ABSTRACT
This study aimed to assess the seasonal influenza vaccine (SIV) coverage rate, and to assess knowledge, attitudes, and practice of health-care workers (HCWs) concerning the SIV. In this multicenter cross-sectional study conducted in Qassim region, Saudi Arabia, a validated questionnaire was distributed randomly among HCWs. Of 523 responses from HCWs across different institutions, 282 (53.9%) respondents were females and most respondents were aged between 30 and 39 years. Overall, 48.6% of participants had been regularly vaccinated with the SIV, and 70% were willing to be vaccinated in the coming season. Reasons for HCWs’ non-adherence to the SIV included their having previously had influenza, which was not severe (20.7%), and that they were young and healthy (19.2%). Belief in the effectiveness of the SIV (72.3%) and knowledge that the SIV should be administered yearly (86.6%) was high among respondents. Less than 50% of respondents believed that vaccine safety concern is the main barrier preventing health-care institutions from providing the SIV to patients. Our study results showed suboptimal SIV coverage among HCWs in Qassim region. Educational programs and campaigns regarding the risk of influenza infection, as well as the provision of adequate information, and highlighting the importance of HCWs being vaccinated are essential. Easy access to and availability of the SIV in each region is crucial for improved vaccine coverage. Health-care institutions need to more actively encourage staff to undergo influenza vaccinations on a regular basis, especially during the influenza season.
Introduction
Seasonal influenza is one of the most common vaccine-preventable diseases in the world. Influenza infection can be serious and life-threatening in some patients such as young children (<2 years of age), elderly people (>65 years), pregnant women, patients with chronic cardiac or respiratory disease, and immunocompromised patients. Most influenza infection complications are related to the respiratory system, although neurological and cardiac complications have been reported.Citation1 Worldwide, mortality has been reported to be approximately between 290,000 and 640,000 deaths annually due to severe influenza infection.Citation2 The seasonal influenza vaccine (SIV) was first developed in 1933, and year-to-year effectiveness differs; however, vaccine effectiveness has been reported to reach up to 60%. The United States Flu Vaccine Effectiveness Network estimated vaccine effectiveness from 2004 to 2018, and reported effectiveness to range from 10% to 60%, with a mean effectiveness of 41%.Citation3 The World Health Organization (WHO) declared that the H1N1 influenza pandemic in 2009 had involved more than 208 countries and led to >250,000 deaths.Citation4 Health-care workers (HCWs) are at a more significant risk of influenza infection than the general population; therefore, the Centers for Disease Control and Prevention (CDC), the Advisory Committee on Immunization Practices (ACIP), and the Saudi Ministry of Health (MOH) have recommended that HCWs receive an SIV. In most countries, despite health authorities’ recommendations for SIV, suboptimal vaccine coverage in the general population and among HCWs persists. In the Middle Eastern and North African (MENA) countries, for example, in Lebanon, vaccine coverage remains low, at approximately 6%. Reasons for low vaccine coverage have been reported to include lack of influenza awareness, political and cost issues, and limited collaboration between private and governmental hospitals.Citation5,Citation6
The importance for HCWs vaccination is not only to prevent them from becoming ill but also to avoid the spread of infection to the patients and the community. Vaccine coverage among HCWs is low, at approximately 30%, and declining in some European countries whereas, in the United States, vaccine coverage has been reported to be approximately 78%. The higher coverage rate in the USA may be due to mandatory vaccination requirements in some health-care centers.Citation7,Citation8
In our study of HCWs in Saudi Arabia, SIV coverage among HCWs was found to range from 38% to 88%. Some HCWs indicated concerns in regard to the effectiveness and safety of the SIV, which made them hesitant to proceed with a SIV. Moreover, a lack of awareness of the Saudi Arabian Health Authority’s recommendations, and unavailability of the vaccine were other reasons given for not receiving the SIV. In Saudi Arabia, injectable trivalent influenza vaccine (TIV) is the vaccine that has been offered via Ministry of health in 2017–2018 seasons. There are few studies conducted to assess the knowledge, attitudes, and practices of HCWs toward vaccine use in Saudi Arabia; however, no study has been conducted in the Qassim region.Citation9–Citation15
Identifying barriers and HCWs’ concerns in regard to the SIV is essential to increase their awareness of the vaccine’s importance. This study aimed to assess the SIV coverage rate among HCWs as well as the knowledge, attitudes, and practices of HCWs regarding the SIV.
Materials and methods
Study design and setting
This multicenter cross-sectional study was conducted using a self-administered questionnaire, between May 2018 and July 2018. The study population comprised HCWs (doctors, nurses, pharmacists, dietitians, laboratory personnel, physical therapists, occupational therapists, respiratory therapists, and radiology technologist) working in Qassim region, Saudi Arabia. Interns and medical students were excluded from the study.
Sampling
In total, 12,900 HCWs work in Qassim region across the region’s primary health-care centers (PHC) and secondary and tertiary hospitals. A multistage random sampling technique was used for participant selection. We included all hospitals and PHCs in Qassim region derived from an official Saudi MOH list of health-care centers. Using a computer-generated simple random sampling technique, we selected 30 of 201 hospitals and PHCs from different areas in the Qassim region. A convenience sampling approach was used to select participants from among the HCWs. Six data collectors (4th and 5th year medical students) distributed 600 anonymous self-administered printed questionnaires.
Questionnaire
The questionnaire collection was undertaken on the same day and the study objectives were explained to the participants, with emphasis on the importance of the data and confidentiality. Participant consent was received prior to completion of the questionnaire.
The questionnaire was adopted from Alshammari et al.’s 2014 study, with some modifications.Citation11 The questionnaire was validated in two steps. First, it was revised by three faculty members with clinical and research experience. Second, following a pilot study with a sample size of 30 HCWs who were not included in this study, minor Arabic and English language modifications were made.
Ethics
The Qassim Ethical Committee reviewed and approved this study.
Statistical analysis
The data were password-protected, and confidentiality of all data was ensured. To obtain a proportion of 0.05 among the targeted population with definite characteristics, at a Z-statistical value of 1.96 and a significance level of 0.05, the required sample size was N = 384, based on the formula: N = z2pq\d2.
The questionnaire included five main sections. In the first section, participant demographic data comprising characteristics such as age, sex, nationality, professional title, specialty, and place of work within the Qassim region were included. The second section concerned participants’ attitudes toward the SIV, with questions in relation to whether participants annually underwent an SIV, and the reasons for not undertaking to receive an SIV. The third section assessed the participants’ knowledge concerning influenza virus transmission, the frequency of having an SIV, vaccine risks, and vaccine effectiveness. The fourth section questioned the participants on practices at their workplace and on their interest in training, in relation to SIVs. The last section explored participant awareness of CDC, ACIP, and Saudi MOH SIV recommendations, the clinical manifestations of influenza infection, and risks associated with influenza infections in HCWs.
Statistical analysis was performed, data were transferred to a Microsoft Excel spreadsheet and, after data cleaning and coding, data were exported to the Statistical Packages for Social Sciences (SPSS) version 20 for further tabulation. Descriptive and inferential statistical analyses were performed, and all categorical variables were presented as numbers and percentages. A p-value of 0.05 (95% confidence interval) was used to determine statistical significance. The statistical analyses measured the relationship between socio-demographic characteristics and knowledge, attitudes, practices, and awareness in relation to the SIV, using the Mann–Whitney U-test and the Kruskal–Wallis test. Normality tests were also conducted using the Shapiro-Wilk and the Kolmogorov–Smirnov tests to determine whether the distribution of data followed a normal distribution pattern. Based on the results, all data that were not normally distributed were deemed to be non-parametric data.
To evaluate the HCWs’ knowledge of the SIV, three questions were included and each positive response scored 1 point, while a negative response was scored as 0. The total score was calculated through adding the scores for all three questions (minimum score, 0; maximum score, 3). A maximum score of 2–3 indicated good knowledge while a minimum score of 0–1 indicated poor knowledge.
Assessment of HCWs’ attitudes to the SIV was determined using three questions, which we categorized as 1 point for the most appropriate response, and the total score was calculated through adding the scores for all three questions (minimum score, 0; maximum score, 3). A maximum score of 2–3 indicated a positive attitude, while a minimum score of 0–1 indicated a negative attitude.
The measurement of practices of HCWs in relation to SIVs, which involved 10 questions, was undertaken through scoring each appropriate response as 1 point, and an inappropriate response as 0, and the total score was calculated through adding the scores for all 10 questions (minimum score, 0; maximum score, 10). A score range of 6–10 signified good practices while a score range of 0–5 signified poor practices.
The measurement of HCWs’ awareness of the SIV, involving 14 questions, was undertaken through scoring each correct response as 1 point, and each incorrect response scored 0 points. The total score was calculated through adding the scores for all 14 questions (minimum score, 0; maximum score, 14). A score range of 8–14 was considered as good awareness whereas a score range of 0–7 was considered as poor awareness.
Results
Of the 600 questionnaires distributed, 523 responses were collected from HCWs (87% response rate) who were subsequently voluntarily enrolled into this study, of whom 282 (53.9%) were females and 241 (46.1%) were males. Most respondents were aged 30–39 years, with 196 (37.5%) aged <30 years old, while 118 (22.6%) were aged ≥40 years. More than half (51.1%) of the respondents were of Saudi Arabian nationality. Most respondents were nurses (44.9%), followed by doctors (28.3%), pharmacists (8.8%), laboratory specialists (7.8%), radiology technologist (2.7%), and other medical professionals (7.5%) such as physical, occupational, and respiratory therapists. Approximately 80% of the respondents were working at hospitals while 18.5% worked in PHCs, as shown in .
Table 1. Participants’ socio-demographic variables.
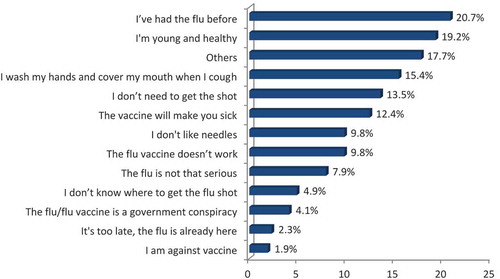
Overall, 48.6% of the respondents were vaccinated annually, and 70.0% were willing to receive flu vaccination for the coming season. Most respondents (72.3%) considered that the SIV was effective in preventing influenza, 84.1% were aware that the CDC recommended HCWs receive an SIV, while a high number (86.6%) knew that the SIV should be administered every year (). Reasons for non-adherence to receiving an SIV are shown in .
Table 2. HCWs’ knowledge and attitudes concerning the SIV.
shows the practices of HCWs in relation to the SIV. Most respondents (67.9%) believed that administering the SIV should be made mandatory in clinical practice. Most respondents (75.1%) considered that the main reason for promoting the SIV was to prevent HCWs’ exposure to influenza via patients with influenza. Only 26.2% of respondents had participated in training or continuing education concerning the SIV in the previous 12 months; however, most (62.1%) were interested in participating in SIV-related training. Moreover, >65% of the HCWs considered that PHCs or hospitals offered the SIV to their patients or stated that their center had standing supply orders for the SIV.
Table 3. HCWs practices concerning the SIV.
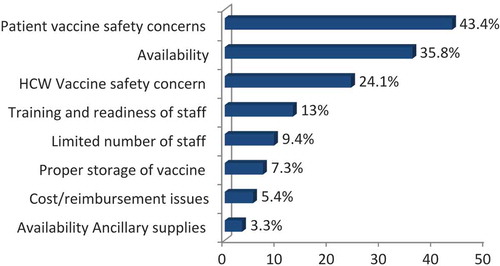
In total, 43% of the HCWs considered the main barrier preventing their institution from providing patients with an SIV was due to patient safety concerns. Other reasons concerned SIV availability (35.8%), vaccine safety concerns among the HCWs (24.1%), training and staff preparedness (13.0%), the limited number of staff (9.4%), appropriate SIV storage (7.3%), cost/reimbursement issues (5.4%), and the availability of ancillary supplies (3.3%),as shown in .
Figure 2. Distribution of the barriers to provision of the SIV in health-care institutions (N = 523).
shows HCW awareness concerning the SIV. In total, 51.4% of the respondents were not aware of the ACIP/CDC guidelines regarding the SIV. Approximately 78% of the HCWs stated that influenza was more serious than a common cold, and 92% were aware of influenza symptoms. Additionally, 91.8% of the respondents were aware that influenza could be spread via coughing and sneezing, 63.9% of the respondents considered that the HCWs could transmit infection even when feeling well, while 51.4% recommended that children aged >6 months should receive an annual SIV.
Table 4. HCWs’ awareness of influenza and the SIV.
Both male and female HCWs had good SIV knowledge levels as well as negative attitudes toward the SIV. We found that both knowledge of the SIV (p < .001) and attitudes in relation to the SIV correlated statistically (p < .001), while practices and awareness had no significant correlation. All three age groups revealed good knowledge categories, while those aged <30 years, 30–39 years, and ≥40 years had positive and negative attitudes. Nonetheless, the professional groups involved showed a statistically significant difference in knowledge (p < .001), attitudes (p < .001), practices (p < .001), and awareness (p = .004). All three age group categories had poor practices as well as poor awareness levels. Statistical tests revealed that both knowledge (p = .003) and attitudes (p < .001) differed significantly between the groups while both practices and awareness showed no correlation ().
Table 5. The correlation between knowledge, attitudes, practices, and awareness versus the socio-demographic characteristics of HCWs concerning the SIV (N = 523).
Discussion
Influenza is one of the most common vaccine-preventable diseases in the world and has a significant impact on public health. HCWs should prioritize vaccinations, not only to prevent illness in themselves, with a consequent inability to undertake their work, but also to prevent the spread of infection to patients. This study aimed to explore the SIV coverage rate among HCWs, as well as the knowledge, attitudes, and practices of HCWs in Qassim region, Saudi Arabia.
To determine the prevalence of confirmed H1N1 cases in both clinical and non-clinical HCWs, Balkhy et al. (2010) studied the epidemiological study of H1N1 influenza among HCWs in Saudi Arabia. Among HCWs, they reported an SIV adherence rate of 46.2%, which was two times higher than for non-clinical HCWs. They also reported an H1N1 virus attack rate of 6.0% among clinical HCWs and 4.3% among non-clinical HCWs. This finding confirmed the higher risk of influenza infection among HCWs especially the frontline HCWs.Citation15
Alshammari et al. reported that only 38% of HCWs received the SIV in the 2012 influenza season in Riyadh while, in another study from the same location in 2016, a similar SIV prevalence rate (50.5%) was obtained, with a slightly lower proportion (42.5%) of participants willing to receive another SIV in the coming season.Citation10,Citation11 Furthermore, in the eastern region of Saudi Arabia, the SIV prevalence rates were found to be similar (34.4% and 41.0%, respectively).Citation13,Citation14 Our study results showed that a (48.6%) of HCWs had been vaccinated against the SIV, we observed that the pattern of SIV compliance is increasing with time in Saudi Arabia and This is reflecting the Saudi Arabian Health Authority efforts to optimize SIV coverage.
In 2015, Haridi et al.Citation12 reported a high SIV vaccination rate (88.3%) in the western region of Saudi Arabia; however, they obtained a 20% higher rate than in the previous season.Citation12 This increase in vaccine coverage was because the SIV was made mandatory for participation in pilgrimages, with financial and non-financial incentives. In our study, 70% of the HCWs planned to receive the SIV prior to the coming season (2019), which is similar to increased compliance with SIV rates found throughout Saudi Arabia.
The SIV prevalence rates for HCWs in Gulf countries have been significantly different compared to those of other countries. In the United Arab Emirates, Kuwait, and Oman, SIV prevalence rates among HCWs have been reported to be 24.7%, 67.2%, and 46.4%, respectively.Citation16 In some European countries, SIV prevalence rates among HCWs have been reported to be generally low (Spain, 55.3%; Italy, 10.4%; Germany, 25%).Citation17–Citation20 In the United States, the rates of SIV adherence were higher than those reported in our study (United States, 78%).Citation8 The higher SIV rate in the United States could be because the health authorities have mandatory vaccination for HCWs. However, some experts prefer persuasion as an alternative to mandatory SIV.Citation21 In our study, 67.9% of the respondents considered that the SIV should be mandatory for HCWs to improve the vaccine coverage rate.
The CDC, the WHO, and the Saudi MOH strongly recommend the use of the SIV for HCWs. However, most of the HCWs in Saudi Arabia and some of the Gulf countries have been reported as being unaware of this recommendation.Citation16 In our study, nearly 50% of the respondents were unaware of the official recommendations concerning the SIV, and 20% were not aware if their institution provided SIVs. This suggests that there should be more focused attention on ensuring more effective SIV implementation and providing robust strategies to ensure better awareness concerning the current SIV recommendations.
To improve the SIV compliance, 67.9% of the participants in our study believed that SIV should be mandatory for clinical practice. Mandatory SIV is one of the strategies which have been applied for some health care centers at United States and Australia, which has increased SIV uptake to 90%. The mandatory SIV strategy has been endorsed by CDC and the Society for Healthcare Epidemiology (SHEA) to improve the SIV compliance for HCWs. On the other hand, some experts believed that using the soft power and further education to HCWs will increase the compliance without need for mandatory SIV.Citation21,Citation22
The main reasons given for receiving the SIV were found to be similar to those of previous studies, such as ‘to avoid illness’ or ‘to avoid the spread of the influenza virus’. In our study, 72.3% of the respondents considered an SIV to be effective in preventing influenza, 84.3% were in agreement with CDC recommendations concerning the SIV, and 86.6% were aware that SIVs should be administered annually. The main reasons given for HCW non-adherence to the SIV were that the respondents had previously contracted influenza and that they considered it not to be a severe illness (20.7%), followed by their being young and healthy and not requiring this vaccination (19.2%). These reasons differed from those provided in other published articles concerning the SIV in Saudi Arabia.Citation9–Citation14
Non-adherent HCWs appeared not to be aware that the SIV contained various subtypes of the influenza virus (one subtype of influenza B and two subtypes of influenza A); hence, their belief that the SIV was unnecessary if they had previously had influenza. Additionally, despite the high percentage of respondents who considered the SIV to be effective and knew of the health authorities’ recommendation, vaccination coverage remained suboptimal. Furthermore, most participants in our study were aware of influenza illness symptoms, the mode of transmission, and the risk of influenza but 30% were not aware if wither their institution offer SIV. Awareness about availability of SIV in the workplace is essential to improve SIV uptake in HCWs.
A relatively low percentage (26.2%) of the HCWs had participated in SIV training or continuing education, while 60% of the respondents indicated that they were interested in participating in future training sessions. These findings concerning a preference for training appear to be consistent with the results of a study undertaken in Riyadh.Citation11 In our study, the HCWs considered the main barriers to providing the SIV to patients were concerns for patient safety in regard to the SIV and non-availability of the SIV, which were consistent with Al Shammari et al.’s findings.Citation11
Our study found that pharmacists were more likely to comply with routine vaccination compared to other professional groups, as were radiology technologist. This finding is likely to be because other professional groups received lower scores concerning their knowledge, attitudes, practices, and awareness regarding the SIV. However, we anticipated that HCWs working at hospitals would have a higher adherence to regular vaccination than those working in a PHC. However, our study showed that there were negative attitudes or poor awareness to regular vaccination among HCWs at both hospitals and PHCs. Although we found HCWs’ attitudes to have had a significant effect (p < .001) on their practice/center in terms of receiving the SIV, we were unable to determine a relationship between knowledge (p = .160), practices (p = .073), or awareness (p = .527). Moreover, we also found that females have better knowledge and attitude score compared to males (p-<.001) and younger age group (<30 years old) had more knowledge (p-.003) and better attitude (p-<.001) toward SIV.
Moreover, several studies also showed a relationship between knowledge, attitudes, practices, and awareness regarding SIV among professional groups, but could not determine a significant effect.Citation10–Citation12 However, Al Shammari, et al. (2014) found no difference between the vaccination rates among pharmacists compared to other HCWs. Furthermore, physicians were found to be less likely to receive vaccinations compared to other HCWs, while nurses were most likely to be vaccinated and had a higher rate of vaccination (p-.01).Citation11
This study had some limitations. First, SIV status was self-reported by the respondents, and their responses were not subject to independent verification, and recall bias may have potentially influenced the results. Second, convenience sampling was a limitation because of the possibility of bias during data collection; therefore, our results cannot be generalized to other HCWs. Moreover, questions used to assess respondent’ SIV knowledge were not extensive and might not have accurately reflected their knowledge levels. However, this was the first study undertaken in Qassim region using a large sample size and including both PHCs and hospitals.
Conclusion
Our study findings provide further insight into SIV prevalence rates among HCWs as well as their levels of knowledge, attitudes, practices, and awareness of the SIV. Our results showed suboptimal SIV coverage among HCWs in Qassim region. Ensuring educational programs and campaigns concerning the risk of influenza infection, as well as providing adequate information and emphasizing the importance of vaccination for HCWs are essential. Easy access to and availability of the SIV in Saudi Arabia is crucial for improved vaccine coverage. A mandatory annual SIV for HCWs is recommended to i SIV vaccine coverage. Health-care institutions should more actively encourage their staff to undergo an SIV on a regular basis, particularly during the influenza season.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
Acknowledgments
I wish to thank all respondents who volunteered for this study. I also thank the following medical students for their efforts with data collection: Ahmad Alhumaid, Rasha Almotairi, Shoug AlRumaih, Abdulrahman Alomairi, Alaa Alsaykhan, and Fatmah Almohaimeed.
Additional information
Funding
References
- Recommendations V. Guidelines of the ACIP. [Accessed 2019 May 18]. https://www.cdc.gov/vaccines/hcp/acip=recs/general-recs/immunocompetence.
- Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, Gran JM, Schanzer D, Cowling BJ, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018;391:1285–3000. doi:10.1016/S0140-6736(17)33293-2.
- Centers for Disease Control and Prevention. Seasonal influenza vaccine effectiveness, 2005–2018. Influenza. [Accessed 2019 May 18]. https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm.
- Dawood FS, Iuliano AD, Reed C, Meltzer MI, Shay DK, Cheng PY, Bandaranayake D, Breiman RF, Brooks WA, Buchy P, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis. 2012;687–95. doi:10.1016/S1473-3099(12)70152-4.
- Jorgensen P, Mereckiene J, Cotter S, Johansen K, Tsolova S, Brown C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36:442–52. doi:10.1016/j.vaccine.2017.12.019.
- Al Awaidi AS, AbuHasan M, Akcay M, Aksakal FN, Bashir U, Elahmer O, Esteghamati A, Gahwagi M, Mirza YK, Derrar F, et al. Influenza vaccination situation in Middle-East and North Africa countries: Report of the 7th MENA Influenza Stakeholders Network (MENA-ISN). J Infect Public Health. 2018;11:845–50. doi:10.1016/j.jiph.2018.07.003.
- Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum Vaccin Immunother. 2018;14:772–89. doi:10.1080/21645515.2018.1486156.
- Black CL, Yue X, Ball SW, Fink RV, de Perio MA, Laney AS, Williams WW, Graitcer SB, Fiebelkorn AP, Lu PJ, et al. Influenza vaccination coverage among health care personnel—United States, 2017–18 influenza season. MMWR Morb Mortal Wkly Rep. 2018;67:1050. doi:10.15585/mmwr.mm6738a2.
- Alenazi BR, Hammad SM, Mohamed AE. Prevalence of seasonal influenza vaccination among primary healthcare workers in Arar city, Saudi Arabia. Electron Physician. 2018;10:7217. doi:10.19082/7217.
- Alqartun NA. Attitude towards seasonal influenza vaccination by healthcare workers. Egypt J Hosp Med. 2018;70:12.
- Alshammari TM, AlFehaid LS, AlFraih JK, Aljadhey HS. Health care professionals’ awareness of, knowledge about, and attitude to influenza vaccination. Vaccine. 2014;32:5957–61. doi:10.1016/j.vaccine.2014.08.061.
- Haridi HK, Salman KA, Basaif EA, Al-Skaibi DK. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J Hosp Infect. 2017;96:268–75. doi:10.1016/j.jhin.2017.02.005.
- Rehmani R, Memon JI. Knowledge, attitudes and beliefs regarding influenza vaccination among healthcare workers in a Saudi hospital. Vaccine. 2010;28:4283–87. doi:10.1016/j.vaccine.2010.04.031.
- Al-Tawfiq JA, Antonyb A, Abedb MS. Attitudes towards influenza vaccination of multi-nationality health-care workers in Saudi Arabia. Vaccine. 2009;27:5538–41. doi:10.1016/j.vaccine.2009.06.108.
- Balkhy HH, El-Saed A, Sallah M. Epidemiology of H1N1 (2009) Influenza among healthcare workers in a tertiary care center in Saudi Arabia: a 6-month surveillance study. Infect Control Hosp Epidemiol. 2010;31:1004–10. doi:10.1086/656241.
- Abu-Gharbieh E, Fahmy S, Rasool BA, Khan S. Influenza vaccination: healthcare workers attitude in three Middle East countries. Int J Med Sci. 2010;7:319–25. doi:10.7150/ijms.7.319.
- Godoy P, Castilla J, Mayoral JM, Martín V, Astray J, Torner N, Toledo D, Soldevila N, González-Candelas F, García S, et al. Influenza vaccination of primary healthcare physicians may be associated with vaccination in their patients: a vaccination coverage study. BMC Fam Pract. 2015;16:44. doi:10.1186/s12875-015-0259-0.
- Rabensteiner A, Buja A, Regele D, Fischer M, Baldo V. Healthcare worker’s attitude to seasonal influenza vaccination in the South Tyrolean province of Italy: barriers and facilitators. Vaccine. 2018;36:535–44. doi:10.1016/j.vaccine.2017.12.007.
- Böhmer MM, Walter D, Falkenhorst G, Müters S, Krause G, Wichmann O. Barriers to pandemic influenza vaccination and uptake of seasonal influenza vaccine in the post-pandemic season in Germany. BMC Public Health. 2012;12:938. doi:10.1186/1471-2458-12-938.
- Lehmanna BA, Ruiter RAC, Chapmanb G, Koka G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine. 2014;32:6986–90. doi:10.1016/j.vaccine.2014.10.034.
- Edmond MB. Mandatory flu vaccine for healthcare workers: not worthwhile. In: Open forum infectious diseases (Vol. 6, No. 4, p. ofy214). US: Oxford University Press; 2019. p. 214. doi:10.1093/ofid/ofy214
- Chean R, Ferguson JK, Stuart RL. Mandatory seasonal influenza vaccination of health care workers: a way forward to improving influenza vaccination rates. Healthcare Infect. 2014 Jun 1;19(2):42–44. doi:10.1071/HI13041.