them (counteracting hypothesis H5). It is possible that in the collaborative planning + need supportive communication condition actors, through increased knowledge about motivation, were more able to accurately assess their degree of autonomous motivation, compared to the other groups which received no need supportive communication training. Our study found carrying out plans to exercise together was not practical for many parent dyads. This may have led to decreased autonomous motivation and less confidence in partner support. We tentatively suggest that mothers, being time poor, did not sufficiently engage with the intervention, and, thus, were able to realize that their autonomous motivation for PA was low; their partners were also able to discern this lack of engagement by having less confidence in the mothers to support them.
Actor-partner effects
We also found some concordance among dyads, although we did not have any specific hypotheses for these relations. Over time, partners’ sedentary time, moderate PA, and total MVPA were associated with actors’ corresponding values. Also, personal autonomous reasons for PA for actors at baseline were positively associated with personal autonomous reasons for partners at the follow-up. These findings indicate that a ripple effect may have taken place between the mothers’ activity and reasons for exercise, and their partners’ corresponding values (or vice versa). The findings support past research, which has found that if one partner adopts a new healthier behaviour, their spouse may be more likely to follow suit (Jackson et al., Citation2015). Balneaves et al. (Citation2014) also found that taking part in a lifestyle intervention, for some women had a positive health behaviour ripple effect to partners, children, and friends. These findings are unsurprising, given the literature on romantic partners has shown that health behaviours are concordant across couples (Arden-Close & McGrath, Citation2017) and people often partner with others of a similar health status (Van Dellen, Boyd, Ranby, MacKillop, & Lipkus, Citation2016). There is also evidence of similar associations in best friend dyads’ PA (Lopes, Gabbard, & Rodrigues, Citation2013), and parent–adolescent dyads in terms of autonomous motivation (Dwyer et al., Citation2017). Recruiting both mothers and their partners to our intervention, may have increased the likelihood of ripple effects emerging, as an intervention aimed to prevent excessive gestational weight gain, did not lead to untreated partners losing a significant amount of weight (Hagobian et al., Citation2016).
Strengths, limitations, and future research directions
We have shown that it is possible to recruit postpartum mothers and, to a large extent, their spouse to a dyadic PA intervention. This study provided an opportunity for postpartum mothers to take part in a PA intervention, without leaving their home, overcoming the barriers of inconvenient locations and high costs associated with postnatal PA classes (Saligheh, McNamara, & Rooney, Citation2016). We were inclusive in our approach and allowed mothers to self-select any significant other, increasing generalizability. We also provided more choice than Prestwich et al. (Citation2012), as participants could exercise together or separately. Strengths of our study also include the use of a RCT design and the testing of two treatments groups against a minimal treatment group, the use of both face-to-face and online components, and the objective assessment of both actor and partner PA and sedentary behaviour. This dyadic intervention to promote PA uses SDT as one of its theoretical frameworks and compares the use of collaborative planning with and without need supportive communication training.
As with all real-world interventions, this study had limitations. We did not pre-register the trial. Pre-registering is becoming increasingly important as it prevents the selective reporting of outcomes, helps the public know trials they could enrol in, and avoids unnecessary duplication (International Committee of Medical Journal Editors, Citation2020). However, the trial was submitted to the lead author's University, by means of a PhD feasibility proposal and the lack of significant findings indicates outcomes were not selectively reported.
Most of the analyses were underpowered to detect significant effects. The analyses which were adequately powered (based on the Monte Carlo Simulations) are the ones with highly informative powers. Many pilot studies have fewer than 18 participants per group, we do not know as much about the efficacy of intervention conditions with data from a small sample (Leon, Davis, & Kraemer, Citation2011). We had group sizes ranging from 30–38 participants at baseline, but some people did not complete all the surveys or wear the accelerometers. A pilot study should incorporate testing of the outcome measures and serves to help develop the intervention (Leon et al., Citation2011). Yet, a pilot study should not be considered a run-through of whether the hypotheses were supported (Leon et al., Citation2011). We went beyond a traditional pilot study by including formal hypotheses testing, even though there was limited knowledge about the intervention and its effect on the population being studied (postpartum mothers). The smaller sample size in pilot studies contributes to why hypothesis testing is not strictly needed. Given the small sample, the results of all analyses should be interpreted with caution. Yet, we felt it was important to get a sense of which intervention treatments might have worked and which did not work in terms of postpartum mothers and their partners’ PA.
In relation to specific components of the intervention, engagement with the Facebook website was poor; in fact, no participants posted on the collaborative planning condition’s page. This may be due to the small number of participants who were in the groups at any given time, as the workshop sessions were staggered over 6 months. The groups were designed to promote social connectedness, but participants waited for the researcher to initiate discussions, possibly because they did not know other participants. In hindsight, we should have initiated discussions among participants with researcher-led tips or invited their Facebook friends to join (as in Kernot, Olds, Lewis, & Maher, Citation2014).
If the participants attended a face-to-face session to meet others, they may have been more likely to engage in online discussion. We intended to run face-to-face workshops with groups of 3–4 pairs. The workshops were designed to prompt discussion among the dyads about how they can overcome barriers and to offer suggestions to the wider group. Most participants (n = 84) opted to watch a video of the workshop at home (for 10 individuals the researcher was also present), which is indicative of the challenges of offering a face-to-face intervention with this time poor population group. Thus, they missed out on connecting with a wider group. Miller, Trost, and Brown (Citation2002) found that mothers who received printed information and participated in discussion groups with other young mothers were more likely to achieve PA recommendations compared to a control group.
We encouraged the dyads in the control condition to spend 5–10 minutes thinking about whether to exercise together or separately and setting a goal for the desired activity (e.g. ‘I will play tennis twice a week’). They were encouraged to discuss with their partner what they wanted to do. This process may this have led to some participants in this condition forming collaborative plans, although they did not receive any targeted planning strategies. This might have contributed to the somewhat limited intervention effects in increasing levels of PA.
We encouraged the dyads to create plans to exercise together or separately (while their partner provided support). This task proved challenging for dyads where the partner worked full-time or lived separately. We encouraged some pairs to phone each other to ‘check-in’ when exercising separately (e.g. to ask their partner if they managed to carry out their plans or to offer need support). Prestwich et al. (Citation2012) found that when dyads plan to exercise together, they have greater PA compared to planning individually or not planning. It seems that some mothers and their partners made dyadic plans (i.e. target persons forming plans for their own PA together with their partners, see Knoll et al., Citation2017), while most individuals made a combination of dyadic and collaborative plans. Thus, we deviated slightly from previous collaborative implementation intention research where dyads needed to exercise together. The dyad may not always be able to engage in PA together due to childcare commitments or differences in ability/difficulties during childbirth. Future studies should explore further strategies to help parent dyads support each other when exercising individually (e.g. supportive phone calls/checking-in with their partner), as collaborative implementation intentions were not suited for many dyads which comprised of postpartum mothers.
Participants selected a somewhat active or not active partner, (i.e. they both had to score less than 24 units on the LSI index of an adapted version of Godin’s (Citation2011) PA Questionnaire) which sometimes meant they settled for their second choice of partner or someone of a similar low PA status. Future studies could explore whether greater PA is achieved through pairing an inactive individual with an active partner. It may be useful to pair participants with a physically active role model of a similar status who could serve as their inspiration (e.g. a physically active mother who balances PA with the demands of childcare). These role models could work with the participants to provide support and promote PA.
Finally, mothers, being time poor, may not readily engage with PA interventions. The mothers who signed up to join our study may not be reflective of the general population. They may have been more motivated to fit PA around their childcare commitments than other mothers who declined the trial, as childcare commitments did not stop them from signing up to the study. It would be useful to interview mothers who were participating as well as decliners, to find out what recruitment strategies are most acceptable and the barriers to taking part. The outcomes of these interviews would be particularly warranted if we decided to conduct a full definitive trial, as we would need to recruit a larger sample size.
To make the results more generalizable to different categories of families it may have been useful to explicitly target Facebook groups or face-to-face support groups for other types of family situations. Recruitment strategies could be further improved by setting-up a group of parents from different backgrounds (e.g. work full-time/unemployed, have childcare/no childcare, previously was active/never active). We did not manage to recruit any same-sex couples to the study. We are also unaware if the participants’ child(ren) were adopted or biological, or if they were from ‘nuclear or blended families’. These groups of parents could provide feedback on the recruitment flyers and patient-facing documentation, to help us recruit parents from as many different family situations as possible. However, generalizability of the study was aided by recruiting through a variety of mediums including flyers, Facebook posts, and from family and parenting centres.
Implications for progressing to a main trial
In order to progress this pilot study to a full trial, we suggest a number of modifications to address specific issues. Some participants completed the measures but did not engage with the intervention. In contrast, many participants felt that completing the measures was the part of the program they found hardest to engage with and were often late in completing the measures or wearing the accelerometers. Consequently, we recommend that researchers emphasise the purpose of a ‘research study’. We needed to emphasise how the program provided a scaffold in which to structure PA but relies on the scientific assessment of PA and is not to be confused with a prescribed exercise program at a gym or exercise facility. We also needed to bring the material ‘alive’. For instance, involving the dyads in active role plays to discuss problems they may encounter in PA and strategies to overcome them, and how to speak to each other in a need supportive way or use amusing quizzes or blogs about PA.
In hindsight we were asking the mothers to structure their lives around the program not the other way around, e.g. completing measures at pre-specified time points, creating space in their schedule to be more active, and changing how they communicate with each other. Completing questionnaires, watching a workshop, or engaging with Facebook/online, may take time away from family life. We should have adapted every component of the intervention around the lifestyle of being a mother with a young child. Perhaps we could have focused on any times the mothers were currently active or communicate in a supportive way with their partner and encourage them to reflect on how that makes them feel and the barriers to increasing those behaviours.
We could have used a bottom up approach, asking mothers why they want to be more active and if they were to describe an ‘active mother’ what would this look like, what would this mean to them, and how would they achieve that. It may have been more appropriate to ask mothers to text the researcher if they have achieved PA rather than complete a survey and for the researcher to send short video modules or text tips about how to get the whole family to be more active. Potentially, we could have harnessed more social support from other dyads in the intervention. For instance, promoting the use of a ‘confession time’ chat function where parents can share their stories about using controlling language and offer suggestions about how to make the language more supportive, or where they have not struggled with their plans, and problem solve how to fit them into their lives. The Facebook groups were meant for this purpose, but we needed to start the discussion and prompt parents to share their stories. We could also ask parents to chat or share videos about how their child is developing, and how this relates to PA e.g. ‘I have found my toddler releases emotions/pent-up energy by dancing or running’. All these strategies would only be effective if we recruited more participants to the intervention and created an interactive social environment, thus we were limited in our ability to carry out the proposed strategies during the constraints of a pilot study. For example, even with role plays and a platform for discussion, this relied on mothers being actively engaged and enough participants who want to contribute. We have shown limited numbers of engagement in our Facebook groups. A full trial is thus warranted, with a greater sample size, more funding and external partners to make phone apps, videos, and the creative content such as websites and Facebook group posts more interactive and engaging.
Conclusion
To our knowledge, this trial was the first dyadic PA intervention aimed at postpartum parent couples. With new responsibilities and lifestyle changes, postpartum mothers face a unique set of barriers to PA (Connolly et al., Citation2014). Although we showed that it is possible to recruit postpartum mothers and to a large extent their spouses, collaborative planning and need supportive communication strategies had somewhat limited effects in increasing levels of PA and unexpected effects on motivation and confidence. We hope our results will inform future dyadic studies for PA promotion in couples with young children.
Supplemental Material
Download MS Word (175.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics statement
This study was approved by the ethics board at Curtin University, Western Australia, approval number HRE2017-0045-04.
Additional information
Funding
References
- Arden-Close, E., & McGrath, N. (2017). Health behaviour change interventions for couples: A systematic review. British Journal of Health Psychology, 22, 215–237. doi:https://doi.org/10.1111/bjhp.12227
- Asparouhov, T., & Muthén, B. (2010). Bayesian analysis using Mplus: Technical implementation. Mplus Technical Report. Retrieved from http://www.statmodel.com
- Baldwin, S. A., Fellingham, G. W., & Baldwin, A. S. (2016). Statistical models for multilevel skewed physical activity data in health research and behavioral medicine. Health Psychology, 35, 552–562. doi:https://doi.org/10.1037/hea0000292
- Balneaves, L. G., Van Patten, C., Truant, T. L., Kelly, M. T., Neil, S. E., & Campbell, K. L. (2014). Breast cancer survivors’ perspectives on a weight loss and physical activity lifestyle intervention. Supportive Care in Cancer, 22, 2057–2065. doi:https://doi.org/10.1007/s00520-014-2185-4
- Bartholomew, K. J., Ntoumanis, N., & Thøgersen-Ntoumani, C. (2010). The controlling interpersonal style in a coaching context: Development and initial validation of a psychometric scale. Journal of Sport and Exercise Psychology, 32, 193–216. doi:https://doi.org/10.1123/jsep.32.2.193
- Bellows-Riecken, K. H., & Rhodes, R. E. (2008). A birth of inactivity? A review of physical activity and parenthood. Preventive Medicine, 46, 99–110. doi:https://doi.org/10.1016/j.ypmed.2007.08.003
- Benyamini, Y., Ashery, L., & Shiloh, S. (2011). Involving husbands in their wives’ health behaviour: Does it work? Applied Psychology: Health and Well-Being, 3, 66–86. doi:https://doi.org/10.1111/j.1758-0854.2010.01041.x
- Berli, C., Bolger, N., Shrout, P. E., Stadler, G., & Scholz, U. (2018). Interpersonal processes of couples’ daily support for goal pursuit: The example of physical activity. Personality and Social Psychology Bulletin, 44, 332–344. doi:https://doi.org/10.1177/0146167217739264
- Brooks, S. P., & Gelman, A. (1998). General methods for monitoring convergence of iterative simulations. Journal of Computational and Graphical Statistics, 7, 434–455. doi:https://doi.org/10.1080/10618600.1998.10474787
- Burkert, S., Scholz, U., Gralla, O., Roigas, J., & Knoll, N. (2011). Dyadic planning of health-behavior change after prostatectomy: A randomized controlled planning intervention. Social Science & Medicine, 73, 783–792. doi:https://doi.org/10.1016/j.socscimed.2011.06.016
- Canadian Society for Exercise Physiology. (2002). Retrieved from https://www2.fgcu.edu/mariebcollege/RS/files/EIM_PAR_Q1.pdf
- Carr, R. M., Prestwich, A., Kwasnicka, D., Thøgersen-Ntoumani, C., Gucciardi, D. F., Quested, E., & Ntoumanis, N. (2019). Dyadic interventions to promote physical activity and reduce sedentary behaviour: Systematic review and meta-analysis. Health Psychology Review, 13, 91–109. doi:https://doi.org/10.1080/17437199.2018.1532312
- Carson, V., Adamo, K., & Rhodes, R. E. (2018). Associations of parenthood with physical activity, sedentary behavior, and sleep. American Journal of Health Behavior, 42, 80–89. doi:https://doi.org/10.5993/AJHB.42.3.8
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic.
- Connolly, C. P., Feltz, D. L., & Pivarnik, J. M. (2014). Overcoming barriers to physical activity during pregnancy and the postpartum period: The potential impact of social support. Kinesiology Review, 3, 135–148. doi:https://doi.org/10.1123/kr.2013-0009
- Depaoli, S., & Van de Schoot, R. (2017). Improving transparency and replication in Bayesian statistics: The WAMBS-checklist. Psychological Methods, 22, 240–261. doi:https://doi.org/10.1037/met0000065
- Department of Health. (2019). Australia’s physical activity and sedentary behaviour guidelines and the Australian 24-hour movement guidelines. Retrieved from http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines
- Dwyer, L. A., Bolger, N., Laurenceau, J. P., Patrick, H., Oh, A. Y., Nebeling, L. C., & Hennessy, E. (2017). Autonomous motivation and fruit/vegetable intake in parent–adolescent dyads. American Journal of Preventive Medicine, 52, 863–871. doi:https://doi.org/10.1016/j.amepre.2017.01.011
- Enders, C. K. (2010). Applied missing data analysis. New York, NY: Guilford Press.
- Esliger, D. W., Rowlands, A. V., Hurst, T. L., Catt, M., Murray, P., & Eston, R. G. (2011). Validation of the GENEA accelerometer. Medicine and Science in Sports and Exercise, 43, 1085–1093. doi:https://doi.org/10.1249/MSS.0b013e31820513be
- Evenson, K. R., Aytur, S. A., & Borodulin, K. (2009). Physical activity beliefs, barriers, and enablers among postpartum women. Journal of Women’s Health, 18, 1925–1934. doi:https://doi.org/10.1089/jwh.2008.1309
- Ferrari, R. M., Siega-Riz, A. M., Evenson, K. R., Moos, M. K., Melvin, C. L., & Herring, A. H. (2010). Provider advice about weight loss and physical activity in the postpartum period. Journal of Women’s Health, 19, 397–406. doi:https://doi.org/10.1089/jwh.2008.1332
- Fitzpatrick, J., Gareau, A., Lafontaine, M. F., & Gaudreau, P. (2016). How to use the actor-partner interdependence model (APIM) to estimate different dyadic patterns in Mplus: A step-by-step tutorial. The Quantitative Methods for Psychology, 12, 74–86. doi:https://doi.org/10.20982/tqmp.12.1.p074
- Fjeldsoe, B. S., Miller, Y. D., & Marshall, A. L. (2013). Social cognitive mediators of the effect of the MobileMums intervention on physical activity. Health Psychology, 32, 729–738. doi:https://doi.org/10.1037/a0027548
- Godin, G. (2011). The godin-shephard leisure-time physical activity questionnaire. Health & Fitness Journal of Canada, 4, 18–22. doi:https://doi.org/10.14288/hfjc.v4i1.82
- Gore, J. S., Bowman, K., Grosse, C., & Justice, L. (2016). Let’s be healthy together: Relational motivation for physical health is more effective for women. Motivation and Emotion, 40, 36–55. doi:https://doi.org/10.1007/s11031-015-9523-9
- Hagobian, T. A., Phelan, S., Gorin, A. A., Phipps, M. G., Abrams, B., & Wing, R. R. (2016). Effects of maternal lifestyle intervention during pregnancy on untreated partner weight: Results from fit for delivery study. Obesity, 24, 23–25. doi:https://doi.org/10.1002/oby.21368
- Hamilton, K., & White, K. M. (2010a). Understanding parental physical activity: Meanings, habits, and social role influence. Psychology of Sport and Exercise, 11, 275–285. doi:https://doi.org/10.1016/j.psychsport.2010.02.006
- Hamilton, K., & White, K. M. (2010b). Parental physical activity: Exploring the role of social support. American Journal of Health Behavior, 34, 573–584.
- Hancox, J. E., Ntoumanis, N., Thøgersen-Ntoumani, C., & Quested, E. (2015). Self-determination theory. In J. MiddelKamp (Ed.), Europeactive’s essentials of motivation and behaviour change for fitness, health and sport professionals (pp. 68–84). Nijmegen: Black Box Publishers.
- International Committee of Medical Journal Editors. (2020). Clinical trials. Retrieved from http://www.icmje.org/recommendations/browse/publishing-and-editorial-issues/clinical-trial-registration.html
- Jackson, S. E., Steptoe, A., & Wardle, J. (2015). The influence of partner’s behavior on health behavior change: The English longitudinal study of ageing. JAMA International Medicine, 175, 385–392. doi:https://doi.org/10.1001/jamainternmed.2014.7554
- Jackson, B., Whipp, P. R., Chua, K. P., Dimmock, J. A., & Hagger, M. S. (2013). Students’ tripartite efficacy beliefs in high school physical education: Within-and cross-domain relations with motivational processes and leisure-time physical activity. Journal of Sport and Exercise Psychology, 35, 72–84. doi:https://doi.org/10.1123/jsep.35.1.72
- Kenny, D. A., Kashy, D. A., & Cook, W. L. (2006). Dyadic data analysis. New York, NY: The Guildford Press.
- Kenny, D. A., & Ledermann, T. (2010). Detecting, measuring, and testing dyadic patterns in the actor–partner interdependence model. Journal of Family Psychology, 24, 359–366. doi:https://doi.org/10.1037/a0019651
- Kernot, J., Olds, T., Lewis, L. K., & Maher, C. (2014). Usability testing and piloting of the mums step it up program-A team-based social networking physical activity intervention for women with young children. PloS One, 9, e108842. doi:https://doi.org/10.1371/journal.pone.0108842
- Knoll, N., Hohl, D. H., Keller, J., Schuez, N., Luszczynska, A., & Burkert, S. (2017). Effects of dyadic planning on physical activity in couples: A randomized controlled trial. Health Psychology, 36, 8. doi:https://doi.org/10.1037/hea0000423
- Koestner, R., Otis, N., Powers, T. A., Pelletier, L., & Gagnon, H. (2008). Autonomous motivation, controlled motivation, and goal progress. Journal of Personality, 76, 1201–1230. doi:https://doi.org/10.1111/j.1467-6494.2008.00519.x
- Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 1–12. doi:https://doi.org/10.3389/fpsyg.2013.00863
- Leon, A. C., Davis, L. L., & Kraemer, H. C. (2011). The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research, 45, 626–629. doi:https://doi.org/10.1016/j.jpsychires.2010.10.008
- Leslie, E., Owen, N., Salmon, J., Bauman, A., Sallis, J. F., & Kai Lo, S. (1999). Insufficiently 17 active Australian college students: Perceived personal, social, and environmental 18 influences. Preventive Medicine, 28, 20–27. doi:https://doi.org/10.1006/pmed.1998.0375
- Lewis, B. A., & Ridge, D. (2005). Mothers reframing physical activity: Family oriented politicism, transgression and contested expertise in Australia. Social Science & Medicine, 60, 2295–2306. doi:https://doi.org/10.1016/j.socscimed.2004.10.011
- Lim, B. S. C., & Wang, C. K. J. (2009). Perceived autonomy support, behavioural regulations in physical education and physical activity intention. Psychology for Sport and Exercise, 10, 52–60. doi:https://doi.org/10.1016/j.psychsport.2008.06.003
- Lopes, V. P., Gabbard, C., & Rodrigues, L. P. (2013). Physical activity in adolescents: Examining influence of the best friend dyad. Journal of Adolescent Health, 52, 752–756. doi:https://doi.org/10.1016/j.jadohealth.2012.12.004
- Marques, A., Santos, T., Martins, J., Matos, M. G. D., & Valeiro, M. G. (2018). The association between physical activity and chronic diseases in European adults. European Journal of Sport Science, 18, 140–149. doi:https://doi.org/10.1080/17461391.2017.1400109
- Merom, D., Delbaere, K., Cumming, R., Voukelatos, A., Rissel, C., Van der Ploeg, H. P., & Lord, S. R. (2014). Incidental and planned exercise questionnaire for seniors: Validity and responsiveness. Medicine & Science in Sports & Exercise, 46, 947–954. doi:https://doi.org/10.1249/mss.0000000000000196
- Miller, Y. D., Trost, S. G., & Brown, W. J. (2002). Mediators of physical activity behavior change among women with young children. American Journal of Preventive Medicine, 23, 98–103. doi:https://doi.org/10.1016/S0749-3797(02)00484-1
- Milne, S., Orbell, S., & Sheeran, P. (2002). Combining motivational and volitional interventions to promote exercise participation: Protection motivation theory and implementation intentions. British Journal of Health Psychology, 7, 163–184. doi:https://doi.org/10.1348/135910702169420
- Molloy, G. J., Dixon, D., Hamer, M., & Sniehotta, F. F. (2010). Social support and regular physical activity: Does planning mediate this link? British Journal of Health Psychology, 15, 859–870. doi:https://doi.org/10.1348/135910710X490406
- Muthén, L. K., & Muthén, B. O. (1998–2018). Mplus user’s guide. Los Angeles: Muthén & Muthén.
- Muthén, L. K., & Muthén, B. O. (2002). How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling: A Multidisciplinary Journal, 9, 599–620. doi:https://doi.org/10.1207/S15328007SEM0904_8
- Muthén, B. O., Muthén, L. K., & Asparouhov, T. (2017). Regression and mediation analysis using Mplus. Los Angeles, CA: Muthén & Muthén.
- Ntoumanis, N., Ng, J. Y. Y., Prestwich, A., Quested, E., Hancox, J. E., Thogersen-Ntoumani, C., … Williams, G. C. (in press). A meta-analysis of self-determination theory-informed studies in the health domain: Effects on motivation, health behaviour, physical and psychological health. Health Psychology Review.
- Ntoumanis, N., Quested, E., Reeve, J., & Cheon, S. H. (2018). Need supportive communication: Implications for motivation in sport, exercise, and physical activity. In B. Jackson, J. A. Dimmock, & J. Compton (Eds.), Persuasion and communication in sport, exercise, and physical activity (pp. 155–169). Abingdon: Routledge.
- Olsen, M. K., & Schafer, J. L. (2001). A two-part random-effects model for semicontinuous longitudinal data. Journal of the American Statistical Association, 96, 730–745. doi:https://doi.org/10.1198/016214501753168389
- Pereira, M. A., Rifas-Shiman, S. L., Kleinman, K. P., Rich-Edwards, J. W., Peterson, K. E., & Gillman, M. W. (2007). Predictors of change in physical activity during and after pregnancy: Project viva. American Journal of Preventive Medicine, 32, 312–319. doi:https://doi.org/10.1016/j.amepre.2006.12.017
- Phongsavan, P., McLean, G., & Bauman, A. (2007). Gender differences in influences of 16 perceived environmental and psychosocial correlates on recommended level of 17 physical activity among New Zealanders. Psychology of Sport and Exercise, 8, 939–950. doi:https://doi.org/10.1016/j.psychsport.2006.11.004
- Prestwich, A., Conner, M., Lawton, R., Bailey, W., Litman, J., & Molyneaux, V. (2005). Individual and collaborative implementation intentions and the promotion of breast self-examination. Psychology & Health, 20, 743–760. doi:https://doi.org/10.1080/14768320500183335
- Prestwich, A., Conner, M. T., Lawton, R. J., Ward, J. K., Ayres, K., & McEachan, R. R. C. (2012). Randomized controlled trial of collaborative implementation intentions targeting working adults’ physical activity. Health Psychology, 31, 486–495. doi:https://doi.org/10.1037/a0027672
- Prestwich, A., Conner, M. T., Lawton, R. J., Ward, J. K., Ayres, K., & McEachan, R. R. C. (2014). Partner and planning-based interventions to reduce fat consumption: Randomized controlled trial. British Journal of Health Psychology, 19, 132–148. doi:https://doi.org/10.1111/bjhp.12047
- Prestwich, A., Lawton, R. J., & Conner, M. T. (2003). The use of implementation intentions and the decision balance sheet in promoting exercise behaviour. Psychology & Health, 18, 707–721. doi:https://doi.org/10.1080/08870440310001594493
- Prestwich, A., Perugini, M., & Hurling, R. (2009). Can the effects of implementation intentions on exercise be enhanced using text messages? Psychology & Health, 24, 677–687. doi:https://doi.org/10.1080/08870440802040715
- Prestwich, A., Perugini, M., & Hurling, R. (2010). Can implementation intentions and text messages promote brisk walking? A randomized trial. Health Psychology, 29, 40–49. doi:https://doi.org/10.1037/a0016993
- Rhodes, R. E., Blanchard, C. M., Benoit, C., Levy-Milne, R., Naylor, P. J., Downs, D. S., & Warburton, D. E. (2014). Physical activity and sedentary behavior across 12 months in cohort samples of couples without children, expecting their first child, and expecting their second child. Journal of Behavioral Medicine, 37, 533–542. doi:https://doi.org/10.1007/s10865-013-9508-7
- Ryan, R. M., & Deci, E. L. (2017). Self-determination theory: Basic psychological needs in motivation, development, and wellness. New York: Guilford Publications.
- Saligheh, M., McNamara, B., & Rooney, R. (2016). Perceived barriers and enablers of physical activity in postpartum women: A qualitative approach. BMC Pregnancy and Childbirth, 16, 131. doi:https://doi.org/10.1186/s12884-016-0908-x
- Shields, C. A., & Brawley, L. R. (2006). Preferring proxy-agency: Impact on self-efficacy for exercise. Journal of Health Psychology, 11, 904–914. doi:https://doi.org/10.1177/1359105306069092
- Spiegelhalter, D. J., Best, N. G., Carlin, B. P., & Van Der Linde, A. (2002). Bayesian measures of model complexity and fit. Journal of the Royal Statistical Society: Series B (Statistical Methodology), 64, 583–639. doi:https://doi.org/10.1111/1467-9868.00353
- Su, Y. L., & Reeve, J. (2011). A meta-analysis of the effectiveness of intervention programs designed to support autonomy. Educational Psychology Review, 23, 159–188. doi:https://doi.org/10.1007/s10648-010-9142-7
- Van Dellen, M. R., Boyd, S. M., Ranby, K. W., MacKillop, J., & Lipkus, I. (2016). Willingness to support partner’s smoking cessation: A study of partners of smokers. Journal of Health Psychology, 21, 1840–1849. doi:https://doi.org/10.1177/1359105314567209
- Van de Schoot, R., & Depaoli, S. (2014). Bayesian analyses: Where to start and what to report. The European Health Psychologist, 16, 75–84. Retrieved from http://www.ehps.net/ehp/index.php/contents/issue/view/ehp.v16.i2/showToc
- Vickers, A. J., & Altman, D. G. (2001). Analysing controlled trials with baseline and follow up measurements. BMJ, 323, 1123–1124. doi:https://doi.org/10.1136/bmj.323.7321.1123
- Williams, G. C., Grow, V. M., Freedman, Z. R., Ryan, R. M., & Deci, E. L. (1996). Motivational predictors of weight loss and weight-loss maintenance. Journal of Personality and Social Psychology, 70, 115. doi:https://doi.org/10.1037/0022-3514.70.1.115
- Zyphur, M. J., & Oswald, F. L. (2015). Bayesian estimation and inference: A user’s guide. Journal of Management, 41, 390–420. doi:https://doi.org/10.1177/2F0149206313501200
