ABSTRACT
Introduction
A healthy lifestyle could have a positive impact in reducing the incidence of some long-term sequelae secondary to pediatric cancer treatments. Motivational communication (MC) is effective at improving healthy lifestyle habits, especially when patients experience change as a challenge. To date, there is no available intervention program using MC that promotes healthy lifestyles in pediatric oncology.
Objectives
The aim of this study was to develop the first MC training program for professionals in pediatric oncology and assess its feasibility and acceptability.
Materials and methods
Following standard procedures involving professionals, we developed a professional-targeted training named the Motivation Cafés, consisting in six sessions of core MC skills for healthcare professionals who wish to positively impact lifestyles of families in pediatric oncology. We used a mixed-methods quantitative-qualitative study to assess the program feasibility and acceptability. Professionals in nutrition and physical activity (N = 16) attended two rounds of the training and completed surveys to evaluate the training. They reported self-efficacy and knowledge in MC. Participation and retention rates were used to assess acceptability and feasibility, and a thematic analysis of the open-ended questions was performed to identify strengths and weaknesses of the program to further refine the program. We used non-parametric statistics to compare pre-post changes on measures of self-efficacy and knowledge in MC.
Results
Attendance and retention (average 4.2/6 sessions completed) were high, suggesting very good adherence and feasibility. We also found high levels of acceptability and pertinence of the program (i.e. >90%). The results suggested probable improvements in self-efficacy and knowledge, but these were not statistically significant given the limited sample size.
Conclusion
The training Motivation Cafés is now ready to be pilot tested in pediatric cancer care centers.
Introduction
Medical advances afford survival rates often higher than 80% in pediatric cancer, with some highly prevalent malignancies reaching a 90% cure rate in developed countries such as Canada and the United States (Hunger et al., Citation2012; Iyer, Balsamo, Bracken, & Kadan-Lottick, Citation2015). However, these medical improvements take their toll in adulthood for most cured children who have undergone these intensive cancer treatments, resulting in significant late effects such as cardiometabolic sequelae (Bhakta et al., Citation2017; Meacham et al., Citation2010). Most common pediatric cancers are associated with increased frequency of cardiometabolic outcomes, obesity, and a deterioration in physical fitness in almost 75% of survivors (Levy et al., Citation2017). These debilitating and life-threatening conditions can occur decades after treatment (Hudson et al., Citation2013; Levy et al., Citation2017) and influence the quality of life of survivors (Brinkman et al., Citation2016).
Risk minimization in this very vulnerable population implies attending to risk factors of cardiometabolic conditions such as a sedentary lifestyle and diet. Studies have suggested the beneficial impact of nutrition and physical activity in the context of adult cancer (Demark-Wahnefried & Jones, Citation2008). Research also suggests that physical activity can benefit younger patients (i.e. pediatric and young adults) undergoing chemotherapy (Huang & Ness, Citation2011). The musculoskeletal, cardiovascular, and immune systems may be strengthened, resulting in the short- and long-term prevention or mitigation of treatment side effects (e.g. inflammation, chronic fatigue) (Soares-Miranda et al., Citation2013; Wolin, Ruiz, Tuchman, & Lucia, Citation2010). However, studies also show that pediatric and adult cancer survivors tend to be less physically active than the general population (Demark-Wahnefried & Jones, Citation2008).
In childhood cancer survivors, a better adherence to healthy dietary patterns, such as the Mediterranean diet, improves metabolic and anthropometric status (e.g. visceral and subcutaneous adiposity, waist circumference) (Tonorezos et al., Citation2013). Unfortunately, survivors often do not follow dietary recommendations with 46%–88% nonadherence to the Mediterranean diet and 51% of energy intake from highly processed food (Bérard et al., Citation2020; Robien, Ness, Klesges, Baker, & Gurney, Citation2008). Furthermore, treatments often induce a change in taste in patients, leading them to eat more fatty and salty meals, modify their appetite and alter their eating behaviors, as reported by their primary caregiver (Skolin et al., Citation2006). A healthy lifestyle in this context refer to a Mediterranean diet, exercising at least 3×/week as recommended by the Canadian health authorities, and avoiding harmful behaviors such as smoking. But these often remain difficult targets for individuals and families to achieve (Robien et al., Citation2008).
By encouraging cancer patients and their families to adopt a healthier lifestyle, it would be possible, from a preventive medicine perspective, to reduce the incidence of some long-term sequelae secondary to cancer treatments (Amireault, Fong, & Sabiston, Citation2018; Magill et al., Citation2014). As cardiometabolic processes are cumulative, change for a healthier lifestyle should occur as soon as possible during treatment or in aftercare (Hudson et al., Citation2013). To do so, both researchers and practitioners have suggested promoting motivation using specific communication techniques. Motivational interviewing (MI) is a directive and collaborative conversational style that helps to strengthen a person’s motivation and commitment to change by exploring and resolving its ambivalence (Miller & Rollnick, Citation2013). Motivational communication (MC) is a flexible, hybrid version of MI anchored in cognitive–behavioral therapy and the self-determination theory (SDT) of change (Deci & Ryan, Citation2002, Citation2012; Rouleau et al., Citation2015). The MC approach combines a series of strategies exploring ambivalence and motivation to change in patients who are trying to adopt a sustainable healthy lifestyle via behavioral modifications (Rouleau et al., Citation2015). The aim is to support patients in identifying what motivates them intrinsically, and to help them modify risky lifestyle behaviors by addressing their ambivalence towards change (Deci & Ryan, Citation2002, Citation2012). MC incorporates aspects that are not recognized as components of MI (e.g. decisional balance). The approach of MC is also strongly embedded in the three psychological needs that are the pillars of SDT: the needs for competence, social relationships, and autonomy. In MC, change is highly facilitated when the individual feels able to act in a specific environment (competence), when she/he feels connected with the interventionist (social relationships), and when he/she feels being at the origin of her/his behavior (Deci & Ryan, Citation2012; Dragomir et al., Citation2020). MC is designed to emphasize the autonomy of the patient by favoring a respectful and constructive relationship with the professional (Laurin & Lavoie, Citation2011). Importantly, MC also makes use of inputs from the Transtheoretical Model of Change that was developed in parallel with MI in order to operationalize individual status and guide target and tool selection (Freeman & Dolan, Citation2001; Miller & Rollnick, Citation2009). A good example is the staging of change: precontemplation, contemplation, preparation, action, maintenance, and relapse.
To date, MI has been studied in more than 200 randomized trials and 1000 publications across a range of disciplines and clinical settings (CMHA, Citation2017), and it is associated with favorable outcomes (Heather, Rollnick, Bell, & Richmond, Citation1996; Heckman, Egleston, & Hofmann, Citation2010; Jensen et al., Citation2011). In pediatric populations, the use of MI has helped improve dietary adherence to diabetic treatment and obesity and has decreased high-risk sexual behaviors (Berg-Smith, Stevens, Brown, & Smith, Citation1999; Channon et al., Citation2007; Knight et al., Citation2003). Motivational techniques have also been associated with improvements in substance abuse, diet, and physical activity (Lundahl et al., Citation2013). However, compared to interventions with adults, there are fewer applications of motivational techniques in pediatrics. Specifically, family interventions are still scarce due to various factors such as the developmental context of the family (e.g. parents adjusting their parenting style to match the child’s needs for independence), the systemic presentation of distress (e.g. high levels of conflict in the family, opposing views between child and parent), and the responses of families to life cycle stages (Naar-King & Suarez, Citation2011; Nock & Ferriter, Citation2005; Nock & Kazdin, Citation2005).
In cancer care, applications of motivational strategies have exclusively focused on adult populations. They have targeted physical activity, weight loss, and diet (Demark-Wahnefried & Jones, Citation2008; Spencer & Wheeler, Citation2016). In this context, studies have shown results that align with other areas of study suggesting that motivational techniques are particularly effective at improving healthy lifestyles when compared to no counseling at all, to phone calls with no MI content, to print material only, or to verbal advice (Spencer & Wheeler, Citation2016).
Training programs designed for professionals do exist (Barwick, Bennett, Johnson, McGowan, & Moore, Citation2012; Rouleau et al., Citation2015) and may rely on undergraduate interventionists (Kumar et al., Citation2017). Professionals may also receive credits in MC/MI as part of their university curriculum. Evaluation studies of these programs systematically support training effects for all MI skills, despite variations in training structure, outcome measures, and the quality of studies (Barwick et al., Citation2012). The research evaluating training programs for professionals applying motivational strategies to pediatric populations have focused on adolescent health, particularly substance abuse (Eenshuistra, Harder, & Knorth, Citation2020; Mitcheson, Bhavsar, & McCambridge, Citation2009; Seigart, Veltman, Willhaus, & Letterle, Citation2018; Vallabhan et al., Citation2017).
To date, there is no available training program in MC explicitly for health professionals working in pediatric oncology settings (i.e. with expertise in lifestyle/behavioral change). The specificity of the clinical context, the vulnerability of the population, and the need to positively influence the family as a unit, are aspects that warrant novel developments (Bass, Citation2018). New training programs are timely, aiming at promoting healthy lifestyles in pediatric oncology in order to develop new skills in clinical and research settings.
In the present project, we aimed to develop the first MC training program for professionals working in pediatric oncology. As a first objective, we wished to develop and refine a training program in MC. Based on current behavioral program development models, we wished to study the feasibility and acceptability (e.g. attendance, retention, pertinence) of the training. As a second objective, we wished to explore if the training would be related to increases in self-efficacy and knowledge of MC. These key outcomes are pertinent targets as previous studies have shown that MC training programs improved knowledge, as well as confidence and intention (i.e. self-efficacy) in using MC (Rouleau et al., Citation2015).
Method
Development of the training program
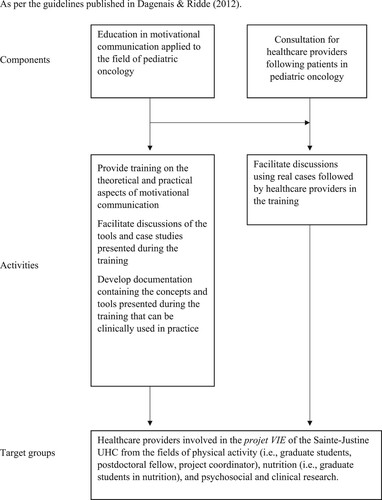
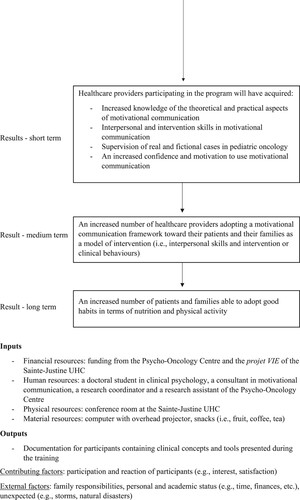
We first gathered a team of MC specialists from the CanChange network as well as researchers and clinicians in pediatric hematology-oncology from our healthcare center (Sainte-Justine UHC) in Montreal.Footnote1 To develop the first version of the program, we favored an active involvement of end-users (i.e. professionals, clinicians, healthcare providers) via regular participation of and consultation with the executive research team, in order to ensure their training needs were being met. To guide the development of the training, we followed steps suggested in the Obesity-Related Behavioral Intervention Trials (ORBIT) to define the intervention (Czajkowski et al., Citation2015). The initial phase consists of determining the elements and format of the program for adaptation to the context and further clinical relevance. Accordingly, after a thorough literature review on previous experiences of MC in pediatrics, we met with three clinicians and team leaders in nutrition and exercise counseling from our center to identify their most frequent challenges and needs when addressing lifestyle change in this context. One-on-one consultations were conducted in the Fall of 2017 with them to identify expected issues or barriers encountered during interventions with children and adolescents with cancer and their families. We explored organizational preferences regarding participation in training sessions on MC. This was done to assist in the creation of tools and to make decisions regarding the core topics to include in the training (e.g. pediatric oncology cases, role-playing showing patients’ resistance and ambivalence, supervision on existing cases). Following this phase, we chose the core topics to be included in the training (i.e. the key methods and complex skills of MC) and the format of the training (i.e. a series of short sessions focusing on active learning and practice). The research team also agreed on a logic model, presenting the interconnections between the target population, program components, intervention procedures, outcomes (short-, medium-, and long-term) and behavioral targets (). Following educational standards and to ensure reproducibility, we created a training manual for practitioners, with instructions and procedures for future program facilitators.
Figure 1. Logic model: Motivational Cafés. As per the guidelines published in Dagenais and Ridde (Citation2012).
The training is called Motivation Cafés and consists of six core MC skills training sessions for healthcare professionals and providers who wish to positively impact lifestyles of families in pediatric oncology (). The focus was set on diet and physical activity counseling as these are the most prominent themes in pediatrics. Motivation Cafés covers key-factors of motivation and commitment, stages of change, active listening, questioning, ambivalence, and an integration of acquired knowledge and competencies (Freeman & Dolan, Citation2001; Miller & Rollnick, Citation2013). The context and cases are specific to clinical aspects and challenges encountered in pediatric oncology. For example, the case of Justin, a fictitious 10-year-old boy described in Session 2, demonstrates three different stages of behavior change in terms of physical activity, when he is experiencing fatigue due to chemotherapy treatments. Each session is organized to follow a given set of activities: the theoretical content of MC, an intervention tool related to the theory presented, role-playing based on case studies, and some supervision time offered by the instructors to provide feedback targeting issues reported by participants. To ensure that all instructions and communications are consistent with MC principles, the sessions were supervised by a certified consultant in MC (CL, CanChange fellow). Her primary role was to support and enrich the training program and help supervise the participants. Participants were given access to the manual within and between sessions.
Table 1. Themes, content, tools and activities of the Motivation Cafés training program.
The Motivation Cafés training manual describes in detail the theory and intervention tools, with examples of transcripts. In addition, the transcripts of each role-play are provided. At the bottom of each transcript, we included additional questions for participants designed to self-reflect about their own clinical skills and knowledge. We also included an infographic summarizing the key intervention tools of MC (e.g. a scale of motivation or confidence to work on patient ambivalence) to be used with patients depending on their readiness for change stage (e.g. contemplation) (Freeman & Dolan, Citation2001; Miller & Rollnick, Citation2013). Copies of the manual and the infographic are available in English and in French as online supplementary material to this article.
Refinement of the training Motivation Cafés
Refining the training design consists of detailing its components, delineating its intensity, frequency and duration, and preparing the program for preliminary testing (Czajkowski et al., Citation2015). This process aims to improve the program’s strength and efficiency (i.e. best potential clinical effect on the target population with the minimum waste of resources) while ensuring that it will not harm the target population. This part focuses on the feasibility and acceptability of the program. The whole research process was approved by the local research ethics committee (ethics approval number 2017-1413), and all participants provided written consent.
Participants
We recruited a convenience sample of healthcare professionals in our center via email, during short presentations at team meetings, and via team leaders. To be included in this study, participants had to be involved in an ongoing multimodal intervention program focusing on nutrition and physical activity counseling with families who had a child being treated for cancer at our cancer care center (CHU Sainte-Justine, Citation2019). Participants also had to have direct contact with patients and families. The training intended to target professionals in nutrition and physical activity, as we used examples and cases formulations from those fields. As this part focused on refinement, we did not specify any exclusion criteria, such as previous training in MC or other related techniques.
Procedures
A sequential mixed-method design was used to evaluate the feasibility and acceptability of the training. We used self-reported questionnaires that had both open-ended questions and forced-choice questions using Likert scales. The first round of the training sessions was conducted in May and June 2018 following a schedule that met participants’ needs. The next step was to assess and refine the training by taking into consideration survey results. A second refined version of the training was then field tested in a second round with another group of participants during Fall 2018.
Measures
Demographics
We collected sociodemographic information for participants: age, sex, occupation, years of experience, education, and previous participation in MC training or related techniques.
Social validity
We used the Social Validity Questionnaire (SVQ) from Ogez et al. (Citation2019). This is a French-language version of questions developed by Kazdin (Citation2005) and Manne, Mee, Bartell, Sands, and Kashy (Citation2016) to fit the clinical context of pediatric oncology. This questionnaire was completed at the end of each session. It includes 2 items measuring the pertinence (i.e. items 1 and 3) and 3 items on acceptability (i.e. items 2, 4, and 5) of the training program: (1) ‘I find the training useful to help me in my interventions’; (2) ‘I recommend the training to another professional’; (3) ‘I find the training important/relevant for the patients I follow’; (4) ‘I learned something new from this training’; (5) ‘I find that the training has met its objectives’. The questionnaire also includes two open-ended questions requesting participants to report their evaluation of the structure and content of each session (e.g. ‘what are the strengths of the training’; ‘what are the points that need to be improved’). When appropriate, participants provided their responses on a self-report measure with seven forced choice questions about whether they agreed with statements about pertinence and acceptability (1 = totally disagree to 7 = totally agree). Items were summed into two scores: Pertinence (inter-item r = 0.62) and Acceptability (inter-item r = 0.38).
Self-efficacy
We developed a 10-item questionnaire selecting 8 items from the Self-Efficacy questionnaire-12 (SE-12; Axboe, Christensen, Kofoed, & Ammentorp, Citation2016, items #1, 2, 4, 8–12) and two self-created items to specifically address confidence and motivation. The tool was named SE-10 and closely tapped aspects being trained in the Motivation Cafés. The instrument assesses the participant’s self-described competence (self-efficacy), confidence, and motivation to use MC in his or her everyday practice. It was administered at the start of each individual session. The confidence and motivation items are rated from 1 to 10 (single item scores). Participants provided their responses about whether they felt confident and/or motivated using MC (1 = not at all confident or not at all motivated to 10 = totally confident or totally motivated): e.g. ‘In the past two weeks, how confident were you applying MC strategies to your patients’. The perceived competence or capability to use MC is composed of eight items with a total range of 8–80. Sample items include: ‘In the past two weeks, how certain are you that you have been able to: … successfully check patient’s understanding of the information given, … successfully make a plan based on shared decisions between you and the patient’, etc. Participants responded about whether they were certain concerning their competence to use MC (1 = very uncertain to 10 = totally certain) (inter-item r = 0.35). The questionnaire also includes open-ended questions to collect the experience of participants on successful/unsuccessful communication skills since the last session.
Knowledge
We used the MC Knowledge Questionnaire (MCKQ) adapted by Dr. Kim Lavoie and based on original work by Barwick et al. (Citation2012) (K. Lavoie, personal communication, April 20, 2018). Participants provided their responses on a self-report measure with 14 multiple-choice items, with total scores varying from 0 to 14, and reported as percentages, reflecting participants’ knowledge of MC. For each item, the respondent had to choose between two to six possible answers, when appropriate. A sample item is: ‘True or false? Ambivalence is especially present in the stages of contemplation and preparation’. The instrument was assigned only to the Fall participants of the second round of the program following participants’ suggestion from the first round. The instrument was administered twice, before the training (i.e. pre) and at the end of the six-session program (i.e. post) and at three and six months. No consistency coefficient is available for this count score (Streiner, Citation2003).
Analysis
We documented feasibility with participation and retention rates. We described quantitative scores of acceptability, pertinence, self-efficacy, and knowledge, and used non-parametric Wilcoxon signed rank sum and Friedman one-way repeated measure analysis tests to compare changes across time. The Cohen’s d was used to calculate effect sizes and we calculated frequencies when appropriate. To compare change across Summer/Fall training sessions, we used the Mann–Whitney U test. To further explore if changes in these outcomes would be associated with attendance, we correlated percent changes in self-efficacy and knowledge with number of sessions attended. Quantitative data were managed in IBM SPSS v24. Using the principles of thematic analysis (Braun & Clarke, Citation2012), we also identified and described themes from the written content collected in response to open-ended questions. The qualitative data were treated and coded in a Microsoft Excel 2010 spreadsheet. Emergent descriptive themes were identified and associated with corresponding quotes by reading the comments and producing a list of key elements for each theme. The coding book was built progressively and used as a reference throughout the coding and verification process. As textual answers to open-ended questions were short and simple, a systematic intercoder assessment was not necessary, and a structured summary of participants feedback was created. Qualitative themes were triangulated with observation notes from the sessions and the general appreciation of the intervention’s facilitators.
Results
We invited 23 professionals, 19 agreed to participate, but only 16 took part to the sessions (participation = 70%) and were subsequently evaluated. The participants were all active in pediatric oncology: 9 (56%) were specialists in physical activity, 4 (25%) were nutritionists, 1 (6%) was a child psychologist, 1 (6%) was a nurse and 1 (6%) was a researcher. The latter two were involved in the coordination of clinical and research activities in pediatric oncology. The participants were, on average, 28 ± 6 years old and primarily women (n = 15, 93%). Eight (50%) professionals mentioned having attended MC training in the past either formally (e.g. at a university or in a hospital), or informally (i.e. readings or tutorials). Five participated in both the Summer and Fall training sessions. Attendance for the Summer and Fall sessions was N = 14 and N = 7, respectively.
Feasibility and acceptability of the training
Participation
On average, participants attended 4.2 (±2.7) training sessions with 9 (56%) attending more than three, and 6 (37%) attending more than four sessions. Four (25%) attended all six sessions. Five participants from the first Summer round felt it was necessary to continue their training and participated in the second Fall round.
Acceptability and pertinence
Participants ended each encounter by completing the SVQ questionnaire. Overall, they considered the encounters as highly acceptable (M = 93.2%) and pertinent (M = 93%). These results were similar across both training periods with Summer/Fall mean acceptability rates of 93.2% and 93.2%, respectively, and Summer/Fall mean pertinence rates of 92.8% and 93.1%, respectively. When examining results by session, we found median scores of acceptability for individual sessions to be: S1: 90.5%, S2: 90.5%, S3: 100%, S4: 100%, S5: 100%, S6: 100%, and; pertinence to be: S1: 100%, S2: 96.5%, S3: 100%, S4: 100%, S5: 92.9%, S6: 100%, showing high homogeneity and high scores across sessions.
Strengths of the intervention. These high scores were also reflected by responses to open-ended questions. Participants appreciated the content they found clear and relevant as they perceived it offered structured intervention tools tailored to their needs (e.g. P19: ‘Examples that allow me to approach patients differently’). In fact, they reported that skills and communication tools were used between training sessions and reported them as beneficial when interacting with patients and families. In addition, belonging to a stable group throughout the six-session training favored mutual support among participants. Participants shared their clinical experiences and how they solved issues, which helped others conceptualize and plan their own interventions. They reported that one of the highlights of the training was the use of role-playing based on scenarios specific to the pediatric hematology-oncology setting. For example, P1 reported: ‘Practicing scenarios and reflecting on them allowed me to be more comfortable with the tools’. Finally, participants were particularly satisfied with the time allotted in each session to apply theoretical principles into practice. They felt this practical part provided a safe space to practice the intervention tools. For example, P1 reported: ‘I appreciated the practical aspect, because the theory seems easy to do, but it is difficult to apply’ and, P15 reported: ‘I loved the practice with the musical chair exercise … An excellent way to integrate everything’.
Issues raised. First, as scenarios were specific, participants questioned generalizability to other situations. For example, P8 reported: ‘The situations are slightly easy or rosy, so you may consider building various story options in which things do not develop as expected’. This also points to the necessity of more complex cases. Second, participants found that time management was an issue. Some found the sessions were scheduled too late after their work shift and that trainers did not respect the schedule, some sessions lasting longer than planned (sessions were planned to last one hour). Finally, participants also felt that they needed more concise material, such as a formal document synthesizing the theory and tools. For example, P10 reported: ‘It would be great to have the tools summarized and provided in paper format, so that we could take notes’.
Adjustments made to intervention. From these remarks following the Summer round, we refined the training for the Fall. First, although it was judged already excellent, we further improved transferability to practice by reinforcing the family intervention content. Although research regarding motivational approaches in family interventions is still at an early stage, we revamped the last session, initially serving as a recap session, to include family intervention tools. Second, we made sure to adhere to the schedule and set an appropriate training moment in the day (i.e. at lunch time instead of after their work shift). Third, to better support the participants, we prepared a one-page infographic summarizing the theoretical model underpinning MC and the communication tools addressed in the training (supplementary material).
Changes in self-efficacy
Here, we explored changes in self-reported competence, confidence, and motivation to use MC in the future. Scores from the SE-10 were converted in percentage for participants attending two or more sessions (n = 15). When examining differences between the scores of the first and last attended session, we observed that scores increased, on average, by 20% in competence, 11% in confidence, and 7% in motivation. Yet, none of these differences reached statistical significance (Wilcoxon p > 0.078). Changes were consistent across Summer and Fall sessions (Mann–Whitney p > 0.464). When examining correlations between self-efficacy changes and the number of sessions attended, we observed no association (r < 0.10, p > 0.731). Effect sizes for the Summer sessions were d = 0.70 (medium, Cohen, Citation2016) for perceived competence, d = 0.74 (medium) for the confidence to use MC, and d = 0.23 (small) for the motivation to use MC. We found small effect sizes for the Fall sessions, with d = 0.14, d = 0.23, and d = −0.14, respectively.
In response to open-ended questions, participants reported having used MC communication tools between training sessions, for example: questioning patients on advantages and disadvantages of change, establishing a treatment plan in collaboration with the patient, reflecting the feeling and/or the ambivalence, identifying and questioning barriers to change, and actively listening to the needs of patients. They assessed some interventions as particularly beneficial when interacting with patients and families. For example, P4 responded: ‘I explore and rephrase with the patient the advantages of change, making the patient feel capable’; P8 responded: ‘I was able to establish a relationship of trust, normalize the patient’s difficulties, and reflect on the patient’s values’; P14 responded: ‘I asked permission to make some suggestions to the patient, and I was able to establish reachable objectives’, and; P16 responded: ‘I restated the patient’s mentioned difficulties, and asked open-ended questions without directing the conversation’.
On the other side, participants reported difficulties while using some MC tools and techniques learned during the training, especially when they were dealing with adolescents or their parents. For example, P4 reported: ‘It was more difficult using MC with teens, and showing empathy when they were going with their families through more difficult times’; P15 reported: ‘MC is more challenging with teenagers’, and; P8 reported: ‘It was challenging reinforcing change-talk, establishing clear goals, and questioning parents about what they learned from the session’. Other difficulties experienced by participants were based on using the MC communication style. For example, P21 responded: ‘it’s hard not to provide information as we used to do’, and P19 responded: ‘I had trouble summarizing and focusing on the goals’.
Changes in knowledge
Scores on the MCKQ of the Fall participants tended to increase post-training with baseline/post-training/3-month/6-month follow-ups with Ms (SDs) values of 78 ± 15.7%, 84 ± 7.8%, 91 ± 3.1%, and 90 ± 3.8%. Yet, this increase did not reach statistical significance (Friedman p > 0.221). We observed no significant association when examining correlations between knowledge changes and the number of sessions attended (r < 0.89, p > 0.109).
Discussion
In line with recommendations on program development (Czajkowski et al., Citation2015), we defined and refined the design of the training Motivation Cafés, a manualized training program aimed to enhance MC competencies in healthcare professionals working in pediatric oncology. Following responses to questionnaires, supervision sessions, structured collection of feedback, we assessed the acceptability and feasibility of the program, identifying strengths and limitations, and collected future suggestions for modifications of the training sessions. Until now no training has been available in MC for professionals dealing with the clinical particularities of children, adolescents, and families in pediatric oncology. Few studies estimating the effect of a training in MI or MC in clinicians working with children and adolescents exist (Barwick et al., Citation2012). As a point of comparison, we found a randomized trial evaluating the outcome of an MI training for practitioners working in adolescent substance abuse (Mitcheson et al., Citation2009). Other studies have assessed the implementation of MI training programs in nursing students, and the training of healthcare providers and counselors in the use of MI for youth behavior change (Eenshuistra et al., Citation2020; Seigart et al., Citation2018; Vallabhan et al., Citation2017).
Acceptability and program relevance
The results highlight the acceptability and relevance of the program. First, participation was consistent through both training periods and one-third decided to follow the second round to repeat the training in order to consolidate their newly acquired skills.
Second, the structure of the training program and its components aim to improve MC competency in healthcare professionals working in pediatric oncology through a novel series of sessions combining theoretical presentations, practical exercises, intervention tools applied to typical cases in the field, and supervision for complex situations. Participants at both the Summer and Fall rounds scored high on acceptability and relevance questionnaires. This is noteworthy considering that professionals from the Fall sessions also participated in the Summer sessions, suggesting that the program did not lose its relevance or acceptability over time. Participants emphasized the relevance of presenting and demonstrating structured intervention tools tailored to their patients’ issues. The benefit of having supervision time that afforded interactions between healthcare professionals in the sharing of their experiences was also considered relevant by the participants. Participants highlighted some limitations, the major one being time management, and the fact that the training program initially did not reflect on family interventions. To address those limitations, we proceeded with modifications to improve the second round of the training, following recommendations on program refinement (Czajkowski et al., Citation2015).
When reviewing the literature on MC, we only found one study addressing program satisfaction. Like with Motivation Cafés, Seigart et al. (Citation2018) demonstrated that nursing students who attended their MI training were very satisfied with the content and simulation experiences. However, they did not find differences in terms of adolescents’ attitudes toward substance use. Given the high satisfaction response in their study, the authors underscored the importance of the implementation of MI in healthcare and the necessity to continue the evaluation of existing training programs (Seigart et al., Citation2018).
Competence in MC, confidence and motivation to use MC
Our results suggest that change was likely with regards to competence, confidence and motivation to use MC. Although results were not statistically significant, small to medium effect sizes on competence, confidence and motivation to use MC suggest changes could be detected if more participants were included. Smaller changes in the Fall round may also be because five participants already were trained in the Summer sessions (i.e. ceiling effect). In fact, when looking at their competence/motivation/confidence values, we observed that participants had higher levels than the rest of the group before training.
Similarly, evaluation of programs designed for professionals working with children or adolescents have not demonstrated statistically significant improvement in outcomes such as competencies. In a randomized trial, Mitcheson et al. (Citation2009) used the MI Treatment Integrity Version 2 (MITI Version 2) to assess practitioner competency in simulated sessions with trained actors and showed no impact upon skill levels. The authors only highlighted an effect on the MI spirit (i.e. embracing MI style and way of being). On the other hand, Eenshuistra et al. (Citation2020) revealed that counselors intervening in residential youth care adhered significantly more to MI behaviors after the training they received. The authors observed that they used fewer behaviors not adhering to MI after training. Some MI competency requirements were however not met such as the ratio of reflections made to questions asked (Eenshuistra et al., Citation2020).
Knowledge in MC
For those who were assessed on knowledge, we observed high results in knowledge on MC before starting training. Most participants, as nutritionists and physical activity professionals, had previously received a past MI training. Although not statistically significant due to a very small sample, changes from 78%, to 90% (i.e. change of +15%) in scores on the MCKQ are suggestive of improvements associated with training.
Limitations
We must recognize the limitations of this study, the first being the sample size. Although we aimed to recruit a variety of professionals, the final numbers for the Fall sessions remained limited and results are not generalizable. Given their central role in patients’ care, other professionals (such as nurses, physicians) could also be trained in the future. The content of the training Motivation Cafés is probably adapted for them but this should be confirmed. Second, although results speak in favor of feasibility and acceptability of the training, the uncontrolled design does not allow for determining the impact of the program on potential outcomes measures. It is also important to note that only a minority of participants followed all six sessions, which may question intervention fidelity. Encouraging consistent participation could call on allowing CE credits to enhance participants’ engagement. Our team is now developing an online version of the Motivation Cafés to cope with the current pandemic, and this too could increase participation. Participants had a high knowledge of MC pre-training, which draws attention to a possible selection bias, the sample holding positive views toward MC. Future research should explore whether the Motivation Cafés yields positive changes using an appropriate study design and the assessment of communication skills in participants. When studying family-level outcomes, it would of course be of major interest to collect the perception of end-users on the program. Finally, other components of a healthy lifestyle could be targeted such as smoking, drinking, and sleeping habits.
In conclusion, we developed a new training for pediatric oncology settings designed to help clinicians communicate better when trying to change health behaviors. The Motivation Cafés appears acceptable and feasible. It is a promising training program to be studied in future research. Although not conclusive, pre-post changes in motivation, self-efficacy, and knowledge, suggest that these are favorably enhanced following training. Future studies should pilot-test the present training and assess gains in competency using objective behavioral measures and control groups. Provided that these future steps are followed and successful, the Motivation Cafés could help improve patients’ health behaviors in the domains of physical activity and nutrition, which is paramount in the pediatric oncology population.
Supplemental Material
Download Zip (1.7 MB)Acknowledgements
We thank all practitioners in pediatric oncology that participated in the present study at Sainte-Justine UHC, with specific mention to Émélie Rondeau and Ariane Lacoste-Julien for their helpful comments and organizational support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available as supplementary material available online.
Additional information
Funding
Notes
1 Catherine Laurin, Daniel Sinnett, Caroline Laverdière, Valérie Marcil, Daniel Curnier, Serge Sultan.
References
- Amireault, S., Fong, A. J., & Sabiston, C. M. (2018). Promoting healthy eating and physical activity behaviors: A systematic review of multiple health behavior change interventions among cancer survivors. American Journal of Lifestyle Medicine, 12(3), 184–199. doi:https://doi.org/10.1177/1559827616661490
- Axboe, M. K., Christensen, K. S., Kofoed, P.-E., & Ammentorp, J. (2016). Development and validation of a self-efficacy questionnaire (SE-12) measuring the clinical communication skills of health care professionals. BMC Medical Education, 16(1), 272. doi:https://doi.org/10.1186/s12909-016-0798-7
- Barwick, M. A., Bennett, L. M., Johnson, S. N., McGowan, J., & Moore, J. E. (2012). Training health and mental health professionals in motivational interviewing: A systematic review. Children and Youth Services Review, 34(9), 1786–1795. doi:https://doi.org/10.1016/j.childyouth.2012.05.012
- Bass, P. F., III. (2018). When cancer strikes a family: Psychosocial issues in pediatric oncology: A child’s cancer diagnosis presents psychosocial issues that the community pediatrician needs to assess and treat for the total well-being of the child, siblings, and parents. Contemporary Pediatrics, 35(2), 12–18.
- Bérard, S., Morel, S., Teasdale, E., Shivappa, N., Hebert, J. R., Laverdière, C., … Marcil, V. (2020). Diet quality Is associated with cardiometabolic outcomes in survivors of childhood leukemia. Nutrients, 12(7), 2137.
- Berg-Smith, S. M., Stevens, V. J., Brown, K. M., & Smith, K. (1999). A brief motivational intervention to improve dietary adherence in adolescents. Health Education Research, 14(3), 399–410. doi:https://doi.org/10.1093/her/14.3.399
- Bhakta, N., Liu, Q., Ness, K. K., Baassiri, M., Eissa, H., Yeo, F., … Robison, L. L. (2017). The cumulative burden of surviving childhood cancer: An initial report from the St Jude Lifetime Cohort Study (SJLIFE). The Lancet, 390(10112), 2569–2582.
- Braun, V., & Clarke, V. (2012). Thematic analysis. In H. Cooper, P. M. Camic, D. L. Long, A. T. Panter, D. Rindskopf, & K. J. Sher (Eds.), APA handbooks in psychology®. APA handbook of research methods in psychology. Research designs: Quantitative, qualitative, neuropsychological, and biological (Vol. 2, pp. 57–71). Washington, DC: American Psychological Association. doi:https://doi.org/10.1037/13620-004
- Brinkman, T. M., Li, C., Vannatta, K., Marchak, J. G., Lai, J.-S., Prasad, P. K., … Krull, K. R. (2016). Behavioral, social, and emotional symptom comorbidities and profiles in adolescent survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 34(28), 3417–3425. doi:https://doi.org/10.1200/JCO.2016.66.4789
- Channon, S., Huws-Thomas, M. V., Rollnick, S., Hood, K., Cannings-John, R. L., Rogers, C., & Gregory, J. W. (2007). A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care, 30, 1390–1395.
- CHU Sainte-Justine. (2019, November 26). Le Projet VIE: Valorisation – Implication – Éducation. CHU Sainte-Justine. https://www.chusj.org/fr/soins-services/H/Hematologie/Projet-Vie
- CMHA. (2017, December). Motivational interviewing beginner. Workshop provided by the Canadian Mental Health Association, Ottawa Branch, Ottawa.
- Cohen, J. (2016). A power primer. In A. E. Kazdin (Ed.), Methodological issues and strategies in clinical research (4th ed., pp. 279–284). Washington, DC: American Psychological Association.
- Czajkowski, S. M., Powell, L. H., Adler, N., Naar-King, S., Reynolds, K. D., Hunter, C. M., … Charlson, M. E. (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971–982. doi:https://doi.org/10.1037/hea0000161
- Dagenais, C., & Ridde, V. (2012). Approches et pratiques en évaluation de programmes. Montreal, QC: University of Montreal Press.
- Deci, E. L., & Ryan, R. M. (2002). Handbook of self-determination research. Rochester, NY: University of Rochester Press.
- Deci, E. L., & Ryan, R. M. (2012). Self-determination theory in health care and its relations to motivational interviewing: A few comments. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 24. doi:https://doi.org/10.1186/1479-5868-9-24
- Demark-Wahnefried, W., & Jones, L. W. (2008). Promoting a healthy lifestyle among cancer survivors. Hematology/Oncology Clinics of North America, 22(2), 319–342. doi:https://doi.org/10.1016/j.hoc.2008.01.012
- Dragomir, A. I., Boucher, V. G., Bacon, S. L., Gemme, C., Szczepanik, G., Corace, K., & Lavoie, K. L. (2020). An international Delphi consensus study to define motivational communication in the context of developing a training program for physicians. Translational Behavioral Medicine, 11(2), 642–652. doi:https://doi.org/10.1093/tbm/ibaa015
- Eenshuistra, A., Harder, A. T., & Knorth, E. J. (2020). Professionalizing care workers: Outcomes of a ‘motivational interviewing’ training in residential youth care. Residential Treatment for Children & Youth. doi:https://doi.org/10.1080/0886571x.2020.1739597
- Freeman, A., & Dolan, M. (2001). Revisiting prochaska and DiClemente’s stages of change theory: An expansion and specification to aid in treatment planning and outcome evaluation. Cognitive and Behavioral Practice, 8(3), 224–234. doi:https://doi.org/10.1016/S1077-7229(01)80057-2
- Heather, N., Rollnick, S., Bell, A., & Richmond, R. (1996). Effects of brief counselling among male heavy drinkers identified on general hospital wards. Drug and Alcohol Review, 15, 29–38.
- Heckman, C., Egleston, B., & Hofmann, M. (2010). Efficacy of motivational interviewing for smoking cessation: A systematic review and meta-analysis. Tobacco Control, 19, 410–416.
- Huang, T.-T., & Ness, K. K. (2011). Exercise interventions in children with cancer: A review. International Journal of Pediatrics, 2011, 1–11.
- Hudson, M. M., Ness, K. K., Gurney, J. G., Mulrooney, D. A., Chemaitilly, W., Krull, K. R., … Robison, L. L. (2013). Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA, 309(22), 2371–2381. doi:https://doi.org/10.1001/jama.2013.6296
- Hunger, S. P., Lu, X., Devidas, M., Camitta, B. M., Gaynon, P. S., Winick, N. J., … Carroll, W. L. (2012). Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: A report from the children’s oncology group. Journal of Clinical Oncology, 30(14), 1663–1669. doi:https://doi.org/10.1200/JCO.2011.37.8018
- Iyer, N. S., Balsamo, L. M., Bracken, M. B., & Kadan-Lottick, N. S. (2015). Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: A review and meta-analysis. Blood, 126(3), 346–353. doi:https://doi.org/10.1182/blood-2015-02-627414
- Jensen, C., Cushing, C., Aylward, B., Craig, J., Sorell, D., & Steele, R. (2011). Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology, 79, 433–440.
- Kazdin, A. E. (2005). Social validity. In B. Everitt & D. Howell (Eds.), Encyclopedia of statistics in behavioral science (pp. 1512–1513). New York, NY: Wiley.
- Knight, K. M., Bundy, C., Morris, R., Higgs, J. F., Jameson, R. A., Unsworth, P., & Jayson, D. (2003). The effects of group motivational interviewing and externalizing conversations for adolescents with type-1 diabetes. Journal of Psychology, Health and Medicine, 8(2), 149–157.
- Kumar, A., Ward, K. D., Mellon, L., Gunning, M., Stynes, S., Hickey, A., … Doyle, F. (2017). Medical student INtervention to promote effective nicotine dependence and tobacco HEalthcare (MIND-THE-GAP): Single-centre feasibility randomised trial results. BMC Medical Education, 17(1), 1–13.
- Laurin, C., & Lavoie, K. L. (2011). L’entretien motivationnel et les changements de comportements en santé. Perspectives Psy, 50(3), 231–237. doi:https://doi.org/10.1051/ppsy/2011503231
- Levy, E., Samoilenko, M., Morel, S., England, J., Amre, D., Bertout, L., … Marcil, V. (2017). Cardiometabolic Risk factors in childhood, adolescent and young adult survivors of acute lymphoblastic leukemia – A petale cohort. Scientific Reports, 7(1), 17684. doi:https://doi.org/10.1038/s41598-017-17716-0
- Lundahl, B., Moleni, T., Burke, B. L., Butters, R., Tollefson, D., Butler, C., & Rollnick, S. (2013). Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling, 93(2), 157–168. doi:https://doi.org/10.1016/j.pec.2013.07.012
- Magill, M., Gaume, J., Apodaca, T., Walthers, J., Mastroleo, N., Borsari, B., & Longabaugh, R. (2014). The technical hypothesis of motivational interviewing: A meta-analysis of MI’s key causal model. Journal of Consulting and Clinical Psychology, 82, 973–983. doi:https://doi.org/10.1037/a0036833
- Manne, S., Mee, L., Bartell, A., Sands, S., & Kashy, D. A. (2016). A randomized clinical trial of a parent-focused social-cognitive processing intervention for caregivers of children undergoing hematopoetic stem cell transplantation. Journal of Consulting and Clinical Psychology, 84(5), 389–401. doi:https://doi.org/10.1037/ccp0000087
- Meacham, L. R., Chow, E. J., Ness, K. K., Kamdar, K. Y., Chen, Y., Yasui, Y., … Mertens, A. C. (2010). Cardiovascular risk factors in adult survivors of pediatric cancer – A report from the Childhood Cancer Survivor Study. Cancer Epidemiology, Biomarkers and Prevention, 19(1), 170–181.
- Miller, W. R., & Rollnick, S. (2009). Ten things that motivational interviewing is not. Behavioural and Cognitive Psychotherapy, 37, 129–140. doi:https://doi.org/10.1017/S1352465809005128
- Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). New York: Guilford Press.
- Mitcheson, L., Bhavsar, K., & McCambridge, J. (2009). Randomized trial of training and supervision in motivational interviewing with adolescent drug treatment practitioners. Journal of Substance Abuse Treatment, 37(1), 73–78. doi:https://doi.org/10.1016/j.jsat.2008.11.001
- Naar-King, S., & Suarez, M. (2011). L’Entretien Motivationnel Avec les Adolescents et les Jeunes Adultes (1ère ed.). Paris: InterEditions.
- Nock, M. K., & Ferriter, C. (2005). Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review, 8, 149–166.
- Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73, 872–879.
- Ogez, D., Bourque, C. J., Péloquin, K., Ribeiro, R., Bertout, L., Curnier, D., … Sultan, S. (2019). Definition and improvement of the concept and tools of a psychosocial intervention program for parents in pediatric oncology: A mixed-methods feasibility study conducted with parents and healthcare professionals. Pilot and Feasibility Studies, 5(1), 1–14.
- Robien, K., Ness, K. K., Klesges, L. M., Baker, K. S., & Gurney, J. G. (2008). Poor adherence to dietary guidelines among adult survivors of childhood acute lymphoblastic leukemia. Journal of Pediatric Hematology/Oncology, 30(11), 815–822. doi:https://doi.org/10.1097/MPH.0b013e31817e4ad9
- Rouleau, C. R., Lavoie, K. L., Bacon, S. L., Vallis, M., Corace, K., & Campbell, T. S. (2015). Training healthcare providers in motivational communication for promoting physical activity and exercise in cardiometabolic health settings: Do we know what we are doing? Current Cardiovascular Risk Reports, 9(29). doi:https://doi.org/10.1007/s12170-015-0457-2
- Seigart, D., Veltman, M., Willhaus, J., & Letterle, C. (2018). Implementation of motivational interviewing training in an undergraduate nursing curriculum: Identifying adolescents at risk for substance use. International Journal of Environmental Research and Public Health, 15(8), 1623. doi:https://doi.org/10.3390/ijerph15081623
- Skolin, I., Wahlin, Y. B., Broman, D. A., Koivisto Hursti, U.-K., Vikström Larsson, M., & Hernell, O. (2006). Altered food intake and taste perception in children with cancer after start of chemotherapy: Perspectives of children, parents and nurses. Supportive Care in Cancer, 14(4), 369–378. doi:https://doi.org/10.1007/s00520-005-0904-6
- Soares-Miranda, L., Fiuza-Luces, C., Lassaletta, A., Santana-Sosa, E., Padilla, J. R., Fernández- Casanova, L., … Lucia, A. (2013). Physical activity in pediatric cancer patients with solid tumors (PAPEC): Trial rationale and design. Contemporary Clinical Trials, 36(1), 106–115. doi:https://doi.org/10.1016/j.cct.2013.05.012
- Spencer, J. C., & Wheeler, S. B. (2016). A systematic review of motivational interviewing interventions in cancer patients and survivors. Patient Education and Counseling, 99(7), 1099–1105. doi:https://doi.org/10.1016/j.pec.2016.02.003
- Streiner, D. L. (2003). Starting at the beginning: An introduction to coefficient alpha and internal consistency. Journal of Personality Assessment, 80(1), 99–103. doi:https://doi.org/10.1207/S15327752JPA8001_18
- Tonorezos, E. S., Robien, K., Eshelman-Kent, D., Moskowitz, C. S., Church, T. S., Ross, R., & Oeffinger, K. C. (2013). Contribution of diet and physical activity to metabolic parameters among survivors of childhood leukemia. Cancer Causes and Control, 24(2), 313–321. doi:https://doi.org/10.1007/s10552-012-0116-6
- Vallabhan, M. K., Kong, A. S., Jimenez, E. Y., Summers, L. C., DeBlieck, C. J., & Feldstein Ewing, S. W. (2017). Training primary care providers in the use of motivational interviewing for youth behavior change. Research and Theory for Nursing Practice, 31(3), 219–232. doi:https://doi.org/10.1891/1541-6577.31.3.219
- Wolin, K. Y., Ruiz, J. R., Tuchman, H., & Lucia, A. (2010). Exercise in adult and pediatric hematological cancer survivors: An intervention review. Leukemia, 24, 1113–1120. doi:https://doi.org/10.1038/leu.2010.54. https://www.nature.com/articles/leu201054#supplementary-information