ABSTRACT
Human papillomavirus (HPV), the most common sexually transmitted infection worldwide, is responsible for a variety of cancers. HPV vaccines can help prevent this infection and its potentially devastating carcinogenic outcomes. Although the incidence of HPV-related oropharyngeal cancers among males is increasing, few studies have been published on HPV knowledge and vaccine acceptability among males. In this cross-sectional study, we assessed knowledge about HPV and the vaccine, as well as its acceptability, among third- and fourth-year male medical students in Jeddah, Saudi Arabia. Respondents were enrolled in any of the medical colleges in Jeddah from February to December 2018. A validated survey was used to collect information on HPV infection and vaccine knowledge and to ask questions assessing vaccine acceptability. HPV knowledge scores were created, and vaccine acceptability predictors were assessed with logistic regression. We collected data from 517 participants. Approximately 74% of the students had heard of HPV, with a mean knowledge score of 5.9 ± 4.6 out of 16; only 42% had heard of the HPV vaccine, with a mean knowledge score of 0.9 ± 1.6 out of 7. Among the respondents, 48.9% were interested in receiving the HPV vaccine. Although HPV infection and vaccine knowledge did not correlate with vaccine acceptability, those who had previously received the hepatitis B vaccine were more interested in receiving the HPV vaccine. In conclusion, male medical students had low HPV knowledge. Improving their HPV knowledge is important, as they are future health-care providers. The promotion of HPV vaccines in this potentially influential group is crucial for achieving effective disease prevention.
Introduction
Human papillomavirus (HPV) is a group of viruses that consists of at least 100 subtypes.Citation1 It is the most common sexually transmitted infection worldwide and has a global prevalence of 11.7%.Citation2 In most individuals, the infection resolves asymptomatically. However, in about 10% of cases, the infection persists and eventually causes cutaneous and mucocutaneous lesions such as warts, or in some cases, cancer.Citation3 Of the 14 million new cancer cases reported in 2012, 15.4% were caused by infectious agents, and 29.5% of those were attributed to HPV.Citation4
All HPV vaccines, whether bivalent, quadrivalent, or nine-valent, aim to prevent infection by the two most common carcinogenic viral subtypes: HPV 16 and HPV 18. They are reported to be up to 100% effective in preventing cervical cancers in women and anogenital cancers in both genders;Citation5 the vaccines have also decreased the prevalence of oral HPV infection by 17% in the United States.Citation6
Since the introduction of HPV vaccines, many studies have been conducted to evaluate the level of knowledge about HPV infection and vaccination in various populations. In both developed and developing countries, knowledge and awareness of HPV and its vaccine were generally low to moderateCitation7–9 but were relatively better in populations with a medical education background or higher.Citation10,Citation11 Studies suggest that factors such as age, sex, race, education level, marital status, gravidity, annual household income, and familiarity with HPV are directly related to awareness of HPV infection and its vaccine.Citation12,Citation13
As various countries began to implement national HPV vaccination programs, vaccine acceptability became a growing area of study. Among many studied factors, knowledge of HPV and the HPV vaccine are some of the well-reported predictors of HPV vaccine acceptability.Citation8 Moreover, a major facilitator of HPV vaccine uptake is physician recommendation, which is reported to increase uptake by as much as 80%.Citation7,Citation14
Local studies have focused primarily on women and have addressed HPV minimally and within the context of cervical cancer,Citation15,Citation16 oral cancer,Citation17 or sexually transmitted infections.Citation18 Furthermore, given the proven efficacy of the vaccines in preventing anogenital and oral HPV infection, as well as their provision of herd immunity,Citation19 many countries have started including them in their vaccination programs among males.Citation20
In Saudi Arabia, the Expanded Program on Immunization (EPI) was launched in 1974, which is implemented as an essential and integral element of primary health care.Citation21 Moreover, a compulsory immunization schedule was established as a vaccination certificate, from birth until the first grade of school, which is administered through the Ministry of Health’s primary health-care centers by primary health-care providers.Citation22 The Saudi Food and Drug Administration approved prophylactic HPV vaccines – Bivalent vaccine (Cervarix), and Quadrivalent vaccine (Gardasil) – in 2010 for females aged 11 to 26 years.Citation21 In the updated Saudi National Immunization Schedule published in 2019, HPV vaccines were incorporated into females’ routine vaccine schedules.Citation23 But they remain optional for males in Saudi Arabia. HPV vaccines are available in some private hospitals and clinics, along with a few major hospitals in Saudi Arabia. They are also offered at routine office visits in family medicine and pediatric clinics.Citation24 HPV vaccines are provided and given to patients – whether males or females – upon their request.
Because of the steady increase in HPV-related malignancies – especially among men – it is crucial to determine this population’s knowledge of HPV infection and their views on available vaccines.Citation25 Most studies published on HPV or the HPV vaccine focused on women as the targeted population of study, or on cervical cancer and its risk factors. However, HPV has rarely been addressed as a separate entity. As such, it was important for us to investigate the male population, and to assess their HPV knowledge and acceptability of the vaccines. Furthermore, HPV vaccines for males have yet to be included in the national vaccination program in many parts of the world including Saudi Arabia. Therefore, more effort is needed to educate future health-care providers about its importance.
Therefore, we aimed to assess the levels of HPV knowledge and vaccine acceptability among a sample of male medical students. Knowledge assessment among this population could enable the development of health education programs, which are of utmost importance, given that these students are future health-care providers and, as such, will have a significant influence on the choices made by their future patients.
Materials and methods
Study design
In this cross-sectional study, all male students who were enrolled in the third or fourth year of any medical school in Jeddah, Saudi Arabia, during the 2017–2018 academic year were invited to participate. Third-year (preclinical) and fourth-year (clinical) medical students were chosen because they fall within the age group targeted by the HPV vaccine.
Data sources and items measured
Data were collected by using a self-administered 40-item questionnaire. The first section included questions on sociodemographic characteristics: age, nationality, marital status, having children, academic year, cumulative grade point average (GPA), smoking status, hepatitis B vaccination, and sexually transmitted disease history. Questions regarding knowledge of HPV infection and vaccination were formulated and validated by Waller et al.Citation26 Questions concerning vaccine acceptability were obtained from the National Health and Nutrition Examination Survey Questionnaire of the Centers for Disease Control and Prevention.Citation27 Participants’ general HPV knowledge was assessed in the second section with 18 items. First, participants were asked whether or not they had heard of HPV. The next 16 items were “True/False/I Don’t Know” questions. In this section, participants were asked about the prevalence of HPV, types, modes of transmission, risk factors and preventive measures, signs and symptoms, treatment, and HPV relationship to warts, cervical cancer, and HIV. The last item in this section was intended to determine the students’ sources of HPV infection knowledge.
The third section consisted of eight items that aimed to assess how much the participants knew about the HPV vaccine. The first question asked whether they had heard of the vaccine. The next seven items were “True/False/I Don’t Know” questions, which assessed their knowledge of the dose, target population for administration, the need for Pap smear testing among HPV vaccinated individuals, and the protective role of the vaccine against sexually transmitted diseases, genital warts, and cervical cancer.
The fourth and final section addressed participants’ vaccine acceptability. The first three items asked whether the student had received the vaccine, whether they would be interested in receiving it, and, if they were not interested in getting vaccinated, their reasons for choosing not to do so. The next three questions asked about whether they thought that education programs would help them make the decision to be vaccinated, and whether they would discuss the HPV vaccine with their male and female patients.
Data collection
Participants were recruited from all medical schools in Jeddah: King Abdulaziz University, King Saud bin Abdulaziz University for Health Sciences, Ibn Sina National College for Medical Studies, and Batterjee Medical College. A list of male medical students enrolled in their third and fourth years of medical school during the 2017–2018 academic year was obtained. To help establish a good response rate, each of the data collectors was given a list of medical students to invite to participate. Hard copies of the surveys were distributed to students between classes and during their break time. Unfortunately, the response rate from Batterjee Medical College students was very low despite many attempts to increase it, and thus they were excluded from our analysis.
Ethical considerations
This study was approved by the Biomedical Research Ethics Unit at King Abdulaziz University, Jeddah, Saudi Arabia (No. 043–03-18). Participants were informed that participation was voluntary and that filling in the questionnaire indicated their consent to participate in the study.
Data analysis
Categorical variables are displayed as frequencies and percentages, while continuous variables are presented as means and standard deviations. The GPA of each participant was categorized as high (those with a GPA of at least 3.75 out of 5.0) or low (those with a GPA of less than 3.75). Students were also categorized as ever smokers (current and former) and never smokers.
Total knowledge scores for HPV knowledge and for HPV vaccination knowledge were calculated, by summing the responses of the corresponding section questions. The response of each knowledge question was given a score of 1 for correct answers, and a score of 0 for incorrect and “I Don’t Know” answers. The HPV knowledge scores ranged from 0 to 16, and the HPV vaccination knowledge scores ranged from 0 to 7. Lower scores indicated lower knowledge. The score variable was then categorized; a score of at least 12 out of 16 (75% correct answers) indicated good HPV infection knowledge, whereas a score of 5 (or higher) out of 7 (75% correct answers) indicated good HPV vaccine knowledge.
Predictors of HPV infection knowledge and vaccine acceptability were assessed by using logistic regression. A p-value of <0.05 indicated statistical significance. All data were analyzed with SPSS (Statistical Package for Social Sciences), Version 21.0 (Armonk, NY: IBM Corp).
Results
Sociodemographic characteristics
A total of 517 male medical students with mean age: 21 ± 1.4 years responded to the survey, yielding an overall response rate of 68%. Four hundred ninety-three questionnaires were distributed at King Abdulaziz University, 201 questionnaires at King Saud Bin Abdulaziz University, and 62 questionnaires at Ibn Sina National College. The response rates were 61%, 93%, and 52%, respectively.
As illustrated in , 99.6% of the respondents were single, and only 0.4% had children. The vast majority of students had a high GPA (93.5%). Of the participants, 26.8% percent were ever smokers, 56.2% had received the hepatitis B vaccine, and 0.6% had a history of sexually transmitted diseases.
Table 1. Sociodemographic characteristics of the participants
General HPV knowledge
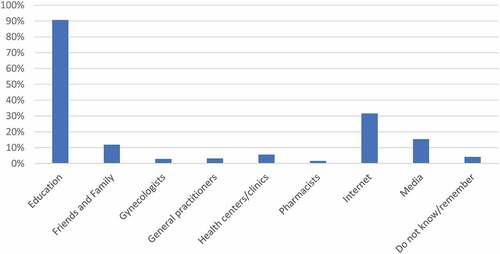
Of the participants, 73.7% had heard of HPV. The mean HPV knowledge score was 5.9 ± 4.6 out of 16. Their scores ranged from 0 (n = 143) to 15 (n = 4). The question that was most frequently answered incorrectly was “HPV usually does not need any treatment,” with 91.9% of the participants answering incorrectly. The question that was most frequently answered correctly was “Having many sexual partners increases the risk of getting HPV,” with 56.9% answering correctly (data not shown). As illustrated in , the most frequently reported source of knowledge was medical school education (90.7%), followed by the Internet (31.6%).
shows the assessment of the predictors of HPV knowledge. Students in their preclinical year were more likely to have good HPV knowledge than were those in their clinical year (odds ratio [OR]: 1.92; 95% confidence interval [CI]: 1.09–3.38). GPA, smoking status, and receiving the hepatitis B vaccine did not significantly affect HPV knowledge.
Table 2. Logistic regression analysis of the predictors of HPV knowledge
HPV vaccine knowledge
Over half of the students reported never having heard of the HPV vaccine (58.4%). The mean HPV vaccine knowledge score was 0.9 ± 1.6 out of 7. The scores ranged from 0 (n = 341) to 6 (n = 5). The question most frequently answered incorrectly was “the HPV vaccine requires three doses” (88.2% of students answered it incorrectly). The question most frequently answered correctly was “HPV vaccines offer protection from all sexually transmitted infections,” with 16.9% of students answering correctly (data not shown).
HPV vaccine acceptability
As illustrated in , 48.9% of participants were interested in receiving the HPV vaccine, and 8.7% reported that they had already received it. A majority of students (79.4%) thought that vaccine awareness programs would help them decide whether or not to receive the vaccine. Among the respondents, 55.2% indicated that they plan to discuss the HPV vaccine with their female patients and 56.9% indicated that they plan to do so with their male patients.
Table 3. Human papillomavirus (HPV) vaccine acceptability among the participants
presents the predictors of HPV vaccine acceptability. Students who did not receive the hepatitis B vaccine were less willing to be vaccinated for HPV than were hepatitis B vaccinated students (OR: 0.62; 95% CI: 0.39–1.00). Students in their preclinical year and students with a high GPA were less likely to be willing to take the HPV vaccine than were students in their clinical year and with a low GPA, respectively; however, the results did not reach statistical significance. HPV infection knowledge, vaccine knowledge, and smoking status did not affect vaccine acceptability. Saudis were more likely to be willing to take the HPV vaccine compared with non-Saudis, but the results lost statistical significance in the multivariate model.
Table 4. Predictors of willingness to receive the HPV vaccine
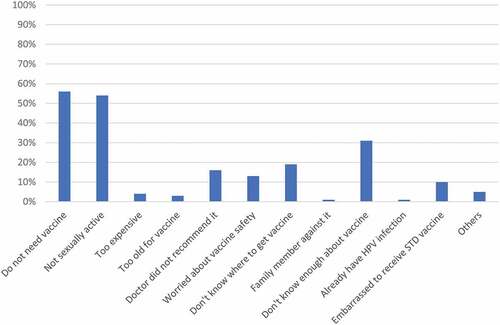
As illustrated in , the most common reason for students to refuse the HPV vaccine was because they felt they did not need it (57%) and because they were not sexually active (55%); 31% reported that they did not know enough about it.
Discussion
Our results highlight the limited knowledge among male medical students regarding HPV and HPV vaccines. The mean knowledge scores indicated that they have “poor knowledge” about these topics. Although most students had previously heard of HPV (73.7%), they incorrectly answered most of the questions regarding it.
Our participants’ mean knowledge scores were lower than those reported in similar participants in studies from other developed countries.Citation10,Citation11 A cross-sectional study of 230 health-care practitioners in New Zealand used the same knowledge assessment tool that we used in our study.Citation10 Their participants’ mean knowledge scores were higher than those of our study at 13.3 out of 16 in the general HPV knowledge section and 6.0 out of 7 in the HPV vaccine section. Predictors of HPV knowledge in that study included recent HPV training (within 1 year). No gender-based differences were mentioned.Citation10
A similar study that used the same assessment tool was conducted in the United States to assess the level of knowledge among undergraduate university students regarding HPV and its vaccine. The mean general HPV knowledge scores in that study were again higher than those in our study (11 out of 16). Their mean HPV vaccine knowledge score was also higher (5.37 out of 7) than ours.Citation11 As previously noted, “feminization” of HPV can lead to potential gender-based biases in public awareness levels;Citation28 a possible reason for our lower HPV and HPV vaccine knowledge scores may be that our study included only males.
A 2015 systematic review evaluated 22 studies for the level of knowledge among adolescent males and the results were comparable to our findings, as most of the studies reported low to moderate HPV knowledge.Citation8 Furthermore, there were discrepancies between studies for the correlation between knowledge and vaccine acceptability. A proportion of the studies, like ours, reported that there was no statistically significant correlation between HPV knowledge and vaccine acceptability.Citation8,Citation29
Rutten et al.Citation30 also published a cross-sectional study of 280 clinicians, assessing their HPV knowledge and potential barriers to HPV vaccination. They found that greater HPV knowledge was associated with a higher rate of HPV vaccine initiation among their patients, suggesting that knowledge is of paramount importance in vaccine promotion.Citation30 Similar results were found by Nickel et al.Citation31 when they surveyed the parents of girls aged 9–17 years, where the factor that was most strongly associated with HPV vaccine status was parental HPV knowledge. This study highlights the important effects of HPV knowledge on vaccination rates.Citation31
To create a better understating of HPV vaccine acceptability and influencing factors, Tatar et al.Citation32 studied 428 male college students enrolled in three Canadian universities. The goal was to identify the psychosocial correlates of HPV vaccine acceptability. Their results showed, unlike that in our study, a significant correlation between high levels of HPV knowledge and greater vaccine acceptability.Citation32 Because our study sample consisted of medical students who might have had a good understanding of vaccinations in general and of their importance in preventing disease, our students’ lack of specific HPV vaccine knowledge did not likely influence their willingness to be vaccinated. Furthermore, we had fewer participants with good HPV knowledge, which may have resulted in a lack of statistical efficiency in detecting an effect.
In our study, we found that prior vaccination with hepatitis B was a significant predictor of willingness to receive the HPV vaccine. Similarly, in their meta-analysis, Newman et al.Citation33 found that not receiving the hepatitis B vaccine correlated negatively with willingness to receive the HPV vaccine. However, smoking cigarettes had a positive correlation with vaccine acceptability.Citation33
Factors such as fear of injections, fear of vaccine side effects, lack of knowledge about the vaccine, and not being sexually active are some of the barriers to receiving the HPV vaccine that have been reported in the literature.Citation34,Citation35 The most frequently reported barriers in our study were the perception of not needing the HPV vaccine, not being sexually active, and the lack of HPV vaccine knowledge.
To the best of our knowledge, this study is one of the few to have addressed HPV knowledge and vaccine acceptability among men, and to examine HPV as a separate entity outside the context of sexually transmitted diseases, cervical or oral cancers. Our study is also one of the first to address the Saudi male’s HPV knowledge and willingness to receive the HPV vaccines. Given the sample we have opted to study, we were able to determine the HPV vaccine acceptability in an age group that is eligible to receive the vaccine, along with assessing their potential trends in promoting HPV vaccines to their future patients.
This study has a few limitations. Although our sample size was relatively large, the response rate (68.8%) was slightly lower than our initial target of at least 70%. Moreover, the effect of factors such as marital status, and history of sexually transmitted diseases on HPV knowledge could not be assessed because of the small number of participants in some of the categories. Furthermore, we were not able to compare HPV knowledge and vaccine acceptability between the colleges as we wouldn’t have had an adequate sample size if we stratified analyses by school. Despite our participants demonstrating a lack of knowledge, our studied sample is considered well educated, with knowledge in the medical field in particular. And as such, the results cannot be generalized to the general population of Saudi Arabia. However, it can be generalizable to populations with a similar medical background.
Despite these limitations, our results provide valuable information on the awareness of male medical students about HPV infection and the HPV vaccine. These data will be useful for encouraging medical schools in including more HPV-centered content in their study curriculum, along with aiding in the design and implementation of community education programs for the general population.
Conclusions and recommendations
The results of our study highlight the low level of knowledge among male medical students about HPV infection and its vaccine. Since HPV infection is a preventable disease, it is important to improve medical undergraduates’ knowledge about it and ways to prevent it, as they are future health-care providers. The promotion of HPV vaccine acceptance and use in this vaccine-appropriate age group as a potentially influential population is crucial for maximizing disease prevention in our community. Formulating a universally recognized and accepted tool for assessing the willingness to receive vaccines is also important. Further studies should be conducted on the general population as well in order to report the need for, and the direction of, public health initiatives.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Supplemental Material
Download MS Word (40.8 KB)Acknowledgments
We acknowledge, with thanks, Deanship of Scientific Research for technical and financial support. We also thank Sarah Makhdum for participating in proposal writing, data collection, and initial stages of manuscript writing; Rawan Arif for her guidance in proposal writing; and Yasser Merdad for technical assistance in data analysis. We also acknowledge Shahad Bakhashwain, Dania Kouther, Majid Hejazi, and Hosam Bin Seddeq for their efforts in data collection.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- World Health Organization. Human papillomavirus (HPV) and cervical cancer; 2019 Jan 24 [accessed 2019 Jan 30]. https://www.who.int/en/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer.
- Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30:F12–F23. doi:10.1016/j.vaccine.2012.07.055.
- Centers for Disease Control and Prevention. Cancers associated with human papillomavirus, United States—2011–2015. Report No. 4. Atlanta (GA): Centers for Disease Control and Prevention, USCS Data Brief; 2018 Oct 31. [accessed 2019 Dec 12]. https://www.cdc.gov/cancer/uscs/about/data-briefs/no4-hpv-assoc-cancers-UnitedStates-2011-2015.htm.
- Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S ICO/IARC information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in the world. Summary Report; 17 June 2019. [accessed 2019 Aug 28]. https://www.hpvcentre.net/statistics/reports/XWX.pdf.
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019 [accessed 2020 Oct 30;68:698–702. doi:10.15585/mmwr.mm6832a3externalicon.
- Chaturvedi AK, Graubard BI, Broutian T, Pickard RKL, Tong Z-Y, Xiao W, Kahle L, Gillison ML. Effect of prophylactic human papillomavirus (HPV) vaccination on oral HPV infections among young adults in the United States. J Clin Oncol. 2018;36:262–67. doi:10.1200/JCO.2017.75.0141.
- Loke AY, Kwan ML, Wong Y-T, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Commun Health. 2017;8:349–62. doi:10.1177/2150131917742299.
- Prue G, Shapiro G, Maybin R, Santin O, Lawler M. Knowledge and acceptance of human papillomavirus (HPV) and HPV vaccination in adolescent boys worldwide: a systematic review. J Cancer Policy. 2016;10:1–15. doi:10.1016/j.jcpo.2016.09.009.
- Zhang Y, Wang Y, Liu L, Fan Y, Liu Z, Wang Y, Nie S. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16:216. doi:10.1186/s12889-016-2873-8.
- Sherman SM, Bartholomew K, Denison HJ, Patel H, Moss EL, Douwes J, Bromhead C. Knowledge, attitudes and awareness of the human papillomavirus among health professionals in New Zealand. PLoS One. 2018;13:e0197648. doi:10.1371/journal.pone.0197648.
- Albright AE, Allen RS. HPV misconceptions among college students: the role of health literacy. J Community Health. 2018;43:1192–200. doi:10.1007/s10900-018-0539-4.
- Turhan E, Cetin S, Cetin M, Abacigil F. Awareness and knowledge levels of 18-year-old and older individuals regarding human papillomavirus (HPV) and HPV vaccine in Hatay, Turkey. J Cancer Educ. 2019;34:234–41. doi:10.1007/s13187-017-1292-6.
- McBride KR, Singh S. Predictors of adults’ knowledge and awareness of HPV, HPV-associated cancers, and the HPV vaccine: implications for health. Health Educ Behav. 2018;45:68–76. doi:10.1177/1090198117709318.
- Massey PM, Boansi RK, Gipson JD, Adams RM, Riess H, Dieng T, Prelip ML, Glik DC. Human papillomavirus (HPV) awareness and vaccine receptivity among Senegalese adolescents. Trop Med Int Health. 2017;22:113–21. doi:10.1111/tmi.12798.
- Sait KH. Attitudes, knowledge, and practices in relation to cervical cancer and its screening among women in Saudi Arabia. Saudi Med J. 2009;30:1208–12.
- Almajnuni AS, Balubaid AS, Alzhrani AS, Alkayyal MS, Alghamdi AS, Allam HS, Abdou AMA, Sheba MAF. Assessment of the awareness toward cancer cervix, early detection and prevention of risk factors among Saudi males and females. Egypt J Hosp Med. 2018;70:699–702. doi:10.12816/0043827.
- Alhazzazi TY. Evaluation of head and neck cancer awareness and screening status in Jeddah, Saudi Arabia. Asian Pac J Cancer Prev. 2016;17:1135–39. doi:10.7314/apjcp.2016.17.3.1135.
- Fageeh WM. Sexual behavior and knowledge of human immunodeficiency virus/aids and sexually transmitted infections among women inmates of Briman Prison, Jeddah, Saudi Arabia. BMC Infect Dis. 2014;14:290. doi:10.1186/1471-2334-14-290.
- Drolet M, É B, Pérez N, Brisson M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019;394:497–509. doi:10.1016/S0140-6736(19)30298-3.
- European Centre for Disease Prevention and Control (ECDC). Human papillomavirus infection: recommended vaccinations. Vaccine Scheduler; [accessed 2020 March 13]. https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=38&SelectedCountryIdByDisease=−1.
- Saudi Food & Drug Authority. National manual for surveillance of adverse events following immunization in Saudi Arabia. 2016 [accessed 2020 Sep 02]. https://old.sfda.gov.sa/ar/drug/resources/DocLib2/Drug-resoyrce-2143.pdf
- Immunization Schedule: Ministry of Health. 2018 [accessed 2020 Sep 01]. https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/vaccination/Pages/vaccination1.aspx.
- National Immunization Schedule: Ministry of Health. 2019 [accessed 2020 Oct 29]. https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/HealthTips/Documents/Immunization-Schedule.pdf
- Hussain AN, Alkhenizan A, McWalter P, Qazi N, Alshmassi A, Farooqi S, Abdulkarim A. Attitudes and perceptions towards HPV vaccination among young women in Saudi Arabia. J Family Community Med. 2016;23(3):145–50. doi:10.4103/2230-8229.189107.
- American Cancer Society. Key statistics for oral cavity and oropharyngeal cancers; 2019 Jan 9 [accessed 2019 March 25]. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html.
- Waller J, Ostini R, Marlow LAV, McCaffery ZG. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev Med. 2013;56:35–40. doi:10.1016/j.ypmed.2012.10.028.
- Centers for Disease Control and Prevention, National Center for Health Statistics. National health and nutrition examination survey: questionnaires, datasets, and related documentation 2015/2016. [accessed 2017 Nov 30]. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
- Daley EM, Vamos CA, Thompson EL, Zimet GD, Rosbergger Z, Merrell L, Kline NS. The feminization of HPV: how science, politics, economics and gender norms shaped US HPV vaccine implementation. Papillomavirus Res. 2017;3:142–48. doi:10.1016/j.pvr.2017.04.004.
- Shetty S, Prabhu S, Shetty V, Shetty AK. Knowledge, attitudes and factors associated with acceptability of human papillomavirus vaccination among undergraduate medical, dental and nursing students in South India. Hum Vaccin Immunother. 2019;15:1656–65. doi:10.1080/21645515.2019.1565260.
- Rutten LJF, St. Sauver JL, Beebe TJ, Wilson PM, Jacobson DJ, Fan C, Breitkopf CR, Vadaparampil ST, Jacobson RM. Clinician knowledge, clinician barriers, and perceived parental barriers regarding human papillomavirus vaccination: association with initiation and completion rates. Vaccine. 2017;35:164–69. doi:10.1016/j.vaccine.2016.11.012.
- Nickel B, Dodd RH, Turner RM, Waller J, Marlow L, Zimet G, Ostini R, McCaffery K. Factors associated with the human papillomavirus (HPV) vaccination across three countries following vaccination introduction. Prev Med Rep. 2017;8:169–76. doi:10.1016/j.pmedr.2017.10.005.
- Tatar O, Pereza S, Naz A, Shapiroa GK, Rosbergerab Z. Psychosocial correlates of HPV vaccine acceptability in college males: a cross-sectional exploratory study. Papillomavirus Res. 2017;4:99–107. doi:10.1016/j.pvr.2017.11.001.
- Newman PA, Logie CH, Doukas N, Asakura K. HPV vaccine acceptability among men: a systematic review and meta-analysis. Sex Transm Infect. 2013;89:568–74. doi:10.1136/sextrans-2012-050980.
- Maier C, Maier T, Neagu CE, Vlădăreanu R. Romanian adolescents’ knowledge and attitudes towards human papillomavirus infection and prophylactic vaccination. Eur J Obstet Gynecol Reprod Biol. 2015;195:77–82. doi:10.1016/j.ejogrb.2015.09.029.
- Al-Shaikh GK, Almussaed EM, Fayed AA, Khan FH, Syed SB, Al-Tamimi TN, Elmorshedy HN. Knowledge of Saudi female university students regarding cervical cancer and acceptance of the human papilloma virus vaccine. Saudi Med J. 2014;35:1223–30. doi:10.15537/smj.2015.2.11250.