?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
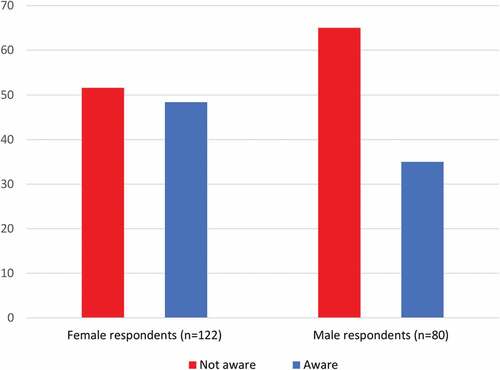
There is limited data on the HPV immunization status of Latino/Hispanic youth in the USA. In Los Angeles County in 2015, 54,973 (34.3%) college students were of Latino/Hispanic background. We examined Los Angeles County college students’ awareness of HPV and HPV-related disease, HPV vaccine recommendations, and their vaccination status. This study surveyed 212 Los Angeles college students from January to April 2018. In a convenience sampling study, a 31-question, IRB-approved survey was administered face-to-face to college students 18 years and older at California State University settings in Los Angeles County. Almost two-thirds of the male (65%) and half of the female (51.6%) respondents did not know that the HPV vaccine is recommended through 26 years of age, and 47.6% did not know they can get the HPV vaccine at the college student health center or youth-friendly clinics. Ethnicity, family income, and the highest level of education in the family had a significant impact on immunization rates. Self-reported and actual HPV knowledge levels were significantly associated with vaccination status. Educational strategies focusing on the logistics of receiving the HPV vaccine and HPV vaccine catch-up eligibility for college students may be effective in decreasing racial disparities in vaccine receipt.
Introduction
Human Papillomavirus (HPV) is the leading cause of cervical cancer, which caused 4,120 deaths among women in 2016 in the US.Citation1 Ironically, it is also the most common sexually transmitted infection, affecting up to 80% of women over their lifetime. HPV infection can also lead to genital warts as well as other types of cancers, including cancers of the oropharynx, vagina, vulva, penis, and anus. HPV infection with certain viral strains (seven high-risk types that are associated with cancers and two low-risk types that are associated with genital warts) is preventable with vaccination.Citation2,Citation3
The Advisory Committee on Immunization Practices (ACIP) at the Centers for Disease Control and Prevention (CDC), composed of 61 experts in medicine, community health, infectious diseases, health policy, and research publishes vaccine recommendations in the United States by age group, including the at-risk patient groups based on their comorbidities and contraindications.Citation4 ACIP determined the optimum age of HPV vaccination to be 11–12 years but recommended the vaccine to be administered to females through 26 years old and males up to 21 years old (26 years old in men who have sex with men (MSM)).Citation5 Therefore, there is a significant amount of time for “catch-up” if patients do not receive the complete vaccine series early on.
Studies have found that, along with women attending sexually transmitted disease (STD) clinics, college women have the highest prevalence of HPV infection.Citation6 Despite the fact that college students often have access to health resources (including immunizations) on their campuses through student health services, HPV immunization rates in college students are significantly below the US Department of Health and Human Service’s Healthy People 2020 goals.Citation7 While the Healthy People 2020 goal is for 80% of females and males to be vaccinated by 13–15 years of age, studies have found vaccination rates of lower than 60% among male and female college students.Citation8,Citation9 In addition to low HPV vaccination rates among college students, there are racial and gender disparities in HPV vaccine uptake with lower vaccination rates among college males compared to females,Citation10 and African Americans compared to whites.Citation11
Although the anti-vaccination controversy is one of the drivers for parental refusal and therefore lower immunization rates, some studies suggest that the low HPV vaccination rates among college students is also related to deficits in knowledge as well as willingness to receive the vaccine.Citation12,Citation13 While multiple studies have shown that the majority of young adult or college students are generally aware of HPV and the fact that it is sexually transmitted,Citation14–Citation16 there is a lack of more detailed understanding of the virus and its related health conditions.Citation16 For example, while it is known that nearly all men and women will contract HPV at some point in their lives,Citation17 studies have demonstrated a lack of awareness among college students regarding the prevalence of HPV and their risk of becoming infected with the virus.Citation15,Citation16,Citation18 Barnard, et al.Citation14 and Gerend, et al.Citation15 found that most college students (56% and greater than 75%, respectively) did not agree that they were at risk for HPV infection. Only 13.6% of college student respondents in a study by Sandfort, et al.,Citation16 correctly identified the prevalence of HPV acquisition among sexually active people. This study showed that many college students were unaware that the virus is transmitted through skin-to-skin contact, that condoms do not fully protect against HPV and that it is not transmitted through body fluids.Citation16 One study among minority college students demonstrated that many (20%) did not know that HPV can cause cancer.Citation18
Previous studies have demonstrated disparities in the levels of HPV knowledge among various groups of college students. For example, knowledge of HPV tends to be greater among women than men,Citation14–Citation16 with women demonstrating greater awareness of HPV transmission, HPV health risks for women, signs and symptoms of infection, and existence of a vaccine than men.Citation16
Most studies so far have focused on understanding the gaps in college students’ knowledge of HPV disease and its consequences, and HPV vaccination as a broad approach for prevention. However, there is limited data on the students’ knowledge of logistics of access to the HPV vaccine, such as where and until what age they can receive the vaccine. In this study, we examined Los Angeles County college students’ awareness of HPV disease, self-reported HPV vaccination status, and knowledge of HPV vaccination logistics, including the availability of the vaccine at college health centers/youth-friendly community clinics and until what age they can get vaccinated.
Materials and methods
Thomas et al.Citation19 developed an electronic student HPV survey (SHPVS) tool, based on Neuman’s Systems Model (NSM) and Health Belief Model (HBM), at Florida International University. Their goal was to measure young adults’ perception of the severity of HPV infection, vulnerability to HPV infection, and barriers to the completion of HPV vaccine series.
In January 2018, as a part of International HPV Coalition’s efforts to promote International HPV Day in LA County, we developed a 31-question multiple-choice survey based on SHPVS and other HPV surveys. Questions to assess the knowledge of college students on the logistics of HPV vaccination (where and until what age they can get the vaccine) were included. The study was IRB approved (WIRB No 1920852–43973015, Appendix 1).
We conducted a cross-sectional study at a Southern California state university campus. A peer-to-peer education approach was employed. A group of students at the university were trained on HPV disease and prevention as immunization community health educators (ICHE), and they administered the survey in-person to other students at various locations on the university’s campus by giving the respondents either a paper copy of the survey or link to an online version. After the survey administration, the ICHEs educated their peers on HPV disease and vaccine logistics. The survey was administered between February and April 2018. Data were collected on participant demographics, sexual history, HPV vaccination status, awareness of HPV-related conditions and CDC HPV vaccine recommendations.
All demographic variables, except for gender, were recoded to create larger categories for statistical analysis (e.g., the original six categories of the ethnicity variable were recoded to three categories, Caucasian, Hispanic and Other). Selected demographic characteristics of the study population were stratified by vaccination status. Chi-squared tests were used to detect significant associations between HPV vaccination status and demographic characteristics, self-reported and actual level of knowledge, and whether or not the participants’ health-care providers had spoken to them about the HPV vaccine (p-value < 0.05). A multivariate logistic regression model was constructed using the likelihood ratio tests. Analyses were completed using R 3.4.3.
For each of the 23 potential predictors (all 31 survey questions, except ZIP code, Q8, Q9, Q13, Q15 – Q17, Q18), we looked at the likelihood ratio test between a model with a single predictor and a model with only one intercept and selected only variables with p-value <0.25 in order to reduce the number of potential predictors.
Next, we fit a multiple logistic regression model using the 20 potential predictors and likelihood ratio test to compare nested models (including one additional variable to the reduced model to create the full model) and using a p-value < 0.05 to determine which of the two models was a better fit. Additionally, a model’s Akaike information criterion (AIC) was taken into consideration for model selection. In order to have adequate cell size for chi-squared tests to analyze the relationship between the dependent and independent variables, the students whose response was “I don’t know” when asked whether or not they received the HPV vaccine were considered “not vaccinated” (n = 102, 50.5%).
The final model includes the following variables: highest level of education in the family, yearly income, whether or not their healthcare provider had spoken to them or their parents about the HPV vaccine, and level of knowledge of HPV, HPV-related disease prevention and HPV transmission. The sensitivity (proportion of respondents correctly identified as having been or currently undergoing vaccination) of this model is 0.81 and the specificity (proportion of respondents correctly identified as being unvaccinated) is 0.7255. Adjusted odds ratio and 95% confidence intervals were calculated.
Results
Two hundred and twelve (212) individuals responded to the survey; 10 were excluded from the data analysis because of missing information. The average age of survey participants was 212.4 years old. The demographic characteristics are summarized in . Overall, 60.4% (122/202) of the respondents were female, 43.6% (88/207) were Latino/Hispanic, 91.6% (185/202) were heterosexual, 46.0% (93/202) indicated that the highest education level in their immediate family is “some college credit but no degree”, and 50.9% (103/202) indicated that their yearly family income is between $60,000 and $100,000.
Table 1. Demographic characteristics of respondents.
Forty-nine percent (49.1%) of the respondents (n = 104) indicated that they have received the HPV vaccine or are in the process of completing the series and 27.3% (n = 55) reported that they were not immunized. Fifty students (23.6%) indicated that they did not know whether or not they had received the vaccine.
At the time of the survey, 86.7% (182/210) of the respondents were sexually active. Nineteen percent (19.1%; 22/122) of the females and 2.5% (2/80) of the males reported that they have received treatment for a sexually transmitted disease (STD).
We examined the students’ self-perceived level of HPV knowledge and actual level of knowledge. The majority of the students reported that they had at least some knowledge of HPV transmission (146/202, 72.3%), HPV-related diseases (142/202, 70.3%), prevention of HPV (148/202, 73.3%) and of the HPV vaccine (144/202, 71.3%) (Supplemental Table 1). The self-reported knowledge level of HPV disease and HPV vaccine awareness (i.e. How much do you know about HPV prevention, transmission, related conditions, and vaccine?) were significantly related to the vaccination status in Chi-square analyses, with those reporting to have “some knowledge” or “a great deal of knowledge” more likely to be vaccinated than those reporting to have “no knowledge” (p < .001 for all questions).
Fifty-five percent (55%) of the students answered four or more of the seven knowledge questions (in quiz format) correctly (Supplemental Table 2). The mean composite knowledge score was 4.4 out of 7 (62%) among vaccinated versus 2.8 (40%) among unvaccinated students. None of the 12 students who had zero correct answers were vaccinated. In addition, in Chi-square analysis, not having heard of HPV was significantly associated with being unvaccinated (p < .05). Seventy-six (76.2%) of the female and 76.3% of the male respondents knew that both genders are recommended to receive the HPV vaccine. However, 52.0% of the female and 65.0% of the male respondents did not know that the HPV vaccine is recommended through 26 years of age (). A large proportion of the participants (47.6%) were unaware that HPV vaccination is provided by their student health clinic or local, youth-friendly clinics.
In logistic regression model analysis, self-perceived or actual level of HPV knowledge did not influence the self-reported immunization status. Age and gender had no statistically significant impact, but the ethnicity, highest level of education in the family and income correlated with the self-reported HPV immunization status (). Hispanic/Latino respondents were significantly less likely to be vaccinated than Caucasian and Other ethnicities (40.9% versus 62.7% and 50.8%; p = .01). Those with higher levels of education in the family (some college degree or less) or those with higher family incomes (≥ $60K) were more likely to be vaccinated (). Interestingly, those who reported the highest level of education in their family as masters, professional or doctorate degree were 27.3% less likely to be immunized than students with the highest level of education in their family being some college credit (no degree) or trade/technical/vocational training (). Sexual history, including age of sexual debut, number of sexual partners, or history of STD treatment had no impact on the rate of self-reported HPV immunization status (Supplemental Table 3).
Table 2. Logistic regression analyses of the factors influencing the rate of self-reported HPV immunization.
Finally, healthcare provider (HCP) communication on the HPV vaccine was significantly associated with being vaccinated; 74.0% (74/100) of the vaccinated and 24.5% (25/102) of the unvaccinated students reported that their HCP has spoken to them or their parents about the HPV vaccine (p < .001).
Discussion
This study examined the self-reported HPV vaccination rates and knowledge of HPV disease, prevention and vaccine logistics among Los Angeles County college students in 2018. We found that close to one-third of the responding college students were not immunized. Surprisingly, one-quarter of the responding students did not know their immunization status. Though 49.1% of respondents in our study reported to have received the vaccine, a rate higher than the rate reported in other studies of college students,Citation11 it is still well below the US Department of Health and Human Services’ 2020 objective, which is for 80% of females and males to be vaccinated by age 13–15 years.Citation7
We found that respondents who were Hispanic (compared to non-Hispanic), with lower family income or lower level of education in the immediate family, were significantly less likely to be vaccinated against HPV. Previous studies have also demonstrated income as a predictor of HPV vaccination,Citation20 and studies on the effects of social determinants of health on HPV vaccination found that higher vaccination uptake correlated with low worry about vaccine cost and having health insurance.Citation21,Citation22 Our finding on education level as another predictor of vaccination status may reflect the fact that lower level of education is often a root cause of lower income.
Cohen, et al.Citation23 demonstrated that the HPV vaccination rate is lower for Hispanic women in college compared to the rate for white women in college, a finding corroborated by our study. Lower vaccination rates among Latinos may reflect some Latino parents’ concerns that HPV vaccination will lead to premarital sexual activity, which have been shown to be a barrier to vaccination, although recent studies and our data indicate that HPV vaccination is unrelated to the age of sexual debut or sexually risky behavior.Citation20,Citation24
While many investigators have studied HPV vaccination among Latino/Hispanic youth,Citation15,Citation25,Citation26 those studies focus mostly on high-risk male populations or Hispanic populations in the Southeast United States. The country of origin profile of Latinos in the Southeast USA is different than that in the Southwest. For example, the largest group of Latino individuals in Los Angeles, California are from Mexico, followed by El Salvador and Guatemala, whereas in Miami, Florida the largest group reports origins from Cuba, followed by Colombia and Puerto Rico.Citation27 Among US Latinos, based on the county of origin, there are socioeconomic, cultural and demographic differences that may influence health literacy, health beliefs, and behaviors. Los Angeles County is also unique because according to the Pew Research Center 2014 American Community Survey, the Hispanic population makes up 49% of the total population and it has the largest share of Hispanics among those under 18 years of age (58.6%).Citation27
Previous studies have also addressed HPV prevalence, vaccination rates, and knowledge among men. Men have a higher prevalence of HPV compared to females, with the highest prevalence between the ages of 25 and 29 years.Citation28 Lee et al.Citation9 utilized the 2015 College Student Health Survey to analyze HPV vaccination behaviors of 2,516 male college students and showed that 54.5% of male respondents between 18 and 20 years of age and 45.5% of those between 21 and 26 years of age reported that they had received the complete HPV vaccine series (p < .001). Thompson et al.Citation10 reported that older men aged 22–26 years were less likely to be immunized than younger men and that non-Hispanic Blacks had the lowest rate of increase in HPV vaccination rate over time. Cooper et al.Citation29 recently conducted a survey study in a large Southeastern university in the USA and observed that although half of the male students were sexually active and most knew about HPV, 71% did not intend to get vaccinated. In our study, the average age of students was 21 ± 2 years, and 36.9% were male with a self-reported HPV immunization rate of 45%. This rate is similar to that reported by Lee et al. and is not significantly different from the rate observed in female students in this study. However, only 35% of the male students were aware that they could get the HPV vaccine through 26 years of age.
Racial disparities in HPV infection have been found. Black men have been shown to have the highest HPV prevalence compared to other groups.Citation30 The rates of penile cancers are higher in blacks compared with whites and among Hispanics compared to non-Hispanics. In addition, HPV-associated anal and rectal cancers are higher in black men compared to white men.Citation31
Previous studies have examined racial disparities in HPV knowledge. A recent study found that HPV knowledge and awareness was significantly lower among black women than white women 18 years and older,Citation32 and another study found that Hispanic and non-Hispanic black women were less aware of HPV infection and vaccination, and were also less likely to report having been vaccinated, than non-Hispanic white women.Citation33 In our study, 75% of the respondents reported to belong to a minority group and less than 10% reported to have a great deal of knowledge of HPV transmission (9%), HPV-related conditions (7%), HPV prevention (8%) and the HPV vaccine (6%).
Education on HPV infection may help improve immunization rates. In our study, respondents with a higher self-perceived or actual knowledge level of HPV were more likely to be vaccinated. Earlier papers have shown conflicting results in terms of the association between HPV knowledge and vaccination status. While some have shown that HPV knowledge and awareness of college students correlate with having received the vaccine,Citation10 others have shown that knowledge was not correlated with HPV vaccination status, but instead, with subjective norms (complying with the expectations of others such as doctors’ recommendations, peers’ or mothers’ wishes) and lower perceived behavioral control.Citation34,Citation35 LaJoie et al.Citation36 examined the factors associated with HPV immunization among University of Louisville students in Kentucky, and observed that parental influence (aOR = 5.32, 2.71–13.03), strong preference for the respondent’s partner to be vaccinated (aOR = 4.04, 95% CI: 2.31–7.05) and having access to a free vaccine (aOR 1.90, 1.05–3.41) increased the likelihood of being vaccinated.Citation36 In our study, we did not focus on the role of society’s influence on youth to get vaccinated but rather focused on the knowledge of logistic factors.
Previous studies have focused on college students’ general lack of knowledge of prevalence of HPV and modes of HPV transmission and prevention.Citation14–Citation16,Citation18 A recent cross-sectional survey of 256 undergraduate students from University of South Carolina showed that college students had limited knowledge of the prevention, symptoms, and consequences of HPV infection. The investigators proposed that college health professionals may help to increase student HPV awareness and vaccination.Citation37
College health centers have been proposed to play a role in improving HPV immunization rates. A recent study from the University of Utah showed that a computer-automated electronic medical record provider alert for eligible male patients improved the HPV immunization rate for male students visiting the college health center.Citation38 There is limited data on whether the students are aware of the availability of HPV vaccine in this setting. Omer et al.Citation39 conducted a survey study among 527 undergraduate students at an urban private religious-affiliated and a rural public university in Georgia and found that approximately one-third of the students did not know where to get the HPV vaccine. In our study, almost half of the students (48%) did not know that they can get the HPV vaccine at the college health center. Most 4-year colleges (including the university from which students were surveyed; personal communication) stock and administer the HPV vaccine.Citation40 The lack of college student knowledge about this resource highlights the need to better publicize the HPV vaccination-related services offered by college health centers. The HPV vaccine is also available to California youth at community clinics and retail pharmacies; however, most responding students in our study were unaware of this availability. There is a need to inform youth about the logistics of healthcare resources as they are transitioning into adulthood.
The majority of responding students in our study were unaware that the HPV vaccine is recommended for women and men through 26 years of age. This may reflect a misconception that the vaccine is only administered to younger individuals. These gaps in knowledge may explain why many college students are not asking for the vaccine and should guide future efforts to increase vaccination rates among this population.
Strong recommendation from a healthcare provider (HCP) has been shown to be the most effective communication strategy to improve HPV vaccine uptake.Citation41 Similarly, in our study, vaccinated students were more likely to have had their HCP speak to them or their parents about the HPV vaccine. Interestingly, almost one-quarter (23.6%) of the college students in our study did not know their immunization status, demonstrating a lack of communication between the provider and these patients. This suggests that there is a need for a formal health status communication as young adults are transitioning from pediatric to adult medicine.
Limitations of the study include small sample size, limited geographic distribution and subjective responses to the survey questions. The strengths of the study are that it was conducted in a setting with a large Latino/Hispanic population, its peer-to-peer format allowed culturally and linguistically competent data collection, and its study design allowed the capture of information from the general college student community rather than only those who are interested in HPV or clinical research.
Disclosure of potential conflicts of interest
The authors report no conflicts of interest.
Supplemental Material
Download MS Word (40.2 KB)Acknowledgement
The authors thank Dr. Anna-Barbara Moscicki, Professor of Pediatrics at UCLA, Division Chief of Adolescent and Young Adult Medicine, and Associate Vice Chair of Clinical Research at UCLA School of Medicine for her guidance on the development of this manuscript.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016: cancer Statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi:10.3322/caac.21332.
- Joura EA, Giuliano AR, Iversen O-E, Bouchard C, Mao C, Mehlsen J, Moreira ED, Ngan Y, Petersen LK, Lazcano-Ponce E, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med. 2015;372:711–23. doi:10.1056/NEJMoa1405044.
- Giuliano AR, Palefsky JM, Goldstone S, Moreira ED, Penny ME, Aranda C, Vardas E, Moi H, Jessen H, Hillman R, et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N Engl J Med. 2011;364:401–11. doi:10.1056/NEJMoa1007994.
- Centers for disease control and prevention. ACIP Members November 27, 2017 - June 30, 2018. Atlanta, Georgia: Centers for Disease Control and Prevention; 2018. https://www.cdc.gov/vaccines/acip/committee/charter.html
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination — updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405–08. doi:10.15585/mmwr.mm6549a5.
- Revzina NV, DiClemente RJ. Prevalence and incidence of human papillomavirus infection in women in the USA: a systematic review. Int J STD AIDS. 2005;16:528–37. doi:10.1258/0956462054679214.
- Healthy People. Immunization and infectious diseases. Atlanta, Georgia: Centers for Disease Control and Prevention; 2020.
- Lindley LL, Elkind JS, Landi SN, Brandt HM. Receipt of the human papillomavirus vaccine among female college students in the United States, 2009. J Am Coll Health. 2013;61:18–27. doi:10.1080/07448481.2012.750607.
- Lee HY, Lust K, Vang S, Desai J. Male Undergraduates’ HPV vaccination behavior: implications for achieving HPV-associated cancer equity. J Community Health. 2018;43:459–66. doi:10.1007/s10900-018-0482-4.
- Thompson EL, Vamos CA, Vázquez-Otero C, Logan R, Griner S, Daley EM. Trends and predictors of HPV vaccination among U.S. College women and men. Prev Med. 2016;86:92–98. doi:10.1016/j.ypmed.2016.02.003.
- Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sex Transm Infect. 2010;86:74–78. doi:10.1136/sti.2009.037705.
- Daley EM, Vamos CA, Buhi ER, Kolar SK, McDermott RJ, Hernandez N, Fuhrmann HJ. Influences on human papillomavirus vaccination status among female college students. J Womens Health. 2010;19:1885–91. doi:10.1089/jwh.2009.1861.
- Navalpakam A, Dany M, Hajj Hussein I. Behavioral perceptions of Oakland University female college students towards human papillomavirus vaccination. PLoS One. 2016;11:e0155955. doi:10.1371/journal.pone.0155955.
- Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: implications from the precaution adoption process model. PLoS One. 2017;12:e0182266. doi:10.1371/journal.pone.0182266.
- Gerend MA, Magloire ZF. Awareness, knowledge, and beliefs about human papillomavirus in a racially diverse sample of young adults. J Adolesc Health. 2008;42:237–42. doi:10.1016/j.jadohealth.2007.08.022.
- Sandfort JR, Pleasant A. Knowledge, attitudes, and informational behaviors of college students in regard to the human papillomavirus. J Am Coll Health. 2009;58:141–49. doi:10.1080/07448480903221368.
- Centers for Disease Control and Prevention. What is HPV? Atlanta, Georgia: Centers for Disease Control and Prevention; 2019.
- Jones SG, Mathis-Gamble K, Fenkl EA. Minority college students’ HPV knowledge, awareness, and vaccination history. J Assoc Nurses AIDS Care. 2017;28:675–79. doi:10.1016/j.jana.2017.04.008.
- Thomas T, Dalmida S, Higgins M. The student human papillomavirus survey: nurse-led instrument development and psychometric testing to increase human papillomavirus vaccine series completion in young adults. J Nurs Meas. 2016;24:226–44. doi:10.1891/1061-3749.24.2.226.
- Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13-17 years - United States. Atlanta, Georgia: Centers for Disease Control and Prevention; 2011.
- Gerend MA, Zapata C, Reyes E. Predictors of human papillomavirus vaccination among daughters of low-income Latina mothers: the role of acculturation. J Adolesc Health. 2013;53:623–29. doi:10.1016/j.jadohealth.2013.06.006.
- Morales-Campos DY, Parra-Medina D. Predictors of human papillomavirus vaccine initiation and completion among Latino mothers of 11- to 17-year-old daughters living along the Texas-Mexico border. Fam Community Health. 2017;40:139–49. doi:10.1097/FCH.0000000000000144.
- Cohen TF, Legg JS. Factors associated with HPV vaccine use among Hispanic college students. J Allied Health. 2014;43:241–46.
- Rohde RL, Adjei Boakye E, Christopher KM, Geneus CJ, Walker RJ, Varvares MA, Osazuwa-Peters N. Assessing university students’ sexual risk behaviors as predictors of human papillomavirus (HPV) vaccine uptake behavior. Vaccine. 2018;36:3629–34. doi:10.1016/j.vaccine.2018.05.022.
- Thomas TL, Stephens DP, Johnson-Mallard V, Higgins M. Young hispanic men and human papillomavirus vaccination choices. J Transcult Nurs. 2016;27:103–08. doi:10.1177/1043659614526759.
- Fernandez ME, McCurdy SA, Arvey SR, Tyson SK, Morales-Campos D, Flores B, Useche B, Mitchell-Bennett L, Sanderson M. HPV knowledge, attitudes, and cultural beliefs among Hispanic men and women living on the Texas-Mexico border. Ethn Health. 2009;14:607–24. doi:10.1080/13557850903248621.
- Pew Research Center. Hispanic population and origin in select U.S. metropolitan areas. Washington, DC: Pew Research Center; 2014.
- Lewis RM, Markowitz LE, Gargano JW, Steinau M, Unger ER. Prevalence of genital human papillomavirus among sexually experienced males and females aged 14–59 years, United States, 2013–2014. J Infect Dis. 2018;217:869–77. doi:10.1093/infdis/jix655.
- Cooper DL, Zellner-Lawrence T, Mubasher M, Banerjee A, Hernandez ND. Examining HPV awareness, sexual behavior, and intent to receive the HPV vaccine among racial/ethnic male college students 18-27 years. Am J Mens Health. 2018;12:1966–75. doi:10.1177/1557988318803163.
- Gargano JW, Unger ER, Liu G, Steinau M, Meites E, Dunne E, Markowitz LE. Prevalence of genital human papillomavirus in males, United States, 2013–2014. J Infect Dis. 2017;215:1070–79. doi:10.1093/infdis/jix057.
- Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, Razzaghi H, Saraiya M. Human papillomavirus–associated cancers — United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2016;65:661–66. doi:10.15585/mmwr.mm6526a1.
- Ojeaga A, Alema-Mensah E, Rivers D, Azonobi I, Rivers B. Racial disparities in HPV-related knowledge, attitudes, and beliefs among African American and White Women in the USA. J Cancer Educ. 2019;34:66–72. doi:10.1007/s13187-017-1302-8.
- Ford JL. Racial and ethnic disparities in human papillomavirus awareness and vaccination among young adult women: racial and ethnic disparities in HPV awareness and vaccination. Public Health Nurs. 2011;28:485–93. doi:10.1111/j.1525-1446.2011.00958.x.
- Ratanasiripong NT. Factors related to Human Papillomavirus (HPV) vaccination in college men. Public Health Nurs. 2015;32:645–53. doi:10.1111/phn.12198.
- Ratanasiripong NT, Cheng A-L, Enriquez M. What college women know, think, and do about human papillomavirus (HPV) and HPV vaccine. Vaccine. 2013;31:1370–76. doi:10.1016/j.vaccine.2013.01.001.
- LaJoie AS, Kerr JC, Clover RD, Harper DM. Influencers and preference predictors of HPV vaccine uptake among US male and female young adult college students. Papillomavirus Res. 2018;5:114–21. doi:10.1016/j.pvr.2018.03.007.
- Kasymova S, Harrison SE, Pascal C. Knowledge and awareness of human papillomavirus among college students in South Carolina. Infect Dis Res Treat. 2019;12:117863371882507.
- Martin S, Warner EL, Kirchhoff AC, Mooney R, Martel L, Kepka D. An electronic medical record alert intervention to improve HPV vaccination among eligible male college students at a University Student Health Center. J Community Health. 2018;43:756–60. doi:10.1007/s10900-018-0480-6.
- Ragan KR, Bednarczyk RA, Butler SM, Omer SB. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: identifying health decision-making behaviors and uptake barriers. Vaccine. 2018;36:331–41. doi:10.1016/j.vaccine.2017.07.041.
- Habel MA, Coor A, Beltran O, Becasen J, Pearson WS, Dittus P. The state of sexual health services at U.S. Colleges and Universities. J Am Coll Health. 2018;66:259–68. doi:10.1080/07448481.2018.1431896.
- Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34:1187–92. doi:10.1016/j.vaccine.2016.10.045.
Appendix 1.
Data elements collected in HPV awareness survey
Age
Zip code
Gender
Ethnicity
Sexual orientation
Highest education level in immediate family (parents)
Average yearly income (theirs or their family’s)
Sexual history (if they have had intercourse/oral sex, age of first sexual activity, number of sexual partners, received treatment for STD)
If they have received the HPV vaccine
If they have a condition like lupus, arthritis or thyroid disease that requires them to take immune-suppressing medications like prednisone
If their doctor has spoken to them/their parents about the vaccine
How they learned about the vaccine
What they do to protect themselves against HPV
If they have experienced genital warts
If they have received a pap smear
If they have received a diagnosis of abnormal cervical cells
If they have been diagnosed with cervical cancer
If they have been diagnosed with cancers of the throat, vagina, vulva, penis, anus, or rectum
If their family members have been diagnosed with cervical cancer
If their family members have been diagnosed with cancers of the throat, vagina, vulva, penis, anus, or rectum
Level of knowledge of HPV and HPV-related disease prevention
Knowledge of how females can protect themselves against cervical cancer
Level of knowledge of HPV transmission
How they think HPV is transmitted
Level of knowledge of HPV-related conditions and diseases
What diseases they think HPV can cause
Level of knowledge of HPV vaccine
Who they think the vaccine is recommended for
If they think people with poor immune systems are at higher risk for HPV-related cancers
If they know that the vaccine is recommended for women and men between the ages of 9 and 26 years
If they know that they can get the HPV vaccine at the college student health center or youth-friendly clinics