ABSTRACT
Aim
This study aims to determine the causes of vaccine mistrust among family healthcare professionals (FHP) in the unit where they serve and vaccine hesitancy of families.
Method
The study group consisted of 682 FHPs working in a primary health care institution. The data collection tools of the study included a sociodemographic data form and a vaccine hesitancy data form. Pearson’s chi-square analysis and logistic regression analysis were performed to analyze the data.
Findings
To the question of “Do you trust the active ingredient in the vaccines?”, only 2.1% of FHPs responded “I do not trust” and 18.9% answered “I am indecisive”. 70.7% of FHPs said that at least one vaccine hesitant family was in the unit where they served. The most important reasons stated by FHPs on behalf of such families were vaccine mistrust (73.2%), the belief that they may be harmful for the child (58.7%), and the belief that vaccines cause autism (55.6%). In the univariate analysis, vaccine mistrust was significantly higher in FHPs who were measles-hesitant and responded “The decision to get vaccinated or not should belong to the family voluntarily”. From logistic regression analysis, vaccine mistrust in FHPs increased 2.8-fold for those who did not think vaccination should be compulsory, 2.7-fold for those who did not think that vaccination refusal should be legally enforced, and 1.61-fold for those under age 35 years.
Conclusion
It was observed that FHPs had high sensitivity and positive attitudes toward vaccination in general.
Introduction
Vaccine hesitancy is defined by The SAGE Working Group on Vaccine Hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccination services.”Citation1 Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines. It is influenced by various factors, including complacency, convenience, and confidence.Citation1 In 2019, the World Health Organization (WHO) stated that vaccine hesitancy and refusal are among the top 10 global health threats and must be resolved.Citation2 WHO data showed that there were 142,300 measles-related deaths in worldwide 2018, and most of those cases were children under 5 who were not vaccinated.Citation3 It was also reported that the number of measles cases in 2019 was approximately 3 times higher than in the previous year and that the situation was getting worse. Vaccine hesitancy and refusal are among the most important causes of the global measles outbreakCitation2,Citation3 and have been increasing in the community and in families worldwide.Citation4–Citation6 Vaccine hesitancy has been reported in >90% of countries in the world.Citation7 The percentage of families with vaccine hesitancy is estimated to be between 25% and 70% in France,Citation8 19% in Canada,Citation9 and 20% in Saudi Arabia.Citation10 In a study conducted with a large sample in Europe, it was found that 20% of European families delay vaccinations, 12% refuse them, and 28% are hesitant; however, vaccine hesitancy rates vary across countries, ranging between 9% and 42% in selected European countries.Citation11 To prevent and reduce vaccine hesitancy, it is necessary to identify its causes.Citation4 The reasons for vaccine hesitancy among families are complex. The three most important causes of vaccine hesitancy worldwide are 1) the risk–benefit ratio of the vaccine, taking into account “vaccine safety concerns” and “fear of side effects”; 2) the lack of knowledge and awareness of vaccination and its importance; and 3) religion, culture, gender and socioeconomic issues regarding vaccines.Citation12 Similarly, in their study, Topçu et al. showed that the main causes of vaccine refusal by families were “vaccine safety concerns,” “fear of side effects,” and lack of trust in providers in Turkey.Citation13
The number of unvaccinated children has also significantly increased in Turkey.Citation14 In 2015, a family filed a lawsuit against mandatory vaccination; the parents wanted the right to grant or withhold consent to vaccinate their children and, after winning the lawsuit, did not have their children vaccinated. This situation was reported in newspapers and on social media as a victory for the parents. Following this, groups led by many religious and philosophically active people increased their anti-vaccination discourse. Within this social environment, vaccine hesitancy has shown a significant increase in Turkey, as many parents have decided not to vaccinate their children, refusing to give their consent.Citation15According to data from the Ministry of Health, the number of families who refused to have their children vaccinated was 183 in 2011, 12,000 in 2016, and 23,600 in 2017.Citation14 According to data from the Turkey Demographic and Health Survey 2018, the rate of 12-to-23-month-old children with full vaccination decreased from 74% in 2013 to 67% in 2018, and there is a concern that this rate may further decrease.Citation16
In the national immunization program of Turkey, vaccines are given only to pregnant or pediatric patients. Vaccination services are among the core duties of family healthcare professionals (FHPs). The Expanded Program on Immunization in Turkey aims to ensure that all children can be vaccinated free of charge against diphtheria, pertussis, tetanus, measles, tuberculosis, poliomyelitis, hepatitis B, rubella, mumps, pneumococcal and haemophilus influenzae type b infections, hepatitis A, and chickenpox. Pediatric vaccines against influenza, meningococcal disease, and rotavirus are recommended to families and administered optionally. In Turkey, diphtheria, polio, and maternal and neonatal tetanus have been eliminated via an effective vaccination program.Citation17According to the WHO, the number of measles cases in our country was 2890 in 2019.Citation18 The incidence of some vaccine-preventable diseases (mumps, rubella, pertussis) is below 1/100,000.Citation19
The most important factor affecting vaccination behavior is trust in vaccines. Healthcare professionals play an important role in ensuring trust in vaccines and the success of immunization services. While healthcare professionals are among the most reliable sources of information about vaccines in the community, some healthcare professionals are reported to have lost confidence in vaccines.Citation6 Although healthcare professionals are taught the importance of vaccination in the reduction of mortality and morbidity in vaccine-protected diseases and the fight against infectious diseases, as well as the success achieved via vaccines (eradication of smallpox, elimination of polio and tetanus, etc.), the question of why healthcare professionals do not trust vaccines has become an increasingly important research topic. Compared to individuals in the community, healthcare professionals are expected to have more evidence-based information in vaccines.Citation6,Citation20,Citation21 Healthcare professionals’ perceptions of the benefits and safety of vaccines should be evaluated not only as a measure of their attitudes toward vaccines, but also as an indicator of their vaccine-related information.Citation22 According to the relevant literature, the trust of healthcare professionals in vaccines directly affects their behavior and willingness to recommend vaccines to their patients and those they serve.Citation22,Citation23
The findings of the WHO and many studies by other groups emphasize that the knowledge and attitudes of healthcare personnel play a key role in the success of vaccination services.Citation20,Citation24 In their systematic review, Rainey et al. found that the most important reasons for the non-vaccination of society in middle- and low-income countries were the inaccurate and inadequate knowledge of healthcare workers and their apathy to vaccination.Citation24 Some studies stated that healthcare workers lack information about vaccines, especially the safety of vaccines.Citation25,Citation26 Healthcare workers are the most effective and reliable source of information for immunization services,Citation6,Citation20,Citation21,Citation24 and their positive attitudes toward vaccination have a strong effect on its success.Citation23 Healthcare workers with vaccine hesitancy may provide less information about vaccines to others, and their attitudes and behavior may contribute to vaccine hesitancy and reduce confidence in vaccines. Moreover, they may less willing to vaccinate. These factors can have a strong impact on parents’ decision not to vaccinate.Citation6,Citation20,Citation23
We lack information about the causes of vaccine hesitancy in families in Turkey,Citation13 where vaccination rates have been decreasingCitation16 and the number of families with vaccine hesitancy has been increasing.Citation14 To overcome this, the causes of vaccine hesitancy should be determined, vaccine hesitancy should be monitored at the local and national levels, and strategies should be developed to increase vaccine acceptance.Citation27
It is known that vaccine hesitancy has been increasing among healthcare professionals. Therefore, increasing trust in vaccines among healthcare professionals and determining and monitoring the factors influencing vaccine hesitancy will be important for the development of interventions and for conducting studies in future. The aims of the study are as follows;
To determine the factors affecting FHPs’ trust in the content of pediatric vaccines.
To determine the frequency of vaccine-hesitant families in various regions in Turkey based on statements from FHPs serving those regions.
Methods
Setting and sample
Due to the implementation of free-of-charge immunization services by FHPs at family medicine departments in Turkey, FHPs constitute the study group. Primary healthcare services in Turkey are the responsibility of family physicians. There are 26,252 Family Medicine Units in 7979 Family Healthcare Centers (FHCs) in Turkey.Citation28 Each FHC consists of a physician and an FHP, a healthcare professional with the title of midwife, nurse, emergency medicine technician, or medical officer working in the family medicine system. The FHPs Federation is a national federation that protects and promotes all FHP rights. The main aim of the FHPs Federation is to ensure coordination and integrity in the health system in order to improve and support the service.
The study population consisted of FHPs (N = 26,252) working in Family Medicine Units in Turkey. For this cross-sectional study, the sample size goal was at least 379 people with 50% unknown prevalence, 1% absolute deviation, and 95% confidence level. This sample size was calculated on OpenEpi, Version 3, an open source calculator.Citation29 A total of 682 FHPs from different regions of Turkey completed the study.
Measurements/instruments
The data included two sections: a socio-demographic data form and a healthcare professionals’ hesitancy data form.Citation6,Citation8,Citation10,Citation20–Citation23 Sociodemographic questions included age, title, year of employment, educational background, and the average number of pregnant women and infants/children followed up each month. Questions on the vaccine hesitancy form included FHPs’ influenza vaccination status within the past year, time since last tetanus vaccine, attitude toward measles vaccination in a measles outbreak, their child(ren)’s vaccination status according to the national vaccination schedule, whether they trust the content of vaccines, and the presence of vaccine-hesitant parents in the family healthcare unit where they serve. In addition, 5 questions regarding opinions about the vaccines were asked in the form of 3-point Likert-type scale (“I agree,” “I disagree,” and “I have no idea”).
Data collection/procedure
Data were collected with an online survey via Google Form. The survey was shared electronically using Google Drive’s online service system (https://docs.google.com/forms/d/1QYtU3GqOA4hP4sjLKCVKXsquQ34rIqmotZjmQmMWPo/edit), with the link sent to the federation and to e-mail addresses of individuals. The survey was announced 5 times on WhatsApp communication groups or via e-mail between November and December 2019. Individuals with access to the survey link completed the survey. The data were downloaded in csv format and were analyzed after being revised and standardized.
Data analysis
Statistical analysis was performed using SPSS 20.0 statistical software. Descriptive statistics were presented as mean, standard deviation, number, and percentage. The dependent variable of the study was trust in vaccines, which was determine using the question “Do you trust the content of pediatric vaccines?” with the answers classified as dichotomous data into “Yes” or “No”/“uncertain”. The independent variables of our study were the views of FHPs about vaccination. The answers were coded dichotomously as “Agree” or “Disagree”/“Undecided.” Measles vaccination attitude was coded as ‘‘I do” or ‘‘I do not’’; tetanus vaccination status as “<10,” or “10ʹ’; age as ‘‘<35ʹ’ or ‘‘≥35ʹ’; vaccine-hesitant family presence in the family healthcare unit where they work as ‘‘yes’’ or ‘‘no’’; and educational status as ‘‘high school,’’ ‘‘university,’’ or “postgraduate.’’ Factors related to FHPs’ trust in vaccines were evaluated by Pearson’s chi-square analysis. Logistic regression analysis incorporating independent variables that were significant in the univariate analysis was used to predict trust in vaccines. Independent variables included in the regression analysis were: age; attitude toward measles vaccination; thinking that vaccines should be mandatory; thinking that being vaccinated should be voluntary; thinking that vaccination refusal should be punishable by imprisonment or high fines; believing that adequate information and counseling is provided in the unit worked; and providing explanations that vaccinating families not only protects themselves, but also protects the society. The enter method was applied for logistic regression analysis and odds ratio (OR) values were presented with the 95% confidence interval (CI 95%). If the p-value was less than 0.05, the difference was considered statistically significant.
Ethics
This study was conducted in accordance with the principles of the World Medical Association Helsinki Declaration. Permission was obtained from the Balıkesir University Faculty of Medicine Clinical Research Ethics Committee (Date: August 7, 2019; 2019/90) and the institution where the application was conducted.
Findings
Of the 682 FHPs who completed the study, 42.2% were between 35 and 44 years old. In addition, 64.22% of them were midwives, 81.1% were university graduates, and 34.9% had worked for 10–20 years (). The average number of 0-to-59-month-old children followed by FHPs was 199.35 ± 147.53 and the average number of pregnant women followed was 29.54 ± 19.29. The number of FHPs participating in the study was higher in regions with a high population density: 17.4% of respondents were from Istanbul (Turkey’s largest city), 18.1% from the Marmara Region, 22.2% from the Aegean Region, 9.1% from the Eastern Region, 12% from the South region, 7.2% from the North region, and 12.7% from the Central Anatolian region.
Table 1. The descriptive statistics of FHPs (midwife, nurse, emergency medicine technician, or medical officer) in Turkey in 2019 (n = 682)
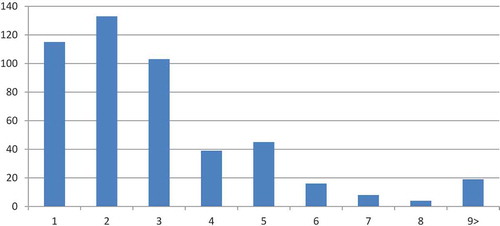
Of the FHPs who participated in the study, 15.8% stated that they had received a seasonal influenza vaccine in the last year and 76.4% had received a tetanus vaccine in the last 10 years. To the question of whether they would be vaccinated if a measles outbreak occurred, 59.1% of FHPs responded “I will get vaccinated,” whereas 2.4% answered “I will not get vaccinated” and 4.7% said “I have no idea.” Only 3 (0.5%) of the FHPs stated that they did not vaccinate their children. To the question “Do you trust the active ingredient in the vaccine?”, 2.1% answered “I do not trust” and 18.9% responded “I have no idea.” For 70.7% of the FHPs, there was at least one vaccine-hesitant family in the unit where they served (.). shows the number of vaccine-hesitant families.
Table 2. Vaccination status and attitudes of family healthcare professionals toward some vaccines in Turkey in 2019 (n = 682)
Upon examination of the reasons identified by FHPs who stated that there was at least one vaccine-hesitant family in the unit they served, it was seen that the most important reasons were vaccine mistrust (73.2%), the belief that vaccines may be harmful to children (58.7%), the belief that vaccines may cause autism (55.6%), information pollution in media/communication (40.2%), and religious causes (39.2%; ).
Table 3. The reasons for vaccine hesitancy in vaccine-hesitant families according to FHPs’ statements (n = 482)
Some of the FHPs’ attitudes toward vaccination are presented in . Of the FHPs, 12.6% stated that “the decision to get vaccinated or not should belong to the family voluntarily” and 97.5% declared that “I explain to families that vaccination protects not only themselves but also the society.” In addition, 94.4% expressed that “sufficient information and counseling are provided in the unit I work,’’ 87.1% stated ‘‘I think vaccines should be compulsory,’’ and 73.9% responded that “there must be legal sanctions that involve imprisonment or high fines for vaccine refusal” ().
Table 4. Some of the views of FHPs toward vaccination (n = 682)
Vaccine mistrust was significantly higher among the FHPs who responded “I will not get vaccinated if there is a measles outbreak” and “the decision whether to get vaccinated or not should belong to the family voluntarily” (p < .05). Vaccine content mistrust was significantly higher in young (<35) FHPs who responded “I do not agree” with the statement “I explain to families that vaccination protects not only themselves but also the society,” who stated that there is not enough information and counseling about vaccines in the unit where they work, who thought that vaccines should not be compulsory, and who believed that there should not be legal sanctions against vaccination refusal (p < .05; ).
Table 5. Factors affecting FHPs’ trust in vaccine content (n = 628)
Among the independent variables included in the logistic regression model to determine the factors affecting the trust of the healthcare professionals in the content of vaccines, vaccine mistrust increased 2.78 times (CI 95% 1.45–5.31) for those who did not think vaccination should be compulsory, 2.68 times (CI 95% 1.64–4.37) for those who did not think that vaccination refusal should be legally enforced, and 1.61 times for those under 35 (CI 95% 1.06–2.45; ).
Table 6. Factors affecting FHPs’ trust in vaccines according to logistic regression analysis
Discussion
In our study, the variables affecting FHPs’ trust in vaccines were examined. We also asked FHPs about the presence of families with vaccine refusal in the units in which they serve and the reasons for vaccine hesitancy of FHPs. A causal relationship with the vaccine-hesitant parent was not evaluated cross-sectionally in this study. The reasons for vaccine hesitancy among families were presented as descriptive data. The most important findings of this study were the existence of FHPs who did not trust the content of the vaccines and stated that they had concerns about the content of vaccines.
In our study, the rate of influenza vaccination in healthcare professionals was found to be low. However, this finding is similar to others in the literature, and it has been reported in many European countries that the influenza vaccination rate among healthcare professionals is between 15% and 29%.Citation30
Nearly two-thirds of the FHPs reported that they had received a tetanus vaccination in the past decade. According to the literature, tetanus immunity appears to be quite good. According to the systematic review by Randi et al., the Tdap (Tetanus, diphtheria, pertussis) vaccination rate among healthcare workers varies between 6.1% and 66.8%.Citation31 In family health centers in Turkey, a tetanus toxoid vaccine is routinely administered to pregnant women. The positive attitude of healthcare professionals toward vaccination has a strong effect on the success of vaccination.Citation20
FHPs can be both a risk group for measles and a source of infection for patients and the community. In our study, approximately one-fifth of the FHPs had received a measles vaccine; thus, the measles vaccination rate among participants in our study is quite low. In France, the measles vaccination rate for nurses is 63%.Citation26 More than half of the FHPs were not immune to measles. The FHPs responding as not having received a measles vaccine was 2.4%. In France, the MMR (Measles, Mumps and Rubella) vaccine hesitancy rate has been reported to be 1.6% in nurses.Citation32 In Hungary, vaccine hesitancy was reported to be the highest for the MMR vaccine (compared to other vaccines) among healthcare professionals.Citation33 Because measles has extremely high infectiousness, monitoring of measles immunization rates of healthcare professionals in Turkey is important.
Among the reasons for vaccine refusal reported by the healthcare professionals in the family healthcare units, the most important are vaccine mistrust, the belief that they may be harmful for the child, the belief that vaccines may cause autism, exposure to information pollution in media/communication, and religious reasons. The primary reason for most vaccine refusals reported by healthcare professionals in Europe is the fear of the side effects.Citation6 Similar to the aforementioned studies, the causes of vaccine hesitancy reported by families in Saudi Arabia were concerns related to vaccine safety, fear of side effects, and the belief that the MMR vaccine causes autism.Citation10 The most important reasons in Italy have been reported to be insufficient information, fear of side effects, and doubts of the efficacy of the vaccine.Citation34 In their studies conducted on families who refuse vaccines in different regions in Turkey, Topçu et al. found that the most important reasons for vaccine refusal were the perceived danger of vaccines for children and mistrust in the vaccines, similar to our findings.Citation13 However, unlike our study, the other important reasons they identified were that families believe in natural immunization and that there is no benefit of vaccines, reasons that are related to the higher use of alternative medicine by hesitant families.Citation13
It has been reported that some of the FHPs lost their trust in vaccines. Although the hesitancy rates of FHPs are generally low, the effects on patients may be significant.Citation35 In European Union countries, trust in general practitioners has been reported to vary from vaccine to vaccine and from vaccines in general to measles and influenza vaccines. Healthcare professionals who have vaccine mistrust may be less likely to increase community confidence in vaccines and recommend vaccination to patients and may also be less likely to choose to vaccinate themselves and their children.Citation36 Vaccine mistrust has been reported to be the most important cause of vaccine hesitancy among FHPs. Vaccine mistrust can cause hesitancy among professionals against certain vaccines. In this case, it negatively affects healthcare professionals’ attitudes and behaviors toward recommending vaccinations to society and families.Citation35
Healthcare professionals who do not trust vaccines will have more negative attitudes and behavior toward being vaccinated and will not support the compulsory application of vaccines and sanctions on this issue. Factors affecting healthcare professionals’ trust in vaccines were found to be associated with having a negative opinion of vaccines. It has been shown that health professionals’ having correct information increases their trust in the content of the vaccine. Some studies revealed that health professionals lack information about vaccines, especially about the safety of vaccines. In a study conducted on general practitioners in France, it was found that vaccination controversies were more common in those who obtained information about vaccines from mass media.Citation37 Another factor that affects trust in vaccines is age: Vaccine mistrust is significantly higher in healthcare professionals under the age of 35. Similarly, in the literature, mistrust and hesitancy are higher in young age groups. It is thought that this may be due to young FHPs’ lack of awareness and knowledge about vaccines and vaccine-preventable diseases and the lack of information on immunization and vaccine-preventable diseases in undergraduate curricula. In contrast to our findings, general practitioners’ vaccination hesitancy were found to be more common in the older age group in France.Citation36 In addition, in their study, Massot and Epaulard found that young midwives had greater trust toward vaccination than older midwives.Citation37
According to the findings of the qualitative study by the European Center for Disease Prevention and Control, the main reason for vaccine mistrust among healthcare professionals was found to be mistrust in the government, authorities in the field of healthcare, physicians, and the pharmaceutical industry. Citation38
Although there was substantial trust in the authorities, the government, and the WHO in Romania, a considerable degree of mistrust in the pharmaceutical industry existed among FHPs, as they believed that the companies prioritize financial issues instead of public health, conceal side effects, and pressure physicians. Similarly, Greece is among the countries where mistrust in institutions are very common. Physicians in Greece had similar opinions to their Romanian counterparts in terms of mistrust in companies, the government, and the health system.Citation38 In a study conducted in healthcare providers in Canada, a significant mistrust in vaccine recommendations by pharmaceutical companies and legal authorities was expressed by FHPs, and they were particularly skeptical of adult vaccination.Citation39
Factors affecting vaccine hesitancy include lack of responsibility, social pressure, and the feeling of autonomy. In addition, doubts about the pros and cons of vaccination are important reasons for the low vaccination rates among healthcare workers.Citation40
Our study has several strengths. The reasons for vaccine hesitancy of the families being served by FHPs in Turkey were determined. It is the first study to determine the causes of vaccine hesitancy with such broad participation in Turkey. It also enabled the determination of the behaviors, attitudes, and opinions of FHPs about vaccination. This study may contribute to future studies and inform public healthcare experts who are monitoring, evaluating, and developing strategies for vaccine hesitancy. The findings of this study are also important for their potential contribution to the development of the hypotheses of future qualitative studies.
The most important limitation of the study is that it was cross-sectionally conducted in FHPs in Turkey. Therefore, the data are not thought to reflect the data of Turkey. In addition, it is thought that FHPs who are more sensitive about vaccine hesitancy have answered at a higher rate. Another important limitation is that there is no comparison between regions. Further prospective and qualitative studies are needed to address these limitations.
It was observed that the FHPs had a high awareness of vaccination and had a positive opinion in general. According to the FHPs, the most important causes of vaccine hesitancy in the family healthcare units they served were vaccine mistrust, the belief that vaccination may be harmful, and the belief that vaccines may cause autism. Vaccine mistrust was significantly higher in younger FHPs who thought that vaccines should not be mandatory and that there should be no sanctions for vaccination.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Authors’ contributions
SY participated in the design of the study, acquisition of data, performed the statistical analysis and drafted the manuscript. HT, AD and ME participated in acquisition of data. All authors read and approved the final manuscript.
Acknowledgments
We are grateful to all the participants who kindly agreed to participate in our survey.
Additional information
Funding
References
- MacDonald NE. SAGE working group on vaccine hesitancy.Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;14;33(34):4161–64. doi:https://doi.org/10.1016/j.vaccine.2015.04.036.
- World Health Organization: WHO. [Internet]. Ten threats to global health in 2019. [ accessed 2020 Feb 27]. https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019
- World Health Organization: WHO. [Internet]. More than 140,000 die from measles as cases surge worldwide. [ accessed 2020 Feb 27]. https://www.who.int/news-room/detail/05-12-2019-more-than-140-000-die-from-measles-as-cases-surge-worldwide
- Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhouc Y, Dube E, Schuster M, MacDonald NE, Wilson R. The SAGE working group on vaccine hesitancy. measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165–75. doi:https://doi.org/10.1016/j.vaccine.2015.04.037.
- Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ. The SAGE working group on vaccine hesitancy. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33:4180–90. doi:https://doi.org/10.1016/j.vaccine.2015.04.040.
- Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, Suk J, Celentano LP, Kramarz P, Larson HJ. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34(41):5013–20. doi:https://doi.org/10.1016/j.vaccine.2016.08.029.
- Lane S, MacDonald EN, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF joint reporting form data-2015–2017. Vaccine. 2018;36(26):3861–67. doi: 10.1016/j.vaccine.2018.03.063.
- Ward JK, Peretti-Watel P, Bocquier A, Seror V, Verger P. Vaccine hesitancy and coercion: all eyes on France. Nat Immunol. 2019;20(10):1257–59. doi:https://doi.org/10.1038/s41590-019-0488-9.
- Shen SC, Dubey V. Addressing vaccine hesitancy: clinical guidance for primary care physicians working with parents. Can Fam Physician. 2019;65:175–81.
- Alsubaie SS, Gosadi IM, Alsaadi BM, Albacker NB, Bawazir MA, Bin-Daud N, Almanie W, Alsaadi M, Alzamil F. Vaccine hesitancy among Saudi parents and its determinants. Result from the WHO SAGE working group on vaccine hesitancy survey tool. Saudi Med J. 2019;40(12):1242–50. doi:https://doi.org/10.15537/smj.2019.12.24653.
- Hadjipanayis A, van Esso D, Del Torso S, Dornbusch HJ, Michailidou K, Minicuci N, Pancheva R, Mujkic A, Geitmann K, Syridou G. Vaccine confidence among parents: large scale study in eighteen European countries. Vaccine. 2020;38(6):1505–12. doi:https://doi.org/10.1016/j.vaccine.2019.11.068.
- Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF joint reporting form data-2015–2017. Vaccine. 2018;36(26):3861–67. doi: 10.1016/j.vaccine.2018.03.063.
- Dubé E. Addressing vaccine hesitancy: the crucial role of healthcare providers. Clin Microbiol Infect. 2017;23(5):279–80. doi:https://doi.org/10.1016/j.cmi.2016.11.007.
- Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine. 2014 27;32(38):4860–65. doi:https://doi.org/10.1016/j.vaccine.2013.11.006.
- Karlsson LC, Lewandowsky S, Antfolk J, Salo P, Lindfelt M, Oksanen T, Kivimäki M, Soveri A. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among Finnish healthcare workers. PLoS One. 2019;14(10):e0224330. doi:https://doi.org/10.1371/journal.pone.0224330.
- Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL. Larson HJ vaccine hesitancy and healthcare providers. Vaccine. 2016 20;34(52):6700–06. doi:https://doi.org/10.1016/j.vaccine.2016.10.042.
- Topçu S, Almış H, Başkan S, Turgut M, Orhon FŞ, Ulukol B. Evaluation of childhood vaccine refusal and hesitancy intentions in Turkey. Indian J Pediatr. 2019;86(1):38–43. doi:https://doi.org/10.1007/s12098-018-2714-0.
- Hacettepe University Institute of Population Studies. 2018 Turkey demographic and health survey. Ankara: Hacettepe University Institute of Population Studies, T.R. Presidency of Turkey Directorate of Strategy and Budget and TÜBİTAK; 2019.
- Turkish Medical Association. [Internet]. Sağlık Bakanlığı’nı Aşılama Konusunda Göreve Davet Ediyoruz! – TTB Halk Sağlığı Kolu. [ accessed 2020 January 12]. http://www.ttb.org.tr/halk_sagligi/2018/04/13/saglik-bakanligini-asilama-konusunda-goreve-davet-ediyoruz/
- World Health Organization: WHO. [Internet]. Improving vaccination demand and addressing hesitancy. [ accessed 2020 Jan 12]. https://www.who.int/immunization/programmes_systems/vaccine_hesitancy/en/
- OpenEpi Menu [Internet]. Openepi.com. 2020 [accessed 15 March 2020]. http://www.openepi.com/Menu/OE_Menu.htm
- Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum Vaccin Immunother. 2018;14(3):772–89. doi:https://doi.org/10.1080/21645515.2017.1348442.
- Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. 2017;26;12:e0170550.
- Ishola DA Jr, Permalloo N, Cordery RJ, Anderson SR. Midwives’ influenza vaccine uptake and their views on vaccination of pregnant women. J Public Health. 2013;35:570–77. doi:https://doi.org/10.1093/pubmed/fds109.
- Randi BA, Sejas ONE, Miyaji KT, Infante V, Lara AN, Ibrahim KY, Lopes MH, Sartori AM. A systematic review of adult tetanus-diphtheria-acellular (Tdap) coverage among healthcare workers. Vaccine. 2019;37(8):1030–37. doi:https://doi.org/10.1016/j.vaccine.2018.12.046.
- Wilson R, Zaytseva A, Bocquier A, Nokri A, Fressard L, Chamboredon P, Carbonaro C, Bernardi S, Dubé E, Verger P, et al. Vaccine hesitancy and self-vaccination behaviors among nurses in southeastern France. Vaccine. 2020;38(5):1144–51. doi:https://doi.org/10.1016/j.vaccine.2019.11.018.
- World Health Organization. Measles and rubella surveillance data. [accessed 2020 Mar 16]. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/
- Kun E, Benedek A, Mészner Z. Vaccine hesitancy among primary healthcare professionals in Hungary. Orv Hetil. 2019;160(48):1904–14. doi:https://doi.org/10.1556/650.2019.31538.
- Facciolà A, Visalli G, Orlando A, Bertuccio MP, Spataro P, Squeri R, Picerno I, Di Pietro A. Vaccine hesitancy: an overview on parents’ opinions about vaccination and possible reasons of vaccine refusa.l. J Public Health Res. 2019;8(1):1436. doi:https://doi.org/10.4081/jphr.2019.1436.
- Karafillakis E, Larson HJ. The paradox of vaccine hesitancy among healthcare professionals. Clin Microbiol Infect. 2018;24(8):799–800. doi:https://doi.org/10.1016/j.cmi.2018.04.001.
- Le Marechal M, Fressard L, Agrinier N, Verger P, Pulcini C. General practitioners’ perceptions of vaccination controversies: a French nationwide cross-sectional study. Clin Microbiol Infect. 2018;24(8):858–64. doi:https://doi.org/10.1016/j.cmi.2017.10.021.
- Wilson R, Zaytseva A, Bocquier A, Nokri A, Fressard L, Chamboredon P, et al. Vaccine hesitancy and self-vaccination behaviors among nurses in SouthEastern France. Vaccine 2020;38(5):1144-51.
- Kun E, Benedek A, Mészner Z.Vaccine hesitancy among primary healthcare professionals in Hungary. Orv Hetil 2019;160(48):1904–14.
- Facciolà A, Visalli G, Orlando A, Bertuccio MP, Spataro P, Squeri R, et al. Vaccine hesitancy: An overview on parents' opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res 2019;8(1):1436.
- Karafillakis E, Larson HJ. The paradox of vaccine hesitancy among healthcare professionals. Clinical Microbiology and Infection 2018;24(8):799-800. doi:https://doi.org/10.1016/j.cmi.2018.04.001
- Le Marechal M, Fressard L, Agrinier N, Verger P, Pulcini C.General practitioners' perceptions of vaccination controversies: A French nationwide cross-sectional study. Clin Microbiol Infect 2018;24(8):858-64.
- Massot E, Epaulard O. Midwives' perceptions of vaccines and their role as vaccinators: The emergence of a new immunization corps.Vaccine. 2018 16;36(34):5204–09. doi:https://doi.org/10.1016/j.vaccine.2018.06.050
- European Centre for Disease Prevention and Control. Vaccine hesitancy among healthcare workers and their patients in Europe – A qualitative study. Stockholm: ECDC; 2015.
- MacDougall DM, Halperin BA, MacKinnon-Cameron D, Li L, McNeil SA, Langley JM, Halperin SA. The challenge of vaccinating adults: attitudes and beliefs of the Canadian public and healthcare providers. BMJ Open. 2015 29;5(9):e009062
- Maltezou HC, Theodoridou K, Ledda C, Rapisarda V, Theodoridou M. Vaccination of healthcare workers: is mandatory vaccination needed? Rev Vaccines. 2019 Jan;18(1):5-13. doi:https://doi.org/10.1080/14760584.2019.1552141