ABSTRACT
Background
Intrinsic values and priorities influence decision-making and are, therefore, important to consider explicitly in intervention development. Although health is generally considered an important value, individuals often make unhealthy choices, indicating a values disconnect.
Study aim
To investigate how becoming aware of a disconnect between the value assigned to health and the effort devoted to health is related to intentions and commitment for behavioural change and physical activity among inactive adults.
Methods
We performed a secondary exploratory analysis on previously collected data. The intervention included a values exercise based on the Disconnected Values Model (DVM) that made disconnected values explicit to participants in two study arms. We compared participants with a disconnect (n = 138) with participants without a disconnect (n = 101) regarding intentions and commitment for behavioural change and physical activity and sitting time 2–4 weeks follow-up. Logistic and linear regression analyses were performed to analyse the data.
Results
Between-group differences were found for the intention to devote more effort to health (OR = 3.75; 95%CI: 2.05; 6.86) and for the intention to become more physically active (OR = 2.21; 95%CI: 1.10; 4.46), indicating that significantly more participants with a disconnect were motivated to change, compared to participants without a disconnect. No between-group differences were found for commitment, intention strength, follow-up physical activity and sitting time.
Conclusion
Making explicit a disconnect regarding health in an active choice intervention was associated with intentions to become more physically active. Still, it did not translate in significant behaviour change at 2–4 weeks follow-up.
Trial registration
ClinicalTrials.gov: NCT04973813. Retrospectively registered.
Trial registration:
ClinicalTrials.gov identifier: NCT04973813..
Introduction
Physical inactivity is a leading risk factor for non-communicable diseases and premature mortality worldwide (World Health Organization, Citation2009). Interventions promoting physical activity usually target individual or environmental factors that are specified in behaviour change models (e.g. the Theory of Planned Behaviour (Ajzen, Citation1991) or Health Belief Model (Rosenstock, Citation1974)), including individual attitudes, self-efficacy, social norms, and perceived barriers (Kwasnicka et al., Citation2016; Landais et al., Citation2020; Michie et al., Citation2009; Rhodes et al., Citation2017). Interventions targeting these factors generally achieve small effects, especially in the long term (Howlett et al., Citation2019; McEachan et al., Citation2011). It might be relevant to take a decision-making approach to physical activity to improve long-term behavioural maintenance. Specifically, individuals could be encouraged to make more active decisions regarding their health behaviour.
In active decision-making, individuals are empowered to autonomously determine their courses of action based on a consideration of personal values (Landais et al., Citation2022a). Personal values are desirable goals that serve as guiding principles in a person’s life and are central to active decision-making (Schwartz, Citation2012; Schwartz et al., Citation2012). A focus on values activates an abstract mindset, which has been associated with increased self-control, meaning that individuals can better pursue long-term desires and suppress immediate, concrete temptations (Fujita & Han, Citation2009 Sweeney & Freitas, Citation2014;). Previous research has shown the potential of active, value-congruent decision-making and self-determination in fostering commitment to behavioural change (Brinthaupt et al., Citation2013; Cioffi & Garner, Citation1996; Deci & Ryan, Citation2000; Landais et al., Citation2022a). Moreover, value-congruent decisions promote individual autonomy (Landais et al., Citation2022a), a basic psychological need according to self-determination theory. Autonomous decisions are considered increasingly important in public health and healthcare (Douma et al., Citation2020; Elwyn et al., Citation2014) and have positively been associated with intrinsic motivation, well-being, satisfaction, and behavioural persistence (Deci & Ryan, Citation2000; Zuckerman et al., Citation1978).
The pursuit of multiple values by individuals may lead to conflicts between values (Schwartz, Citation2012). For instance, pursuing physical activity and good health may conflict social and work related values (e.g. because of time constraints) (Landais et al., Citation2022b). In Motivational Interviewing, a counselling method that aims to enhance an individual's motivation to change, the experience of conflicting values is referred to as ambivalence. Ambivalence may result from a conflict between short-term and long-term values, between individualistic and collectivistic values, or from valuing one behaviour that interferes with another valued behaviour (Wagner & Sanchez, Citation2002). It is the relative importance of multiple values in relation to each other that guides behaviour (Schwartz, Citation2012). Resolving ambivalence by supporting individuals in clarifying the relative importance of conflicting values may increase motivation to change (Wagner & Sanchez, Citation2002).
One specific model that explicitly considers the role of personal values in the physical activity domain is the Disconnected Values Model (DVM) (Anshel, Citation2008). The DVM is partly based on Motivational Interviewing and assumes that sustainable behaviour change is more likely if an individual actively identifies personal values, detects a misalignment (i.e. disconnect) between personal values and unhealthy behavioural patterns, and concludes that the disconnect can be reduced by behaving in a more value-congruent way (Anshel, Citation2008). These premises are rooted in cognitive dissonance theory, which states that people strive for internal psychological consistency and are, therefore, motivated to reduce cognitive dissonance (Festinger, Citation1957). Since perceiving a disconnect is suggested to elicit cognitive dissonance, this can motivate individuals to behave in line with their values to reduce the dissonance. Previous research in a physical activity context has shown that interventions based on the DVM effectively improved physical fitness, lipid profiles, and mental well-being (Anshel et al., Citation2010; Anshel & Kang, Citation2007; Anshel & Kang, Citation2010).
In the current study, we performed a secondary exploratory analysis on previously collected data by Landais et al. (Citation2022a) to investigate how an intervention that increases awareness of a disconnect between the value assigned to health and the actual effort devoted to healthy behaviour is related to intentions, commitment, and actual behavioural change in inactive adults. As such, it provides deeper insight into the working mechanisms behind the active choice intervention by Landais et al. (Citation2022a). Ultimately, these insights could be used to improve individuals’ intentions, commitment and behaviour change regarding physical by supporting decisions in line with people’s values. Based on the DVM, we hypothesised that, as a result of the intervention, individuals with a disconnect are more willing to devote effort to health and to become more physically active and have stronger intentions and higher commitment toward physical activity than individuals without a disconnect. In addition, we expected higher physical activity levels and less sitting time at 2–4 weeks follow-up in individuals with a disconnect.
Methods
Design and setting
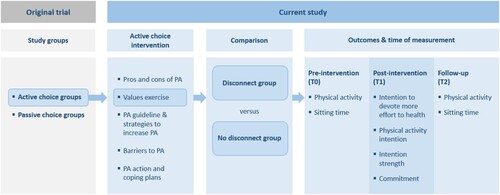
This study analysed data collected during a web-based pre-test, post-test randomised controlled trial by Landais et al. (Citation2022a) in September and October 2020 (retrospectively registered, NCT04973813). The original trial consisted of four study arms and aimed to investigate the effectiveness of promoting an active choice (two arms) versus passive choice (two arms) regarding physical activity on self-reported behavioural outcomes (e.g. physical activity behaviour) and psychological outcomes (e.g. physical activity intention; commitment). The current study used the combined data from the two study arms consisting of physically inactive participants who completed an active choice intervention, including a values exercise that made disconnected values explicit. Data from the passive choice intervention (i.e. the two other study arms of the original trial) were not used. In the current study, we compared participants with a ‘disconnect’ (n = 138; as assessed by the researchers; see ‘Study groups’) with participants without a disconnect (n = 101) on a subset of the outcomes (see ‘Outcomes’).
Before the trial intervention, participants completed the short form of the International Physical Activity Questionnaire (IPAQ) to assess baseline physical activity levels. The post-intervention questions, which assessed psychological outcomes, followed directly after the intervention. Approximately 2–4 weeks follow-up, participant completed the IPAQ short form again and some questions assessing psychological outcomes. An overview of the study design is presented in . The Medical Ethics Review Committee of VU University Medical Center confirmed that no ethical approval was required for this study (number: 2020.142).
Figure 1. Study design. Abbreviations: PA Physical activity. We included active choice group participants of the original trial in the current study. The current study focusses on the values exercise, comparing participants with a disconnect with those that had no disconnect in this exercise. Outcomes were assessed pre-intervention (T0), post-intervention (T1) and at follow-up (T2).
Participants
The trial data were collected within the ISO-certified Flycatcher Internet Research panel (www.flycatcher.eu). Panel members were Dutch adults (i.e. 18 years and over) who voluntarily signed up for research participation. Individuals were included in the trial if they reported low physical activity levels (i.e. if they were on less than five days a week physically active for 30 min or more and engaged in less than 150 min of physical activity in total throughout an average week (Scottish Physical Activity Screening Question (Scot-PASQ), Citation2013)). Individuals not able to walk a minimum of 100 metres, wheelchair users, and pregnant women were excluded from the trial. Participants in the current study were the ones from the two study arms that received an active choice intervention (Landais et al., Citation2022a).
Intervention
Participants in the current study all completed a web-based active choiceFootnote1 intervention (Additional file 1). A detailed description of the intervention, including theoretical foundations and behaviour change techniques, was outlined by Landais et al. (Citation2022a). In short, the intervention asked participants about the pros and cons of their current behaviour and increasing physical activity, comparable to a ‘decisional balance sheet’ (Janis & Mann, Citation1977), and to indicate the pros/cons considered most important. Subsequently, participants completed a values exercise (see below). Next, participants read the Dutch physical activity guideline (Gezondheidsraad. Beweegrichtlijnen, Citation2017) and strategies to increase physical activity. They were asked to report personal barriers to physical activity. Participants in one of the active choice groups of the original trial who indicated that they considered increasing their physical activity levels were additionally asked to make physical activity action and coping plans (n = 98) (Bélanger-Gravel et al., Citation2013; Gollwitzer & Sheeran, Citation2006; Sheeran et al., Citation2005).
Values exercise
The intervention’s values exercise was based on the Disconnected Values Inventory (DVI), an exercise derived from the Disconnected Values Model (Anshel, Citation2008). The DVI first asks individuals about the importance of several key values (e.g. health, family) and the effort individuals put into each of these values. In case of a disconnect, individuals are asked if they think the disconnect is acceptable, given its costs and long-term consequences. Only if the disconnect is considered unacceptable, it is expected that individuals consider committing to behaviour change (Anshel & Kang, Citation2007). Individuals with a disconnect are encouraged to develop an action plan to replace the negative habit with new routines (Anshel, Citation2008).
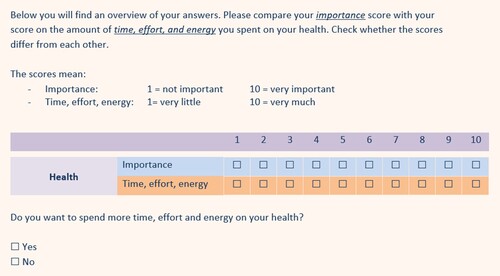
Our values exercise first asked participants to rate the importance of several values, including health, responsibility, performance (e.g. at work), pleasure, family, friendship, and balance (e.g. between work and private life), on a scale of 1 (not important) to 10 (very important). These values were chosen based on the DVI (Anshel & Kang, Citation2010) and a prior qualitative study (Landais et al., Citation2022b), in which different participants participated. Next, participants were asked to rate the time, effort, and energy they devoted to each of those values in the past year on a scale of 1 (not much) to 10 (very much). After that, we presented participants with their ratings on the two questions regarding ‘health’ (i.e. its importance and the devoted time, effort, and energy), as shown in . As such, it made disconnected values explicit to individuals. Finally, we asked whether they perceived a discrepancy between the ratings and whether they were willing to devote more time, effort, and energy to their health (yes/no). We deliberatively asked about ‘willingness’ rather than ‘acceptability’, as usual in the DVI (Anshel & Kang, Citation2010), to get participants to think about behavioural change.
Figure 2. A component of the values exercise that presented participants with their ratings for the importance of health and the time, effort, and energy devoted to health in the past year. In the values exercise, participants were presented their ratings for the importance of health and the time, effort, and energy devoted to health in the past year and asked to compare those ratings. Subsequently, they were asked whether they were willing to spend more time, effort and energy on their health.
Study groups
We compared two groups in this study: participants who completed a web-based active choice intervention with a values ‘disconnect’ and participants who completed the same intervention without a values ‘disconnect’. A disconnected values score (disconnect yes/no) was computed by subtracting participants’ ratings on ‘the time, effort, and energy – shortly ‘effort’ – devoted to health’ from ‘the importance of health’ (Anshel & Kang, Citation2010). We used a cut-off point to define a disconnect: a discrepancy of ≥2 points between the importance of health and the effort devoted to health (with the assigned importance being higher than the invested effort). This cut-off value was chosen based on mean disconnected values reported in studies using the DVI, which ranged between 2.98 (pre-test) and 1.70 (post-test) (Anshel & Kang, Citation2010; Brinthaupt et al., Citation2010). Participants had to give at least some importance to their health to be categorized as having a disconnect. Therefore, participants rating the importance of health ≤5 were excluded from analyses. We defined ‘no disconnect’ as a ≤ 1 point discrepancy between the importance of health and the effort devoted to health, including negative differences scores (i.e. the assigned importance being lower than the effort invested).
Procedure
The original trial disseminated the pre-intervention, intervention, and post-intervention questionnaires between September 4 and 22, 2020. All panel members (n = 9395) were invited by e-mail by the research agency, along with brief information about the study topic and an estimated time to complete the questionnaire and intervention (10–20 min). Five questions were used to check individuals’ eligibility, as specified in the Participants section. If eligible panel members consented to participate, they were randomised to one of four groups using the SPSS function ‘random sample of cases’ for simple random sampling. Follow-up data collection took place from September 24 to October 9, 2020.
Outcomes
Intention to devote more effort to health, physical activity intention, intention strength, commitment, physical activity behaviour and sitting time constituted the main outcome measures of the current study. Intention to devote more effort to health was assessed during the completion of the intervention (directly after the values exercise) as follows: ‘Do you want to spend more time, effort, and energy on your health?’ (yes/no). The intention to become more physically active was assessed dichotomously (yes/no). Intention strength and commitment to becoming more physically active were both assessed with one item using a 10-point scale. Physical activity intention, intention strength, and commitment were assessed directly post-intervention. Physical activity and sitting time were assessed pre-intervention and at follow-up using the short form of the International Physical Activity Questionnaire (IPAQ) (International physical activity questionnaire, Citation2012; van Poppel et al., Citation2004), which has reasonable reliability and validity (Craig et al., Citation2003). The IPAQ assesses time spent in vigorous and moderate-intensity activities and walking over the past seven days. For each of these activities, the metabolic equivalent of task (MET)-minutes per week were calculated (i.e. a measure of energy expenditure relative to being at rest) (Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and long forms, Citation2005). By summing the vigorous, moderate and walking MET-minutes/week scores, we obtained a combined total physical activity MET-minutes/week score. Total scores of <10 min were recoded ‘zero’, and scores of ≥16 h were excluded (pairwise deletion). For sitting time, which was assessed by 1 IPAQ item, we excluded cases with ≥ 20 h of daily sitting time from the analysis because such values seemed invalid. shows the assessment of the outcome measures, including the time of measurement.
Table 1. Assessment of outcome measures.
A few additional outcomes were assessed in the original trial (Landais et al., Citation2022a), including self-efficacy, values-congruence, active choice, autonomous choice, and satisfaction with the choice, since these outcomes were expected to differ between individuals who made a more active versus more passive choice. However, in the current study, we had not expectations concerning between-group differences for these outcomes; therefore, we did not analyse them in the current study.
Data analysis
All analyses of the current study were secondary exploratory analyses. A logistic regression analysis investigated the relationship between the presence of disconnect (yes/no) and physical activity intention. Linear regression analyses were performed to analyse the relationship between the presence of a disconnect (yes/no) and intention strength, commitment, physical activity and sitting time. We used the follow-up measurement as the dependent variable for physical activity and sitting time and adjusted it for the baseline measurement. Outliers in the IPAQ data were excluded from analyses (i.e. values exceeding 1.5 interquartile ranges below the 25th percentile or above the 75th percentile). Outcomes with a heavily skewed distribution were log-transformed for the regression analyses to meet the assumption of normal distribution. We reported the median and interquartile range (IQR) in that case. Only participants who completed the values exercise were included in the analyses. We examined potential effect modification of action and coping planning on intention strength, commitment, physical activity and sitting time, since only part of the participants were asked to make action and coping plans during the intervention (n = 98; 65 in the disconnect group and 33 in the no-disconnect group). Pairwise deletion was applied for missing data. All analyses were performed in SPSS for Windows version 26. We used a significance level of .05.
Sensitivity analyses
We conducted sensitivity analyses with different disconnect cut-offs to explore whether this would yield different results. The sensitivity analyses were conducted on the main outcomes: intention to devote more effort to health, physical activity intention, intention strength, commitment, and physical activity and sitting time. In the first set of sensitivity analyses, we defined a disconnect as a discrepancy of ≥1 point between the importance of health and the effort devoted to health (n = 179) and ‘no disconnect’ as a ≤ 0 points discrepancy between the importance of health and the effort devoted to health, including negative differences scores (n = 60).
In the second set of sensitivity analyses, we used a fixed cut-off instead of a relative difference to define ‘disconnect’. In these analyses, a ‘disconnect’ was a score of ≥7 on the importance of health and a score of ≤5 on the effort devoted to health (n = 49). ‘No disconnect’ was defined as ‘the importance of health and the effort devoted to health both scored ≥7’ (n = 147).
Results
Study population
Of 946 eligible panel members (see Landais et al. (Citation2022a) for a participant flow diagram), 239 individuals were included in the current study: 138 with a disconnect and 101 without a disconnect. The mean time interval between the baseline and follow-up measurement was 18 days (range: 9–33 days).
shows participants’ characteristics for the disconnect versus no disconnect group. The percentage of participants with a physical or mental health condition was relatively high in both groups (i.e. 63% in the disconnect group; 70% in the group without disconnect). Groups did not significantly differ regarding health condition, gender, age, educational level, employment status, living with children, ethnicity. However, participants with a disconnect reported significantly more barriers to physical activity (M = 3.08, SD = 1.33) than participants without a disconnect (M = 2.69, SD = 1.36).
Table 2. Characteristics of participants (n = 239, aged 18–97 years) with and without a disconnect between the importance of health and the time, effort, and energy devoted to health
shows that individuals with a disconnect considered health somewhat more important and their discrepancies were larger on all values compared to individuals without a disconnect. Only for ‘performance’, the discrepancies were negative, indicating that participants, especially those with a disconnect regarding health, rated the effort devoted to performance higher than its importance.
Table 3. The importance of several values and the time, effort, and energy devoted to them in the past year by group.
Main analyses
shows that significantly more participants with a disconnect were willing to devote more effort to their health (84.1%) than participants without a disconnect (58.4%); OR = 3.75; 95%CI: 2.05; 6.86. Concerning physical activity intention, significantly more participants with a disconnect were willing to become more physically active (88.0%) compared to participants without a disconnect (76.8%); OR = 2.21; 95%CI: 1.10; 4.46. Intention strength and commitment to become more physically active were somewhat higher in participants with a disconnect than in participants without a disconnect; however, between-group differences were not significant.
Table 4. Outcomes for participants with and without a disconnect between the importance of health and the time, effort, and energy devoted to health.
Regarding behavioural change, the IPAQ results showed that participants with a disconnect were not more physically active and did not spend less time sitting between the pre- and post-intervention measurements compared to participants without a disconnect. We found no effect modification of ‘making action and coping plans’ on intention strength, commitment, physical activity or sitting time.
Sensitivity analyses
Since we used different definitions of ‘disconnect’ and ‘no disconnect’ for the sensitivity analyses, the group compositions differed from the main analyses. Table 5 (Additional file 2) shows the results of the first sensitivity analysis. The results were largely comparable to the main analyses. However, contrary to the main analyses, we found a significantly higher intention strength for participants with a disconnect (M = 6.53, SD = 2.15) than for those without a disconnect (M = 5.69; SD = 2.44); β = 0.84; 95%CI:0.18; 1.51. Table 6 (Additional file 2) presents the outcomes of the second sensitivity analysis, using a fixed cut-off for disconnect. The results were largely comparable to the main analyses; however, there was no significant difference in physical activity intention.
Discussion
We studied how a disconnect between the value assigned to health and the actual effort devoted to healthy behaviour is related to intentions, commitment, and actual behavioural change in inactive adults, assuming that disconnects motivate behavioural change. In line with our hypothesis, a significantly higher number of individuals with a disconnect than those without a disconnect intended to devote more time, effort, and energy to health – the odds were more than three times higher in the disconnect group compared to the group without a disconnect. Moreover, the odds that individuals with a disconnect intended to become more physically active after the intervention were more than two times higher compared to individuals without a disconnect. However, contrary to expectations, no significant differences were found regarding intention strength, commitment, physical activity, and sitting time. These findings indicate that awareness of a disconnect between the value assigned to health and the effort devoted to health increases individuals’ physical activity intentions but does not translate to a significant behaviour change within 2–4 weeks.
The positive findings for intention contribute to the evidence previously collected in this field (Anshel & Kang, Citation2010; Brinthaupt et al., Citation2010). Previous DVM studies, in which disconnected values were assessed pre- and post-intervention, demonstrated that values regarding ‘health’ became significantly less disconnected and that exercise commitment and physical fitness significantly increased (Anshel & Kang, Citation2010; Brinthaupt et al., Citation2010). According to the DVM, this can be explained by the cognitive dissonance experienced by individuals who become aware of a disconnect. As people generally strive for internal psychological consistency, it is thought that people are motivated to reduce the cognitive dissonance, for instance by setting intentions to behave in line with one’s values (Festinger, Citation1957).
Behavioural changes in physical activity and sitting time within 2–4 weeks were not found, indicating the well-known intention-behaviour gap (Sheeran & Webb, Citation2016). This lack of effect may be explained by the fact that individuals with a disconnect reported more barriers to physical activity. Moreover, our findings suggest that individuals with a disconnect had different value priorities than individuals without a disconnect as they reported a different pattern of importance attached to other values. Specifically, individuals with a disconnect on health exhibited larger disconnects regarding the value assigned to performance than the group without a health disconnect. Although this was not statistically tested, this might mean that the disconnect group devoted much time, effort, and energy to performance-related activities (e.g. work), reducing the available time for physical activity (Bailis et al., Citation2011).
The lack of between-group differences in commitment is notable, considering the degree to which this concept relates to intentions and motivation, which are central in the DVM and SDT. We may have operationalised ‘commitment’ sub-optimally; to our knowledge, validated questionnaires to measure behavioural commitment are lacking to date.
Strengths and limitations
A strength of our work lies in the design of the values exercise based on the decision-making literature, the DVM, and cognitive dissonance theory and intended to make disconnected values explicit. In the exercise, we focused on deeper-held values rather than preferences and specifically provided participants with values important in decision-making about physical activity.
The main limitation of this study is the use of an arbitrary cut-off to define a disconnect between the importance of health and the effort devoted to health. The chosen cut-off may have affected the results since it determined how the groups were divided. We performed two sensitivity analyses with different cut-offs to overcome this limitation. These analyses yielded largely similar results; therefore, we can cautiously assume that the chosen cut-off for ‘disconnect’ in the main analyses did not significantly affect our findings.
We did not perform a power analysis for the current study. Consequently, group sizes may have been too small to reach significance in the analyses. Moreover, we acknowledge that we performed multiple tests, which increases the risk of a Type I error.
An additional limitation is that the IPAQ short form was used to assess behavioural outcomes. This measure may not have been the most accurate method for assessing pre–post intervention physical activity, as it is designed primarily for large scale surveillance (Limb et al., Citation2019). Moreover, previous studies comparing self-reported IPAQ data with accelerometer data showed that participants tend to over-report vigorous physical activity and underreport sitting time (Cerin et al., Citation2016; Dyrstad et al., Citation2014). Accelerometers would have obtained more reliable results; however, we used the IPAQ questionnaire for feasibility reasons.
We included participants of a broad age range in our study; individuals aged 18–97 years participated. Young adults have different physical conditions compared to older adults; therefore, it remains unclear whether making individuals aware of a values disconnect differently impacts adults of different ages. Furthermore, we included participants with and without a health condition. Most participants reported having a physical or mental health condition, which could have influenced our results since some health conditions limit the possibility to engage in physical activity.
Conclusion
In addition to the results of the original RCT (Landais et al., Citation2022a), this study provides a deeper insight into the working mechanisms behind the values exercise, a key component of the active choice intervention. In line with the DVM, our study demonstrated that awareness of a disconnect between the value assigned to health and the effort devoted to health increases individuals’ physical activity intentions. As such, it adds to the more common behaviour change interventions that usually focus on constructs such as self-efficacy and attitudes. Follow-up research using a pre-test post-test design needs to explore what is needed to increase commitment to physical activity and physical activity behaviour.
Authors’ contributions
All authors contributed to the conceptualization of the study and the development of the intervention and questionnaire. LL analysed the data and drafted the manuscript. All authors interpreted the data. JJ checked the quantitative analyses. JJ, OD, EV and DT critically reviewed and edited drafts of the manuscript. All authors approved the final manuscript.
Informed consent
All participants provided informed consent.
Ethics approval
( ) Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board/Ethics committee. See details under Methods. (X) The study received an exemption from an Institutional Review Board/Ethics committee; See details under Methods.
Supplemental Material
Download MS Word (23.8 KB)Supplemental Material
Download MS Word (87.5 KB)Acknowledgements
We thank all participants for their participation in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
Notes
1 We used the definition of active choice as proposed by Landais et al. (2022): a conscious and autonomous choice in which an individual is aware that there is a choice, actively weighs the pros and cons of choice options, considers personal values, and thinks about specific personal goals, potential barriers to achieving those goals, and ways to cope with those barriers.
References
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211.
- Anshel, M. H. (2008). The disconnected values model: Intervention strategies for exercise behavior change. Journal of Clinical Sport Psychology, 2(4), 357–380.
- Anshel, M. H., Brinthaupt, T. M., & Kang, M. (2010). The disconnected values model improves mental well-being and fitness in an employee wellness program. Behavioral Medicine, 36(4), 113–122.
- Anshel, M. H., & Kang, M. (2007). Effect of an intervention on replacing negative habits with positive routines for improving full engagement at work: A test of the disconnected values model. Consulting Psychology Journal: Practice and Research, 59(2), 110.
- Anshel, M. H., & Kang, M. (2007). An outcome-based action study on changes in fitness, blood lipids, and exercise adherence, using the disconnected values (intervention) model. Behavioral Medicine, 33(3), 85–100.
- Anshel, M. H., & Kang, M. (2010). Brinthaupt TM. A values-based approach for changing exercise and dietary habits: An action study. International Journal oF Sport and Exercise Psychology, 8(4), 413–432.
- Bailis, D. S., Thacher, T. M., Aird, N. C., & Lipschitz, L. J. (2011). Affective and behavioral traces of goal conflict with physical activity. Basic and Applied Social Psychology, 33(2), 128–144.
- Bélanger-Gravel, A., Godin, G., & Amireault, S. (2013). A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychology Review, 7(1), 23–54.
- Brinthaupt, T. M., Kang, M., & Anshel, M. H. (2010). A delivery model for overcoming psycho-behavioral barriers to exercise. Psychology of Sport and Exercise, 11(4), 259–266.
- Brinthaupt, T. M., Kang, M., & Anshel, M. H. (2013). Changes in exercise commitment following a values-based wellness program. Journal of Sport Behavior, 36(1), 3.
- Cerin, E., Cain, K. L., Oyeyemi, A. L., Owen, N., Conway, T. L., Cochrane, T., et al. (2016). Correlates of agreement between accelerometry and self-reported physical activity. Medicine & Science in Sports & Exercise, 48(6), 1075.
- Cioffi, D., & Garner, R. (1996). On doing the decision: Effects of active versus passive choice on commitment and self-perception. Personality and Social Psychology Bulletin, 22(2), 133–147.
- Craig, C. L., Marshall, A. L., Sjöström, M., Bauman, A. E., Booth, M. L., Ainsworth, B. E., et al. (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise, 35(8), 1381–1395.
- Deci, E. L., & Ryan, R. M. (2000). The" what" and" why" of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry, 11(4), 227–268.
- Douma, L. N., Uiters, E., Verweij, M. F., & Timmermans, D. R. (2020). Autonomous and informed decision-making: The case of colorectal cancer screening. PLoS One, 15(5).
- Dyrstad, S. M., Hansen, B. H., Holme, I. M., & Anderssen, S. A. (2014). Comparison of self-reported versus accelerometer-measured physical activity. Medicine & Science in Sports & Exercise, 46(1), 99–106.
- Elwyn, G., Dehlendorf, C., Epstein, R. M., Marrin, K., White, J., & Frosch, D. L. (2014). Shared decision making and motivational interviewing: Achieving patient-centered care across the spectrum of health care problems. The Annals of Family Medicine, 12(3), 270–275.
- Festinger, L. (1957). A theory of cognitive dissonance. Stanford university press.
- Fujita, K., & Han, H. A. (2009). Moving beyond deliberative control of impulses: The effect of construal levels on evaluative associations in self-control conflicts. Psychological Science, 20(7), 799–804.
- Gezondheidsraad. Beweegrichtlijnen. (2017). Den Haag: Gezondheidsraad, 2017. Contract No.: publicatienr. 2017/08.
- Gollwitzer, P. M., & Sheeran, P. (2006). Implementation intentions and goal achievement: A meta-analysis of effects and processes. Advances in Experimental Social Psychology, 38, 69–119.
- Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and long forms (2005). IPAQ Research Committee. www.ipaq.ki.se.
- Howlett, N., Trivedi, D., Troop, N. A., & Chater, A. M. (2019). Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Translational Behavioral Medicine, 9(1), 147–157.
- International physical activity questionnaire. (2012). www.ipaq.ki.se.
- Janis, I. L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment. Free press.
- Kwasnicka, D., Dombrowski, S. U., White, M., & Sniehotta, F. (2016). Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychology Review, 10(3), 277–296.
- Landais, L. L., Damman, O. C., Jelsma, J. G., Verhagen, E. A., & Timmermans, D. R. (2022a). Promoting an active choice among physically inactive adults: A randomised web-based four-arm experiment. International Journal of Behavioral Nutrition, 19(1), 1–15.
- Landais, L. L., Damman, O. C., Schoonmade, L. J., Timmermans, D. R., Verhagen, E. A., & Jelsma, J. G. (2020). Choice architecture interventions to change physical activity and sedentary behavior: A systematic review of effects on intention, behavior and health outcomes during and after intervention. International Journal of Behavioral Nutrition, 17, 1–37.
- Landais, L. L., Jelsma, J. G., Dotinga, I. R., Timmermans, D. R., Verhagen, E. A., & Damman, O. C. (2022b). Office workers' perspectives on physical activity and sedentary behaviour: A qualitative study. BMC Public Health, 22(1), 1–10.
- Limb, E. S., Ahmad, S., Cook, D. G., Kerry, S. M., Ekelund, U., Whincup, P. H., et al. (2019). Measuring change in trials of physical activity interventions: a comparison of self-report questionnaire and accelerometry within the PACE-UP trial. International Journal of Behavioral Nutrition and Physical Activity, 16(1), 1–11.
- McEachan, R. R. C., Conner, M., Taylor, N. J., & Lawton, R. J. (2011). Prospective prediction of health-related behaviours with the theory of planned behaviour: A meta-analysis. Health Psychology Review, 5(2), 97–144.
- Michie, S., Abraham, C., Whittington, C., McAteer, J., & Gupta, S. (2009). Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychology, 28(6), 690.
- Rhodes, R. E., Janssen, I., Bredin, S. S., Warburton, D. E., & Bauman, A. (2017). Physical activity: Health impact, prevalence, correlates and interventions. Psychology & Health, 32(8), 942–975.
- Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education Monographs, 2(4), 328–335.
- Schwartz, S. H. (2012). An overview of the Schwartz theory of basic values. Online readings in Psychology and Culture, 2(1), 11.
- Schwartz, S. H., Cieciuch, J., Vecchione, M., Davidov, E., Fischer, R., Beierlein, C., et al. (2012). Refining the theory of basic individual values. Journal of Personality and Social Psychology, 103(4), 663.
- Scottish Physical Activity Screening Question (Scot-PASQ). (2013). www.paha.org.uk/: NHS Health Scotland.
- Sheeran, P., Milne, S., Webb, T. L., & Gollwitzer, P. M. (2005). Implementation intentions and health behaviour.
- Sheeran, P., & Webb, T. L. (2016). The intention–behavior gap. Social and Personality Psychology Compass, 10(9), 503–518.
- Sweeney, A. M., & Freitas, A. L. (2014). Relating action to abstract goals increases physical activity reported a week later. Psychology of Sport and Exercise, 15(4), 364–373.
- van Poppel, M. N. M., Chin, A., Paw, M. J. M., & van Mechelen, W. (2004). Reproduceerbaarheid en validiteit van de Nederlandse versie van de International Physical Activity Questionnaire (IPAQ). Tijdschrift voor Gezondheidswetenschappen (TSG), 82(7), 457–462.
- Wagner, C. C., & Sanchez, F. P. (2002). The role of values in motivational interviewing. Motivational Interviewing: Preparing People for Change, 2, 284–298.
- World Health Organization. (2009). Global health risks: Mortality and burden of disease attributable to selected major risks. World Health Organization.
- Zuckerman, M., Porac, J., Lathin, D., & Deci, E. L. (1978). On the importance of self-determination for intrinsically-motivated behavior. Personality and Social Psychology Bulletin, 4(3), 443–446.
