ABSTRACT
Background:
Adolescence is the most crucial part of life. The vulnerability of adolescent mothers is even more pronounced and can affect various health aspects. While they suffer from social and emotional stresses shortly after giving birth, the long-term effect after the post-partum period of adolescent pregnancy on the mental outcomes holds prime importance. Thus, this systematic review aims to ascertain the association between adolescent pregnancy on mental health outcomes.
Methods:
The search strategy was run in June 2023 on databases including PubMed, CINAHL, Scopus, Psych Info, and Embase . Quality assessment of the studies was done using the National Institute of Health (NIH)’s National Heart, Lung and Blood Institute (NHLBI) tool for observational studies. For studies that measured similar outcomes, a meta-analysis was conducted.
Findings:
The search strategy yielded 21 results from all databases and cross-referencing. Of these, all except for one (case–control) were cross-sectional and cohort studies. The pooled analysis found a significant association between adolescent pregnancy and depression (RR 1.34; 95% CI 1.05, 1.72, 6 studies, heterogeneity: Chi2 P 0.01; I2 = 60%); however, no association was found in anxiety (RR 1.05; 95% CI 0.26, 4.14, 2 studies; heterogeneity: Chi² P = 0.0003; I2 = 93%) and suicidal ideation (RR 3.21; 95% CI 0.17, 59.33; 3 studies; heterogeneity: Chi2 P < 0.00001; I2 = 98%).
Implication:
These findings suggest that the mental health needs of adolescent mothers must be addressed and innovative and effective interventions that support and address the mental health needs of adolescent mothers are needed to improve their mental health.
Introduction
The current shift in the disease paradigm has brought mental health issues to the prime focus globally. While its consideration is integral to every population, adolescent pregnancy and its impact on overall mental health are the most pressing issues (Sedgh et al., Citation2015). In 2017, 12 million females aged 15–19 gave birth in developing countries (World Health Organization, Citation2019). Central Africa has an adolescent fertility rate of 129.5 per 1000 (Ganchimeg et al., Citation2014) compared to Australia, a developed country with a fertility rate of 9.2 per 1000 in the same year (Ganchimeg et al., Citation2014). Although significantly lower than in marginalized communities, high rates of adolescent pregnancies are prevalent, especially in larger populated countries, including the United States, indicating 57 pregnancies per 1000 15–19-year-olds (Sedgh et al., Citation2015).
Teenage pregnancy typically focuses on pregnancy between the ages of 15 and 19 due to lesser data collection and discrepancies on teenage pregnancies before the age of 15 (Xavier et al., Citation2018). Adolescent pregnancies are highly risky, with maternal and foetal welfare at risk knowing to impose adverse pregnancy complications (WHO; Khatoon et al., Citation2021). These include higher rates of preeclampsia, systemic infections, urinary infections, puerperal endometritis, preterm delivery, very low birth weight, and perinatal mortality (Azevedo et al., Citation2015). Further complications arise, past the birth of the child, showing conclusive evidence of the correlation between behaviour and health problems in the children of adolescent mothers (Lee et al., Citation2021).
Adolescent pregnancy is strongly associated with marginalization and stigmatization. The impacts of adolescent pregnancy are widely known to create socioeconomic and educational disadvantages, ultimately creating a more significant problem with intergeneration issues as an outcome (Mann et al., Citation2020). Adolescent mothers have reported struggling immensely due to stigmatization and stereotyping within society, such as higher rates of unemployment and low levels of education (Govender et al., Citation2020). Pregnancy and postpartum mental health outcomes have been evaluated as a strong area in research fields, indicating that depression in postpartum is significantly higher in adolescent mothers compared to older age groups (Govender et al., Citation2020; Vanderkruik et al., Citation2021). The resulting factors are likely to lead to increased mental health implications.
Another proposed view, regarding the possible association with poor mental health outcomes in adolescent mothers, is the stress process theory which provides a perspective on alternate confounding factors. Falci et al. suggest that the possible build-up of chronic strain among adolescent mothers may be the underlying reason for poor mental health outcomes due to low educational achievement, underemployment, and poor social circumstances, as supported by other literature (Falci et al., Citation2010). Mental health issues, particularly after a crucial phase of life, i.e. adolescent motherhood, hold great public health importance. Young mothers living with mental illness after birth are also at an increased risk of suicidal ideations and attempts, relationship dysfunction within families, and somatic illnesses (Bulloch et al., Citation2009; Van der Kooy et al., Citation2007). Conversely, this also affects the health outcomes of their children, who are at risk of developmental deficits and delinquent behaviours (Hammerton et al., Citation2015; Letourneau et al., Citation2013; Van der Kooy et al., Citation2015).
It has previously been poorly researched and defined how adolescent pregnancy impacts mental health on a more long-term scale. The most previously relevant published study on adolescent pregnancy and mental health beyond the post-partum period represented inconclusive evidence and association due to the entanglement of factors shown within the research (Xavier et al., Citation2018). Thus, this systematic review aims to synthesize more recent literature predicting adolescent pregnancy-related mental health outcomes compared to older mothers.
Materials and methods
Information sources and search strategy
This systematic review was guided by the Preferred Items for Systematic Reviews and Meta-analyses guidelines (Page et al., Citation2021). The study was exempted from the ethical review approval. Before the commencement of the review, it had been registered online on PROSPERO (CRD42022333535). The review has been conducted as per the registration, without any modifications. The databases searched included PubMed, SCOPUS, Embase, CINAHL, and PsycINFO. The search strategy was made with the help of the librarian (refer to annexure 1). Ancestry searching was also done to identify hand-searched articles which might have been omitted from the databases. It involved reviewing the reference lists of identified articles and relevant systematic reviews to ensure a thorough exploration of the available evidence and uncover additional studies that may not have been captured through traditional database searches, enhancing the inclusivity and comprehensiveness of this review (Higgins et al., Citation2023).
A research strategy for each search engine was formatted specifically to each engine to include a range of relevant literature and keep a record of the number of articles and the date searched. The key starting search terms to build the search strategy were ‘teenage pregnancy’ and ‘mental disorder’. Three reviewers (ZSL, NE, and IT) searched various search engines from the commencement of the research study, with the last consultation of databases such as PubMed, CINAHL, Scopus, Psych Info, and Embase on 14 June 2023.
Eligibility criteria
Key eligibility criteria were determined for the collection of research studies. Determining factors to include a study indicated that focused on the mental wellbeing of adolescent mothers below the age of 20. We included studies that compared mental health outcomes, among mothers who were pregnant in adolescence, with mothers who were pregnant in adulthood. Due to adolescent pregnancies being less reported in very young people (<13 years), studies comparing different adolescent age groups and not with non-adolescent groups were excluded. Similarly, studies that included adolescents and young women (10–25) and compared with older mothers (>25 years) were excluded as outcomes were not separately reported for adolescents. Studies were excluded if they reported the mental health of fathers or offspring.
Given sufficient published research indicating mental health outcomes of adolescent pregnancy during the postpartum period, studies of mental health outcomes were only recorded if indicated beyond the post-partum period of one year or more after the birth of the child. Specific mental health conditions for inclusion were, namely post-traumatic stress disorder, depression, anxiety, substance abuse, and suicide. Other factors leading to the exclusion of research were those obtaining data looking at irrelevant comparison groups, such as adolescents who had given birth but did not show custody of the child and adolescents whose pregnancy was terminated. Studies were only included if they were published or available in English. Due to the implication of the study focusing on a global scale, there was no need to have any geographical exclusion criteria as all global data were warranted. In addition, there were no restrictions for the year of publication or study design except for other systematic reviews, case reports, and case series, which were excluded.
Data collection process
Once eligibility was determined and the literature was extracted from the search engines, the exportation of the relevant literature began with the importation into Covidence as the primary screening and data extraction tool. (Covidence, Citation2022) A team of four reviewers (KAR, NE, IT, and ZL) screened the studies for possible inclusion in the systematic review. The team members performed the screening independently, where every article was to be screened by up to two reviewers from the team. Any disagreements at the title, abstract, and full-text screening were resolved by an expert from the team (ZSL). The studies, which were agreed upon by the team for their possible inclusion, then entered the final stage of data extraction, quality assessment, and data synthesis (meta-analysis). The data were extracted in duplicates by three independent reviewers (KAR, NE, and IT).
Information extracted from the studies included the name of the primary author and year of publication, study design, setting (country), and participant characteristics, including population, age, and sample size. In addition to this, mental health outcomes, which were measured along with the name of the tools, were extracted along with their numbers. Lastly, timelines were also noted (how many months after post-partum).
Risk of bias assessment
The basis of the study design for each study has been the determining factor in evaluating the risk of bias for the methodological assessment. The National Institute of Health (NIH) and National Heart, Lung, and Blood Institute (NHLBI) quality assessment tool for observational cohort and cross-sectional studies was used for observational studies (National Heart Lung and Blood Institute, Citation2013). If the study did not have ‘no’ in any of the components, the quality was marked as high. Similarly, if the study had ‘no’ in 1–2 components, the quality was marked as moderate, and if the study had ‘no’ on >2 components, the quality was marked as low.
These methodological assessors determine and eliminate this bias by analysing the cofounders and co-interventions of the study and how they were addressed. Signalling questions are asked and answered to determine bias. As a result, it can be determined whether bias is low, somewhat biased, or high bias (Sterne et al., Citation2019). Three authors (KAR, IT, and NE) evaluated each article to evaluate the risk of bias further; any discrepancies were resolved by an expert from the team (ZSL).
Synthesis of results
A quantitative synthesis using meta-analysis was performed using Review Manager version 5.4 (CitationCollaboration TC) by two research team members (KAR and ZSL). Dichotomous outcomes were pooled using a summary risk ratio (RR) along with a 95% confidence interval, and continuous outcomes were pooled using mean difference (MD) along with a 95% confidence interval. A random-effect model was used to account for statistical heterogeneity for all these measures. The statistical heterogeneity was assessed using I2 and its significance. The heterogeneity was also visually inspected on the forest plots (Hansen et al., Citation2022). A sub-group analysis was performed for outcomes, such as depression and anxiety, based on different tools used by the included studies. Due to sparse and heterogeneous mental health outcomes reported, pooled estimates were only generated for depression, anxiety, and alcohol/drug/substance misuse. All other outcomes are reported narratively in the results. In addition, the authors of two studies (Gavin et al., Citation2011; Stiffman et al., Citation1987) were contacted for data clarification. Due to the tight timeline of the current review, we decided that authors who did not reply or get back to us after 30 August 2022 would not be included to ensure the progress of the current review. Only one author clarified the outcomes, and therefore, the results from that study were pooled (Stiffman et al., Citation1987); however, we decided not to pool the outcomes from the other study (Gavin et al., Citation2011).
Results
Study selection
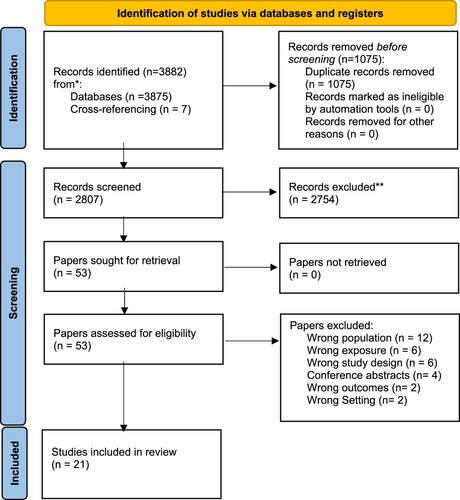
A total of 3875 records were obtained from initial hits and seven papers were obtained from cross-referencing. After removing duplicates, 2807 studies entered title and abstract screening, and 54 studies reached the full-text screening stage after removing 2754 irrelevant studies. At full-text, 32 studies were excluded with their reasons for exclusion (), 21 studies were finally included in this review, and only nine were meta-analysed.
A PRISMA flow diagram explains the process of the inclusion of the studies in the systematic review.
Study characteristics
presents the study characteristics in detail. Of the 21 studies, 12 were conducted in the United States of America (U.S.A.) (Buckingham-Howes et al., Citation2017; Deal & Holt, Citation1998; Gavin et al., Citation2011; Horwitz et al., Citation1996; Kalil & Kunz, Citation2002; Patel & Sen, Citation2012; Schmidt et al., Citation2006; Stiffman et al., Citation1987; Taylor, Citation2009; Vicary & Corneal, Citation2001; Walker & Holtfreter, Citation2016; Whitworth, Citation2017). The remaining studies were from New Zealand (Boden et al., Citation2008; Jaffee, Citation2002), Australia (Aitken et al., Citation2016), France (Iacobelli et al., Citation2014), Bangladesh (Li et al., Citation2021), South Africa (Mokwena et al., Citation2016), United Kingdom (UK) (Maughan & Lindelow, Citation1997), and Thailand (Piyasil, Citation1998). There was one multi-centric study conducted in the U.S.A. and the UK (Henretta et al., Citation2008). Except for one study which was case–control (Iacobelli et al., Citation2014), all remaining were either cross-sectional (Deal & Holt, Citation1998; Li et al., Citation2021; Mokwena et al., Citation2016; Piyasil, Citation1998; Stiffman et al., Citation1987) or cohort (Aitken et al., Citation2016; Boden et al., Citation2008; Buckingham-Howes et al., Citation2017; Gavin et al., Citation2011; Henretta et al., Citation2008; Horwitz et al., Citation1996; Jaffee, Citation2002; Kalil & Kunz, Citation2002; Maughan & Lindelow, Citation1997; Patel & Sen, Citation2012; Schmidt et al., Citation2006; Vicary & Corneal, Citation2001; Walker & Holtfreter, Citation2016; Whitworth, Citation2017). Outcome measures were assessed at varied time duration after post-partum. These included, between 1 and 5 years (Boden et al., Citation2008), 17 months (Deal & Holt, Citation1998), 18 months (Iacobelli et al., Citation2014), up to 48 months (Schmidt et al., Citation2006), at least 12 months (Aitken et al., Citation2016; Horwitz et al., Citation1996; Li et al., Citation2021; Whitworth, Citation2017), over 2 years and up to 7 years (Buckingham-Howes et al., Citation2017), up to 12 years (Vicary & Corneal, Citation2001), over 17 years (Gavin et al., Citation2011). The remaining studies did not specify the age of assessment (Henretta et al., Citation2008; Jaffee, Citation2002; Kalil & Kunz, Citation2002; Maughan & Lindelow, Citation1997; Taylor, Citation2009) or no specified time but mentioned post-partum 1 year (Mokwena et al., Citation2016; Patel & Sen, Citation2012; Piyasil, Citation1998; Stiffman et al., Citation1987; Walker & Holtfreter, Citation2016).
Table 1. Characteristics of the included studies.
Varied outcomes were reported by different studies (). The mental health outcomes reported were self-acceptance (Taylor, Citation2009), self-control (Walker & Holtfreter, Citation2016), self-esteem (Walker & Holtfreter, Citation2016), self-image (Vicary & Corneal, Citation2001), mental component summary (Aitken et al., Citation2016; Patel & Sen, Citation2012), loneliness (Vicary & Corneal, Citation2001), anxiety (Boden et al., Citation2008; Iacobelli et al., Citation2014; Mokwena et al., Citation2016; Piyasil, Citation1998; Stiffman et al., Citation1987), depression (Boden et al., Citation2008; Buckingham-Howes et al., Citation2017; Deal & Holt, Citation1998; Gavin et al., Citation2011; Henretta et al., Citation2008; Horwitz et al., Citation1996; Iacobelli et al., Citation2014; Jaffee, Citation2002; Kalil & Kunz, Citation2002; Mokwena et al., Citation2016; Piyasil, Citation1998; Schmidt et al., Citation2006; Stiffman et al., Citation1987; Taylor, Citation2009; Vicary & Corneal, Citation2001; Walker & Holtfreter, Citation2016; Whitworth, Citation2017), somatic symptoms (Mokwena et al., Citation2016), antisocial behaviours (Maughan & Lindelow, Citation1997; Mokwena et al., Citation2016), conduct disorders (Stiffman et al., Citation1987), emotional problems (Maughan & Lindelow, Citation1997), coping (Mokwena et al., Citation2016), other psychiatric disorder/comorbidity (Iacobelli et al., Citation2014; Maughan & Lindelow, Citation1997), home stress and satisfaction (Vicary & Corneal, Citation2001), conflicts (Vicary & Corneal, Citation2001), disagreement management (Vicary & Corneal, Citation2001), purpose in life (Taylor, Citation2009), suicidal ideations (Boden et al., Citation2008; Stiffman et al., Citation1987), suicidal attempts (Boden et al., Citation2008; Stiffman et al., Citation1987), suicide attempt (Boden et al., Citation2008; Iacobelli et al., Citation2014; Li et al., Citation2021), substance dependence (Boden et al., Citation2008; Stiffman et al., Citation1987), smoking (Gavin et al., Citation2011), alcohol or marijuana use (Gavin et al., Citation2011; Patel & Sen, Citation2012), and self-intoxication (Iacobelli et al., Citation2014).
Table 2. Outcomes Reported in the Included Studies.
Table 2. Continued.
Risk of bias with studies
Twenty studies were conducted either on cross-sectional or cohort studies. Of these, 11 studies were of high quality (Aitken et al., Citation2016; Boden et al., Citation2008; Gavin et al., Citation2011; Henretta et al., Citation2008; Horwitz et al., Citation1996; Jaffee, Citation2002; Kalil & Kunz, Citation2002; Maughan & Lindelow, Citation1997; Patel & Sen, Citation2012; Vanderkruik et al., Citation2001; Walker & Holtfreter, Citation2017), three were of moderate quality (Deal & Holt, Citation1998; Taylor, Citation2009; Walker & Holtfreter, Citation2016), four were of low quality (Li et al., Citation2021; Mokwena et al., Citation2016; Schmidt et al., Citation2006; Stiffman et al., Citation1987), and two studies were not assessed because they were abstract only (Buckingham-Howes et al., Citation2017; Piyasil, Citation1998). In addition, there was only one case–control study which was of low quality (Iacobelli et al., Citation2014) ().
Table 3. Quality assessment of the included studies.
Depression and anxiety
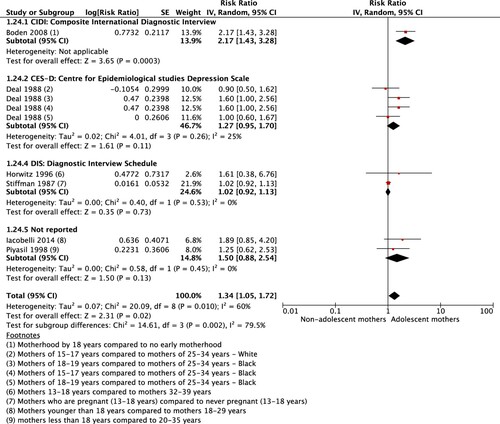
Of the 21 studies, 17 reported on depression (Boden et al., Citation2008; Buckingham-Howes et al., Citation2017; Deal & Holt, Citation1998; Gavin et al., Citation2011; Henretta et al., Citation2008; Horwitz et al., Citation1996; Iacobelli et al., Citation2014; Jaffee, Citation2002; Kalil & Kunz, Citation2002; Mokwena et al., Citation2016; Piyasil, Citation1998; Schmidt et al., Citation2006; Stiffman et al., Citation1987; Vanderkruik et al., Citation2001; Vicary & Corneal, Citation2016; Walker & Holtfreter, Citation2017) and five on anxiety (Boden et al., Citation2008; Jaffee, Citation2002; Mokwena et al., Citation2016; Piyasil, Citation1998; Stiffman et al., Citation1987). Varied kinds of scales were used for assessing depression, such as the Composite International Diagnostic Interview scale (CIDI) (Boden et al., Citation2008), Centre for Epidemiological studies Depression Scale (CES-D) (Deal & Holt, Citation1998; Henretta et al., Citation2008; Kalil & Kunz, Citation2002; Taylor, Citation2009; Vicary & Corneal, Citation2016; Walker & Holtfreter, Citation2017), Brief Symptom Inventory scale (BSI) (Gavin et al., Citation2011), Diagnostic Interview Schedule scale (DIS) (Jaffee, Citation2002; Stiffman et al., Citation1987; Vanderkruik et al., Citation2001), General Health Questionnaire (GHQ) (Mokwena et al., Citation2016), and Beck Depression Inventory (BDI) (Schmidt et al., Citation2006). Two studies did not report the scale they used to assess depression (Buckingham-Howes et al., Citation2017; Iacobelli et al., Citation2014; Piyasil, Citation1998). The pooled estimates from included studies showed depression was significantly higher among mothers who became mothers during adolescence than those who became mothers in adulthood (RR 1.34; 95% CI 1.05, 1.72, 6 studies, heterogeneity: Chi2 P 0.01, I2 60%) (). There were three studies that reported mean depression scores (Kalil & Kunz, Citation2002; Taylor, Citation2009; Walker & Holtfreter, Citation2017). The estimates showed a significantly higher depression mean score among adolescent mothers than non-adolescent mothers (MD 0.76; 95% CI 0.52, 0.99; 3 studies; heterogeneity: Chi2 P 0.27, I² 25%).
The scales used to measure anxiety were CIDI scale (Boden et al., Citation2008), DIS (Jaffee, Citation2002), and GHQ (Mokwena et al., Citation2016). The remaining two studies did not report the scale used to measure anxiety (Piyasil, Citation1998; Stiffman et al., Citation1987). The estimates showed insignificantly higher anxiety scores among adolescent mothers than non-adolescent mothers (RR 1.05; 95% CI 0.26, 4.14, 2 studies; heterogeneity: Chi2 P 0.0003, I2 93%).
Substance dependence and substance use
Two studies reported substance dependence (Boden et al., Citation2008; Stiffman et al., Citation1987). The pooled estimates showed an insignificantly higher substance dependence among adolescent mothers (RR 1.12; 95% CI 0.60, 2.10; 2 studies; heterogeneity: Chi2 P 0.22; I2 34%). Gavin et al. showed a significantly lower alcohol/marijuana use among adolescent mothers (Citation2011). The same study also reported smoking and showed significantly lower smoking among adolescent mothers than non-adolescent mothers (Gavin et al., Citation2011). Patel et al. reported mean alcohol/marijuana use among adolescent mothers. The estimates from the study showed an insignificantly lower alcohol/marijuana use among adolescent mothers than among non-adolescent mothers (Citation2012) ().
Table 4. Adolescent pregnancy and mental health outcomes.
Suicidal ideation and suicidal attempt
Two studies reported suicidal ideation (Boden et al., Citation2008; Taylor, Citation2009) and three studies reported suicidal attempts (Boden et al., Citation2008; Iacobelli et al., Citation2014; Li et al., Citation2021). The pooled estimates showed an insignificantly higher suicidal ideation among adolescent mothers than among non-adolescent mothers (RR 1.77; 95% CI 0.51, 6.14; 2 studies; heterogeneity: Chi2 P 0.0001, I2 93%). Similarly, an insignificantly higher suicidal attempt was found among adolescent mother than among non-adolescent mothers (RR 3.21; 95% CI 0.17, 59.33; 3 studies; heterogeneity: Chi2 P < 0.00001, I² 98%). One study reported self-intoxication (Iacobelli et al., Citation2014). However, the estimate showed a significantly higher self-intoxication among adolescent mothers than among non-adolescent mothers (RR 5.00; 95% CI 1.10, 22.70) ().
Other mental health outcomes
Only one study reported somatic symptoms using the GHQ scale (Mokwena et al., Citation2016). The estimates showed significantly lower somatic symptoms among adolescent mothers than among non-adolescent mothers. Two studies reported antisocial behaviour using the Rutter B-2 Scale (Maughan & Lindelow, Citation1997) and the GHQ scale (Mokwena et al., Citation2016). Maughan et al. showed a significantly higher risk of antisocial behaviour among adolescent mothers than among non-adolescent mothers (Citation1997). Stiffman et al. (Citation1987) used the Diagnostic Interview for Children and Adolescents (DICA) to assess conduct disorders. The estimates from the study showed a significantly lower conduct disorder among adolescent mothers than among non-adolescent mothers (Stiffman et al., Citation1987). Two studies reported other psychiatric disorders/morbidities (Iacobelli et al., Citation2014; Maughan & Lindelow, Citation1997). The pooled estimates from the studies showed a significantly higher psychiatric morbidity among adolescent mothers than among non-adolescent mothers.
A forest plot shows the pooled estimates from the included studies reporting depression in adolescent mothers.
Other outcomes reported in the studies were home stress and satisfaction (Vicary & Corneal, Citation2001), conflict (Vicary & Corneal, Citation2001), managing disagreements (Vicary & Corneal, Citation2001), loneliness (Vicary & Corneal, Citation2001), self-image (Vicary & Corneal, Citation2001), self-acceptance (Taylor, Citation2009), self-control (Walker & Holtfreter, Citation2016), and self-esteem (Walker & Holtfreter, Citation2016). The studies did not provide enough information to calculate the estimates. However, they narratively reported no difference in home stress and satisfaction, conflict, managing disagreements, and loneliness (Vicary & Corneal, Citation2001). Low self-esteem and self-control were significantly correlated with delinquent behaviours among adolescent mothers.
Discussion
The systematic review aimed at assessing the pregnancy-related mental health outomes in adolescent mothers compared to older mothers. Of the 21 studies, 20 were cross-sectional and cohort studies and only one study was case–control. All the studies used different scales to assess mental outcomes. However, there were fewer studies that used similar scales; thus, pooled estimates were obtained. There was significantly higher depression, insignificantly higher anxiety, and substance dependence seen among adolescent mothers compared to among non-adolescent mothers. However, mean depression scores were significantly higher in adolescent mothers. Similarly, suicidal ideation and suicidal attempts were insignificantly higher among adolescent mothers. Conversely, self-intoxication was significantly higher among adolescent mothers. Interestingly, smoking and alcohol use showed an inverse relationship with adolescent pregnancy where adolescent mothers were found to smoke less than the non-adolescent mothers.
Of all the mental health outcomes reported, depression and anxiety were the most common mental health conditions experienced by adolescents during their post-partum period. Due to the sparse heterogeneity between the studies, the estimates obtained cannot be directly applied to all adolescent mothers around the globe. There was also a discrepancy in the age categories of adolescent mothers and their comparison with young adult mothers. However, the findings suggested that adolescent pregnancy is associated with poor mental health outcomes. This set the ground for implications for research in the form of more prospective studies so that outcome ascertainment related to adolescent pregnancy can be ensured.
All the included studies were observational. Observational studies are in the middle of the hierarchy of evidence. Of the 21 included studies, 11 were of high quality, three were of moderate quality, five were of low quality, and for two studies quality was not assessed as those were abstract only. Additionally, the association between adolescent pregnancy and mental health outcomes cannot be explained as completely causal. There is a need to conduct more follow-up studies so that a cause–effect relationship can be established. However, a comprehensive search strategy was made with appropriate key terms, databases, and cross-referencing to identify relevant papers. This has resulted in reduced selection bias in this systematic review. The eligibility criteria for the possible inclusion of the studies in the review barely prevent any relevant article from getting missed to be included in the final data synthesis.
Our review showed a potential association between adolescent pregnancy and the occurrence of depression. The findings are consistent with the literature which shows that mild to moderate depressive symptoms are very much common anytime during the post-partum period among adolescent mothers ranging from 2.5% to 57% (Brown et al., Citation2012). Mutahi et al. conducted a systematic review to identify mental health problems experienced by pregnant adolescents and young mothers only in the African region (Citation2022). The qualitative analysis performed by this review identified depression being the most common mental health problem (Mutahi et al., Citation2022). Additionally, our findings add to what is already known about the unfavourable effects of early marriage and the frequent expectation of childbirth that follows after teenage pregnancy (UNFPA, Citation2013). Although reporting of other mental health conditions was limited, our findings showed that anxiety was also insignificantly associated with adolescent pregnancy. A recent review showed a 15–20% of the prevalence of anxiety among mothers during antenatal care, with the rates highest from LMICs (Dennis et al., Citation2017; Fawcett et al., Citation2019; Fisher et al., Citation2012). It is important to note that anxiety is significantly associated with post-partum depression, prematurity, preterm births, and reduced breastfeeding attitude among mothers (Grigoriadis et al., Citation2019; Staneva et al., Citation2015). The adolescent population undergoes many unique combinations of changes; this is also accompanied by life stressors such as those experienced in schools, unplanned pregnancies, societal roles, relationship dynamics, and the transition towards adulthood. All these factors put teenage at higher risk of experiencing mental health issues, and this risk is further amplified during pregnancy (Reid & Meadows-Oliver, Citation2007). All these experiences can hinder access to available healthcare services because of financial dependence, associated stigma with teenage pregnancy, and poor relationship dynamics with parents or partners (Jorns-Presentati et al., Citation2021).
The literature highlights developmental and socio-emotional interplay in parenting adolescence that contributes to the higher prevalence of depression and anxiety. Parenting adolescents involves identity formation, autonomy struggles, peer relationships, academic pressures, and challenges posed by technology and social media; communication difficulties, risk-taking behaviours, and mood swings add complexities (Shifflet-Chila et al., Citation2016). The transition to adulthood and societal expectations contributes to stress for adolescents (Kim & Kim, Citation2020). Recognizing these stressors within the developmental and socio-emotional context is vital for fostering positive mental health outcomes.
Our review also showed that adolescent mothers were more likely to present with suicidal ideation and suicidal attempts. Regardless of being pregnanct, suicidal ideations and suicidal attempts are a huge concern for adolescent population. There are evidence that shows risk of suicide considerably higher amongst teenage mothers as compared to other mothers (Huang et al., Citation2012). These findings are consistent with a systematic review conducted in 2020 assessed the association between perinatal depression with increased risk of depression among offspring during adolescence and young adulthood period. The findings highlighted a 70% increase in the odds of offspring depression in adolescents whose mothers had perinatal depression (Tirumalaraju et al., Citation2020). Another qualitative study in Kenya identified that adolescent pregnancy presents with increased suicidal behaviour because of lack of familial support during crucial pregnancy years, intimate partner violence, social isolation and stigmatization from society for getting pregnant at an early age, and chronic physical illnesses (Musyimi et al., Citation2020).
Our review included most of the studies from developed regions (U.S.A., New Zealand, and France), which may affect the health-seeking behaviours of the adolescent population. In the U.S.A., the age of consent starts from 16 years of age. Given the higher prevalence of teenage pregnancy in the U.S.A., the state has allowed teenage mothers to continue their education in the same school, and they have the right to take time off from school for prenatal visits, childbirth, abortion care, or other health reasons (TACAdmin, Citation2021). The laws in New Zealand (Pregnancy Rights Your Legal Options during and after Pregnancy, Citation2021) are also similar. These laws play a pivotal role in increasing the access of adolescent mothers to healthcare services, leading to better pregnancy outcomes as a whole.
It is essential to discuss that discrepancy in age categories between adolescent mothers and young adult mothers might impact pregnancy-related mental health outcomes. Adolescent mothers may confront increased stress, anxiety, and concerns related to social stigma and identity due to their younger age (Hodgkinson et al., Citation2014). In addition, adolescents may encounter higher levels of societal stigma and judgement about their age and pregnancy, potentially contributing to mental health challenges (Mutahi et al., Citation2022). Furthermore, adolescents may have limited autonomy in decision-making, potentially contributing to feelings of powerlessness during pregnancy (Mweteni et al., Citation2021). On the contrary, young adult mothers may exhibit more developed coping mechanisms and psychological resilience, potentially fostering a more positive mental health outlook during pregnancy (Alves et al., Citation2023). In addition, young adult mothers may face comparatively less societal judgement, positively influencing their mental well-being during pregnancy (Bedaso et al., Citation2021). Also, young adult mothers may have greater autonomy and decision-making power, positively impacting their sense of control and agency (Acharya et al., Citation2010).
There are several strengths and limitations of the study. For this review, a comprehensive search strategy was used for all the databases and thus, the likelihood of missing any relevant study is near minimal. The selection criteria for this review were stringent and detailed. The level of evidence coming from these studies was low given that the majority of studies were cross-sectional. The observational studies, particularly cross-sectional studies, would only provide a snapshot of the exposure and the outcome, making it hard to assess the causal relationship between adolescent pregnancy and mental health outcomes. The majority of the studies provided diverse mental health outcomes. Given the sparse and heterogeneous reporting of the outcomes, a meta-analysis could only be performed with fewer outcomes such as depression, mean depression scores, anxiety, suicidal ideation, and suicidal attempts. There was also a variability seen in the kind of scales used, resulting in more heterogenous, pooled estimates with increased statistical heterogeneity i.e. I2%. To account for this, a sub-group analysis was performed based on different scales used by the studies for the same outcomes. It can be noted that the majority of the studies were conducted among adolescents living in developed countries. There were no studies that were from developing, low-and-middle-income countries (LMICs), resulting in limited to no generalizability in these settings. These are the countries with higher adolescent pregnancy rates; (World Health Organization, Citation2019) thus, this review cannot be transferred to adolescent mothers living in LMICs. This highlighted a big research gap from LMICs and warrants studies to assess the pregnancy-related mental health outcomes in adolescent mothers living in developing and underdeveloped parts of the world. The limitation of the review itself was the restriction to only take articles that are published in the English language.
Conclusion
The findings from this systematic review have opened new doors for the practices and policies. The associations identified through the meta-analysis were significant enough to make direct applications in practice. This might be due to substantial heterogeneity in the methodology and the statistics. There is a need to consider age before predicting mental health in general practice. To mitigate any mental health illnesses for adolescent mothers, it is important to make mental health screening integral in antenatal care right from the beginning, and keeping follow-ups to assess any mental stressors soon after delivery and 1-year after the post-partum period. This will help achieve Goal 3 of the Sustainable Development Goal (SDGs) which aims to ‘ensure healthy lives and promote well-being for all at all ages’. In addition, adolescent pregnant mothers being at increased risk of mental illnesses must be tailored with unique interventions such as counselling and social groups interventions. Thus, effectiveness studies to reducing mental illnesses among adolescent mothers must be explored. Lastly, there is a need to link health services across varied sectors including education and social protection programmes for the adolescent and young adults along with their caregivers.
Open Scholarship

This article has earned the Center for Open Science badge for Open Materials. The materials are openly accessible at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022333535.
Supplemental Material
Download MS Word (14.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data used from primary studies asre within the manuscript.
Ethics statement
Institutional Review Board Statement: Not applicable.
Additional information
Funding
References
- Acharya, D. R., Bell, J. S., Simkhada, P., Van Teijlingen, E. R., & Regmi, P. R. (2010). Women’s autonomy in household decision-making: A demographic study in Nepal. Reproductive Health, 7(1), 1–12. https://doi.org/10.1186/1742-4755-7-15/TABLES/3
- Aitken, Z., Hewitt, B., Keogh, L., LaMontagne, A. D., Bentley, R., & Kavanagh, A. M. (2016). Young maternal age at first birth and mental health later in life: Does the association vary by birth cohort? Social Science & Medicine, 157, 9–17. https://doi.org/10.1016/J.SOCSCIMED.2016.03.037
- Alves, A. C., Souza, R. T., Mayrink, J., Galvao, R.B., Costa, M.L., Feitosa, F.E., Rocha Filho, E.A., Leite, D.F., Tedesco, R.P., Santana, D.S. and Fernandes, K.G. (2023). Measuring resilience and stress during pregnancy and its relation to vulnerability and pregnancy outcomes in a nulliparous cohort study. BMC Pregnancy and Childbirth, 23(1), 1–15. https://doi.org/10.1186/S12884-023-05692-5/TABLES/6
- Azevedo, W. e. d., Diniz, M. a., Fonseca, E. é. V., Azevedo, L. i. d., & Evangelista, C. r. (2015). Complications in adolescent pregnancy: Systematic review of the literature. Einstein, 13(4), 618–626. https://doi.org/10.1590/S1679-45082015RW3127
- Bedaso, A., Adams, J., Peng, W., & Sibbritt, D. (2021). The relationship between social support and mental health problems during pregnancy: A systematic review and meta-analysis. Reproductive Health, 18(1), 1–23. https://doi.org/10.1186/S12978-021-01209-5
- Boden, J. M., Fergusson, D. M., & John Horwood, L. (2008). Early motherhood and subsequent life outcomes. Journal of Child Psychology and Psychiatry, 49(2), 151–160. https://doi.org/10.1111/J.1469-7610.2007.01830.X
- Brown, J. D., Harris, S. K., Woods, E. R., Buman, M. P., & Cox, J. E. (2012). Longitudinal study of depressive symptoms and social support in adolescent mothers. Maternal and Child Health Journal, 16(4), 894–901. https://doi.org/10.1007/S10995-011-0814-9
- Buckingham-Howes, S., Wang, Y., Oberlander, S. E., & Black, M. M. (2017). Early maternal depressive symptom trajectories: Associations with 7-year maternal depressive symptoms and child behavior. Journal of Family Psychology, 31(4), 387–397. https://doi.org/10.1037/fam0000242
- Bulloch, A. G., Williams, J. V., Lavorato, D. H., & Patten, S. B. (2009). The relationship between major depression and marital disruption is bidirectional. Depression and Anxiety, 26(12), 1172–1177. https://doi.org/10.1002/DA.20618
- Collaboration TC. Review Manager version 5.0. revman.cochrane.org
- Covidence. Covidence - Better systematic review management. Retrieved March 11, 2022, from https://www.covidence.org/
- Deal, L. W., & Holt, V. L. (1998). Young maternal age and depressive symptoms: Results from the 1988 National Maternal and Infant Health Survey. American Journal of Public Health, 88(2), 266–270. https://doi.org/10.2105/AJPH.88.2.266
- Dennis, C. L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. British Journal of Psychiatry, 210(5), 315–323. https://doi.org/10.1192/BJP.BP.116.187179
- Falci, C. D., Mortimer, J. T., & Noel, H. J. (2010). Parental timing and depressive symptoms in early adulthood. Advances in Life Course Research, 15(1), 1–10. https://doi.org/10.1016/J.ALCR.2010.05.001
- Fawcett, E. J., Fairbrother, N., Cox, M. L., White, I. R., & Fawcett, J. M. (2019). The prevalence of anxiety disorders during pregnancy and the postpartum period: A multivariate Bayesian meta-analysis. The Journal of Clinical Psychiatry, 80(4). https://doi.org/10.4088/JCP.18R12527
- Fisher, J., de Mello, M. C., Patel, V., Rahman, A., Tran, T., Holton, S., & Holmes, W. (2012). Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bulletin of the World Health Organization, 90(2), 139–149. https://doi.org/10.2471/BLT.11.091850
- Ganchimeg, T., Ota, E., Morisaki, N., Laopaiboon, M., Lumbiganon, P., Zhang, J., Yamdamsuren, B., Temmerman, M., Say, L., Tunçalp, Ö, Vogel, J. P., Souza, J. P., & Mori, R. (2014). Pregnancy and childbirth outcomes among adolescent mothers: A World Health Organization multicountry study. BJOG: An International Journal of Obstetrics & Gynaecology, 121(Suppl. 1), 40–48. https://doi.org/10.1111/1471-0528.12630
- Gavin, A. R., Lindhorst, T., & Lohr, M. J. (2011). Adolescent mothers : Results from a 17-year longitudinal study. Women Health, 51(6), 525–545. https://doi.org/10.1080/03630242.2011.606355
- Govender, D., Naidoo, S., & Taylor, M. (2020). “I have to provide for another life emotionally, physically and financially”: Understanding pregnancy, motherhood and the future aspirations of adolescent mothers in KwaZulu-Natal South, Africa. BMC Pregnancy and Childbirth, 20(1), 1–21. https://doi.org/10.1186/S12884-020-03319-7/TABLES/2
- Grigoriadis, S., Graves, L., Peer, M., Mamisashvili, L., Tomlinson, G., Vigod, S. N., Dennis, C.-L., Steiner, M., Brown, C., Cheung, A., Dawson, H., Rector, N. A., Guenette, M., & Richter, M. (2019). A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Archives of Women's Mental Health, 22(5), 543–556. https://doi.org/10.1007/S00737-018-0930-2
- Hammerton, G., Mahedy, L., Mars, B., Harold, G. T., Thapar, A., Zammit, S., & Collishaw, S. (2015). Association between maternal depression symptoms across the first eleven years of their child’s life and subsequent offspring suicidal ideation. PLoS ONE, 10(7), e0131885. https://doi.org/10.1371/JOURNAL.PONE.0131885
- Hansen, C., Steinmetz, H., & Block, J. (2022). How to conduct a meta-analysis in eight steps: A practical guide. Management Review Quarterly, 72(1), 1–19. https://doi.org/10.1007/S11301-021-00247-4/TABLES/1
- Henretta, J. C., Grundy, E. M. D., Okell, L. C., & Wadsworth, M. E. J. (2008). Early motherhood and mental health in midlife: A study of British and American cohorts. Aging & Mental Health, 12(5), 605–614. https://doi.org/10.1080/13607860802343084
- Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (Eds.). (2023). Cochrane handbook for systematic reviews of interventions version 6.4 (2nd ed.). John Wiley & Sons.
- Hodgkinson, S., Beers, L., Southammakosane, C., & Lewin, A. (2014). Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics, 133(1), 114–122. https://doi.org/10.1542/PEDS.2013-0927
- Horwitz, S. M., Livingston, M., Hoff, R. A., Harley, I., & Jekel, J. F. (1996). Depression in former school-age mothers and community comparison subjects. Journal of Affective Disorders, 40, 95–103. https://doi.org/10.1016/0165-0327(96)00047-X
- Huang, H., Faisal-Cury, A., Chan, Y.-F., Tabb, K., & Wayne Katon, P. R. M. (2012). Suicidal ideation during pregnancy: Prevalence and associated factors among low-income women in São Paulo, Brazil. Archives of Women's Mental Health, 15(2), 135–138. https://doi.org/10.1007/s00737-012-0263-5
- Iacobelli, S., Robillard, P. Y., Gouyon, J. B., Nichols, M., Boukerrou, M., Barau, G., & Bonsante, F. (2014). Longitudinal health outcome and wellbeing of mother-infant pairs after adolescent pregnancy in Reunion Island, Indian Ocean. International Journal of Gynecology & Obstetrics, 125(1), 44–48. https://doi.org/10.1016/j.ijgo.2013.09.029
- Jaffee, S. R. (2002). Pathways to adversity in young adulthood among early childbearers. Journal of Family Psychology, 16(1), 38–49. https://doi.org/10.1037/0893-3200.16.1.38
- Jorns-Presentati, A., Napp, A. K., Dessauvagie, A. S., Stein, D. J., Jonker, D., Breet, E., Charles, W., Swart, R. L., Lahti, M., Suliman, S., Jansen, R., van den Heuvel, L. L., Seedat, S., & Groen, G. (2021). The prevalence of mental health problems in sub-Saharan adolescents: A systematic review. PLoS ONE, 16, 1–23. https://doi.org/10.1371/journal.pone.0251689
- Kalil, A., & Kunz, J. (2002). Teenage childbearing, marital status, and depressive symptoms in later life. Child Development, 73(6), 1748–1760. https://doi.org/10.1111/1467-8624.00503
- Khatoon, F., Saba, I., Ghafoor, M., Rajpar, A. P., Mahmood, A., & Ali, M. (2021). Adverse maternal and fetal outcomes of adolescent pregnancy. Journal of The Society of Obstetricians and Gynaecologists of Pakistan, 11(1), 41–44. Accessed September 29, 2022. https://jsogp.net/index.php/jsogp/article/view/401
- Kim, T., & Kim, J. (2020). Linking adolescent future expectations to health in adulthood: Evidence and mechanisms. Social Science & Medicine, 263, 113282. https://doi.org/10.1016/J.SOCSCIMED.2020.113282
- Lee, J. O., Jeong, C. H., Yuan, C., Boden, J. M., Umaña-Taylor, A. J., Noris, M., & Cederbaum, J. A. (2021). Externalizing behavior problems in offspring of teen mothers: A meta-analysis. Journal of Youth and Adolescence, 49(6), 1146–1161. https://doi.org/10.1007/s10964-020-01232-y.
- Letourneau, N. L., Tramonte, L., & Willms, J. D. (2013). Maternal depression, family functioning and children’s longitudinal development. Journal of Pediatric Nursing, 28(3), 223–234. https://doi.org/10.1016/J.PEDN.2012.07.014
- Li, J., Imam, S. Z., Jing, Z., Wang, Y., & Zhou, C. (2021). Suicide attempt and its associated factors amongst women who were pregnant as adolescents in Bangladesh: A cross-sectional study. Reproductive Health, 18(1), 1–9. https://doi.org/10.1186/s12978-021-01127-6
- Mann, L., Bateson, D., & Black, K. I. (2020). Teenage pregnancy. Australian Journal of General Practice, 49(6), 310–316. https://doi.org/10.31128/AJGP-02-20-5224
- Maughan, B., & Lindelow, M. (1997). Secular change in psychosocial risks: The case of teenage motherhood. Psychological Medicine, 27(5), 1129–1144. https://doi.org/10.1017/S0033291797005576
- Mokwena, J. P., Govender, S., & Setwaba, M. B. (2016). Health and well-being among teenage mothers in a rural South African community. Journal of Psychology in Africa, 26(5), 428–431. https://doi.org/10.1080/14330237.2016.1219539
- Musyimi, C. W., Mutiso, V. N., Nyamai, D. N., Ebuenyi, I., & Ndetei, D. M. (2020). Suicidal behavior risks during adolescent pregnancy in a low-resource setting: A qualitative study. PLoS ONE, 15(7), e0236269. https://doi.org/10.1371/JOURNAL.PONE.0236269
- Mutahi, J., Larsen, A., Cuijpers, P., Peterson, S. S., Unutzer, J., McKay, M., John-Stewart, G., Jewell, T., Kinuthia, J., Gohar, F., Lai, J., Wamalwa, D., Gachuno, O., & Kumar, M. (2022). Mental health problems and service gaps experienced by pregnant adolescents and young women in Sub-saharan Africa: A systematic review. eClinicalMedicine, 44, 101289. https://doi.org/10.1016/j.eclinm.2022.101289
- Mweteni, W., Kabirigi, J., Matovelo, D., Laisser, R., Yohani, V., Shabani, G., Shayo, P., Brenner, J., & Chaput, K. (2021). Implications of power imbalance in antenatal care seeking among pregnant adolescents in rural Tanzania: A qualitative study. PLoS ONE, 16(6), https://doi.org/10.1371/JOURNAL.PONE.0250646
- National Heart Lung and Blood Institute. 2013. Study Quality Assessment Tools. Published 2013. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372. https://doi.org/10.1136/BMJ.N71
- Patel, P. H., & Sen, B. (2012). Teen motherhood and long-term health consequences. Maternal and Child Health Journal, 16(5), 1063–1071. https://doi.org/10.1007/s10995-011-0829-2
- Piyasil, V. (1998). Anxiety and depression in teenage mothers : A comparative study. Journal of the Medical Association of Thailand, 81(2), 124–129.
- Pregnancy Rights Your Legal Options during and after Pregnancy. (2021). Retrieved November 26, 2023, from www.communitylaw.org.nz
- Reid, V., & Meadows-Oliver, M. (2007). Postpartum depression in adolescent mothers: An integrative review of the literature. Journal of Pediatric Health Care, 21(5), 289–298. https://doi.org/10.1016/J.PEDHC.2006.05.010
- Schmidt, R. M., Wiemann, C. M., Rickert, V. I., & Smith, E. O. B. (2006). Moderate to severe depressive symptoms among adolescent mothers followed four years postpartum. Journal of Adolescent Health, 38(6), 712–718. https://doi.org/10.1016/j.jadohealth.2005.05.023
- Sedgh, G., Finer, L. B., Bankole, A., Eilers, M. A., & Singh, S. (2015). Adolescent pregnancy, birth, and abortion rates across countries: Levels and recent trends. Journal of Adolescent Health, 56(2), 223–230. https://doi.org/10.1016/J.JADOHEALTH.2014.09.007
- Shifflet-Chila, E. D., Rena Harold, L. D., Victoria Fitton, L. A., & Ahmedani, B. K. (2016). Adolescent and family development: Autonomy and identity in the digital age. Children and Youth Services Review 70, 364–368.
- Staneva, A., Bogossian, F., Pritchard, M., & Wittkowski, A. (2015). The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women and Birth, 28(3), 179–193. https://doi.org/10.1016/J.WOMBI.2015.02.003
- Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366. https://doi.org/10.1136/BMJ.L4898
- Stiffman, A. R., Earls, F., Robins, L. N., Jung, K. G., & Kulbok, P. (1987). Adolescent sexual activity and pregnancy: Socioenvironmental problems, physical health, and mental health. Journal of Youth and Adolescence, 16(5), 497–509. https://doi.org/10.1007/BF02202943
- TACAdmin. (2021). Legal rights in teenage pregnancy for teen mom & parents | Texas Adoption Center. Published 2021. Retrieved November 26, 2023, from https://texasadoptioncenter.org/blog/teenage-pregnancy-legal-rights/
- Taylor, J. L. (2009). Midlife impacts of adolescent parenthood. Journal of Family Issues, 30(4), 484–510. https://doi.org/10.1177/0192513X08329601
- Tirumalaraju, V., Suchting, R., Evans, J., Goetzl, L., Refuerzo, J., Neumann, A., Anand, D., Ravikumar, R., Green, C. E., Cowen, P. J., & Selvaraj, S. (2020). Risk of depression in the adolescent and adult offspring of mothers with perinatal depression: A systematic review and meta-analysis. JAMA Network Open, 3(6), e208783. https://doi.org/10.1001/JAMANETWORKOPEN.2020.8783
- UNFPA. 2013. UNPFA state of the World’s Population. Motherhood in Childhood. Unfpa. Published online 2013:ii-116. http://www.unfpa.org/sites/default/files/pub-pdf/EN-SWOP2013-final.pdf
- Van der Kooy, K., van Hout, H., Marwijk, H., Marten, H., Stehouwer, C., & Beekman, A. (2007). Depression and the risk for cardiovascular diseases: Systematic review and meta analysis. International Journal of Geriatric Psychiatry, 22(7), 613–626. https://doi.org/10.1002/GPS.1723
- Vanderkruik, R., Gonsalves, L., Kapustianyk, G., Allen, T., & Say, L. (2021). Mental health of adolescents associated with sexual and reproductive outcomes: A systematic review. Bulletin of the World Health Organization, 99(5), 359–373. https://doi.org/10.2471/BLT.20.254144
- Van Der Waerden, J., Galéra, C., Larroque, B., Saurel-Cubizolles, M. J., Sutter-Dallay, A. L., & Melchior, M. (2015). Maternal depression trajectories and children’s behavior at age 5 years. The Journal of Pediatrics, 166(6), 1440–1448.e1. https://doi.org/10.1016/J.JPEDS.2015.03.002
- Vicary, J. R., & Corneal, D. A. (2001). A comparison of young women’s psychosocial status based on age of their first childbirth. Family & Community Health, 24(2), 73–84. https://doi.org/10.1097/00003727-200107000-00009
- Walker, D‘A, & Holtfreter, K. (2016). Adolescent motherhood, depression, and delinquency. Journal of Child and Family Studies, 25(3), 939–948. https://doi.org/10.1007/s10826-015-0268-6
- Whitworth, T. R. (2017). Teen childbearing and depression: Do pregnancy attitudes matter? Journal of Marriage and Family, 79(2), 390–404. https://doi.org/10.1111/jomf.12380
- World Health Organization. (2019). Adolescent pregnancy. Retrieved September 1, 2022, from https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy
- Xavier, C., Benoit, A., & Brown, H. K. (2018). Teenage pregnancy and mental health beyond the postpartum period: A systematic review. Journal of Epidemiology and Community Health, 72(6), 451–457. https://doi.org/10.1136/JECH-2017-209923