ABSTRACT
Unvaccinated animal science and veterinary students are at risk of Q fever, a vaccine-preventable zoonotic disease transmitted from animals to humans. We investigated students’ perspectives on Q fever prevention using a One Health approach combining animal, human and environmental health. Animal science and veterinary students enrolled at the University of Adelaide in 2019 were invited to participate in an online survey to explore their perceptions about Q fever and prevention strategies. We undertook descriptive analysis and logistic regression. Overall, 46% of students reported little to no knowledge of Q fever. Over three-quarters of students reported transmission of Q fever via aerosol inhalation and animal culling, whilst other modes including sexual transmission between humans (7%) was poorly identified. The majority of students reported exposure to cattle, sheep and goats. Of those who reported vaccination status, 5% veterinary and 61% animal science students were unvaccinated for Q fever. Challenges concerning vaccination included cost, time and access to healthcare with strategies aimed at promoting awareness, improving healthcare access and subsidized and mass vaccination. Knowledge of Q fever among respondents, particularly about disease transmission was suboptimal. As a key principle to One Health approach, adherence to biosecurity guidelines during contact with animals could potentially reduce zoonoses including Q fever transmission. Improving access to Q fever vaccine for unvaccinated students is a priority. Findings underscore that university policy for Q fever vaccination needs to consider subsidized vaccination for both animal science and veterinary students.
Introduction
Coxiella burnetii, the causative bacterium of Q fever is present in a wide range of reservoirs including livestock, and companion and wild animals.Citation1–3 Generally, humans contract Q fever from animals via airborne routes after the organism settles in dust from birth and other body fluids and becomes aerosolized.Citation4–6 In humans, Q fever may cause asymptomatic infection and clinically compatible disease including acute influenza-like illness, chronic Q fever and post Q fever fatigue syndrome.Citation4,Citation7,Citation8 Q fever commonly affects certain occupational groups who work with animals including farmers, abattoir workers, veterinarians, veterinary nurses, veterinary students and wildlife workers.Citation3,Citation9,Citation10
Given that unimmunized people have an increased risk of contracting Q fever, vaccination plays a significant role in disease prevention.Citation11 However, vaccination may not be sufficient to control and prevent Q fever, particularly when potential community spread of Q fever ensues.Citation4 In addition, the vaccine for Q fever is costly and only registered in Australia.Citation4,Citation12 The One Health approach has been classically described as a realm of health with its focus on infectious diseases, particularly zoonoses.Citation6 One Health dismantles the complex interactions between animal, human and the environment, which are often thought to facilitate zoonoses transmission to humans with the potential to cause pandemics as seen in the COVID-19 pandemic.Citation6 One Health integration has been shown to be efficient in controlling Q fever,Citation13 both in Australia and internationally. In a farm outbreak in Victoria, Australia, human vaccination and environmental measures were indispensable, while in the Netherlands’ community outbreak, animal vaccination, biosecurity and environmental measures were applied.Citation14,Citation15 However, concomitant measures across the human, animal and environmental domains together constitute the best case scenario as shown in the Netherlands’ outbreak with human vaccination introduced sometime after the outbreak had occurred.Citation15
Animal science and veterinary students are at risk of Q fever because of their contact throughout their academic and professional careers, with a range of animals that are known to be reservoirs of Coxiella burnetii. Studies have found that veterinary students are at increased risk of being seropositive for Coxiella burnetii, and also of developing Q fever compared to other occupational groups working with animals.Citation10,Citation16 As future animal health practitioners, these students need to have sufficient knowledge of Q fever and control and prevention approaches.Citation10 This study aimed to investigate animal science and veterinary students’ knowledge, attitudes and perceptions about Q fever and its prevention, and to assess their Q fever vaccination status. The study further aimed to identify the most likely barriers to vaccination and to seek students’ suggestions about vaccination promotion strategies in order to inform Q fever vaccination policies and recommendations to support their safety while studying and in their future workplace. Because we hypothesized that protecting future animal health practitioners from Q fever is the cornerstone of a One Health approach to this zoonosis.
Methods
Study design
An online cross-sectional survey was undertaken among animal science and veterinary students enrolled at the University of Adelaide (UoA) between 14 March and 6 September 2019. The survey instrument (Supplementary File 1) consisted of 22 questions (21 closed and 1 open) across five sections; (1) demographic information, (2) knowledge and perceptions about Q fever including transmission, risks and impacts, (3) perceived exposure to animals and Q fever prevention practices including vaccination, (4) potential barriers to vaccination and (5) vaccination promotion strategies.
Study site and population
This study was conducted in the state-wide School of Animal and Veterinary Sciences (SAVS) of UoA, South Australia.Citation17 Three degree programs in ‘Animal and Veterinary Science’ study area were included: Animal Science Program ─ (1) 3 year Bachelor of Science (BSc Animal Science); Veterinary Program ─ (2) 3 year Bachelor of Science (BSc Veterinary Bioscience); and (3) 3 year Doctor of Veterinary Medicine (DVM) with students completing the DVM after successful completion of Veterinary Bioscience. All students enrolled in the three degree programs in 2019 across all years were invited to participate in the survey.
Data collection
External groups with knowledge of Q fever pilot tested the questionnaire readability and content, and suggested changes were incorporated. An e-mail invitation was sent to students enrolled in SAVS by course coordinators and lecturers of each respective year across degree programs. A reminder e-mail was sent two weeks following the initial invitation. Participation in the survey was voluntary.
Statistical analysis
Students’ demographic characteristics were descriptively analyzed. Relationship between students’ self-reported Q fever knowledge and Q fever prevention practices, perceptions about transmission and recommended vaccination strategies were assessed using Fisher’s exact test if cell counts were less than or equal to five. Responses to questions concerning knowledge of Q fever were assessed against a four-level Likert scale i.e., nil, little, some and a great deal. Former two scales were collapsed into “little or nil knowledge” variable, and the latter two scales into “a great deal or some knowledge” variable. Responses to exposure to specific animals were collapsed and recoded as always/often = high exposure, sometimes = moderate exposure, rarely = low exposure and never = nil exposure.
Binary logistic regression was undertaken to assess whether Q fever prevention practices varied significantly among students by their level of reported knowledge and vaccination status. Although responses to Q fever prevention practices were collected on a five-level Likert scale (always, often, sometimes, rarely and never), many of the response categories had very small numbers. Therefore, outcomes were collapsed into a binary variable and recoded as yes = always/often/sometimes and no = rarely/never. After recoding, some outcomes were still not sufficiently large to produce an effect estimate and hence excluded from logistic regression.
Perceptions about Q fever vaccine efficacy, safety and costs, barriers for vaccination, and the impact of Q fever on health and business were compared between vaccinated and unvaccinated students using logistic regression analysis. Responses to these predictors of vaccination were assessed against a five-level Likert scale (strongly agree, agree, neither agree nor disagree, disagree and strongly disagree). Responses were collapsed into three strata: (1) strongly agree/agree, (2) neither agree nor disagree and (3) disagree/strongly disagree. Having considered that a predictor had more than two levels of agreement, the algorithm of statistical significance for its association with students’ vaccination status was set to an overall significance rather than stratum specific significance. The positive level of agreement “strongly agree/agree” was considered as the reference category. All models were adjusted for age, sex, year of study and enrollment in a degree program. All statistical analyses were performed using Stata version 15.Citation18 Ethics approval was obtained from the UoA research ethics committee (Approval No: H-2019-040).
Results
Study population
In 2019, the total number of animal science and veterinary students enrolled across all degree programs was 826 (overall cohort), including 694 (84%) current students and 132 (16%) who had taken a leave of absence from study. Current students (study cohort, n = 694) were invited to participate, of whom 317 (46%) completed the survey. Median age of the overall cohort was 21 years (interquartile range ─ IQR, 20–24) while 75% of students in the study cohort were aged ≤24 years (). In the overall cohort, 675 (82%) students were female whilst 253 (80%) students in the study cohort were female (). Of 317 respondents, 46% were studying a DVM, 29% BSc Animal Science and 25% BSc Veterinary Bioscience ().
Table 1. Student characteristics by degree program, 2019
Q fever knowledge and exposure to animals
Of 313 students reporting on Q fever knowledge, 156 (50%) had some, 128 (41%) little, 17 (5%) nil and 12 (4%) a great deal of knowledge about Q fever (). Of 145 DVM students who reported knowledge, 55 (38%) reported little or no knowledge, and 90 (62%) some or a great deal of knowledge. Among 90 animal science students, 51 (57%) reported little or no knowledge, and 39 (43%) some or a great deal of knowledge. Of 78 veterinary bioscience students, 39 (50%) reported little or no knowledge, and 39 (50%) some or a great deal of knowledge. Vaccinated students generally possessed a higher level of knowledge compared to unvaccinated students ().
Table 2. Student characteristics by unvaccinated and vaccinated students, 2019
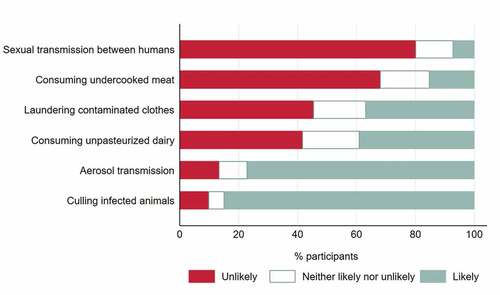
Among the respondents, 77%–85% reported that Q fever is likely to be transmitted through inhalation of contaminated aerosols and the culling of infected animals (). However, 42%–45% reported that Q fever is unlikely to be transmitted through the consumption of unpasteurized dairy products and laundering of clothes of a person who works with animals. Of the respondents, 68% thought that consuming undercooked meat is unlikely to transmit Q fever, and 80% reported sexual transmission between humans is unlikely. All listed transmission modes were associated with students’ level of Q fever knowledge; consuming undercooked meat (p < .001), consumption of unpasteurized dairy (p < .001), aerosol transmission (p = .001), laundering contaminated clothes (p = .004), sexual transmission between humans (p = .001) and culling infected animals (p = .024).
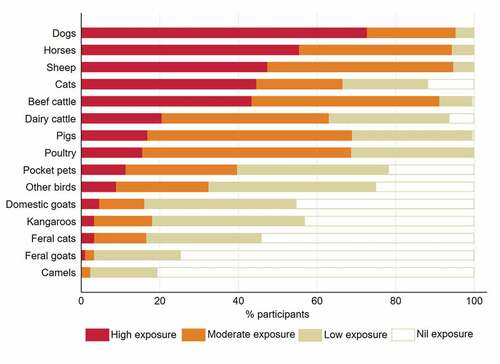
Most respondents (≥89%) across all degree programs reported moderate-high level exposure to one or more high-risk animals (). High exposure to beef cattle, cats, sheep, horses and dogs was reported by 43%–73% respectively (). Predominantly moderate exposure was reported to dairy cattle, pigs and poultry, while students had low to moderate exposure to pocket pets and other birds (). More vaccinated students were found to have high exposure to high risk animals compared to unvaccinated students ().
Q fever prevention practices
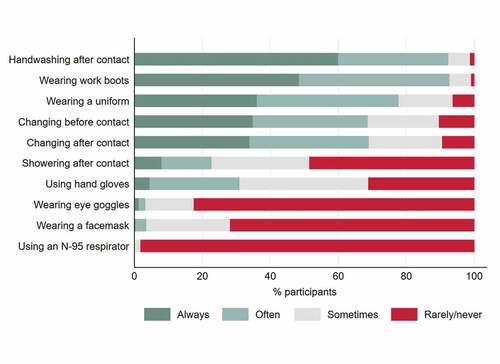
Among the listed Q fever preventive practices, 69%–93% of students always or often washed hands after animal contact, wore work boots and uniform, and changed into/out of uniform or work boots before and after animal contact (). The other preventive measures were only practiced sometimes, rarely or never by 69%–100% students for using hand gloves, showering after contact with animals, and using eye goggles, facemask or N-95 respirator. In general, preventive measures were more commonly practiced by the vaccinated students compared to unvaccinated students except handwashing after animal contact and wearing eye goggles ().
Some prevention practices were associated with students’ reported knowledge such as wearing a uniform (p = .019), using a facemask (p = .028), changing out of uniform or work boots after animal contact (p = .012), using hand gloves (p = .024) and using an N-95 respirator (p = .003) (Supplementary Table 1). Prevention practices having a marginal association with students’ Q fever knowledge included wearing work boots (p = .050) and changing into uniform or work boots before animal contact (p = .053). Other practices such as handwashing after contact (p = .817), showering after contact (p = .412) and using eye goggles (p = .123) were not associated with students’ knowledge of Q fever. However, in logistic regression models Q fever knowledge was unable to produce a significant effect estimate for any of the prevention practices after adjusting for age, sex, year of enrollment and degree program. Likewise, students’ vaccination status as a predictor of Q fever prevention practices did not produce a significant effect estimate for any of the preventive measures.
Attitudes and perceptions toward Q fever vaccine, barriers to vaccination and disease impacts
Most participants (96%) agreed that the available vaccine is effective in preventing Q fever but the cost is a barrier to vaccination (86%). The majority of respondents perceived that time-related to vaccination (73%) and access to a doctor (62%) were also important barriers. Conversely, 72% and 61% of students remained neutral or disagreed with other barriers such as “Q fever vaccine may have serious side effects” and “people’s belief that vaccine does not protect against Q fever” respectively. Most respondents agreed that Q fever has impacts on people’s health (98%), business (93%) and family (90%), despite 45% believing Q fever not to be a serious illness. More than half of participants (58%) agreed that the vaccine for Q fever is harmful to the individuals who have previously been exposed to Q fever i.e., a Coxiella burnetii positive serology.
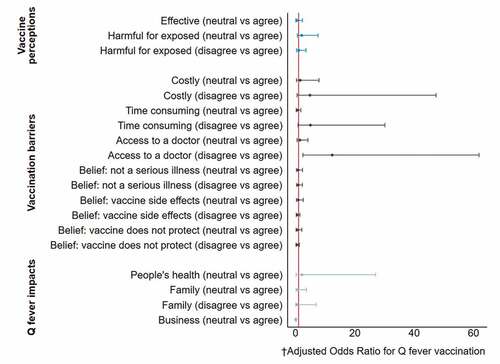
Students who disagreed “access to a doctor” is a barrier to vaccination were 12 times (OR 12.15, 95% CI 2.42–60.98) more likely to be vaccinated compared to those who agreed after adjusting for age, sex, degree program and year of study (). In contrast, the odds of getting vaccinated was 97% (OR 0.03, 95% CI 0.01–0.23) lower among respondents that were neutral to the statement “Q fever has impacts on business” compared to those who agreed.
Figure 4. Relationship between students’ belief about Q fever vaccine, perceived barriers to vaccination, and Q fever’s impact perception and their vaccination status, 2019. † Odds ratio ─ adjusted for age, sex, degree program and year of study. The vertical red line indicates odds ratio = 1 i.e., no relationship
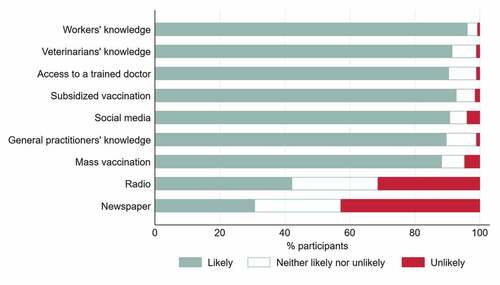
Vaccination status, recommendations and promotion strategies
Of 277 respondents who reported their vaccination status, 221 (80%) were vaccinated and 56 (20%) unvaccinated (). Higher proportion of males were vaccinated compared to females (88% vs 78%). Among those unvaccinated, 46 (82%) students were in animal science, 8 (14%) in veterinary bioscience and 2 (4%) in DVM course (). Students’ vaccination status was associated with their knowledge of Q fever (p < .001) (Supplementary Table 1). Students with some or a great deal of knowledge were more than twice (OR 2.41, 95% CI 1.05–5.52) as likely to get vaccinated compared to those with little or no knowledge after adjusting for age, sex, degree program and year of study. Most students (≥95%) recommended vaccination for at-risk groups including veterinarians, veterinary and animal science students, veterinary nurses and animal attendants, except for administrative staff working in veterinary practices (57%). Most respondents (≥88%) suggested that vaccination promotion strategies are likely to be effective except radio (42%) and newspaper (31%) (). All strategies but subsidized vaccination were associated with students’ knowledge of Q fever: radio (p = .005), newspaper (p = .001), social media (p = .003), subsidized vaccination (p = .117), mass vaccination (p = .007), access to a doctor (p = .006), general practitioners’ knowledge (p = .002), veterinary practitioners’ knowledge (p = .010) and workers’ knowledge (p = .005).
Among the vaccinated students, 17% reported that they were vaccinated >5 years ago (). When students were asked where the responsibility lies for Q fever prevention while studying animal science and veterinary degrees, of 270 students who responded, 127 (47%) suggested it is the University, 101 (37%) believed the students themselves, 28 (10%) reported a mutual responsibility of one or more of the University, students or the Health Department, and 14 (5%) indicated that the Health Department is obliged to ensure vaccination ().
Discussion
This is the first Australian study among animal science and veterinary students to investigate knowledge, attitudes and perceptions about Q fever and its prevention within a One Health framework. Although cross-sectional studies among veterinary students have been conducted in Australia, the focus was on other zoonotic diseases,Citation19 or areas covering antimicrobial stewardship and biosecurity.Citation17
Our findings are a reminder that there is a disconnect between the three domains of a One Health approach, at least regarding Q fever prevention, as has also been witnessed with containment during the COVID-19 pandemic. As evidence suggests, establishing links among the three domains and including human vaccination is integral to practicing environmental prevention measures in farms, and will likely result in better control of Q fever.Citation7,Citation20,Citation21 Our results of a higher proportion of vaccinated male students, greater Q fever knowledge among vaccinated students, and vaccinated students using preventive measures more commonly all highlight the inadequacy of the existing Q fever prevention approach among university animal science and veterinary students.
One of the dissociations was students’ suboptimal or poor knowledge about Q fever across all degree programs, except DVM students who generally possessed greater knowledge. Of particular importance was both first-year veterinary bioscience and animal science students’ concern regarding inadequate knowledge as the prime driver of low uptake of Q fever vaccine among students. Students emphasized that knowledge dissemination is required at the university and community level to prevent Q fever. This is in line with the findings from a previous Australian study where veterinarians and general practitioners affirmed that knowledge and understanding of Q fever are crucial for its prevention.Citation22 Given the students’ inherent risk of exposure, their insufficient knowledge about Q fever transmission not only makes them vulnerable to Q fever,Citation23 particularly when unvaccinated but could undermine students’ successful transition into veterinary practices. We recommend all first-year students enrolling in animal science and veterinary program receive mandatory training on zoonotic diseases, which are currently provided only in DVM (Year 4).
Conversely, students’ compliance with biosecurity guidelines as evidenced by their practices for Q fever prevention was generally good for measures such as wearing a uniform and work boots and handwashing after animal contact, despite the fact that prevention practices did not produce a significant effect estimate probably due to the modest sample size. Nevertheless, practices that are recommended by the Australian Veterinary Association (AVA) for environmental transmission prevention such as wearing a surgical mask, eye goggles and a respirator were low for the most part.Citation24 Although AVA does not routinely recommend wearing a respirator in low transmission scenarios such as visiting a farm, reinforcing respiratory protective measures would help prevent zoonoses including Q fever transmission through airborne routes.Citation25 Considering Q fever vaccination and biosecurity measures as complementary One Health principles, veterinary students should consciously consider these strategies as they are at increased risk of Coxiella burnetii exposure, particularly in their final years of study.Citation10,Citation26 Given veterinary students are prospective practitioners, their perceptions about biosecurity measures are crucial to determine their zoonoses including Q fever susceptibility and workplace behaviors.Citation27–29 Our findings could help cross-validate students’ biosecurity with animal health practitioners’ practices as the latter often attribute their poor practice to the limited availability and training on such measures.Citation29
Although animal science and veterinary students’ demographic profile was consistent with other national and state-level studies,Citation17,Citation19 inter-university and inter-state variations were not considered. Female participants outnumbered male participants, potentially limiting the generalizability of the findings to a male dominant cohort. However, given most students enrolled across the three programs are female, we may consider the findings to be generalizable to the majority of current students. Additionally, as participation in previous surveys conducted among veterinary science and veterinary medicine students across universities in Australia and New Zealand was dominated by female participants,Citation30 our findings are valid for an Australian interstate veterinary science and veterinary medicine students’ cohort. Despite this potential merit, the small sample size of our study may limit the generalizability of findings, meaning our results may not be entirely representative of Australian animal science and veterinary students. In addition, the small sample size limited our ability to calculate effect estimates with higher precision as evidenced by the wide confidence intervals for estimates that were significant.
Despite these limitations, this study is the first to address potential policy issues in the existing Q fever vaccination guidelines at an Australian tertiary education provider level using students’ perspectives. Students generally agreed that Q fever is a serious illness with individual and societal impacts and the available vaccine is effective in preventing Q fever, which is in accordance with findings from a national study among veterinarians and veterinary nurses.Citation31 Moreover, respondents who did not agree that Q fever impacts businesses had lower odds of getting vaccinated compared to those who agreed. Generally, these perceptions should motivate the students to be receptive of vaccination voluntarily, despite vaccination is mandatory for veterinary studies in Australia.Citation31 Moreover, our results of higher likelihood of getting vaccinated among students with higher levels of Q fever knowledge reinforce the necessity of providing students information and education about the disease from the start of their programs.
However, students indicated several deterrents for vaccination including cost and time associated with vaccination and access to a vaccine provider, which Australian meat processors ─ another at-risk group for Q fever also identified as barriers.Citation32 Identified barriers, particularly cost, potentially highlights that if vaccination is not funded for animal science and veterinary studies, more students will remain unvaccinated. A substantial proportion of vaccinated students had their vaccination more than five years earlier, which highlights the importance of having conclusive data on long term immunogenicity and vaccine effectiveness.Citation3,Citation33 Unfortunately, there is no definitive evidence for the exact duration of protection, as students transition into the workforce. Sero-surveillance could be an option to determine the long term effectiveness of the vaccine for Q fever. Until further evidence becomes available, revaccination is contraindicated.Citation3,Citation12 Lack of evidence for revaccination and the potential for ongoing vulnerability to Q fever affirms the importance of a One Health approach: a paradigm shift from a single preventive measure to a holistic framework.
Despite the relatively smaller quantitative estimates in our findings, a substantive number of unvaccinated students indicated exposure to high-risk animals highlighting the potential for strengthening policies to provide students ongoing protection. Except for one student indicating s/he was found seropositive, which is a contraindication for Q fever vaccination,Citation3 we could not rule out if that was the case for everyone who identified themselves as unvaccinated. The existing policy for Q fever vaccination requires all veterinary students to be vaccinated at the beginning of their study unless previously seroconverted and recommends all animal science students to seek vaccination.Citation34 Reportedly, most of the unvaccinated students were studying animal science, and students from all degree programs identified cost as the major barrier to vaccination. Nevertheless, students favored mandatory vaccination as a means to prevent Q fever, yet proposed a subsidy to be accompanied which they believed will ensure maximum uptake of vaccination. Improving Q fever knowledge at all levels including amongst healthcare providers and workers could be improved through strategies such as use of social media as an enabler of increasing uptake. We recommend revision of policies to accommodate partial or complete reimbursement of the associated cost, which could result in higher vaccination coverage.
Conclusion
Across all degree programs, students’ knowledge of Q fever, particularly related to disease transmission was suboptimal, which highlights the importance of access to information as such through incorporating knowledge into the curriculum. Since students’ exposure to high-risk animals was substantive, adherence to biosecurity guidelines during contact with animals not only reduces the chance of Q fever transmission but also protects them from other zoonoses. Given the reported exposure was not substantially different between animal science and veterinary students and a large number of students remained unvaccinated, vaccination should be instituted to confer adequate immunity. Findings underscore that improving access to vaccination through subsidized vaccination, certified immunization providers being available onsite, and designated student time for vaccination should be a priority to protect those who care for animals.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Supplemental Material
Download MS Word (27.2 KB)Acknowledgments
We acknowledge the contribution of all animal science and veterinary students who participated in this study. The authors would like to thank the course coordinators at the School of Animal and Veterinary Sciences, the University of Adelaide who helped getting this survey done. We also wish to thank Jana Maria Bednarz from Adelaide Health Technology Assessment for her statistical inputs. Md R. Rahaman is supported by the Adelaide Scholarships International (ASI) scholarship of the University of Adelaide. H Marshall acknowledges NHMRC support Practitioner Fellowship APP1155066.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
References
- Eldin C, Mélenotte C, Mediannikov O, Ghigo E, Million M, Edouard S, Mege J-L, Maurin M, Raoult D. From Q fever to Coxiella burnetii infection: a paradigm change. Clin Microbiol Rev. 2016;30(1):115–90. doi:10.1128/cmr.00045-16.
- Stevenson S, Gowardman J, Tozer S, Woods M. Life-threatening Q fever infection following exposure to kangaroos and wallabies. BMJ Case Rep. 2015:2015. doi:10.1136/bcr-2015-210808.
- Australian Government. The Australian immunisation handbook. In: Department of health. 10th ed. Canberra (Australia): Commonwealth of Australia; 2015. p. 355–62.
- Anderson A, Bijlmer H, Fournier PE, Graves S, Hartzell J, Kersh GJ, Limonard G, Marrie TJ, Massung RF, McQuiston JH, et al. Diagnosis and management of Q fever - United States, 2013: recommendations from CDC and the Q fever working group. In: CDC, editor. MMWR. Atlanta (Georgia): CDC - National Center for Emerging and Zoonotic Infectious Diseases; 2013. p. 1–28.
- Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12(4):518–53. doi:10.1128/cmr.12.4.518.
- Botelho A. Trends and challenges of Q fever control in animal and human populations. The principles and practice of Q fever: the One Health paradigm; 2017. p. 391–404.
- Porter SR, Czaplicki G, Mainil J, Guatteo R, Saegerman C, Fever: Q. current state of knowledge and perspectives of research of a neglected zoonosis. Int J Microbiol. 2011;2011:248418. doi:10.1155/2011/248418.
- Kaufman HW, Chen Z, Radcliff J, Batterman HJ, Leake J. Q fever: an under-reported reportable communicable disease. Epidemiol Infect. 2018;146(10):1240–44. doi:10.1017/s0950268818001395.
- Sloan-Gardner TS, Massey PD, Hutchinson P, Knope K, Fearnley E. Trends and risk factors for human Q fever in Australia, 1991-2014. Epidemiol Infect 2017;145(4):787–95. [published Online First: 2016/12/09]. doi:10.1017/s0950268816002843.
- de Rooij MM, Schimmer B, Versteeg B, Schneeberger P, Berends BR, Heederik D, van der Hoek W, Wouters IM. Risk factors of Coxiella burnetii (Q fever) seropositivity in veterinary medicine students. PLoS One. 2012;7(2):e32108. doi:10.1371/journal.pone.0032108.
- Chiu CK, Durrheim DN. A review of the efficacy of human Q fever vaccine registered in Australia. N S W Public Health Bull. 2007;18:133–36.
- Seqirus Pty Ltd. Q-vax Q fever vaccine and Q-vax skin test. Product information - TGA approved, Australia. 2016.
- Rahaman MR, Milazzo A, Marshall H, Bi P. Is a One Health approach utilized for Q fever control? A comprehensive literature review. Int J Environ Res Public Health. 2019;16(5). doi:10.3390/ijerph16050730. [published Online First: 2019/03/03].
- Bond KA, Vincent G, Wilks CR, Franklin L, Sutton B, Stenos J, Cowan R, Lim K, Athan E, Harris O, et al. One Health approach to controlling a Q fever outbreak on an Australian goat farm. Epidemiol Infect. 2016;144(6):1129–41. doi:10.1017/s0950268815002368.
- van der Hoek W, Morroy G, Renders NH, Wever PC, Hermans MH, Leenders ACAP, Schneeberger PM. Epidemic Q fever in humans in the Netherlands. In: Toman R, Heinzen RA, et al., editors. Coxiella burnetii: recent advances and new perspectives in research of the Q fever bacterium. Dordrecht (The Netherlands): Springer; 2012. p. 329–64.
- Rahaman MR, Milazzo A, Marshall H, Bi P. Spatial, temporal, and occupational risks of Q fever infection in South Australia, 2007-2017. J Infect Public Health. 2019. doi:10.1016/j.jiph.2019.10.002.
- Hardefeldt L, Nielsen T, Crabb H, Gilkerson J, Squires R, Heller J, Sharp C, Cobbold R, Norris J, Browning G. Veterinary students’ knowledge and perceptions about antimicrobial stewardship and biosecurity-a national survey. Antibiotics (Basel). 2018;7(2). doi:10.3390/antibiotics7020034.
- Stata statistical software: release 15 [program]. College Station (Texus): StataCorp LLC; 2017.
- Mendez D, Foyle L, Cobbold R, Speare R. Survey of rabies vaccination status of Queensland veterinarians and veterinary students. Aust Vet J. 2018;96(5):155–60. doi:10.1111/avj.12692.
- Isken LD, Kraaij-Dirkzwager M, Vermeer-de Bondt PE, Rumke HC, Wijkmans C, Opstelten W, Timen A. Implementation of a Q fever vaccination program for high-risk patients in the Netherlands. Vaccine 2013;31(23):2617–22. [published Online First: 2013/04/16]. doi:10.1016/j.vaccine.2013.03.062.
- van der Hoek W, Dijkstra F, Schimmer B, PM S, Vellema P, Wijkmans C, Ter Schegget R, Hackert V, Van Duynhoven Y. Q fever in the Netherlands: an update on the epidemiology and control measures. Eurosurveillance. 2010;15(12).
- Steele SG, Booy R, Mor SM. Establishing research priorities to improve the One Health efficacy of Australian general practitioners and veterinarians with regard to zoonoses: A modified Delphi survey. One Health. 2018;6:7–15. doi:10.1016/j.onehlt.2018.08.001.
- Chang CC, Lin PS, Hou MY, Lin CC, Hung MN, Wu TM, Shu PY, Shih WY, Lin JH, Chen WC, et al. Identification of risk factors of Coxiella burnetii (Q fever) infection in veterinary-associated populations in southern Taiwan. Zoonoses Public Health. 2010;57(7–8):e95–101. doi:10.1111/j.1863-2378.2009.01290.x.
- Australian Veterinary Association. Guidelines for veterinary personal biosecurity. St Leonards NSW; 2017.
- NASPHV. Compendium of measures to prevent disease associated with animals in public settings, 2009: national association of state public health veterinarians, Inc. (NASPHV). In: CDC, editor. MMWR. Atlanta (Georgia): Centers for Disease Control and Prevention; 2009. p. 1–21.
- Valencia M, Rodriguez CO, Punet OG, Giral I. Q fever seroprevalence and associated risk factors among students from the Veterinary School of Zaragoza, Spain. Eur J Epidemiol. 2000;16:469–76.
- Shirangi A, Fritschi L, Holman CD. Prevalence of occupational exposures and protective practices in Australian female veterinarians. Aust Vet J. 2007;85(1–2):32–38. doi:10.1111/j.1751-0813.2006.00077.x.
- Meadows SL, Jones-Bitton A, McEwen SA, Jansen J, Patel SN, Filejski C, Menzies P. Prevalence and risk factors for Coxiella burnetii seropositivity in small ruminant veterinarians and veterinary students in Ontario, Canada. Can Vet J. 2017;58:397–99.
- Dowd K, Taylor M, Toribio JA, Hooker C, Dhand NK. Zoonotic disease risk perceptions and infection control practices of Australian veterinarians: call for change in work culture. Prev Vet Med. 2013;111(1–2):17–24. doi:10.1016/j.prevetmed.2013.04.002.
- Collins T, Cornish A, Hood J, Degeling C, Fisher AD, Freire R, Hazel SJ, Johnson J, Lloyd JKF, Phillips CJ, et al. Importance of welfare and ethics competence regarding animals kept for scientific purposes to veterinary students in Australia and New Zealand. Vet Sci. 2018;5(3):66. doi:10.3390/vetsci5030066.
- Sellens E, Norris JM, Dhand NK, Heller J, Hayes L, Gidding HF, Willaby H, Wood N, Bosward KL. Q fever knowledge, attitudes and vaccination status of Australia’s veterinary workforce in 2014. PLoS One 2016;11(1):e0146819. [published Online First: 2016/01/13]. doi:10.1371/journal.pone.0146819.
- Milazzo A, Featherstone KB, Hall RG. Q fever vaccine uptake in South Australian meat processors prior to the introduction of the national Q fever management program. Commun Dis Intell. 2005;29(4):400–06. [published Online First: 2006/02/10].
- Marmion BP, Ormsbee RA, Kyrkou M, Wright J, Worswick DA, Izzo AA, Esterman A, Feery B, Shapiro RA. Vaccine prophylaxis of abattoir-associated Q fever: eight years’ experience in Australian abattoirs. Epidemiol Infect. 1990;104(2):275–87. doi:10.1017/S0950268800059458.
- The University of Adelaide. How to apply - veterinary program 2019. [accessed 10 Dec 2019]. https://sciences.adelaide.edu.au/study/animal-veterinary-science/how-to-apply-veterinary-program.