ABSTRACT
The Coronavirus Disease 2019 (COVID-19) pandemic has been growing, including in Japan where it has been estimated that as many as 3.1% of patients positive for new CoV strain SARS-CoV-2 might die of COVID-19-related respiratory failure. Meanwhile, human papillomavirus (HPV) is spreading in Japan. The fatality rate for HPV-associated cancers after infection with HPV is as much as that for COVID-19 in Japan, although the time to disease is much longer for HPV. Among advanced countries, the cervical cancer screening rate in Japanese females is very low. The Japanese Ministry of Health, Labor and Welfare (MHLW) suspended its official recommendation for HPV vaccination in June 2013 due to alleged adverse post-vaccination events in several young girls, such as chronic pain and motor impairment, which were repeatedly reported in the media. Subsequently, the rate for vaccinating girls plummeted from approximately 70% to the current rate of 1% or less. Women should accept HPV vaccination for the eventual prevention of cervical cancer with the same passion they are for COVID-19 testing.
The Coronavirus Disease 2019 (COVID-19) pandemic has been growing, including in Japan where it has been estimated that as many as 3.1% of patients positive for SARS-CoV-2 might die of COVID-19-related respiratory failure.Citation1 The emergence of this virus in Japan led to a declared state of emergency, and most Japanese are taking active preventative measures against infection by wearing a mask, disinfecting their hands and refraining from going out.
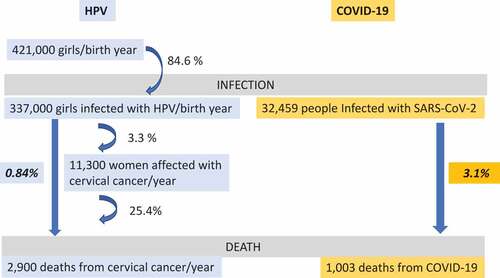
Meanwhile, the human papillomavirus (HPV) continues spreading in Japan. According to the Japanese Ministry of Health, Labor and Welfare (MHLW), 421,000 girls were born in 2019.Citation2 Given that about 84.6% of woman will acquire one or more HPV infections in their lifetime,Citation3 337,000 girls born each year will eventually become HPV infected and 11,300 of these women will be diagnosed with cervical cancer each year.Citation4 Given that HPV infection occurs prior to essentially cases of cervical cancer, the incidence rate of cervical cancer among HPV-infected females is calculated as 3.3%. In 2016, the number of diagnosed cases of cervical cancer and the number of deaths from cervical cancer were 11,283 and 2,871, respectively, Citation4 indicating that the fatality rate of cervical cancer was roughly 25%. Thus, the long-term fatality rate for cervical cancer is calculated as 0.84%, relative to the 3.1% fatality for COVID-19 ().Citation5 Thus, the fatality rate from cervical cancer after infection with HPV is within an order of magnitude of that for SARS-CoV-2 in Japan. How many women know this shocking fact? Few people are afraid enough of HPV infection to routinely abstain from sexual relations, even though it can lead to cervical cancer. Among advanced countries, the cervical cancer screening rate in Japanese females is very low. Should women not be vaccinated for eventual prevention of cervical cancer with the same rigor as they are for COVID-19 testing?
By contrast to HPV, people are afraid of COVID-19, abstaining from going out so as to not get infected, and waiting for the development of a vaccine. These are, in a sense, inevitable behaviors that can be explained by concepts that form the basis of behavioral economics, including availability heuristic and present bias.Citation6 For example, the number of deaths, and especially the deaths of celebrities, from COVID-19 is reported daily in stern tones. Everyone is aware that respiratory distress, and occasional death, can occur within days or weeks after infection with the new CoV strain. On the other hand, HPV infection progresses slowly and silently over many years and can lead to cervical cancer and death. This type of slow death has rarely been reported in Japanese media. Thus, Japanese females have little knowledge of death from HPV infection and cervical cancer.
In Japan, public subsidies for HPV vaccinations began in 2010. In 2013, HPV vaccination became a part of the national routine vaccination program for all girls aged 12–16. However, alleged adverse post-vaccination events in several young girls, such as chronic pain and motor impairment, were repeatedly reported in our media, and the Japanese MHLW suspended its official recommendation for HPV vaccination in June 2013.Citation7 Subsequently, the rate for newly vaccinated girls plummeted from approximately 70% to the current rate of 1% or less.Citation8 Because of a lack of protective HPV vaccination for 7 y, it follows that a strong trend for an increased rate of cervical cancer will inevitably follow in the future.
Fortunately, the MHLW recently started internal discussions for regulatory approval of the 9-valent HPV vaccine (effective against nine types of HPV), which should prevent around 90% of cervical cancers. We believe that this approval will also lead to approval of HPV vaccination for boys and that the governmental recommendation will be resumed as soon as possible. We send our deepest appreciation to the MHLW for persistently working to prevent cervical cancer with the HPV vaccine, while still devoting so much effort to fighting COVID-19.
We gynecologists should disseminate appropriate information to our patients and their families so that Japanese women can overcome their cognitive biases and properly understand the susceptibility to and severity of cervical cancer relative to COVID-19, and act on this understanding by taking HPV vaccine.
Abbreviations
| COVID-19 | = | Coronavirus Disease 2019 |
| HPV | = | human papillomavirus |
| MHLW | = | Ministry of Health, Labor and Welfare |
Ethical statement
This study was approved by the Institutional Review Board and Ethics Committee of the Osaka University Medical Hospital.
Acknowledgments
We would like to thank Dr. G. S. Buzard for his constructive critique and editing of our manuscript.
References
- [ Cited on July 31, 2020] The Ministry of Health. Labour and Welfare. https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html
- [Cited on April 25, 2020] The Ministry of Health. Labour and Welfare. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/suikei19/index.html
- Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex Transm Dis. 2014;41:660–64. doi:10.1097/OLQ.0000000000000193.
- [ cited April 25, 2020]. https://ganjoho.jp/reg_stat/statistics/stat/summary.html
- The Ministry of Health, Labour and Welfare. [accessed 2020 Jul 31]. https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html
- Yagi A, Ueda Y, Kimura T. A behavioral economics approach to the failed HPV vaccination program in Japan. Vaccine. 2017;35:6931–33. doi:10.1016/j.vaccine.2017.10.064.
- The Ministry of Health. Labour and Welfare. [ cited April 25, 2020]. http://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou28/pdf/kankoku_h25_6_01.pdf
- Ikeda S, Ueda Y, Yagi A, Matsuzaki S, Kobayashi E, Kimura T, Miyagi E, Sekine M, Enomoto T, Kudoh K. HPV vaccination in Japan: what is happening in Japan? Expert Rev Vaccines. 2019;18:323–25. doi:10.1080/14760584.2019.1584040.