ABSTRACT
Prevention of congenital rubella is achieved by vaccination of susceptible women of childbearing age. In Italy, the National Plan for Measles and Congenital Rubella Elimination 2010–2015 implemented catch-up vaccination activities targeting susceptible adolescents and young adults, including women of childbearing age. The aim of this study was to assess the immunity against rubella in women of childbearing age in Tuscany (Central Italy) and Apulia (Southern Italy) and pregnant women in Apulia after the implementation of the National Plan for Measles and Congenital Rubella Elimination. Overall, anti-rubella IgG prevalence in women of childbearing age samples was 88.6% in Tuscany and 84.3% in Apulia. The lowest prevalence was observed in samples of 26–35 years old women of childbearing age in Apulia with 77.8%. Only 62.7% of samples from 26–35 years old pregnant women had IgG against rubella, and one sample out of 95 was positive to IgM. The findings of this study highlight the need for increasing awareness on the risk of contracting rubella infection during pregnancy and implement vaccination strategies to create opportunities for administration of rubella containing vaccines in young girls and women of childbearing age.
Introduction
Rubella is a highly contagious viral disease usually affecting children and young adults; if contracted during pregnancy may lead to miscarriage, premature delivery or congenital defects known as Congenital Rubella Syndrome (CRS). The highest risk of CRS is associated with high rates of susceptibility to rubella among women of childbearing age (WOCBA).Citation1
In Italy, live attenuated vaccines against rubella were available since 1972 and were recommended for adolescent girls only. Starting from 1990, immunization with the combined measles-mumps-rubella (MMR) vaccine was recommended for children within the second year of life, but was offered free of charge only by some regions, mainly located in Northern and Central Italy. In 1999 MMR vaccine was included in the national immunization schedule and one dose was recommended in children between 12 and 15 months of age.Citation2 In 2003, Italy approved the first National Plan of Measles and Congenital Rubella Elimination (NPMCRE 2003–2007), targeting to reducing CRS below 1/100,000 live births per year by 2007. The operating goals introduced a two-doses schedule with MMR vaccine in all regions with a booster dose at 5–6 years of age and catch-up vaccinations of older children, adolescents and WOCBA.Citation3,Citation4 As elimination goal for measles and congenital rubella was not achieved, NPMCRE was renewed for 2010–2015 (NPMCRE 2010–2015) and in the National Immunization Prevention Plan for 2017–2019 (PNPV 2017–2019).Citation5-Citation7
In Italy, a national passive surveillance system for congenital rubella and rubella in pregnancy is active since 2005.Citation8 According to the Italian National Institute of Health (ISS) surveillance data, from January 2005 to February 2018 a total 173 cases of rubella in pregnancy and 88 cases of congenital rubella were reported.Citation9 Although the incidence of congenital rubella was below the World Health Organization target of 1/100,000 live births, except for two peaks in 2008 and 2012 (5 and 4/100,000, respectively),Citation10 the underreporting to the national surveillance system should be taken into account as it is estimated to be >50%.Citation11
The present study was performed to assess the profile of rubella susceptibility in WOCBA and in pregnant women in two large Italian regions after the implementation of NPMCRE for 2010–2015.
Methods
The study was performed on serum samples anonymously stored at the serum bank of the Laboratory of Molecular Epidemiology, Department of Molecular and Developmental Medicine of the University of Siena. Samples were collected for various medical checks in compliance with Italian law on Ethics in the province of Siena (Tuscany region, Central Italy) and Bari (Apulia region, Southern Italy) between 2014 and 2016. For each sample information available were age, gender, date and place of sampling. For serum samples collected in Bari, state of pregnancy was also available.
Out of a total of 2500 available serum samples of women between 15 and 45 years of age, 899 were randomly selected by using a computer generated randomization list, stratified by age groups of 15–25, 26–35 and 36–45 years and tested for the presence of specific anti-rubella IgG. In addition, 95 serum samples collected in Bari of pregnant women were randomly selected and stratified in two age groups of 26–35 and 36–45 years and tested for the presence of anti-rubella IgG and IgM.
Specific anti-rubella antibodies were detected by commercial ELISA kits ENZYWELL Rubella IgG and ENZYWELL Rubella IgM, kindly provided by DIESSE (Siena, Italy). Samples were tested using a qualitative method, as indicated by manufactured instructions. Samples were considered positive for IgG when the ratio between the optical density of the sample and that of the cutoff was >1.3, while negative if the ratio was <0.7. Samples were considered positive for IgM with a ratio >1.2 and negative with a ratio <0.8. Samples with borderline result (between 0.7 and 1.3 for IgG and between 0.8 and 1.2 for IgM) were retested. For IgG, the cutoff used corresponded to 10 IU/ml, considered the correlate of protection for rubella.Citation1
Seroprevalence rates were calculated along with the corresponding 95% confidence intervals (CI). Fisher’s exact test and Chi-square test for trend were used for statistical analysis using GraphPad Prism 6 software; statistical significance was set at p < .05, two tailed.
Results
Of the 899 samples tested in total, 57 were borderline and were retest. At retest, still 34 had borderline results and therefore were excluded from the analysis. The mean age of WOCBA was 34 (±7.5) years for Siena samples and 31.7 (±8.1) years for Bari samples. The mean age of pregnant women samples was 33.7 (±4) years. shows the distribution of samples suitable for statistical analysis by age group and place of sampling.
Figure 1. Anti-rubella IgG prevalence in WOCBA from Siena and Bari, and in pregnant women from Bari between 2014 and 2016 by age groups.
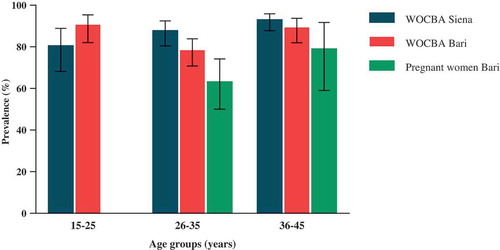
In WOCBA samples collected in Siena, the positivity rate was 88.6% (85.1–91.4; 343/387) and a trend toward increase with age is present (p = .005). 80.0% (68.6–88.1; 52/65) of samples belonging to 15–25 years old age group showed immunity against rubella, followed by 87.3% (80.5–92.0; 117/134) and 92.5% (87.8–95.6; 174/188) in 26–35 and 36–45 years old age groups, respectively. In Bari, the overall seroprevalence was 84.3% (80.3–87.6; 323/383) and a significant lower seroprevalence was observed in WOCBA 26–35 years old age group (77.8%, 70.9–83.5; 130/167) in comparison to the other two age groups (15–25 years old: 90.1%, 82.1–94.9; 82/91 and 36–45 years old: 88.8%, 82.0–93.3; 111/125) (p = .022 vs both). WOCBA 26–35 years old age group samples from Bari were found to be significantly lower also compared to samples of the same age group from Siena (p = .035).
A total of 67.4% (57.4–76.0; 64/95) of pregnant women samples from Bari had antibody against rubella. 62.7% (50.7–73.3; 42/67) of samples of the 26–35 years old age group and 78.6% (60.1–90.1; 22/28) of the 36–45 years old age group were found to be positive. Comparing WOCBA samples from Bari with the pregnant women samples of the same age, a significant difference was found (p < .001), especially between the 26–35 years old age groups of the two population (p = .022). One pregnant woman belonging to the 26–35 age group (1.1%, 0–6.3; 1/95) was found to be positive for anti-rubella IgM, as well as positive for IgG.
Discussion
Prevention of congenital rubella is achieved by maintaining high levels of vaccine coverage (> 95%) in the general population and identification and vaccination of susceptible WOCBA. This seroprevalence study was conducted to evaluate whether the objective of the NPMCRE 2010–2015 of increasing immunity to rubella in WOCBA in two different Italian provinces, Siena (Tuscany) and Bari (Apulia), was achieved. Moreover, immunity to rubella was also assessed in a sample of pregnant women from Bari. Overall, immunity to rubella in WOCBA samples was similar in Siena and Bari, with some significant differences by age groups. In Siena, 20% of WOCBA subjects between 15 and 25 years old had no immunity to rubella. These data are consistent with those published by the Ministry of Health in 2016, where in Tuscany region the 18-year-old subjects (born in 1998) had a vaccine coverage of 85.5% and 79% for the first and second dose, respectively, of rubella containing vaccine.Citation12 In Bari, immunity to rubella in the WOCBA 15–25 years old group was 90%. This value is higher than reported in a seroepidemiological study conducted in 2011–2012.Citation13 The higher proportion of samples with immunity to rubella is most likely due to vaccination campaign for MMR implemented within the framework of NPMCRE 2010–2015. The impact of that vaccination campaign in Apulia region was such that coverage for MMR increased from 87.7% for the first dose and 75.9% for the second dose in 18-years old subjects (born in 1998) to 92.5% and 82.7% respectively in 16-years-old subjects (born in 2000).Citation12,Citation14 However, only 77% of WOCBA samples of 26–35 years old group had immunity to rubella, which is of concern if we consider that in Italy the mean age at the delivery in 2016 was 31.8 years and for most women is the only pregnancy as the total fertility rate per woman is 1.34.Citation15 WOCBA lacking immunity to rubella were born between 1979 and 1990, but catch-up vaccination campaign in school planned by NPMCRE since 2003 targeted only women born between 1991 and 1997 (NPMCRE 2003–2007). Therefore, those WOCBA lacking protective immunity have probably missed vaccination offered by catch-up programmes.Citation13 Meanwhile, the concomitant decrease in the circulation of wild-type virus has reduced the possibility of natural infection-induced immunity. On the other hand, older women born in the 70s, during a high natural virus circulation period, show significantly higher antibody prevalence, possibly because of the higher antibody levels induced by natural infection. In fact, a survey conducted in 1985 showed that the vaccine coverage for rubella in 10 years old girls, the target population for rubella immunization at the time, was 11.3% and 6.1% in Central and Southern Italy, respectively.Citation16
In Bari, the immunity gap for pregnant women samples of the 26–35 years old group, and to less extent to the 36–45 one, is of particular concern as a substantial proportion of the neonates are at high risk of CRS. In addition, the detection of IgM in one sample of pregnant women of 26–35 years old group suggests that rubella virus circulates in this population to an extent that may be wider than what we detected in the limited sample size of this study. The gap in immunity to rubella observed between WOCBA and pregnant women in samples from Bari may also be explained by the fact that a proportion of pregnant women population may be represented by women of recent immigration to Italy. In fact, surveillance data of CRS in Italy reported that 17% of pregnant women who had contracted rubella infection during pregnancy were not Italian and their mean age was 27 years.Citation9
This study has some limitations. Samples may not be representative of the WOCBA or pregnant women population as they were taken for reasons different from the objectives of the study. Limited information was available such as the vaccination status or the trimester of pregnancy.
The Italian Behavioral Risk Factor Surveillance System (PASSI) showed that in the 2013–2016 period, 39.1% of WOCBA had an unknown immune status against rubella or was susceptible to rubella, Citation17 suggesting a low level of awareness about the risk of contracting the infection during pregnancy. In Italy, rubella test is offered free of charge as pre-conception screening and rubella vaccination is offered to susceptible women in any opportunities of encounter (i.e., the anti-tetanus-diphtheria-pertussis booster dose, the anti-human papilloma virus vaccine administration, the first pap-test screening, after delivery or after abortion) (NPMCRE 2010–2015). However, as already observed for other vaccine-preventable diseases,Citation18,Citation19 the vaccination strategy based on the passive offer seems to be not enough for the achievement of the NPMCRE objective to reduce the percentage of susceptible females below 5%.Citation4,Citation13
In conclusion, in Italy in 2017, the vaccine coverage for rubella in 16-years-old adolescents (born in 2001) is about 85% for the first dose and 83% for the second dose of MMR vaccine, Citation20 meaning that a considerable proportion of women entering to childbearing age are susceptible to rubella. It is therefore necessary to develop additional vaccination strategies that will target both Italian and recently immigrant women in order to reduce the pocket of susceptibility to rubella in young girls and WOCBA.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
The authors thank Dr. Dario Soldateschi, who kindly provided IgG and IgM ELISA kits.
Additional information
Funding
References
- WHO. Rubella vaccines: WHO position paper. Wkly Epidemiol Rec. 2011;86(29):301–16.
- Rota MC, Bella A, Gabutti G, Giambi C, Filia A, Guido M, De Donno A, Crovari P, Ciofi Degli Atti ML; G. Serological Study. Rubella seroprofile of the Italian population: an 8-year comparison. Epidemiol Infect. 2007;135(4):555–62. doi:10.1017/S0950268806007400.
- Ministero della Salute. Piano nazionale per l’eliminazione del morbillo e della rosolia congenita 2003–2007. 2003.
- Giambi C, Filia A, Rota MC, Del Manso M, Declich S, Nacca G, Rizzuto E, Bella A; r. regional contact points for. Congenital rubella still a public health problem in Italy: analysis of national surveillance data from 2005 to 2013. Euro Surveill. 2015;20(16). doi:10.2807/1560-7917.ES2015.20.16.21103.
- Ministero della Salute, Piano nazionale per l’eliminazione del morbillo e della rosolia congenita 2010–2015. 2011. 1–36.
- Bechini A, Levi M, Boccalini S, Tiscione E, Panatto D, Amicizia D, Bonanni P. Progress in the elimination of measles and congenital rubella in Central Italy. Hum Vaccin Immunother. 2013;9(3):649–56. doi:10.4161/hv.23261.
- Ministero della Salute, Piano Nazionale Prevenzione Vaccinale 2017-2019.
- Ministero della Salute, Circolare 5 agosto 2005, n.2 “Notifica obbligatoria della infezione da rosolia in gravidanza e della sindrome/infezione da rosolia congenita”. Gazzetta ufficiale n. 211.
- Istituto Superiore di Sanità, Rapporto sulla sorveglianza della Rosolia congenita e in gravidanza, in Rosolia congenita e in gravidanza News. 2018.
- Istituto Superiore di Sanità, Congenital rubella and rubella in pregnancy surveillance report, in Congenital rubella and rubella in pregnancy News. 2016.
- Giambi C, Bella A, Filia A, Del Manso M, Nacca G, Declich S, Rota MC; r. Regional contact points for. Underreporting of congenital rubella in Italy, 2010–2014. Eur J Pediatr. 2017;176(7):955–62. doi:10.1007/s00431-017-2935-7.
- Ministero della Salute, Vaccinazioni dell’adolescente. Anno 2016 (coorte 1998-18 anni). 2017.
- Gallone MS, Gallone MF, Larocca AMV, Germinario C, Tafuri S. Lack of immunity against rubella among Italian young adults. BMC Infect Dis. 2017;17(1):199. doi:10.1186/s12879-017-2724-y.
- Ministero della Salute, Vaccinazioni dell’adolescente. Anno 2016 (coorte 2000-16 anni). 2017.
- ISTAT, Natalità e fecondità della popolazione residente. Anno 2016, in Statistiche report. 2017.
- Salmaso S, Stazi MA, Luzi S, Greco D. Immunization coverage in Italy. Bull World Health Organ. 1987;65:841–46.
- Epicentro, La sorveglianza Passi. I dati per l’Italia: vaccinazione antirosolia periodo 2015–2018.
- Marchi S, Monti M, Viviani S, Montomoli E, Trombetta CM. Measles in pregnancy: a threat for Italian women? Hum Vaccin Immunother. 2019;1–3. doi:10.1080/21645515.2019.1621146.
- Marchi S, Viviani S, Montomoli E, Trombetta CM. Low prevalence of antibodies against pertussis in pregnant women in Italy. Lancet Infect Dis. 2019;19(7):690. doi:10.1016/S1473-3099(19)30269-5.
- Ministero della Salute, Vaccinazioni dell’adolescente. Anno 2017 (coorte 2001 ‐ 16 anni). 2018.
