ABSTRACT
Background: This study was to evaluate the coverage, completeness and timeliness of routine vaccination among children aged 1–7 years in Zhejiang province.
Methods: Demographic information and immunization records of 4613160 children born from Jan 1, 2010 to Dec 31, 2016 were extracted from Zhejiang provincial immunization information system (ZJIIS) on Dec 31, 2017. Vaccination coverage for each vaccine dose and completeness of different vaccine series were calculated by birth cohort, immigration status, and geographic area. The timeliness of vaccine doses scheduled before 12 months of age for the 2016 birth cohort was also examined
Results: Coverage of all the vaccine doses scheduled before 12 months of age and its completeness reached the target goal of 90%. The coverage and completeness decreased substantially in vaccinations scheduled after 12 months old, and most of them were below 90%. The coverage and timeliness estimates of migrant children was lower than those of resident children and the coverage of WenZhou (WZ), Zhoushan (ZS) and Lishui (LS) was lower than other cities across all the birth cohorts. Despite high coverage rates for all antigens by age 12 months, there was a very large range of percent of vaccination delay when comparing different antigens scheduled in the first year of life for the 2016 birth cohort.
Conclusions: This study demonstrated the success and improvement of immunization program in Zhejiang province, and identified some challenges. Strategies such as assessment, feedback, incentives, and exchange program, reminder/recall activity, home visits, immunization requirement for school’s enrollment could be used to reach a higher coverage of the population.
Introduction
The expanded program on immunization (EPI) was launched in 1974 by world health organization (WHO), then had been introduced into China since 1978. The Chinese EPI was established with the introduction of five vaccines, such as Bacillus-Calmette-Guerin (BCG), polio vaccine (PV), diphtheria-tetanus-pertussis vaccine (DTP), measles vaccine (MV) and diphtheria-tetanus vaccine (DT). Hepatitis B vaccine (HepB) had been added into EPI since 2002. The Chinese EPI expanded its coverage on prevention of disease with the introduction of Hepatitis A Vaccine(HepA), Japanese encephalitis vaccine(JEV), meningococcal polysaccharide vaccine-type A(MPV-A), MPV-type A and C(MPV-AC), measles-rubella vaccine (MR) and measles-mumps-rubella vaccine (MMR) in 2009.Citation1 Theoretically, a child needs to get 11 vaccines or 22 vaccine doses before 7 years old. presents the details of immunization schedule in China. As a proportion of children are delivered at home, the policy on BCG and first dose of HepB (HepB1) is not strictly at birth. Although immunization service is delivered free of charge for all children under 7 years old, it can be applied to children up to 14 years old if they have not finished the schedule.
Table 1. Immunization schedule in Chinese EPI.
Vaccination coverage is considered as a key indicator of the performance of EPI. Achieving the very high coverage of routine immunization is necessary for eradicating or eliminating vaccine preventable diseases. Several methods are used to monitor coverage, while each have advantages and disadvantages.Citation2 Most developing countries rely on paper-based system to report administrative coverage estimates, which are often unreliable due to the incomplete or inaccurate primary recording of vaccinations or the inaccurate estimates of population denominators. Household surveys are often proposed, such as the multiple indicators cluster survey (MICS) and the demographic and health survey (DHS), which use the probability sampling methods and the strict quality control process. However, coverage survey can not be routinely performed as it is time-and resource-intensive. Electronic immunization registries can provide the continuous and real-time estimates of vaccination coverage for management activities, such as monitoring vaccine supply and sending reminders to children with overdue vaccinations.Citation3-Citation5
In China, the goal of coverage is at least 90% for each vaccine included in EPI and is at least 95% for two-dose series of measles containing vaccine (MR and MMR).Citation6 In Zhejiang province, vaccination service are provided at the fixed immunization clinics located in the community health centers. In 2014, the vaccination coverage was evaluated among children aged 1–7 years through Zhejiang provincial immunization information system (ZJIIS).Citation7 A substantial decrease trend in vaccine dose scheduled after one year of age was observed and most of them below 90%. Migrant children had lower coverage compared with resident children and the timeliness of immunization was only 70%. To close these gaps, Zhejiang provincial center for disease control and prevention (ZJCDC) had taken many actions, such as extending the vaccination session, increasing the frequency of vaccination service, social mobilization, training program for vaccinators.
The aims of this study were to evaluate the vaccination coverage, completeness and timeliness of the routine immunization among children aged 1–7 years. Moreover, we also compared those estimates by age group, geographical areas and immigration status.
Results
Vaccination coverage in general
A total of 4613160 eligible children were included in this study. Of them, 37.5% were migrant children, and 35.2% were from high-level socio-economic cities, and 49.7% were from low-level socio-economic cities. – presented the vaccination coverage among children aged 1–7 years (N = 4613160), 2–7 years (N = 3840839), 5–7 years (N = 1864321), and 7 years old (N = 551999) on Dec 31, 2017 at both individual and completeness levels. The coverage and completeness of vaccine doses scheduled before 12 months of age reached the goal of 90%. However, the coverage and completeness decreased substantially in vaccine doses scheduled at a later age, and most of them were below 90% at provincial level.
Table 2. Coverage of vaccine doses scheduled ≤ 12 months of age among children aged 1–7 years old*, by vaccine and city.
Table 3. Coverage of vaccine doses scheduled ≤ 24 months of age among children aged 2–7 years old*, by vaccine and city.
Table 4. Coverage of vaccine doses scheduled ≤ 4 years of age among children aged 5–7 years old*, by vaccine and city.
Table 5. Coverage of vaccine doses scheduled ≤ 6 years of age among children aged 7 years old*, by vaccine and city.
Coverage trends of the completeness
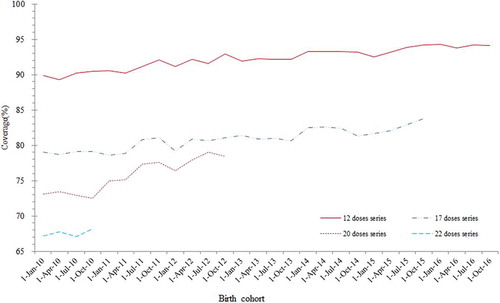
Across the cohorts from 2010 to 2016, the completeness of the 12 doses series scheduled before 12 months old increased gradually over the years and remained above the threshold of 90%. Although the steady increases were also observed in completeness of the 17 doses series, 20 doses series and 22 doses series, the completeness rates of those three series were below 90% across all the relevant birth cohorts (). For the selected four birth cohorts (2010, 2012, 2015 and 2016), the completeness of the relevant doses series were lower among the migrant children than the resident children at both provincial and city level ().
Table 6. Disparities in completeness between migrant and resident children for birth cohort 2010, 2012, 2015 and 2016, by city.
Timeliness
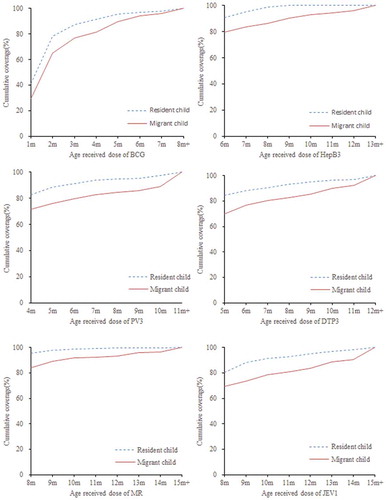
Timeliness of vaccinations scheduled before 12 months of age had been evaluated for the 2016 birth cohort. Only 8.4% of children had delayed their HepB1 vaccinations, but 11%-63% of them had delayed for other vaccinations. Moreover, timeliness of BCG, HepB3, PV3, DTP3 and JEV1 was lower than that of MR (). Compared with the resident children, migrant children were more likely to have delayed vaccinations (). The biggest difference of timely vaccination between them was observed in the 3rd dose of DPT, with a decrease of 14.6% among migrant children. Widening disparities in these vaccine doses between the migrant and the resident children over time were also observed. Although the increase in coverage occurred for both the migrant and the resident children, it was faster for the resident children, resulting in an increasing health disparity over time.
Table 7. Vaccination delay for the 2016 birth cohort.
Discussion
The general coverage of vaccine doses scheduled before 12 months of age and its completeness stably remained over 95%, which was higher than the goal of 90% set by the Chinese EPI. However, the coverage rates went down as cohort age increases. For example, the coverage of BCG for children aged 1–7 years was higher than that for children aged 2–7 years. It mainly was due to the improvements of the Chinese EPI in recent years as the coverage of BCG among children one year old was higher than that of children age ≥ 2 years. Furthermore, the coverage for vaccine doses scheduled after 12 months of age had decreased gradually across all birth cohorts. It reflected that caregivers’ awareness of the primary vaccinations were better than that of the boost vaccination or vaccines scheduled at an older age. The possible reason might be parents’ loss of vaccination awareness when their children got older, or might be the declined frequency of recommended well-child visits when children were over 12 months of age.Citation8-Citation10 Different approaches to overcome the low coverage found in older children were suggested by previous reports: first, the providers could review their immunization information system to identify the children who missed vaccinations and the providers could incorporate reminder/recall activity into their routine practice.Citation11,Citation12 Secondly, the supervisor of EPI at all administrative levels could adopt the assessment, feedback, incentives and exchange (AFIX) method to identify problems, find solutions, support physicians and enhance communications, which had been proved to be a cost-effective way to increase the vaccination coverage.Citation13,Citation14 Third, strategies such as setting school immunization clinics and expanding the day-care centers/elementary schools vaccination requirements could help providers reach a greater coverage for vaccines scheduled at an elder age.Citation15-Citation17
In this study, we found the completeness coverage decreased with more vaccine doses included in the vaccination series at old ages. Another additional finding was that migrant children were more likely not to be fully immunized, which seemed that they did not replicate the patterns of utilization of immunization service among residents. Although we could not explore the specific reasons for these two findings due to the descriptive analyses and limited data from ZJIIS, we attributed high proportion of the missed or drop-out vaccinations to the vulnerability of migrant people in the new sociocultural environment, the complexity of immunization schedule, the poor awareness of completeness of the vaccination schedule, the barriers or vaccination hesitation, and other factors from provider’s aspect. Specifically, the complexity of immunization schedule might make it difficult for caregivers to remember the next vaccination and its due date, especially for vaccine doses schedule at an elder age.Citation18 The knowledge on the importance and necessity of completeness of the immunization schedule was poor among caregivers. For example, our previous study in Zhejiang province found that children from a relative undeveloped area or among migrant people tended to experience more drop outs for DTP.Citation19 Caregivers might not be able to or willing to overcome barriers, like missing work or school, for their children’s vaccination. According to our previous study,Citation19 we assumed that it would be more significant in migrant children, whose parents had not enough time for the primary healthcare and were less aware of the information on vaccination. Furthermore, a proportion of caregivers would be hesitate with childhood vaccinations due to the misconceptions or rumors on vaccine safety from the social media.Citation20 Some determinants from provider’s aspect might also impact the completeness of vaccination. First, system based factors like well-child visit disproportionately might affect the elder children as they had fewer health facility visits than the young. That meant the elder child sometimes needed a separate, special visit for vaccination, while the younger child could get vaccination at the same time of a well-child visit. Second, the frequency of immunization session and the service time of vaccination clinic also played an important role. Our previous study indicated that the frequent session and extending service time were the most beneficial interventions to improve the mothers’ compliance with the immunization schedule.Citation21
Although many children would eventually complete the vaccination schedule, a proportion of them still did not receive those vaccinations timely. However, compared with our previous study, the timeliness of vaccinations scheduled before 12 months old of the 2016 birth cohort was higher than that of the 2010 birth cohort, especially for MR vaccination.Citation7 This remarkable evolution might mainly be a result of the increased attention for timely vaccination in Zhejiang province. Intervention focused on sending reminders through Short Messaging Service (SMS) to caregivers was conducted to improve the timeliness of MR to stop the measles transmission during the measles outbreak in 2008. Due to the effectiveness of this intervention, ZJCDC suggested all immunization clinics should make efforts to enhance timeliness of all childhood vaccinations mainly through raising awareness of physicians and sending SMS to caregivers. Furthermore, timeliness was considered as an important index for assessing the performance of the local immunization program since 2011.
In this study, we found that most of the BCG vaccination was delayed, which was very different with the pattern of HBV1. We speculated that there might be three reasons: first, the lack of mandatory recommendation on BCG vaccination at birth would be an independent risk factor of its delayed administration. However, administration of HBV1 within 24 hours after delivery was required for every registered maternity hospital in China. Second, the lower timeliness might be due to the use of one vial of BCG contained 10 doses, therefor, the majority of immunization clinics provided BCG vaccination service once a week to reduce the vaccine wastage. The average vaccine wastage rate was 80% for BCG over the past five years in Zhejiang province, which was the highest among all EPI vaccines. Third, the lower timeliness might be associated with the uncertainty of the efficacy and safety profile of BCG. As we know, BCG could only protect tuberculous meningitis and miliary tuberculosis rather than community acquired tuberculosis.Citation22 Furthermore, the incidence of adverse event on the injection site after BCG vaccination was frequently reported.Citation23,Citation24 Thus, many parents would have hesitations when they decided to have their children receive BCG dose. However, we recommended BCG should be given to all infants as soon as possible after birth as BCG was currently the only available vaccine for tuberculosis prevention and China was a high tuberculosis burden country with the third highest number of tuberculosis cases reported annually worldwide.Citation25 Interventions focused on recommending all maternity hospitals to give BCG vaccination at birth and using a vial of one dose of BCG and the correction of misunderstanding of BCG vaccination would be useful to close the gaps.
Vaccination coverage continues to vary across areas and it was lower in some cities such as WZ, ZS and LS. Clusters of unvaccinated children leaved communities vulnerable to outbreaks of vaccine preventable diseases like measles or pertussis. Although the two outbreaks of measles in the last decade had improved the awareness of maintaining the uniformly high coverage to interrupt the disease transmission, there were still gaps at sub-provincial level. Financial policy on the investment of EPI at local level, as well as differences in the population characteristics, the scale of migrant children, the accessibility and the policy on immunization check of the kindergarten- or school-entry, might also contribute to variations in vaccination coverage.
There were several limitations to this study. First, the demographic information collected by ZJIIS was limited, which restrained the scope of the research to detect the potential risk factors of vaccination coverage. The potential risk factors we discussed above were speculative, and there might be other barriers or risk factors. Further research on these issues are needed and interventions should be taken if the truly important factors are detected. Second, only children with immunization record in ZJIIS were included, and our results would be overestimated due to the registered children would be more likely to be vaccinated than those not registered.
Conclusion
Our results demonstrated the success and the improvement of EPI in Zhejiang province, and identified some challenges in the meantime. We recommend continuing surveillance on the children aged < 7 years and subpopulations be conducted to estimate the vaccination coverage and to assess the vulnerability to the vaccine preventable diseases. The coverage differences found in this study might provide the evidence to decision-makers, with respect to identifying vulnerable populations and fulfilling the needs of under-immunized children. Providers should make efforts to achieve and maintain the high coverage of vaccines, especially for vaccine doses scheduled after 12 months of age. Strategies such as AFIX, reminder/recall activity, home visits, immunization check of the kindergarten- or school-entry could be used to reach a better coverage.
Methods
Data resources
In this study, anonymized individual records of children, including demographic information and vaccination records were extracted from ZJIIS on Dec 31, 2017. ZJIIS is a computerized, population-based immunization registration system, containing demographic information and vaccination records for children under 7 years old living in Zhejiang province.Citation7 Almost all immunization clinics in Zhejiang province are included in ZJIIS. Child will be registered in ZJIIS with a unique identification number at his/her first time of contact with any immunization clinic in Zhejiang province. Child’s demographic information (such as name, date of birth, gender, family address, phone number, immigration status) and historical and current immunization records should be entered into ZJIIS and these data will be updated in real time if there is any change. Due to the high participation and timely data, ZJIIS provides an in-depth, real-time tool for monitoring the vaccination coverage, which helps programmatic decision-making when used in conjunction with other methods of coverage monitoring.
Study areas
Ten out of eleven cities in Zhejiang province were included in this study. Huzhou city was excluded as it did not participate in ZJIIS. According to the estimates of Gross Domestic Product (GDP) per capita in 2017, we stratified the ten cities into three socio-economic categories: Hangzhou (HZ), Ningbo (NB), Zhoushan (ZS) were classified as the high level for GDP per capita > 15000 USD; Shaoxing (SX), Jiaxing (JX) were classified as the middle level for GDP per capita between 10000 and 15000 USD; Taizhou (TZ), Quzhou (QZ), Lishui (LS), Wenzhou (WZ), Jinhua (JH) were classified as the low level for GDP per capita < 10000 USD.
Target population
Children aged 1–7 years (born from Jan 1, 2010 to Dec 31, 2016) and registered in ZJIIS and not designated as ‘permanently inactive’ (i.e. deceased) or ‘moved or gone elsewhere’ were eligible for inclusion.
Definitions and measurements
The cohort method had been used for data analyses in this study.Citation26 Three-month wide or 12-month wide cohorts were used for time trend analyses, and timeliness or risk factor analyses, respectively. We defined the 2010 birth cohort as the children born between January 1 and December 31, 2010. Other birth cohorts from 2011 to 2016 were defined by analogy. Cohort immunization status was assessed at 12 months of age (for vaccine doses due at 8 months), 24 months of age (for vaccine doses due at 18 months), 5 years of age (for vaccine doses due at 4 years) and 7 years of age (for vaccine doses due at 6 years).
The vaccination coverage was defined as the proportion of vaccinated children among the target population. Vaccination dose was considered invalid if it 1) was administrated before the earliest age of the immunization schedule or 2) was administrated < 28 days from the previous dose for multiple-dose needed vaccines (such as DTP). Invalid dose was excluded from the analyses and considered as non-vaccinated.
Completeness (full immunized) was defined as the proportion of children at specific age range who received all vaccinations scheduled before their current age. “Fully immunized” at 12 months of age (12 doses series) was defined as a child receiving 1 dose of BCG, 3 doses of HepB, 3 doses of PV, 3 doses of DTP, 1 dose of MR and 1 dose of JEV. “Fully immunized” at 24 months of age (17 doses series) was defined as a child receiving 1 dose of BCG, 3 doses of HepB, 3 doses of PV, 4 doses of DTP, 1 dose of MR, 1 dose of JEV, 1 dose of HepA, 1 dose of MMR and 2 doses of MPV-A. “Fully immunized” at 5 years of age (20 doses series) was defined as a child receiving 1 dose of BCG, 3 doses of HepB, 4 doses of PV, 4 doses of DTP, 1 dose of MR, 2 doses of JEV, 1 dose of HepA, 1 dose of MMR, 2 doses of MPV-A and 1 dose of MPV-AC. “Fully immunized” at 7 years of age (22 doses series) was defined as a child receiving 1 dose of BCG, 3 doses of HepB, 4 doses of PV, 4 doses of DTP, 1 dose of MR, 2 dose of JEV, 1 dose of HepA, 1 dose of MMR, 2 doses of MPV-A, 2 doses of MPV-AC and 1 dose of DT.
Timely immunization was defined as the receipt of a scheduled vaccine dose within 30 days of the recommended age, except for the HepB1, which should be vaccinated in 24h after birth.Citation27 For descriptive purposes, we categorized the outcomes for each dose as either vaccine dose “no delay” (timely immunized), “delay of between 1 to 3 months”, or “delay greater than 3 months”. Timeliness was examined only for the 2016 birth cohort and for vaccine doses scheduled before 12 months of age. For vaccines requiring multiple doses (PV, DTP, HepB), only the last dose was evaluated for its timeliness.
Immigration status in ZJIIS is recorded as three types: “migrant child from other province”, “migrant child from other municipalities of Zhejiang Province”, or “resident child”. We combined both “migrant child from other province” and “migrant child from other county in Zhejiang province” as “migrant child” and excluded the foreign child in this study.
Statistical analysis
For data analysis, we organized the database as an Excel (Microsoft Office Excel 2013) file. The vaccination coverage and completeness was calculated by different birth cohorts, cities. Timeliness of different vaccinations were depicted by plotting the cumulative percentage receiving each vaccine dose by age, with the proportion immunized set as 100%. We performed all analysis with SAS (SAS Institute, Inc., Cary, NC, version 9.3).
Ethical considerations
This study was exempt from ethical review since it involved examination of de-identified data.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We would like to thank Lingbo Zhang from Suzhou Shensu Automatic Technology Co., Ltd. for providing assistance with the ZJIIS data.
Additional information
Notes on contributors
Ying Wang
Yu Hu and Yaping Chen conceived and designed the experiments; Yu Hu and Yaping Chen performed the experiments; Yu Hu and Hui Liang analyzed the data; Ying Wang contributed reagents/materials/analysis tools; Yu Hu wrote the paper.
References
- Hu Y, Chen Y, Guo J, Tang X, Shen L. 2014. Completeness and timeliness of vaccination and determinants for low and late uptake among young children in eastern China. Hum Vaccin Immunother. 10:1408–1415. doi:10.4161/hv.28054.
- Cutts FT, Claquin P, Danovaro-Holliday C, Rhoda DA. 2016. Monitoring vaccination coverage: defining the role of surveys. Vaccine. 34:4103–4109. doi:10.1016/j.vaccine.2016.06.053.
- Centers for Disease C, Prevention. . Immunization information system progress–united States. 2004.MMWR Morbidity and Mortality Weekly Report. 2005 54:1156–1157.
- Community Preventive Services Task F. Recommendation for use of immunization information systems to increase vaccination rates. Journal Public Health Management Practice: JPHMP. 2015;21:249–252. doi:10.1097/PHH.0000000000000092.
- Curran EA, Bednarczyk RA, Omer SB. 2013. Evaluation of the frequency of immunization information system use for public health research. Hum Vaccin Immunother. 9:1346–1350. doi:10.4161/hv.24033.
- Hu Y, Wang Y, Chen Y, Li Q. Determinants of inequality in the up-to-date fully immunization coverage among children aged 24-35 months: evidence from Zhejiang province, East China. Hum Vaccin Immunother. 2017;13: 1902–1907. doi:10.1080/21645515.2017.1327108.
- Li Q, Hu Y, Zhong Y, Chen Y, Tang X, Guo J, Shen L Using the immunization information system to determine vaccination coverage rates among children aged 1-7 years: a report from Zhejiang Province, China. Int J Environ Res Public Health. 2014;11:2713–2728. doi:10.3390/ijerph110302713.
- Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. 2013. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: a cross- sectional study. BMC Public Health. 13:908. doi:10.1186/1471-2458-13-908.
- Ndiritu M, Cowgill KD, Ismail A, Chiphatsi S, Kamau T, Fegan G, Feikin DR, Newton CR, Scott JAG. 2006. Immunization coverage and risk factors for failure to immunize within the Expanded Programme on Immunization in Kenya after introduction of new Haemophilus influenzae type b and hepatitis b virus antigens. BMC Public Health. 6:132. doi:10.1186/1471-2458-6-132.
- Oleribe O, Kumar V, Awosika-Olumo A, Taylor-Robinson SD. 2017. Individual and socioeconomic factors associated with childhood immunization coverage in Nigeria. Pan Afr Med J. 26:220. doi:10.11604/pamj.2017.26.38.10312.
- Bosch-Capblanch X, Ronveaux O, Doyle V, Remedios V, Bchir A. 2009. Accuracy and quality of immunization information systems in forty-one low income countries. Tropical Medicine International Health: TM IH. 14:2–10. doi:10.1111/j.1365-3156.2008.02181.x.
- Groom H, Hopkins DP, Pabst LJ, Murphy Morgan J, Patel M, Calonge N, et al. Immunization information systems to increase vaccination rates: a community guide systematic review. Journal Public Health Management Practice: JPHMP. 2015;21:227–248. doi:10.1097/PHH.0000000000000069.
- Massoudi MS, Walsh J, Stokley S, Rosenthal J, Stevenson J, Miljanovic B, Mann J, Dini E Assessing immunization performance of private practitioners in Maine: impact of the assessment, feedback, incentives, and exchange strategy. Pediatrics. 1999;103:1218–1223.
- Rosenberg K, Kayyali A. AFIX Consultations may increase vaccination coverage in younger Adolescents. Am J Nurs. 114;2014:65–66.
- Fogarty KJ, Massoudi MS, Gallo W, Averhoff FM, Yusuf H, Fishbein D. 2004. Vaccine coverage levels after implementation of a middle school vaccination requirement, Florida, 1997-2000. Public Health Rep. 119:163–169. doi:10.1177/003335490411900209.
- Jacobs RJ, Meyerhoff AS. 2004. Effect of middle school entry requirements on hepatitis B vaccination coverage. J Adolescent Health: Official Publication Soc Adolesc Med. 34:420–423. doi:10.1016/j.jadohealth.2003.08.014.
- Shaw J, Tserenpuntsag B, McNutt LA, Halsey N. 2014. United States private schools have higher rates of exemptions to school immunization requirements than public schools. J Pediatr. 165:129–133. doi:10.1016/j.jpeds.2014.03.039.
- Dominguez SR, Daum RS. Physician knowledge and perspectives regarding influenza and influenza vaccination. Hum Vaccin. 1;2005:74–79.
- Hu Y, Chen E, Li Q, Chen Y, Qi X. 2015. Immunization coverage and its determinants among children born in 2008-2009 by questionnaire survey in Zhejiang. China Asia-Pacific Journal Public Health/Asia-Pacific Academic Consortium Public Health. 27:NP1132–43. doi:10.1177/1010539511430995.
- Hu Y. 2015. Does an education seminar intervention improve the parents’ knowledge on vaccination? Evidence from Yiwu, East China. Int J Environ Res Public Health. 12:3469–3479. doi:10.3390/ijerph120403469.
- Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J, Zhang B Does introducing an immunization package of services for migrant children improve the coverage, service quality and understanding? An evidence from an intervention study among 1548 migrant children in eastern China. BMC Public Health. 2015;15:664. doi:10.1186/s12889-015-1998-5.
- Arbelaez MP, Nelson KE, Munoz A. BCG vaccine effectiveness in preventing tuberculosis and its interaction with human immunodeficiency virus infection. Int J Epidemiol. 29;2000:1085–1091.
- Verreck FAW, Tchilian EZ, Vervenne RAW, Sombroek CC, Kondova I, Eissen OA, Sommandas, V., van der Werff, N.M., Verschoor, E., Braskamp, G. and Bakker, J. Variable BCG efficacy in rhesus populations: pulmonary BCG provides protection where standard intra-dermal vaccination fails. Tuberculosis. 2017;104:46–57. doi:10.1016/j.tube.2017.02.003.
- Liu J, Tran V, Leung AS, Alexander DC, Zhu B. BCG vaccines: their mechanisms of attenuation and impact on safety and protective efficacy. Hum Vaccin. 5;2009:70–78.
- Burki TK. 2018. The global cost of tuberculosis. The Lancet Respiratory Medicine. 6:13. doi:10.1016/S2213-2600(17)30468-X.
- Stokley S. 2011. Compliance with recommendations and opportunities for vaccination at ages 11 to 12 years: evaluation of the 2009 national immunization survey-teen. Arch Pediatr Adolesc Med. 165:813–818. doi:10.1001/archpediatrics.2011.138.
- Smith PJ, Humiston SG, Parnell T, Vannice KS, Salmon DA. 2010. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep. 125:534–541. doi:10.1177/003335491012500408.