ABSTRACT
Background: Vaccines against whooping cough (pertussis) and seasonal-influenza are recommended for pregnant women in England. Uptake however varies regionally and by ethnicity. Pregnant women are traditionally vaccinated in primary care, though some hospitals now offer vaccines through antenatal clinics. This mixed-methods evaluation describes the demographic characteristics of women seen in a hospital midwife-led antenatal vaccine clinic and explores vaccine decision making.
Methods: Descriptive statistics of women seen in a London hospital’s midwife-led vaccine clinic were generated from electronic routine maternity records, including data on ethnicity, parity, age and deprivation indices. Reasons for vaccine decline given by women to midwives were categorized by themes. Qualitative interviews of women seen in the clinic were also undertaken.
Results: Between 1st April 2017 and 31st March 2018 the vaccine clinic saw 1501 pregnant women. Of these, 83% received pertussis vaccine and (during flu season) 51% received influenza vaccine, from the clinic. Fewer Black Afro-Caribbean women seen by the clinic were vaccinated, compared to other ethnicities with only 68% receiving pertussis and 34% flu vaccines respectively (p < .05). Among all women delivering at the hospital over the year, 42%, (1334/3147) were vaccinated by the clinic. Qualitative interviews found that reassurance from healthcare professionals, particularly midwives, was the most important factor influencing maternal vaccine decisions.
Conclusions: Midwife-led hospital clinics can offer an effective alternative to primary care provision for vaccines in pregnancy. Consistent with previous work, vaccine uptake varied by ethnicity. Midwives play a key role in the provision of vaccine services and influence women’s vaccine decisions.
Introduction
In 2012 a pertussis (whooping cough) outbreak was declared in England following increased incidence and several infant deaths.Citation1 In response, a maternal pertussis vaccination program was subsequently introduced nationally.Citation2 Vaccination during pregnancy can passively protect young infants before they receive their own routine vaccinations by increasing levels of transplacentally transferred maternal antibody.Citation3 In the UK, vaccination against pertussis is now recommended for all pregnant women between 16 and 32 weeks of pregnancyCitation4 and the program has been shown to be safeCitation5 and effective in reducing cases of infant pertussis and the associated morbidity and mortality.Citation6,Citation7 Similarly, seasonal influenza vaccination is recommended for women at any stage of pregnancyCitation8 to prevent severe illness in womenCitation9 and improve infant outcomes.Citation10,Citation11
Uptake of vaccines in pregnancy – also referred to as maternal immunization – varies nationally and internationally due to a number of barriers and influences on the decision to get vaccinated in pregnancy.Citation12 Maternal vaccine uptake in England varies regionally and has been historically lower in London for both pertussisCitation13-15 and influenza.Citation16 Deprivation and ethnicity are known predictors of lower maternal pertussis vaccine uptakeCitation17,Citation18 as well as for maternal and child influenza vaccine uptake in England.Citation19 Previous work conducted by our group in London found low awareness and low maternal pertussis uptake with variation between different ethnicities, with the lowest uptake among Black Afro-Caribbean womenCitation20 (a demographic group including Black African/Caribbean/Black British and women of any other Black backgroundCitation21).
Healthcare professionals and midwives have been found to be key trusted sources of advice for women’s vaccine decisions.Citation14,Citation20,Citation22–24 A review of strategies to improve uptake of maternal vaccines identified vaccine provision by midwives as an effective strategy to increase coverage of maternal vaccines, Citation25 in concordance with studies outside of the UK which have also found that midwife-delivered maternal vaccination clinics can improve vaccine uptake.Citation26–28 Improving maternal vaccine uptake could additionally enhance uptake of vaccines in childhood: an Australian study found that vaccine hesitancy in pregnancy was associated with lower infant vaccine uptake.Citation29
Traditionally in England, pediatric and adult vaccines are delivered within primary care. Therefore, when maternal vaccines were introduced in recent years, they were also delivered by primary care General Practices (GP). However, in late 2016 some hospital-based antenatal clinics started to offer vaccines to pregnant women.Citation13,Citation23 Midwives experienced in caring for women in pregnancy, were responsible for delivering vaccines in the clinics. However, a lack of data on the use of non-primary care based clinics for the delivery of maternal vaccines remains. Accurate estimation of maternal vaccine uptake, which is estimated from GP records, with this new model of care has been difficult due to data completeness issues. Firstly, the denominator of all pregnant women registered with GPs, used to calculate uptake, is thought to be incompleteCitation13,Citation16 and secondly, it is unknown how many antenatally delivered vaccines are accurately recorded in routine GP records.Citation13,Citation16 A recent commentary summarizing the literature on maternal vaccination delivery within routine antenatal care highlighted the potential of the hospital-based clinic models to improve maternal vaccine uptake in England.Citation30
We therefore conducted an evaluation of a midwife-led vaccination clinic, based in a hospital antenatal care setting, in London. We describe the demographic characteristics of women who received or declined vaccination from the clinic and we explored the decision-making process of women who used the vaccine clinic at the hospital through a number of qualitative interviews.
Methods
Description of the midwife-led vaccine clinic based within antenatal service
In December 2016, a clinic was set up at Imperial College Healthcare NHS Trust to vaccinate pregnant women attending antenatal clinics. The clinic was midwife-led by two part-time dedicated ‘vaccine midwives’ (equivalent to one full-time midwife) who received training on maternal vaccine delivery and counseling. The vaccine midwives were senior, experienced midwives who had received specific training in the administration of vaccines and previously worked in both hospital obstetric and community midwifery roles. Their role was as solely dedicated vaccine midwives during the period of the service evaluation, though if staffing levels were low they would occasionally also see women for routine hospital appointments in the antenatal clinic. The clinic was promoted locally, and women could be referred by other midwives and doctors whilst attending routine antenatal appointments, self-refer, or be opportunistically approached by the vaccine midwives in the antenatal waiting rooms. The vaccine midwives were based in one of the consulting rooms within the routine antenatal clinic. Some women were seen in the vaccine clinic on more than one occasion if they initially declined the vaccine on first contact.
Clinic data analysis
We undertook a one-year clinic evaluation at one hospital site of The Trust between April 2017 and March 2018. The vaccine clinic midwives used a hospital computer based excel spreadsheet to create a dataset, separate from the woman’s computerized maternity notes, to record each woman seen in the vaccine clinic for the purpose of returning data to the clinic commissioners. This dataset, manually entered by the vaccine midwives, recorded the date of the interaction, if women were vaccinated and which vaccines were given. If women declined vaccination, a brief free-text reason for declining was recorded. The delivery of any vaccines was also being recorded as a free text ‘clinic entry’ on each woman’s hospital maternity records. Women attending the clinic were asked to inform their GP if they had been vaccinated at the hospital.
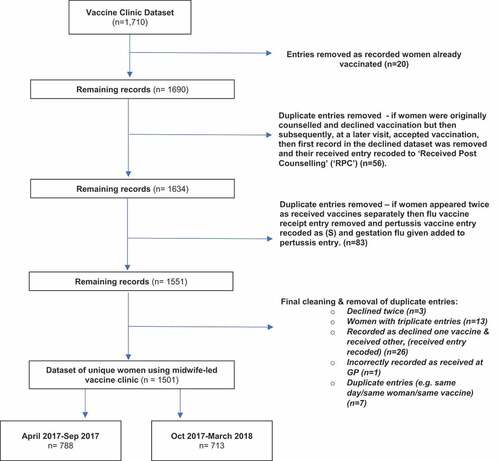
The dataset underwent cleaning to remove duplicate entries (see ) to create the final dataset for analysis, which reflected each individual woman who was seen by the clinic. Some duplicate records arose if women were originally counseled and declined vaccination but then subsequently, at a later clinic visit, were vaccinated on site. Records of women which appeared more than once were checked against individual electronic hospital records to ensure accuracy of final allocation.
Demographic data was generated through the hospital numbers of women seen in the midwife-led clinic and retrieved from the hospital’s electronic maternity records. Data was retrieved on the women’s age bracket (not exact date of birth), estimated due date (used to calculate the gestation when the women were seen), parity, ‘ethnicity or familial background’ and whether they understood English. Postcodes were mapped for each woman to corresponding Index of Multiple Deprivation 2015 decile, in line with standard interpretations.Citation31 Postcodes and hospital numbers were ultimately removed to create the final anonymized dataset for analysis. Due to some missing data, the gestation at the time of vaccination could not be calculated for all individuals (n = 18).
Initial analysis generated overall descriptive characteristics of all women seen in the vaccine clinic. Ethnicities of women were compared to the ethnicities of all women delivering at the hospital site over the same year, as available from the routine hospital record system.
To estimate the proportion receiving or declining flu vaccination the dataset was separated into two, six-month datasets (see ), as flu was only offered for the latter six months of the year, in line with seasonality. Chi-squared test of independence was used to determine association between the different categorical variables such as ethnicity and being vaccinated by the vaccine clinic. The brief free-text reasons recorded by the midwives in the spreadsheet for women who declined vaccination were also categorized and tabulated.
Qualitative interviews
Participants, sampling & recruitment
Participants for interviews were women aged over 18 years receiving (or having recently received) antenatal care at the same hospital, who had been seen by the vaccine midwives. A convenience sample was used, and women were recruited by being approached by one of the vaccine midwives in the antenatal clinic waiting area and given an invitation letter and the participant information sheet. Women who expressed an interest in participating were contacted directly by the researcher for further explanation. Written informed consent was obtained prior to participation. For the interviews, ethical approval was received from the local Hampstead Research Ethics Committee, London, reference number: 13/LO/1712.
Interviews
An Interpretative Phenomenological Analysis (IPA) approachCitation32 was used to enable participants to offer a rich, detailed, first-person account of their experiencesCitation33 and to understand how they approached vaccine decisions in pregnancy. Research questions in IPA focus upon people’s understanding of their experiences and are framed broadly and openly.Citation32
Interview data was derived from either recorded telephone interviews with one researcher (a midwife) or a face-to-face discussion that was recorded between two women and the same midwife researcher. The interview process consisted of open-ended questions which were developed drawing on previous research.Citation20 All main points raised by each participant were summarized at the end of the discussion by the researcher, giving women the opportunity to add or amend as required.
Qualitative interviews data analysis
Interview transcripts were analyzed according to the principles of IPA using an iterative approach. This involved multiple readings and note making, transforming notes into emergent themes, before trying to identify relationships and clustering themes.Citation32,Citation34 Each transcript was re-read several times and analyzed in its entirety before moving onto the next by the same midwife researcher (BD) who interviewed the women.
Results
Clinic use
Between 1st April 2017 and 31st March 2018, 1710 entries of women seen in the clinic were recorded. Of these, 1429 entries showed vaccines administered and 281 vaccination being declined. Following duplicate removal, 1501 unique pregnant women’s records remained, (see ). Between 1st April and 31st September 2017, the vaccine midwives saw 788 women; between 1st October 2017 and 31st March 2018, 713 women were seen. The completeness of the data differed between variables (supplementary tables 2–4).
Women seen in the midwife-led, antenatal maternal vaccine clinic
Between 1st April 2017 and 31st March 2018, 3147 women delivered at the hospital site. Of all women delivering at the hospital, 48% (n = 1501/3147) were seen in the clinic over this time period. Overall, 89% (n = 1334/1501) received one or two maternal vaccines (for full breakdown, see supplementary table 1). Therefore, 42% of all women delivering at the hospital between April 2017 and March 2018 received one or more maternal vaccines via the vaccine clinic (1334/3147 deliveries). Four percent of women (n = 56), received counseling by the vaccine midwives during an earlier appointment and prior to the date when they were eventually vaccinated.
The ethnicity profile of women seen in the vaccine clinic was comparable to all women delivering at the hospital site during the same time period (). In 33%, ethnicity was not recorded. Of women seen in the clinic, 4% (n = 63) were recorded as not understanding English, of which 11% declined vaccination from the clinic.
Table 1. Ethnicities of all women delivering at the hospital compared to all women recorded as using the midwife led maternal vaccine clinic
According to IMD decile ranking, 48% of all women seen in the clinic lived in neighborhoods among the 30% most deprived in England and 28% of women lived in the 20% most deprived areas (supplementary table 2). Fifty four percent were primiparous and the majority (79%) were aged 26–39 years (supplementary tables 3 & 4). On average, women were seen in the vaccine clinic at 25 weeks gestation (range 6–40 weeks).
Pertussis vaccine
Over the entire observation period, 83% of women seen (n = 1252/1501) were vaccinated against pertussis by the antenatal vaccine service.
Flu vaccine
During flu season, 51% (n = 360/713) of women were vaccinated against flu by the antenatal vaccine service. Forty women who were vaccinated with pertussis vaccine by the clinic between April and September 2017 also went onto receive their flu vaccine there later in pregnancy, when they became eligible in the flu season.
Overall, 15% (n = 43) received pertussis and flu vaccines at separate appointments. During flu season, 11% of women (n = 75) received neither pertussis vaccine nor seasonal flu vaccine.
Demographic variation in vaccine receipt
10% of women (n = 155) seen by the clinic were Black-Afro Caribbean (including women of mixed black ethnicities). Only 68% of these women seen in the clinic received pertussis vaccine compared to over 80% of women seen from other ethnicities (, p < .05). During flu season (Oct 2017-Mar 2018) only 36% of Black-Afro Caribbean women received flu vaccine compared to an average of 51% of women from other ethnicities (, p < .05).
Figure 2. Pertussis vaccine receipt by ethnicity April 2017-March 2018
Figure 3. Seasonal flu vaccine receipt by ethnicity October 2017-March 2018
Vaccine receipt was found to be significantly associated with parity: overall, 19% of women of higher parity (greater than 2) declined vaccination compared to 9% of women who were pregnant with their first or second child (supplementary table 5, p < .05). A higher percentage of women aged 16–25 years (17%) declined maternal pertussis vaccine compared to those aged over 25 years (10%), however this did not reach statistical significance (supplementary table 6, p > .05).
Declining or receiving vaccination was not found to be independently associated with deprivation (p ≤ 0.05). However, overall a higher proportion of Black Afro-Caribbean or Mixed-Black Afro-Caribbean ethnicity women lived in deprived areas. Of Black Afro-Caribbean women, 79% lived in neighborhoods among the 40% most deprived in England (IMD score 1–4) compared to 56% of white women.
Free-text reasons recorded for declining
The four most common reasons recorded for women declining vaccination were ‘Declined for personal reasons’ (36/167,22%), ‘Declined as wanted time to consider’ (32/167, 19%), ‘No reason given’ (28/167,17%) and ‘Not believing in vaccines or vaccines in pregnancy’ (26/167, 16%), ().
Table 2. Reasons recorded for women who declined vaccination from the maternal vaccine clinic Oct 2017-March 2018
Qualitative interviews results
Characteristics of women participants
A total of 10 women aged 29 to 44 years and from diverse ethnic backgrounds were recruited for interviews, of whom three had declined and seven had received pertussis vaccination during pregnancy. Six women were nulliparous and four multiparous. Eight were pregnant at the time of interview, with gestations ranging from 27 to 38 weeks, and two women were postnatal.
Attitudes to vaccination
Four main themes arose from the analysis of influences on decision making with regards to maternal vaccination as outlined below using example quotes.
1. Interactions with midwives and health care workers
2. Perceived risk of disease and vaccines
3. Beliefs and experiences
4. Trust or distrust in ‘system’
The first key theme that arose was how interactions with health care workers influenced women’s vaccination decisions. For some women, healthcare workers were seen as knowledgeable, enthusiastic and warm but some women were unhappy with the routine nature of the information provided. Secondly, women’s perceived risks of the vaccine or the disease itself were important factors. For some women the risk of the disease meant they accepted vaccination, whereas others perceived the risks of the vaccine to be too high and they declined vaccination. Thirdly, beliefs and experiences were important influences, either meaning women believed in vaccines or that their ‘holistic’ beliefs meant they declined vaccination. Finally, the women’s trust in the wider public health system were important factors that influenced their decision making with some viewing it negatively and declining vaccination whilst others trusted the system and were vaccinated. Based on the thematic analysis of the interview transcripts women could be characterized into three categories, reflecting their approach to vaccine decision-making: pro-vaccination, anti-vaccination and the hesitant-complier (see supplementary, table 7).
Discussion
Our findings support hospital-based midwife-led antenatal clinics as a model that can make an important contribution to maternal vaccination programs. We believe that this is the first evaluation to describe the demographics of women seen in a hospital based midwife-led maternal vaccine clinic in England. By extracting routinely collected data from electronic hospital maternity records we were able to analyze records of over 1500 women. Of women who were seen in the vaccine clinic, 89% were ultimately vaccinated by the service (with either flu or pertussis). Vaccine receipt among women however was not universal, as a higher proportion of Black Afro-Caribbean women declined vaccination from the clinic, in line with national data on maternal immunization uptake.Citation17 We also report a lower uptake in women of higher parity.
The ethnicity profile of women seen in the vaccine clinic was representative of the overall ethnically diverse local maternity population who deliver at this hospital. Thus, we believe that our findings are relevant to other diverse urban populations with antenatal clinics providing maternal vaccines. By combining quantitative and qualitative data derived from the same setting, our descriptive evaluation is able to provide a picture of both the demographics and the attitudes to vaccine decision making among pregnant women.
Our original study from 2015 found low (26%) maternal pertussis uptake at the same hospital,Citation20 and uptake has clearly improved nationally overall since the introduction of the maternal pertussis programme in 2012.Citation35 Between April 2017 and March 2018, the average national maternal pertussis vaccine uptake reported by Public Health England was 72%, but only 60% in Greater London.Citation35 In two clinical commissioning group areas local to the hospital, the reported uptake was even lower at 52%,Citation36 though it is acknowledged that these figures might underestimate coverage.Citation35 The reported estimated national and regional seasonal influenza vaccine uptake among pregnant women is generally lower than uptake of the pertussis vaccineCitation16 for example, local clinical commissioning groups reported influenza vaccine uptake of only 39% among pregnant women for the same time period.Citation37
During the time period studied, the vaccines delivered by the hospital-based clinic were not being automatically recorded in GP records, as there was no direct data link between the vaccine clinic and general practice. Women attending the clinic were asked to inform their GP. As a consequence, women vaccinated by the clinic might have been missed in the reported regional or national statistics, which come from GP records. Following our study period, a letter notifying GPs of vaccination started to be sent by the clinic as a matter of routine. In order to fully evaluate the impact of antenatal maternal vaccine clinics in England, hospital-based delivered vaccines should be accurately reported within national maternal vaccine estimates, which remain based on GP surveillance data. Whilst our evaluation does not provide local population-level uptake estimates, it does support previous findings of the effectiveness of midwife-delivered vaccine models.Citation25,Citation30,Citation38 A recently reported survey of UK GPs also found that there was support among GPs for antenatal services to deliver maternal vaccine programs in England.Citation39
Other investigators have previously reported on vaccine clinics based within maternity services, for example Green et al. described a midwife clinic based in Lewisham and Greenwich NHS Trust.Citation23 However, the authors did not analyze the demographics of women using the clinic nor reasons for acceptance or declining vaccination from the clinic. A recently reported feedback survey of one hundred women using an antenatal vaccine clinic in England found that 61% endorsed antenatal appointments as the optimal place for vaccine delivery during pregnancy.Citation30 Studies outside of the UK have also found that midwife delivered maternal vaccination models are able to improve maternal vaccine uptake.Citation26,Citation27,Citation40,Citation41 Mohammed et al, reported that a midwife delivered maternal vaccine program in Australia improved uptake in a hospital populationCitation26 but studies have not reported on the impact of midwife provision on overall national maternal vaccine uptake rates.
We and others have previously identified midwives and other healthcare professionals as key influencers in women’s vaccine decisions in pregnancy.Citation14,Citation20,Citation22–25 Our evaluation supports this, given the high proportion of women who received vaccines from midwives at the clinic. Nearly twenty percent of women who declined vaccines from the clinic wanted more time to consider. Four percent of women who initially declined were vaccinated at a subsequent appointment, highlighting the importance of ongoing conversations with midwives in supporting women’s pregnancy vaccine decisions. Three of the women who participated in the qualitative interviews were categorized as ‘hesitant-compliers’, further supporting the notion that conversations with trusted midwives are important in vaccine decision making during pregnancy.Citation22–24 Consistent with our findings, previous qualitative research into vaccine decision making has also highlighted the importance of offering vaccines through non-traditional settings to overcome some parental vaccine hesitancy.Citation42 Midwives should therefore receive training and support to enable them to promote vaccination among pregnant women.Citation43,Citation44
In line with our research in 2015,Citation20 our evaluation continues to show that Black Afro-Caribbean women are less likely to be vaccinated in pregnancy, and a midwife-led service did not appear to resolve this issue. This finding is also consistent with previous studies in different international contexts.Citation12,Citation18,Citation20,Citation45 In England, Byrne et al. found that women of Black-British and Black-Afro-Caribbean ethnicity had the lowest maternal pertussis vaccine coverage and reported that deprivation was linked to low maternal vaccine coverage.Citation17 Black-Afro Caribbean women’s vaccine hesitancy might relate to wider feelings of discrimination by the healthcare system associated with ethnicity and socio-economic deprivation.Citation12,Citation24,Citation46 Further research and community engagement are required to better understand the underlying reasons. Delivery of maternal vaccines has implications beyond the perinatal period as factors underlying suboptimal childhood vaccination in England maybe similar to maternal vaccination factors.Citation17,Citation47 Attitudes toward maternal vaccines have been found to correlate with acceptancy of childhood vaccination,Citation29 and Black-Afro Caribbean ethnicity is also known to be associated with lower childhood vaccine uptake in the UK.Citation46,Citation48 Early, targeted interventions during pregnancy among ethnic minority groups with known lower vaccine uptake could therefore maximize both maternal and childhood vaccine uptake.
McAuslane et al., reported that maternal vaccine receipt in pregnancy in England was associated with ethnicity, deprivation and also parity.Citation18 We did not find that deprivation was associated with maternal vaccine uptake, however we cannot know if more deprived women were less likely to visit the vaccine clinic in the first place. In agreement with McAuslane et al., we also found that more women of higher parity declined vaccination when seen in the clinic compared to women of lower parity.
Our study has some clear limitations: we do not know the number of women vaccinated in primary care during the same time period. This is because we did not have access to the GP records of the women attending the clinic or who delivered at the hospital. Therefore, we cannot provide total vaccine uptake estimates for the whole hospital population. We can only report on the number of women who received or declined vaccines from the antenatal clinic.
Some limitations arise from the use of routine data where for example, ethnicity was not recorded in a third of the women. This may have led to over or underestimation of the association between ethnicity and vaccine receipt. However, given that this percentage is identical for all women recorded as delivering at our hospital, we believe that our sample is representative.
Our results might be subject to selection bias: women who were more likely to decline vaccinations may also have been less likely to be seen in the vaccine clinic in the first place. However, it is important to note that the vaccine midwives were actively approaching women in the antenatal clinic. Women attending the antenatal vaccine clinic could have come from more affluent backgrounds which might explain why in contrast to other studies we did not find an association between deprivation and maternal vaccination.Citation17 The number of women who participated in the qualitative interviews was small, but this is often the case in qualitative studies. Women living in more deprived areas and not speaking English as a first language were possibly less likely to have agreed to take part in the qualitative interviews.
Conclusion
In conclusion, our data supports the significant role of midwives and antenatal clinics in delivering maternal vaccination programmes. Over 40% of all women who delivered at this urban hospital received their vaccines via this antenatal clinic. Uptake in the antenatal vaccine clinic was much higher than the locally reported pertussis vaccine uptake estimates. Our evaluation therefore supports antenatal based midwife-led vaccine clinics as a model that could increase vaccination rates in pregnancy. Further work is needed to understand the relationship between ethnicity and vaccine confidence in England. Accurate tracking of antenatally delivered vaccines between hospital-based services and primary care will be essential to appreciate the full impact of novel models of vaccine delivery on uptake rates.
Ethics
The service evaluation was undertaken as service improvement work and thus ethical approval was not required. The service evaluation was registered with the Maternity Division of Imperial College Healthcare NHS Trust, registration number 242, with approval granted in January 2018. Ethical approval for the MatImms qualitative research was received from the Research Ethics Committee London – Hampstead reference: 13/LO/1712.
Supplemental Material
Download MS Word (35.2 KB)Acknowledgments
The MatImms qualitative research was funded by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London. The views expressed are those of the author and not necessarily those of the NHS, the NIHR, or the Department of Health. This work was also supported by the IMmunising PRegnant women and INfants neTwork (IMPRINT) funded by the UKRI-GCRF Networks in Vaccines Research and Development which was co-funded by the MRC and BBSRC. We are also grateful for the women who gave their time for the qualitative interviews.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/21645515.2020.1770515.
Additional information
Funding
References
- Health Protection Agency. Confirmed pertussis in England and Wales continues to increase. Health Protect Rep 2012;6:15. Available from: https://webarchive.nationalarchives.gov.uk/20140714100655/http://www.hpa.org.uk/hpr/archives/2012/news1512.htm#prtsss.
- Department of Health. “Pregnant women to be offered whooping cough vaccination” [Internet]. 2012 [accessed 2020 Feb]. Available from: https://www.gov.uk/government/news/pregnant-women-to-be-offered-whooping-cough-vaccination
- Jones C, Pollock L, Barnett SM, Battersby A, Kampmann B. Specific antibodies against vaccine-preventable infections: a mother–infant cohort study. BMJ Open. 2013 Jan 1;3(4):e002473. doi:10.1136/bmjopen-2012-002473.
- Public Health England. Vaccination against pertussis (Whooping cough) for pregnant women- 2016 Information for healthcare professionals. 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/529956/FV_JUNE_2016_PHE_pertussis_in_pregnancy_information_for_HP_.pdf.
- Donegan K, King B, Bryan P. Safety of pertussis vaccination in pregnant women in UK: observational study. BMJ. 2014;349:g4219.
- Amirthalingam G, Andrews N, Campbell H, Ribeiro S, Kara E, Donegan K, Fry NK, Miller E, Ramsay M. Effectiveness of maternal pertussis vaccination in England: an observational study. Lancet. 2014 Oct 25;384(9953):1521–28. doi:10.1016/S0140-6736(14)60686-3.
- Sukumaran L, McCarthy NL, Kharbanda EO, Vazquez-Benitez G, Lipkind HS, Jackson L, Klein NP, Naleway AL, McClure DL, Hechter RC, et al. Infant hospitalizations and mortality after maternal vaccination. Pediatrics. 2018 Mar 1;141(3). doi:10.1542/peds.2017-3310.
- Public Health England. The National Influenza Immunisation Programme 2017/18. 2017. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/600532/annual_flu_plan_2017to2018.pdf.
- Pebody RG, McLean E, Zhao H, Cleary P, Bracebridge S, Foster K, Charlett A, Hardelid P, Waight P, Ellis J, et al. Pandemic influenza (H1N1) 2009 and mortality in the United Kingdom: risk factors for death, April 2009 to March 2010. Eurosurveillance. 2010;15(20):pii=19571.
- Nunes MC, Cutland CL, Jones S, Downs S, Weinberg A, Ortiz JR, Neuzil KM, Simões EAF, Klugman KP, Madhi SA, et al. Efficacy of maternal influenza vaccination against all-cause lower respiratory tract infection hospitalizations in young infants: results from a randomized controlled trial. Clin Infect Dis. 2017 Oct 1;65(7):1066–71. doi:10.1093/cid/cix497.
- Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, Ramakrishnan U. Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: a retrospective cohort study. PLoS Med. 2011 May 31;8(5):e1000441. doi:10.1371/journal.pmed.1000441.
- Wilson RJ, Paterson P, Jarrett C, Larson HJ. Understanding factors influencing vaccination acceptance during pregnancy globally: A literature review. Vaccine. 2015;33(47):6420–29. doi:10.1016/j.vaccine.2015.08.046.
- Public Health England. Pertussis vaccination programme for pregnant women update: vaccine coverage in England, October to December 2017, Health Protection Report Vol. 12. (Number 15).
- Winslade CG, Heffernan CM, Atchison CJ. Experiences and perspectives of mothers of the pertussis vaccination programme in London. Public Health. 2017 May;1(146):10–14. doi:10.1016/j.puhe.2016.12.018.
- Public Health England. Pertussis vaccination programme for pregnant women update: vaccine coverage in England, January to March 2018. Health Protection Report. 12(Number 27).
- Public Health England. Seasonal influenza vaccine uptake in GP patients: winter season 2017 to 2018 Final data for 1 September 2017 to 31 January 2018. 2018.
- Byrne L, Ward C, White JM, Amirthalingam G, Edelstein M. Predictors of coverage of the national maternal pertussis and infant rotavirus vaccination programmes in England. Epidemiol Infect. 2018;146(2):197–206. doi:10.1017/S0950268817002497.
- McAuslane H, Utsi L, Wensley A, Coole L. Inequalities in maternal pertussis vaccination uptake: a cross-sectional survey of maternity units. J Public Health (Oxf). 2018 Mar 1;40(1):121–28. doi:10.1093/pubmed/fdx032.
- Tessier E, Warburton F, Tsang C, Rafeeq S, Boddington N, Sinnathamby M, Pebody R. Population-level factors predicting variation in influenza vaccine uptake among adults and young children in England, 2015/16 and 2016/17. Vaccine. 2018;36(23):3231–38. doi:10.1016/j.vaccine.2018.04.074.
- Donaldson B, Jain P, Holder BS, Lindsay B, Regan L, Kampmann B. What determines uptake of pertussis vaccine in pregnancy? A cross sectional survey in an ethnically diverse population of pregnant women in London. Vaccine. 2015;33(43):5822–28. doi:10.1016/j.vaccine.2015.08.093.
- Office National Statistics (ONS). Ethnicity facts and figures. List of ethnic groups [Internet]. 2020 [accessed 2020 Apr]. Available from: https://www.ethnicity-facts-figures.service.gov.uk/ethnic-groups
- Maisa A, Milligan S, Quinn A, Boulter D, Johnston J, Treanor C, Bradley DT. Vaccination against pertussis and influenza in pregnancy: a qualitative study of barriers and facilitators. Public Health. 2018;162:111–17. doi:10.1016/j.puhe.2018.05.025.
- Green D, Labriola G, Smeaton L, Falconer M. Prevention of neonatal whooping cough in England: the essential role of the midwife. Brit J Midwifery. 2017 Apr 2;25(4):224–28. doi:10.12968/bjom.2017.25.4.224.
- Wilson R, Paterson P, Larson HJ. Strategies to improve maternal vaccination acceptance. BMC Public Health. 2019;19(1):342. doi:10.1186/s12889-019-6655-y.
- Bisset KA, Paterson P. Strategies for increasing uptake of vaccination in pregnancy in high-income countries: A systematic review. Vaccine. 2018;36(20):2751–59. doi:10.1016/j.vaccine.2018.04.013.
- Mohammed H, Clarke M, Koehler A, Watson M, Marshall H, Berbers GA. Factors associated with uptake of influenza and pertussis vaccines among pregnant women in South Australia. PLoS One. 2018 Jun 14;13(6):e0197867. doi:10.1371/journal.pone.0197867.
- Krishnaswamy S, Wallace EM, Buttery J, Giles ML. Strategies to implement maternal vaccination: A comparison between standing orders for midwife delivery, a hospital based maternal immunisation service and primary care. Vaccine. 2018;36(13):1796–800. doi:10.1016/j.vaccine.2017.12.080.
- Ogburn T, Espey E, Contreras V, Arroyo P. Impact of clinic interventions on the rate of influenza vaccination in pregnant women. J Reprod Med. 2007;52:753.
- Danchin MH, Costa-Pinto J, Attwell K, Willaby H, Wiley K, Hoq M, Leask J, Perrett KP, O’Keefe J, Giles ML, et al. Vaccine decision-making begins in pregnancy: correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine. 2018;36(44):6473–79. doi:10.1016/j.vaccine.2017.08.003.
- Wilcox CR, Woodward C, Rowe R, Jones CE. Embedding the delivery of antenatal vaccination within routine antenatal care: a key opportunity to improve uptake. Hum Vaccin Immunother. 2019 Jul;24:1–4.
- Department for Communities and Local Government. The English indices of deprivation 2015. Statistical Release. 2015. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015__Statistical_Release.pdf
- Smith A. Reflecting on the development of interpretative phenomenological analysis and its contribution to qualitative research in psychology. Qual Res Psychol. 2004;1:39–54.
- Biggerstaff D, Thompson AR. Interpretative phenomenological analysis (IPA): a qualitative methodology of choice in healthcare research. Qual Res Psychol. 2008 Sep 25;5(3):214–24. doi:10.1080/14780880802314304.
- Pietkiewicz I, Smith JA, Pietkiewicz I, Smith JA. A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Czasopismo Psychol Psychol J. 2014;20:7–14.
- Public Health England. Pertussis vaccination programme for pregnant women update: vaccine coverage in England, April to June 2018. Health Protection Report Volume 12 (Number 42). 2018.
- Public Health England. Prenatal pertussis coverage estimates by area team and clinical commissioning group: england, April 2015 to March 2018. NHS West London (K&C & QPP) CCG and NHS Central London (Westminster) CCG estimates.
- Public Health England. Seasonal flu vaccine uptake in GP patients: final data 1 September 2017 to 31 January 2018, area team and CCG. NHS West London (K&C & QPP) CCG and NHS Central London (Westminster) CCG estimates.
- Webb H, Street J, Marshall H. Incorporating immunizations into routine obstetric care to facilitate health care practitioners in implementing maternal immunization recommendations. Hum Vaccin Immunother. 2014 Apr 28;10(4):1114–21. doi:10.4161/hv.27893.
- Wilcox CR, Little P, Jones CE. Current practice and attitudes towards vaccination during pregnancy: a survey of GPs across England. Brit J General Pra. 2020 Mar 1;70(692):e179LP–e185. doi:10.3399/bjgp20X708113.
- Taksdal SE, Mak D, Joyce S, Tomlin S, Carcione D, Armstrong P, Effler P. Predictors of uptake of influenza vaccination A survey of pregnant women in Western Australia. Aus Family Phy. 2013 Aug;1(42):582–86.
- Alessandrini V, Anselem O, Girault A, Mandelbrot L, Luton D, Launay O, Goffinet F. Does the availability of influenza vaccine at prenatal care visits and of immediate vaccination improve vaccination coverage of pregnant women? PLoS One. 2019 Aug 1;14(8):e0220705–e0220705. doi:10.1371/journal.pone.0220705.
- Attwell K, Smith DT, Ward PR. ‘The unhealthy other’: how vaccine rejecting parents construct the vaccinating mainstream. Vaccine. 2018;36(12):1621–26. doi:10.1016/j.vaccine.2018.01.076.
- Vishram B, Letley L, Jan Van Hoek A, Silverton L, Donovan H, Adams C, Green D, Edwards A, Yarwood J, Bedford H, et al. Vaccination in pregnancy: attitudes of nurses, midwives and health visitors in England. Hum Vaccin Immunother. 2018 Jan 2;14(1):179–88. doi:10.1080/21645515.2017.1382789.
- Ntouva A, Sibal B. RE: ‘Vaccination against pertussis and influenza in pregnancy: a qualitative study of barriers and facilitators’. Public Health. 2019. doi:10.1016/j.puhe.2019.03.017.
- Lu P, O’Halloran A, Williams WW, Lindley MC, Farrall S, Bridges CB. Racial and ethnic disparities in vaccination coverage among adult populations in the U.S. Am J Prev Med. 2015/08/18. 2015 Dec;49(6 Suppl 4):S412–25. doi:10.1016/j.amepre.2015.03.005.
- Forster AS, Rockliffe L, Chorley AJ, Marlow LAV, Bedford H, Smith SG, Waller J. Ethnicity-specific factors influencing childhood immunisation decisions among black and asian minority ethnic groups in the UK: a systematic review of qualitative research. J Epidemiol Community Health. 2017 Jun 1;71(6):544LP– 549. doi:10.1136/jech-2016-207366.
- Tickner S, Leman PJ, Woodcock A. Factors underlying suboptimal childhood immunisation. Vaccine. 2006;24(49):7030–36. doi:10.1016/j.vaccine.2006.06.060.
- Samad L, Tate AR, Dezateux C, Peckham C, Butler N, Bedford H. Differences in risk factors for partial and no immunisation in the first year of life: prospective cohort study. BMJ (Clinical Research Ed). 2006 Jun 3;332(7553):1312–13. doi:10.1136/bmj.332.7553.1312.