ABSTRACT
Despite high HPV prevalence and low vaccination rates in the military, HPV vaccination is not required upon military service initiation. Given that national HPV vaccination rates remain low among people age 19–26 years, military service may represent an opportune time for intervention. The purpose of this study was to quantify the rate of HPV vaccination among young patients entering primary care at a single Veterans Affairs Medical Center (VAMC). Vaccination rates among veterans age ≤ 26 years old at first primary care visit were identified from the institutional data warehouse. Among 1,258 eligible patients, most were male (n = 782). The HPV vaccine initiation rate was 21.2%. Overall, 10.4% of patients received at least 1 HPV vaccine prior to initiating care at the VA (25.2% females and 1.4% males). An additional 10.8% of patients received their first HPV vaccine upon initiating care at the VA. Median age of first HPV vaccination was 21.4 years among patients that initiated the vaccine in the military versus 24.8 years among those that initiated vaccination at the VA. In conclusion, this study demonstrated low HPV vaccination rates both prior to transitioning to VA primary care and once receiving care at the VA. Additionally, among veterans that had not received vaccination upon initiating care at the VA, older age at vaccination was observed. Older age at vaccination may reduce HPV vaccine effectiveness given higher risk of exposure. Addition of HPV to the list of mandated vaccines upon military service initiation should be considered.
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States; it is estimated that nearly 80 million people are currently infected and there are 14 million new infections per year.Citation1 HPV infection has serious health implications including cancer of the cervix, vulva, penis, anus, and oropharynx. The personal and systemic burdens of these diseases represent a major public health concern.
Immunization is not effective in eradication of preexisting HPV infection; vaccination is best given prior to exposure through sexual contact and induces a higher antibody response when given at a younger age.Citation2 Current HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) include routine vaccination at ages 11 or 12 years in males and females, although catch-up vaccines may be given up to age 26. Recent recommendations have shifted to a 2-dose series in adolescents, while patients starting the series on or after age 15 should receive 3 doses, ideally within a 6-month period.Citation3
National rates for initiation of HPV vaccination (≥1 dose) among previously unvaccinated males and females aged 19–26 years remain under 10% while over half of new infections occur between age 15 to 24 years.Citation4,Citation5 Given that previous studies have demonstrated a higher seroprevalence and acquisition rate of HPV among male and female service members as compared to civilians, it is of public health interest to maximize HPV vaccination rates in this population.Citation6–Citation8
Upon entering the military, the Department of Defense (DoD) has a list of mandated vaccinations for new personnel; however, the HPV vaccine, although encouraged, is not required.Citation9 Therefore, young adults joining the military at an age of increasing sexual activity that have not previously been vaccinated remain at risk for preventable cancers. Evaluation of HPV vaccination in the military has demonstrated that rates of vaccine initiation are low (0.4%-26.6%).Citation10–Citation14 The addition of the HPV vaccine to the registry of required immunizations at time of military accession may represent an important opportunity to protect against HPV.
In 2011 there were over 150,000 accessions to the United States military force, 91% of which were age 18–26.Citation15 During the same year, over 70% of the 224,695 military separations were in veterans under 35 years old.Citation16,Citation17 Upon completion of military service, up to 62% of veterans utilize the Veterans Affairs Medical Center (VAMC) system for health care services – patients under 35 years old make up 25% of female VA users and 11.3% of male users.Citation18,Citation19 The transition from the DoD to VA primary care services may represent an opportunity for HPV vaccination not given in the military. However, as care at the VA is often initiated at a later age, by the time a veteran is seen at the VA HPV exposure may have already occurred or the age of eligibility may have passed. Further challenging the issue of care transition are inconsistencies in recording of immunizations that occur outside or previous to the DoD and difficulties in accessing all military health records once a patient is seen at the VA.
The objective of this study was to calculate the HPV vaccination rates among veterans presenting to the VA for primary care visits, and to compare the vaccination initiation rate at the DoD to that at the VA. Characterization of immunization rates may help determine whether addition of HPV to the list of mandated vaccinations at initiation of military service may increase vaccine uptake and vaccination at an earlier age.
Results
There were 1,258 veterans identified that met inclusion criteria. The majority of veterans were male (n = 782; 62.2%). Most patients had previously served in the Army (44.6%), followed by the Marine Corps (23.6%).
The overall HPV vaccination initiation rate in our population of veterans, regardless of vaccination site, was 21.2% (n = 267). The overall rate of HPV vaccine initiation was 11.0% (n = 86) in males and 38.0% (n = 181) among females. (, )
Table 1. Characteristics of overall HPV vaccination status of veterans age ≤26 who initiated primary care at Bronx VAMC between 2011 and 2017.
Overall, 131 patients (10.4%) had documentation of HPV vaccine initiation prior to their first primary care visit at the VA. Of these, 12 patients had documented vaccine initiation prior to active duty entry in the military (age <18). The overall rate of HPV vaccine initiation prior to the first VA visit was 120 (25.2%) for females and 11 (1.4%) for male patients. Patients that had served in the Air Force had the highest rate of vaccination (15/58; 25.9%) followed by the Navy (33/208; 15.9%). ()
Figure 2. Vaccination rate by military branch among service members vaccinated prior to first VA visit, 2011–2017.
The rate of 3-dose series completion for those who began the vaccine series was 67.9% prior to first VA visit (89/131). () Out of 89 patients who began and completed their HPV vaccination prior to first VA visit, 53 had complete data for vaccination dates. The remaining patients had a note in the Computerized Personal Record System (CPRS) electronic medical chart stating that the series was complete but did not have all dates included in the documentation. Of the patients that initiated vaccination prior to the military, 10/12 completed their series prior to the military. The median age of first vaccination for patients who received the HPV vaccine while in the military (age≥18) was 21.4 years (IQR 19.7–23.0). Median interval to series completion among patients who initiated vaccination in the military was 2.1 years (IQR 0.87–3.56).
Table 2. Characteristics of HPV vaccine initiation and completion overall and by vaccination location among veterans age ≤ 26 who initiated primary care at Bronx VAMC between 2011 and 2017.
An additional 136 patients (10.8%) received the HPV vaccine after their first VA primary care visit. There were 86 patients who completed the 3-dose HPV vaccine series after VA visit. () Of this group, 30 had complete vaccination dates documented. Again, the others did not have all dates documented but had a note indicating completion. The median interval time to vaccine series completion was 0.88 years (IQR 0.55–1.35). The median age of first HPV vaccination for patients with available data was 24.8 years (IQR 23.7–25.8). Over a quarter (26.6%) of patients were at the tail end of HPV vaccine eligibility (age 26 years) at time of first VA primary care appointment.
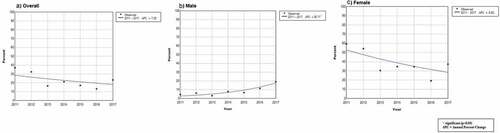
Trend analysis by year of first VA appointment demonstrated that the percent of HPV vaccination significantly increased among male patients with annual percent change +36.7% between 2011 and 2017 (p < 0.05). However, trend analysis of HPV vaccination rates overall and in female patients demonstrated no significant change. ()
Discussion
HPV has the highest incident infection rate of any sexually transmitted infection among United States military personnel.Citation20 Given the long-term cancer risks associated with HPV and the high rate of HPV among US service members, vaccination has an important preventive role.Citation6,Citation8 Failure to initiate vaccination at time of entry into military service may represent an important missed opportunity for vaccination prior to HPV exposure, with potential serious long-term health consequences.
Evaluation of HPV vaccination rates in a cohort of eligible veterans that had primary care visits at the VA demonstrated that overall documented HPV vaccination rates are low among veterans, with approximately 1 in 5 initiating vaccination. Comparison to reported national rates demonstrates several interesting trends. First, data from the 2016 National Health Interview Survey, which excludes active duty military personnel, demonstrated that while HPV vaccine initiation rates at any age among 19–26 year olds were 48.5% and 13.5% among females and males respectively, rates of initiation for those who had not previously received any vaccination before age 19 years were 8.6% and 2.7%, for females and males respectively.Citation5 Therefore, most patients had received the vaccine at a younger age. In our series, the overall HPV vaccination rate among females and males was 38% and 11%, respectively. For females who did not receive any HPV vaccination prior to military service, the initiation rate was 35.5%. Therefore, the military does serve as an important site to capture patients that were not previously vaccinated as adolescents. Second, the rate of recorded HPV vaccines prior to military service in this population was 0.95% which is significantly lower than the previously reported data. It is not possible to tell based on the present study whether this represents specific population-based factors driving low vaccination rates, or more likely, systematic failure to record vaccinations that occurred outside of the military. Future study should identify whether these errors are in recording of vaccinations that occur outside prior to the military or difficulty at the VA in accessing the patient’s vaccination history given prior to transition of care to the VA.
To our knowledge, this is the first study to examine military HPV vaccination in the VA setting. The vaccination rates in our series are similar to those reported in several previous studies that evaluated vaccination in active duty females and demonstrated initiation and completion rates ranging from 15% to 67.8%.Citation10–Citation12,Citation14,Citation21,Citation22 The variation of reported rates likely reflects the setting of most of the studies – specific military health care facilities serving specific military branches.
There is a paucity of literature on HPV vaccination rates in male service members. Studies including men have demonstrated initiation rates ranging from 5.8–32.2% with 3–19% vaccine completion.Citation11,Citation13,Citation14,Citation22 The variation in reported rates reflects small sample sizes in both studies and differences in outcome measures (initiation versus completion). In our series, only 1.4% of males had documentation of HPV vaccine initiation prior to first VA appointment. Although low vaccination rates apply to both genders, it is more prominent in males. However, our study did demonstrate that HPV vaccination initiation for males by year of initial VA appointment increased over the study period which implies a shifting paradigm in male HPV vaccination. Lower HPV vaccine initiation rates among male service members highlights the ongoing challenges in shifting perceptions among providers and patients regarding gender and HPV vaccination. Recent data have reported that 10.7% of US men over 18 years old have received any HPV vaccination.Citation5,Citation23
Delay of initiation of HPV vaccination until VA attendance may increase the likelihood that patients have already been infected with HPV and reduce the effectiveness of the vaccine.Citation2 In this study, the average age of initiation of vaccination was over 24 years old. Furthermore, 26% of patients were too old to be vaccinated at the time of their first VA appointment. Although we did not evaluate HPV prevalence, the results of previous studies on prevalence amongst US service members suggest that exposure is high. A report of incidence of sexually transmitted infections from 2000 to 2012 among active duty service members demonstrated that the incidence of HPV was almost 2 times higher than any other STI.Citation20 High seroprevalence of HPV has been demonstrated with up to 34% seroincidence of new infection occurring, as measured from service entry across a 10-year study period.Citation7,Citation8 Vaccination has been demonstrated to be effective in a military population – a military-wide population based study of over 1 million active duty personnel demonstrated that genital wart incidence decreased after introduction of the HPV vaccine.Citation24
A final issue to note is the time interval between initiation and completion of the HPV vaccine series in this study. It has been shown that a longer time to complete the 3-dose schedule is associated with increased risk of HPV infection and negative sequelae of HPV.Citation25 In this study, although limited by incomplete data, the median interval to vaccine completion was over 1 year. Similarly, Maktabi et al demonstrated that in 270,000 female active duty servicewomen between 2006 and 2011, of the 15% that had vaccine initiation only 15% completed their 3-dose series within the recommended 6 month period.Citation12
The findings of this study are supported by the large sample size; however, there are several limitations. First, it is possible that HPV vaccination rates are underreported in this cohort. Although the military record immunization data is accessible at the VA through an electronic medical record interface, Joint Legacy Viewer (JLV), not all vaccines appeared in both JLV and CPRS, reflecting inconsistency in communication between these two health record systems. However, the vaccination rates previously reported utilizing active duty personnel are similar, supporting the conclusion that vaccination rates among active duty personnel are low. Second, it is possible that some patients were vaccinated outside of the military health system resulting in incomplete data. Current practice in the military is to administer all required vaccines at time of entry to basic training regardless of previous vaccination status. Outside vaccinations may be added to records at a later date, but this is clinician specific and not systematic. As such, vaccines received outside of the military may not have been recorded. The variation in HPV vaccination rates we found between different military branches may similarly be the result of documentation practices, immunization practices, or both. Further research is needed to elucidate this variation. In a recent cohort study of vaccination initiation rates among active duty service members between 2007 and 2017, although the authors were similarly limited in detection of vaccination rates prior to military service, results similarly demonstrated that Air Force members had the highest rate of vaccine initiation for males and females.Citation14 Finally, this study included only patients that had a primary care visit at a single VA in the northeast. Although it is possible that the observed trends are not generalizable to other veteran populations or that vaccination rates differed among patients that went to outside providers instead of the VA, our results support the vaccination rates presented in other studies.
Our findings highlight several areas for potential improvement in HPV vaccination rates among veterans, a high-risk population. First, the HPV vaccine should be added to the required immunization list upon military accession for patients that have not received it prior to entry. Currently, HPV is the only ACIP recommended vaccine not included in the DoD mandatory vaccination list.Citation26 Given high HPV incidence in active duty personnel, vaccination represents an important preventive measure. Second, military and VA providers should make a concerted effort to strongly recommend HPV vaccination. Lack of a strong provider recommendation has been identified as a barrier to HPV immunization.Citation27 Studies in military have demonstrated that strong recommendation by providers does result in increased vaccination rates.Citation21,Citation26 In support of these points, Buechel et al demonstrated that patients with greater knowledge of HPV vaccination and those who perceived it to be recommended by the DoD chain of command were more likely to be vaccinated. Lastly, recording and reporting of HPV vaccination both on military entry and at time of the first primary care visit to the VA should be improved. Military health records may fail to capture vaccination prior to entry or outside of military service and it remains difficult to access all DoD records once the patient is seen at the VA. Creation of a metric to ensure proper documentation of HPV vaccination within the military and upon VA appointment may help reduce gaps in documentation.
The results of this study demonstrate low HPV vaccination rates among US service members, especially in males. Furthermore, among veterans that did receive vaccination upon entering the VA, older age at initiation of vaccination in the setting of high HPV acquisition in the military puts this population at risk for reduced effectiveness in preventing HPV related diseases and cancers. Addition of HPV to the list of mandated vaccine upon accession to military service should be considered.
Patients and methods
Study population
The James J Peters Bronx VA Medical Center (VAMC) institutional Data Warehouse was queried to identify patients with at least 1 primary care visit between January 2011 and December 2017. This study period was selected to include the start of routine HPV vaccine recommendation for males.Citation4 Only patients aged at or below 26 years in 2011–2017 were included. The VAMC reviewed this project and deemed it quality improvement, exempt from full Institutional Review Board review.
Data source
Institutional data, including the local VAMC electronic medical record (Computerized Patient Record System (CPRS), and the Joint Legacy Viewer (JLV), a system which allows viewing of certain Department of Defense (DoD) and national VAMC data, were queried to identify all patients with any recorded HPV vaccination. At our VA facility, JLV is accessible through CPRS and queries DOD data as well as any other VA facility that the patient has visited. The immunization widget in JLV has all immunizations in a centralized location. It is important to note that due to inconsistencies in recording and communication between electronic health record systems, not all DoD vaccinations may appear in JLV and vaccines given prior to military service may not have been recorded. As such, we examined the immunization records and visit notes for all patients that were identified as not having received any HPV vaccination to determine whether any HPV vaccinations were documented. Dates of vaccination were abstracted from charts when available.
Vaccination
The primary outcome of interest in this study was HPV vaccine initiation rates (≥1 vaccine) overall among veterans, and site of vaccination (at the DoD or JJPVAMC). Secondary outcomes of interest included vaccination rate by gender and military branch prior to VA visit, overall vaccination rate (including VA and DoD), and age of first HPV vaccination. HPV vaccination was considered complete in patients that had documentation of having received the entire 3-dose series.
Analysis
Outcomes are presented as a percentage for categorical and median with interquartile range for continuous variables. Jointpoint Regression Program (National Cancer Institute, version 4.6.0.0) was used to calculate percent vaccinated by year of first VA visit and fit a log-linear regression model by gender and military branch. Annual percent change (APC) with p < 0.05 was considered statistically significant.
Disclosure of potential conflicts of interest
Tamar Nobel’s research is funded in part by a grant from the American Cancer Society.
Acknowledgments
The opinions expressed in this manuscript are the sole views of the authors and do not reflect those of the Veterans Affairs Medical Center.
References
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, Su J, Xu F, Weinstock H. Sexually transmitted infections among US women and men. Sex Transm Dis. 2013;40(3):187–193. doi:10.1097/OLQ.0b013e318286bb53.
- Arbyn M, Xu L, Simoens C, Martin-Hirsch PP. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. 2018;(5). doi:10.1002/14651858.CD009069.pub3.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination — updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2016;65(49):1405–1408. doi:10.15585/mmwr.mm6549a5.
- HHS, CDC, NCHHSTP. CDC FACT SHEET incidence, prevalence, and cost of sexually transmitted infections in the United States; 2008 [ accessed 2018 Sept 29]. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/sti-incidence-prevalence-cost-fact-sheet-508.pdf.
- Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — united States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–882. doi:10.15585/mmwr.mm6633a2.
- Goyal V, Mattocks KM, Sadler AG. High-risk behavior and sexually transmitted infections among U.S. active duty servicewomen and veterans. J Womens Health (Larchmt). 2012;21(11):1155–1169. doi:10.1089/jwh.2012.3605.
- Agan BK, Macalino GE, Nsouli-Maktabi H, Wang X, Gaydos JC, Ganesan A, Kortepeter MG, Sanchez JL.. Human papillomavirus seroprevalence among men entering military service and seroincidence after ten years of service. Msmr. 2013;20(2):21–24. [ Accessed 2018 Sept 24]. http://www.ncbi.nlm.nih.gov/pubmed/23461307.
- Masel J, Deiss RG, Wang X, Sanchez JL, Ganesan A, Macalino GE, Gaydos JC, Kortepeter MG, Agan BK. Seroprevalence and seroincidence of herpes simplex virus (2006-2010), syphilis (2006-2010), and vaccine-preventable human papillomavirus subtypes (2000-2010) among US military personnel. Sex Transm Dis. 2015;42(5):253–258. doi:10.1097/OLQ.0000000000000277.
- Vaccine Recommendations by AOR | Health.mil. accessed 2018 Sept 24. https://www.health.mil/Military-Health-Topics/Health-Readiness/Immunization-Healthcare/Vaccine-Recommendations/Vaccine-Recommendations-by-AOR.
- LaRocque JD, Berry-Cabán CS. Human papilloma virus vaccination coverage among soldiers in a military treatment facility, 2007-2010. J Vaccines Vaccin. 2011;02:01. Gynecologic Oncology doi:10.4172/2157-7560.1000116.
- Shen-Gunther J, Shank JJ, Ta V. GardasilTM HPV vaccination: surveillance of vaccine usage and adherence in a military population. 2011. doi:10.1016/j.ygyno.2011.07.094.
- Maktabi H, Ludwig SL, Eick-Cost A, Yerubandi UD, Gaydos JC. Quadrivalent human papillomavirus vaccine initiation, coverage, and compliance among U.S. active component service women, 2006-2011. Msmr. 2012;19(5):16. [ accessed 2018 Sept 29]. http://www.ncbi.nlm.nih.gov/pubmed/22694590.
- Kwon PO, Lay J, Hrncir D, Levin L. Missed opportunities in human papillomavirus vaccination uptake among US air force recruits, 2009-2015. US Army Med Dep J. (1–18):67–75. [ accessed 2018 Nov 24]. http://www.ncbi.nlm.nih.gov/pubmed/30165724.
- Clark LL, Stahlman S, Taubman SB. Human papillomavirus vaccine initiation, coverage, and completion rates among U.S. active component service members, 2007-2017. MSMR. 2018;25(9):9–14. [ accessed 2018 Nov 24]. http://www.ncbi.nlm.nih.gov/pubmed/30272988.
- Population Representation in the Military Services 2011. [ accessed 2018 Nov 24]. https://www.cna.org/pop-rep/2011/.
- United States Department of Defense. Demographics - Profile of the military community. 2011. https://download.militaryonesource.mil/12038/MOS/Reports/2011_Demographics_Report.pdf
- United States Department of Veterans Affairs. Demographic characteristics of veterans who separated in 2011 and 2017. [ accessed 2018 Nov 24]. https://www.data.va.gov/dataset/demographic-characteristics-veterans-who-separated-2011-and-2017.
- United States Department of Veterans Affairs. VA utilization profile FY. 2016. Department of Veterans Affairs. https://www.va.gov/vetdata/
- Department of Veterans Affairs, Veterans Health Administration, Office of Patient Care Services, Health Services P-D, Program. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans. [ Accessed 2018 Sept 29]. http://www.publichealth.va.gov/epidemiology.
- Armed Forces Health Surveillance Center. Sexually transmitted infections, active component, U.S. Armed Forces, 2000-2012. Msmr. 2013;20(2):5–10. [ accessed 2018 Sept 29]. http://www.ncbi.nlm.nih.gov/pubmed/23461303.
- Wedel S, Navarrete R, Burkard JF, Clark MJ. Improving human papillomavirus vaccinations in military women. Mil Med. 2016;181(10):1224–1227. doi:10.7205/MILMED-D-15-00477.
- Buechel JJ, Connelly CD. Determinants of human papillomavirus vaccination among U.S. Navy personnel. Nurs Res. 2018;67(4):341–346. doi:10.1097/NNR.0000000000000282.
- Han JJ, Beltran TH, Song JW, Klaric J, Choi YS. Prevalence of genital human papillomavirus infection and human papillomavirus vaccination rates among US adult men: National Health and Nutrition Examination Survey (NHANES) 2013-2014. JAMA Oncol. 2017;3(6):810–816. doi:10.1001/jamaoncol.2016.6192.
- Nsouli-Maktabi H, Ludwig SL, Yerubandi UD, Gaydos JC. Incidence of genital warts among U.S. service members before and after the introduction of the quadrivalent human papillomavirus vaccine. MSMR. 2013;20(2):17–20. [ Accessed 2018 Sept 29]. http://www.ncbi.nlm.nih.gov/pubmed/23461306.
- Schlecht NF, Diaz A, Shankar V, Szporn AH, Wu M, Nucci-Sack A, Peake K, Strickler HD, Burk RD. risk of delayed human papillomavirus vaccination in inner-city adolescent women. J Infect Dis. 2016;214(12):1952–1960. doi:10.1093/infdis/jiw486.
- Buechel J. Vaccination for human papillomavirus: immunization practices in the U.S. military. Clin J Oncol Nurs. 2018;22(1):104–107. doi:10.1188/18.CJON.104-107.
- Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–1192. doi:10.1016/j.vaccine.2016.01.023.