ABSTRACT
Objective: To evaluate the awareness of College Students (CSs) of HPV vaccine in China and provide evidence-based recommendations for HPV vaccine’s publicity and promotion.
Methods: Web of Science, PubMed, Science of Direct, EBSCO, China National Knowledge Infrastructure and Wanfang Data were searched. A random effects meta-analysis was conducted to determine pooled estimates of Awareness Rate (AR) for HPV vaccine.
Results: Of the 36 studies included, the estimated AR of HPV vaccine was 40.27% (95% CI: 30.86%, 50.06%) among Chinese CSs. The AR of HPV vaccine was stratified by factors as gender, major, area, city, survey time, and sampling method of the study. The pooled AR of HPV vaccine among CSs was as follows: 44.17% (95% CI: 31.65%, 57.09%) and 31.93% (95% CI: 13.25%, 54.30%) for females and males; 44.47% (95% CI: 29.90%, 59.55%) and 12.02% (95% CI: 7.69%, 17.15%) for medical-related and nonmedical majors; 44.47% (95% CI: 28.71–60.82%) and 41.16% (95% CI: 26.48–56.64%) for Eastern and Midwestern region; 48.86% (95% CI: 30.63–67.25%) and 33.19% (95% CI: 22.27–45.12%) for first-tier and second- and third-tier city; 29.67 (95% CI: 11.44–52.16%) and 38.81 (95% CI: 27.14–51.21%) for AR before and after HPV vaccine entered in China; 51.51% (95% CI: 32.21%, 70.53%) and 26.21% (95% CI: 17.41%, 36.10%) for nonrandom and random sampling.
Conclusion: This review indicates that awareness of HPV vaccine among CSs remains relatively low in China compared with European countries. Our findings may provide useful information to better understand the HPV vaccine awareness status among Chinese CSs.
Introduction
Cervical cancer is one of the most common malignant tumors for women worldwide. The incidence and mortality rate of this cancer in China is the first place in female reproductive system malignant tumors, and ranks second in women aged 15–44 years old.Citation1 In 2018, China was the country with the highest estimated number of 106,000 incident cases of cervical cancer and the number of 48,000 deaths.Citation2 The continuous infection of High-Risk Human Papillomavirus (HR-HPV) was considered to have played an important role in the occurrence and development of cervical cancer. The World Health Organization (WHO) has recognized the importance of cervical cancer and other Human Papillomavirus (HPV) related diseases as global public health problems, and reiterated the recommendation that HPV vaccine should be included in the National Immunization Program (NIP).Citation3
Since 2006, three types of HPV vaccines have been approved worldwide to effectively prevent abnormality caused by persistent HR-HPV infection, namely Cervarix® 4, Gardasil® 4 and Gardasil® 9. Therefore, WHO’s position paper on HPV vaccines suggested that the introduction of HPV vaccine should be part of the strategy to prevent cervical cancer and other HPV-related diseases, and HPV vaccination should be carried out in primary target population (women aged 9–14 years) and secondary target population (women aged 15 years and above).Citation3 At present, HPV vaccine remains a non-immunization program vaccine in China, which follows the principle of informed, voluntary and self-funded vaccination. It is officially defined as the supplement to the NIP vaccine. In response to WHO’s global goal of eliminating cervical cancer, it is urgent to enhance people’s knowledge and awareness of HPV vaccine to improve its public coverage. The successful control and prevention of cervical cancer largely depend on the public’s basic cognition of vaccination.
College Students (CSs), generally between 18 and 25 years old, live a more independent and freer lifestyle and are highly susceptible to HPV infection because most of the first sexual behaviors occurred during college years.Citation4 Meanwhile, this age group is highly coinciding with the recommended vaccination age of HPV vaccine in China. In addition, at the childbearing age, CSs will also affect the next generation based on their thoughts and attitudes to HPV vaccine.Citation5 Hence, assessing the awareness and understanding of HPV vaccination among CSs is worthy of attention, which is conducive to successful reduction of potential infection of HPV and control of cervical cancer.
Since the HPV vaccine came into being, numerous papers related to knowledge, attitude, and practice tendencies on HPV vaccination in Chinese CSs have been published.Citation6–11 Most of them were cross-sectional designs in one region,Citation7–11 one organization,Citation11 or among females.Citation6–9 Besides, there have been previous systematic reviews and meta-analyses evaluating HPV awareness and knowledge in China. Meta-analyses conducted by ZhangCitation12 and YuCitation13 concluded that HPV vaccine awareness among Chinese population was low between 2006 and 2015, with AR of 15.95% (95% CI: 12.87%, 19.29%) and 17.13% (95% CI: 14.04%, 20.46%) respectively. However, both studies were performed before the vaccine entered mainland China and reviews of evaluating HPV vaccine awareness among CSs population after that are insufficient. The idea of this study aims to delve into the level of awareness toward HPV vaccine among CSs across the nation.
Materials and methods
Search strategy
A systematic literature search was conducted in the Web of Science, PubMed®, Science of Direct, EBSCO®, China National Knowledge Infrastructure (CNKI®) and Wanfang Data. The search was limited to original articles in English and Chinese, without limitations regarding the year of publication. The last search date was October 8, 2020. The research protocol was registered in the PROSPERO international prospective register of systematic reviews (CRD42020213364).
The search strategy (see Appendix A) consists of combined terms of HPV, human papillomavirus, vaccine, and vaccination. One author (G.Y.) screened all titles and abstracts. Full-text articles were obtained if the abstract fulfills the inclusion and exclusion criteria. Consequently, all full-text articles were reviewed by two researchers independently (G.Y. and Y.Z., or G.Y. and C.C.). Any disagreements between the researchers were resolved by discussion. In case of multiple articles published on the same study population, only the publication with the most relevant results was further evaluated. Additional studies including gray literature were identified by checking reference lists and by Google Scholar retrieval. Also, the reference lists of all the included studies were checked.
Selection criteria
For this review, studies reporting sample size and Awareness Rate (AR), or providing the data that could calculate the AR indirectly among CSs were eligible for inclusion in the meta-analysis. The selection criteria are shown in .
Table 1. Selection criteria
After strict screening, 36 articles were selected ultimately, including 26 in Chinese and 10 in English. Although most of the included studies were published in China, the quality of all the chosen literature could be considered as adequate to considerable quality, because academic articles published in China are still subject to peer-review and academic publication process. The Meta-analysis of Observational Studies in Epidemiology (MOOSE) flow chart of literature retrieval could be illustrated in .
Data extraction
The following general information was extracted from the included articles by one author (G.Y.): first author, collection period, area, region, study participants and setting (i.e., source of participants), sample size, sampling method, and quality level. For the literature that the AR was not directly given, two researchers (C.C. and H.R.) independently calculated it, and those with consistent results were applied. If the results were inconsistent, the third evaluator (B.G.) will intervene, and the final result will be available after discussion depending on consensus. If necessary, we also contacted corresponding authors for additional information to ensure accuracy in the calculation.
We found that there were mainly two ways to ask questions about awareness of HPV vaccine in the included studies: (1) Do you know the HPV vaccine? (2) Have you ever heard of HPV vaccine? Accordingly, the answers to the above questions were YES, NO, and UNCLEAR respectively. If the respondent in the study answered YES, we considered he or she knew about HPV vaccine. If the respondent answered NO or UNCLEAR, we did not consider he or she knew about the HPV vaccine. The AR of HPV vaccine was extracted directly from the literature if it is reported in the study. Otherwise, the AR of HPV vaccine was calculated by dividing the number of people who were aware of the HPV vaccine with the overall sample size.
Statistical analysis
Data were analyzed from October to November 2020 by four reviewers (G.Y., C.C., H.R., and B.G.) in accordance with MOOSE and A MeaSurement Tool to Assess systematic Reviews (AMSTAR) reporting guidelines.Citation14 STATA (Version 15.1, Stata Corp, Texas, USA) software was used for meta-analysis. The score method was used for the Freeman-Tukey double arcsine transformation of the 95% confidence interval on the pooled estimates.Citation15 Meanwhile, sources of heterogeneity (i.e., variation in the research results) were explored using subgroup analyses. I2 statistic was used to describe the heterogeneity across the studies. Conventionally, when I2 ≤ 50%, a fixed effects model was employed; when I2 > 50%, a random effects model was used. Besides, potential publication bias was explored using funnel plots and Egger’s test.Citation16 Sensitivity analysis was performed to evaluate the robustness of the findings. Two-sided p< .05 indicated statistical significance.
Methodological quality appraisal
Evaluation of the methodological quality was independently performed by two reviewers (M.Z. and C.C.), and inconsistencies were determined by the third reviewer (G.Y.) after discussion. The methodological quality of the studies included in this review was assessed using an 11-item checklist which was recommended by Agency for Healthcare Research and Quality (AHRQ) for cross-sectional study.Citation17 An item would be scored 0 if it was answered NO or UNCLEAR; if it was answered YES, then the item scored 1. Article quality was assessed as follows: 0 to 3 points were defined as low quality, 4 to 7 points as moderate quality, and 8 to 11 points as high quality.
Results
Included literature feature
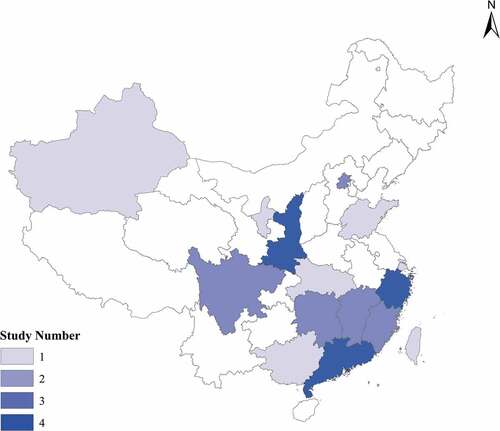
A total of 36 articles were included based on the inclusion and exclusion criteria. The total number of samples was 117,686. The sample size varied widely in different studies, ranging from 105 to 11,236. There were 12 articles on CSs, 6 on female CSs, 1 on male CSs, 2 on medical CSs, and 2 on non-medical CSs. Seventeen researches were conducted in Eastern region, five in Central region, eight in Western region, and three in whole nation. Geographic distribution feature of included studies is illustrated in .
The characteristics of included articles are provided in in detail. Most of the quality of the included articles attained medium scores, ranging from 3 to 8 points based on AHRQ scale, with an average of 6.47. The main loss items of quality evaluation are as follows: (1) Not describe any assessments undertaken for quality assurance purposes; (2) Not describe how confounding was assessed and/or controlled; (3) Not explain how missing data were handled in the analysis; (4) Not clear in the follow-up data.
Table 2. Research characteristics of included studies (n = 36)
Full combined effect value
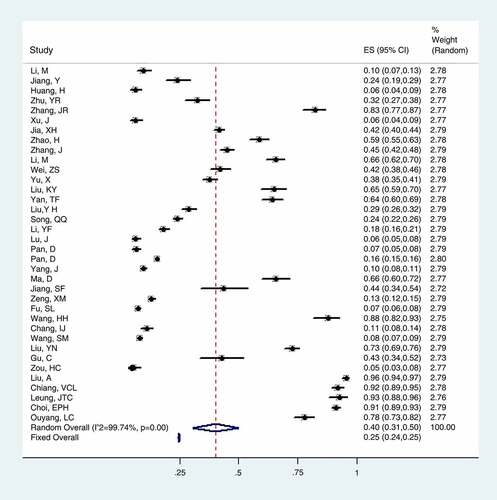
A heterogeneity test was carried out on 36 included articles, and the results reflected that there is a large heterogeneity among the researches, with I2 statistic = 99.74% and p < .001. Hence, random effects model was conducted in the meta-analysis. The pooled AR in 36 articles was 40.27% (95% CI: 30.86%, 50.06%) and forest plot of meta-analysis is shown in .
Subgroup analysis
In this review, subgroup analysis was employed to explore the heterogeneity by stratification as follows: (1) gender, (2) major, (3) area, (4) city, (5) survey time, and (6) sampling method. Subgroup analysis revealed a marked disparity in AR among CSs in China regarding gender, major, city, survey time and sampling method. The results in subgroup analysis are shown in .
Table 3. Subgroup meta-analysis of AR among CSs in China
Sensitivity analysis
According to the results of literature quality evaluation, the meta-analysis was conducted again after 4 articlesCitation11,Citation27,Citation30,Citation40 with relatively low quality were excluded. The results showed that the combined value of AR in the remaining 32 articles was 37.25% (95% CI: 27.68–47.31%), which was similar to the original result by 40.29% (95% CI: 30.86–50.06%), and the combined effect value after elimination basically showed little distinction. The results of sensitivity analysis appeared reliable and robust in this meta-analysis.
Publication bias analysis
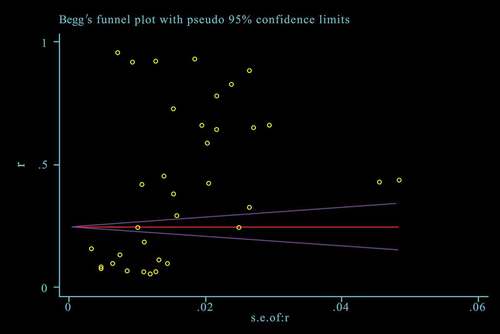
Publication bias in studies was assessed in this review. The funnel plot is shown in by Begg’s test. We can clearly see that the distribution was dispersed, with most of researches in the underside of the funnel plot. Meanwhile, the results calculated by Egger linear regression (p = .008) also indicated that there was a significant publication bias in the meta-analysis.
Discussion
What is Chinese college students’ awareness level toward HPV vaccine?
It is crucial to enhance the public’s awareness of HPV vaccine as an effort to expand the scope of immunization because awareness is an essential step in vaccination. This study demonstrated an estimated value of the AR of HPV vaccine among CSs in China. The results showed that 40.27% (95% CI: 30.86%, 50.06%) of Chinese CSs had heard of HPV vaccine, which is lower than those in Italy (69.9%),Citation48 but higher than those in India (36.8%),Citation49 Turkey (26.6%)Citation50 and Thailand (25.3%).Citation51 It is reasonable to infer that there may be a higher percentage of general population ignorant of the vaccine, given that over half of the highly educated group does not know about HPV vaccine. Apparently, if the target group is unaware of HPV vaccine’s existence, the vaccination is far from a reality. The awareness of HPV vaccine among CSs group in China, compared with other developed countries,Citation52–54 is still weak. This indicates that delivery of HPV vaccination education to CSs in China needs to be reevaluated and valued by authorities. Besides, the literature review showed that there were few studies related to male CSs and North-eastern regions on the awareness of HPV vaccine, which indicates that the aforementioned areas should be prioritized in future research.
Gender
In this review, we found that most of the studies on the knowledge, attitude, and practice of HPV vaccine were conducted among women, and few involved men. And AR of female CSs (44.17%, 95% CI: 31.65%, 57.09%) was higher than male group (31.93%, 95% CI: 13.25%, 54.30%). There is a high probability that HPV vaccine is generally regarded as cervical cancer vaccine by the public in China, which seems to have nothing to do with men. In fact, boys can play an important role in directing their partners or elders to get vaccinated, especially in the CSs group. Meanwhile, the knowledge of HPV vaccination in male group can improve personal hygiene and habits to a certain extent and indirectly reduce HPV infection rate in females, given the truth that men are the primary transmission vector of HPV to women.Citation46 Besides, HPV is responsible for malignancies in men too, including malignant tumors of the anus, penis, oral cavity, and oropharynx. What needed to be clear is that HPV vaccination is also beneficial to boys. Many countries worldwide (US, UK, Australia, etc.) have included boys in National Vaccination Programs to eliminate HPV-related diseases and save lives. Although concurrent efforts to vaccinate both males and females could provide a more effective way to reduce the prevalence of HPV infections in the population,Citation46 male groups have not yet been included in the target population for HPV vaccination in China, owing to production capacity of the vaccine and vaccination regulations. Nevertheless, it is still necessary for men to promote their awareness of this vaccine because only mutual cognition of this virus and its vaccination could lead to the decrease in the incidence of HPV-related STIs (Sexually Transmitted Infections) and cervical cancer.
Major
A total of 36 studies concerning Chinese CSs showed that there was a big gap of AR between medical-related majors (44.47%, 95% CI, 29.90%, 59.55%) and non-medical related majors (12.02%, 95% CI, 7.69%, 17.15%). This is consistent with the results of a Turkish study.Citation55 After all, medical-related majors refer to clinical medicine, nursing, medical imaging, pharmacy, and health management. Students of these majors will learn more about professional knowledge on campus, who act as primary information popularizers and play a critical role in wide spreading of awareness among citizens. Thus, it is reasonable to reckon it urgent, because more than half of the medical-related CSs do not know this kind of vaccine. The relevant knowledge and assessment of HPV could be added in the compulsory or optional courses for medical-related students to increase their cognition of HPV and vaccination. It is helpful to better convey vaccination knowledge to the general population in their future practice.
Region
Two categories, namely area and city, were used to discuss the influence of region on HPV awareness in this study. AR in Eastern region (44.47%, 95% CI: 28.71–60.82%) was slightly higher than that of Midwestern region (41.16%, 95% CI: 26.48–56.64%). At the same time, according to the sample cities included in the literature, two types of cities (first-tier and second- and third-tier cities) were categorized based on political status, economic strength, city size, and regional influence. AR in second- and third-tier cities (33.19%, 95% CI: 22.27–45.12%) was lower than that in first-tier cities (48.86%, 95% CI: 30.63–67.25%). It is obvious that the classification results from cities showed more disparities than areas. The reason for this variation is not entirely clear but it is indicative of gaps in state or municipal policies and strategies regarding publicity of HPV immunization-related knowledge, since the central administration has no compulsory regulations in terms of promotion and publicity of the non-immunization program vaccine. Compared with second-and third-tier cities, residents in first-tier cities have both a relatively higher educational and health consciousness level, and are willing to accept new things. This may account for the discrepancy in AR of HPV vaccine among different types of cities.
Time
It has been demonstrated that immunization awareness has been improved since HPV vaccine came into mainland China (Cervarix® 4 and Gardasil® 4 were approved and licensed in July 2016 and May 2017, and Gardasil® 9 in April 2018), yet CSs in China still have limited knowledge about the HPV vaccination. After all, HPV vaccine is still a new thing in China compared with developed countries. The result seems to be similar in this study. Our findings indicated that AR of CSs regarding HPV vaccine was 29.67% (95% CI: 11.44%, 52.16%) before 2016, and 38.81% (95% CI: 27.14–51.21%) after 2016. Although the awareness of HPV vaccine of CSs has increased after its access to the market, it is still far from sufficient compared with the countries that have incorporated the vaccine in NIP.Citation56–58 This may be owing to insufficient publicity and avoidance of mentioning reproductive organs in traditional Chinese culture. It should be noted that there are still nearly 60% of Chinese CSs who don’t know about HPV vaccine at all after its entry into mainland market. This may reflect the lag of policy propaganda to some extent.
Sampling method
Nonrandom sampling, such as convenience sampling, is more convenient and flexible and favored by researchers in cross-sectional study. Yet we found that there was a significant variance between random (26.21%, 95% CI: 17.41%, 36.10%) and nonrandom (51.51%, 95% CI: 32.21%, 70.53%) sampling about AR of HPV vaccine in this study. As we know, there may be some shortcomings about nonrandom sampling such as small sample size and insufficient representativeness, which may lead to greater heterogeneity in the combined results of meta-analysis even if subgroup analysis is carried out. Meanwhile, nonrandom sampling may increase the positive rate due to the subjectivity of sample selection. This enlightens us to choose random sampling method as far as possible in future observational research, so as to ensure the scientific and random selection process of research objects.
Why have so few Chinese college students heard of the HPV vaccine?
In China, inoculation is an essential part of the Basic Public Health Services (BPHS) of the country and is subject to annual evaluation by the local health administration, such as vaccination status and archives establishment. According to Vaccine Administration Act issued in 2019, vaccines are generally divided into two types, that is, the immunization program vaccine (i.e., vaccinated obligatorily by the government for free, included in NIP) and the non-immunization program vaccine (i.e., vaccinated voluntarily at one’s own expense). However, only the vaccines included in NIP were written into evaluation plan. Therefore, the coverage of non-immunization program vaccines such as HPV vaccine is not regulated and required by the official sectors. Naturally, this leads to divergent policies regarding HPV vaccination in different cities and regions in mainland China. The publicity and promotion of this kind of vaccine gradually become the independent behavior of vaccination institutions for extra service income. Also, residents can only understand the knowledge and vaccination procedures of HPV vaccine through self-cognition or limited publicity channels according to their own needs. There may be obstacles in the equalization of delivery about public vaccination knowledge without administrative intervention. This calls for stricter enforcement of legislation aimed at boosting awareness of HPV vaccination, as well as frequent evaluation of HPV immunization programs.
Besides, in terms of health education for CSs including essential infectious disease education, the central education authority has not enacted specific rules on the curriculum of training for CSs, such as inclusion of health teaching and other related lessons. This also partly explains why most CSs know HPV vaccine online and on TV, rather than in classroom.Citation45 In order to better understand the circumstance of vaccination knowledge imparted to CSs on campus, a cross-sectional survey (by G. Yin, Y. Zhang, C. Chen, M. Zhang, unpublished work) was conducted in Wuhan University and Hubei University in November 2020. The results showed that among 321 valid questionnaires (111 males and 210 females), 82.55% CSs reported that the school did not set up health education-related courses. 86.60% CSs have not taken health education-related courses and 92.83% CSs have never participated in activities relevant to HPV vaccination on campus such as lecture, exhibition and roadshow. Key items and frequencies of the questionnaire are shown in . The survey revealed that the publicity and promotion of HPV vaccination in Chinese universities were inadequate and incomplete. Chinese CSs have a significant demand for HPV-related knowledge. Deficiencies in campus education regarding the delivery of HPV vaccination knowledge for common CSs were still prominent. Therefore, it is urgent to augment public awareness of HPV vaccines to boost its coverage.
Table 4. Health education status of HPV vaccine in Chinese CSs on campus
Recommendations
In light of Knowledge-Attitude-Behavior theory, influence on individual’s health behavior is first through information reception, followed by the expectation of attitude change and subsequent desired behavior changes.Citation59 Therefore, sufficient knowledge acquisition for individuals is an essential component of the immunization process.
First, it is of great importance that the Chinese government should exert its leadership role and integrate various social resources by encouraging closer ties between key stakeholders,Citation60 including vaccine manufacturers, those in healthcare sector, and academia in order to incorporate HPV vaccine into NIP as soon as possible, or at least conduct inoculation in priority groups with the right age like CSs. This is consistent with the recommendations of The Plan for the Elimination of Cervical Cancer proposed by WHO.Citation61 Meanwhile, some effective measures such as necessary legislation should be taken by the Central Health Administration and CDC to avoid information asymmetry in promotion and delivery of HPV vaccine between cities and regions which may lead to unfairness in BPHS.
Second, as the responsible agency for vaccinationFootnote1 of residents, immunization-related health knowledge could be disseminated by CDC, community health service centers and town hospitals, which are acceptable for citizens, particularly CSs. Possible ways are WeChat subscription, official Tiktok, and other online platforms. Besides, health officials and professionals are recommended to promote information quality construction to improve the standards of HPV immunization messages online, since high quality and audience-friendly online messages are important for the cognition and acceptance of HPV vaccine among the public.Citation62
Third, it is suggested that timely, active and targeted education is crucial to improve the awareness level of HPV vaccine among CSs on campus. Related studies indicated that educational interventions to increase HPV awareness and vaccination may help to boost vaccination rate.Citation63 Chang’s study found that a short period of educational intervention can significantly improve the public awareness of HPV vaccine. After one-hour health lecture education, the acceptability of HPV vaccine among college students can be increased from 73% to 82%.Citation6 Therefore, targeted intervention measures such as health courses, lecture education, leaflets and posters could be actively taken to achieve the goal of primary prevention of cervical cancer on campus.
Conclusion
HPV vaccine was a proven method that could effectively prevent the infection of HR-HPV in humans. Cultivating knowledge and awareness among youngsters, especially CSs, may effectively enhance the uptake of HPV vaccine so as to minimize the incidence of HPV-related STIs and cervical cancer. This up-to-date meta-analysis reviews the basic awareness of CSs toward HPV vaccine, which may provide evidence-based suggestions for further promotion of the vaccination coverage. Our study reveals that Chinese CSs’ awareness of HPV vaccine remains suboptimal compared with that of European countries. In response to weak awareness, corresponding measures need to be properly proposed and implemented in a common effort by the health administration, vaccination institution and campus to increase HPV vaccination awareness in CSs.
Strengths and limitations
There have been previous systematic reviews and meta-analyses evaluating HPV awareness and knowledge in China of different population samples, but ours is the most up-to-date review that pays close attention to college students, the primary target group for HPV vaccine. However, there still are some limitations in the review. First, although strict selection and quality assessment were conducted in the included articles, heterogeneity among studies was high owing to the number of studies included and various study populations. Second, the articles included were cross-sectional studies, which inevitably have inherent shortcomings of cross-sectional design. Third, the search strategy excluded articles written in languages other than English and Chinese, whereby relevant results may have been missed. Fourth, although some of the included studies were published in Chinese peer-reviewed academic journals, this may still create some possible bias in the analysis.
Author contributions
G.Y. and M.Z. designed study. G.Y., Y.Z. and C.C. conducted the literature search and review. G.Y., C.C., H.R. and B.G. reviewed citations and extracted data. G.Y. and Y.Z. analysed the data. G.Y. and Y.Z. wrote and edited manuscript. M.Z. supervised review. All authors critically revised for important intellectual content.
Disclosure of potential conflicts of interest
The author declared no competing interests with respect to the research.
Acknowledgments
Thanks are due to Ms. Yuting Liao from Beijing Foreign Studies University for valuable discussion.
Additional information
Funding
Notes
1. According to the National Basic Public Health Services Standard in China, vaccine inoculation is a part of Basic Public Health Services (BPHS) item. Hence, vaccination institutions or vaccinations agency are generally regarded as health institutions with vaccination qualification, including local CDC, community health service centers and town hospitals. The vast majority of vaccination institutions are primary medical institutions, while large public hospitals generally do not undertake the responsibility of inoculation.
References
- Chen WQ, Zheng RS, Baade PD, Zhang SW, Zeng HM, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. doi:10.3322/caac.21338.
- Arbyn M, Weiderpass E, Bruni L, Sanjosé S, Saraiya M, Ferlay J, Bray F. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):E191–E203. doi:10.1016/S2214-109X(19)30482-6.
- World Health Organization. Human papillomavirus vaccines WHO position paper, May 2017–recommendations. Vaccine. 2017;35(43):5753–55. doi:10.1016/j.vaccine.2017.05.069.
- Family Department of National Health Commission. 中国家庭发展报告2015 [CHINA Family Development Report 2015]. Beijing, China: China Population Press; 2015.
- Deng C, Chen XL, Liu YQ. Human papillomavirus vaccination: coverage rate, knowledge, acceptance, and associated factors in college students in mainland China. Hum Vaccin Immunother. 2020;8:1–8. doi:10.1080/21645515.2020.1797368.
- Chang IJ, Huang R, He W, Zhang SK, Wang SM, Zhao FH, Smith JS, Qiao YL. Effect of an educational intervention on HPV knowledge and vaccine attitudes among urban employed women and female undergraduate students in China: a cross-sectional study. BMC Public Health. 2013;13:916. doi:10.1186/1471-2458-13-916.
- Wang HH, Wu SY. HPV vaccine knowledge and perceived risk of cervical cancer among female college students in Taiwan. Asian Pac J Cancer Prev. 2013;14(12):7371–74. doi:10.7314/APJCP.2013.14.12.7371.
- Gu C, Niccolai LM, Yang SB, Wang XH, Tao LJ. Human papillomavirus vaccine acceptability among female undergraduate students in China: the role of knowledge and psychosocial factors. J Clin Nurs. 2015;24:2765–78. doi:10.1111/jocn.12871.
- Leung JTC, Chi-kin L. Revisiting knowledge, attitudes and practice (KAP) on Human Papillomavirus (HPV) vaccination among female university students in Hong Kong. Hum Vaccin Immunother. 2018;14(4):924–30. doi:10.1080/21645515.2017.1415685.
- Zou HC, Wang W, Ma YY, Wang YJ, Zhao FH, Wang SM, Zhang SK, Ma W. How university students view Human Papillomavirus (HPV) vaccination: a cross-sectional study in Jinan, China. Hum Vaccin Immunother. 2016;12(1):39–46. doi:10.1080/21645515.2015.1072667.
- Liu YN, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccin Immunother. 2020;16:116–23. doi:10.1080/21645515.2019.1638727.
- Zhang YR, Wang Y, Liu L, Fan YZ, Liu ZH, Wang YY, Nie SF. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16:216. doi:10.1186/s12889-016-2873-8.
- Yu ZJ, Chen YC, Zhang DD, Song ZX, Pang L, Qu B. Cognition and acceptance of human papillomavirus vaccine in China: a meta-analysis. Chin J Health Stat. 2017;34:578–82.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi:10.1136/bmj.j4008.
- Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39. doi:10.1186/2049-3258-72-39.
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi:10.1136/bmj.315.7109.629.
- Zeng XT, Zhang YG, Kwong JSW, Zhang C, Li S, Sun F, Niu YM, Du L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evidence-based Med. 2015;8(1):2–10. doi:10.1111/jebm.12141.
- Li M, Ju LR, Li BL, Liu F, Zhou QY, Qi J. Survey of the cognition on human papillomavirus and it’s preventive vaccine of junior school student’s parents and university students in Beijing. Chin Journal Woman Child Health Res. 2013;24(1):14–17. doi:10.3969/j.1673-5293.2013.01.006.
- Jiang Y, Pan S, Lou LP, Li L, Liu ZH, Yang CX. Investigation about influencing factors of awareness and attitudes toward HPV vaccine among college students in Chengdu. J Prev Med Intell. 2019;35:179–83.
- Huang H, Zhao FH, Xie Y, Wang SM, Pan XF, Lan H, Chen F, Yang CX, Qiao YL. Knowledge and attitude toward HPV and prophylactic HPV vaccine among college students in Chengdu. Mod Preventive Med. 2013;40:3071–80.
- Zhu YR, Hu XL, Sheng CH. Survey of college students’ knowledge and attitudes towards HPV vaccine. Today Nurse. 2017;11:25–27.
- Zhang JR. Investigation on college students’ understanding of HPV vaccine, vaccination intention and influencing factors. Mod Bus Trade Ind. 2019;8:178–79.
- Xu J, Li YQ. Analysis of college students’ cognition and attitude towards human papillomavirus and HPV vaccine. J Youjiang Med Coll National. 2014;1:72–73. doi:10.3969/j.1001-5817.2014.01.044.
- Jia XH, Xu Q, Yang H, Luo HJ, Zhu BY, Wang Q. An investigation on HPV cognition status and vaccination intention of female college students in Ganzhou. Prac Clin Med. 2019;20(3):86–90. doi:10.13764/j.cnki.lcsy.2019.03.030.
- Zhao H, Tian SJ, Wang XH, Li Q, Xia L. Investigation and analysis on cognition and demand of HPV vaccination for female college students in vocational college. Chin J Soc Med. 2020;37(1):79–81. doi:10.3969/j.1673-5625.2020.01.022.
- Zhang J, Zhang JY, Pang HM, Yang JW, Chen XF, Dong XM. Investigation on acceptance of HPV vaccination and its determinants among college students in Guangzhou city. Chin J Dis ControlPrev. 2018;22(9):965–71. doi:10.16462/j.cnki.zhjbkz.2018.09.022.
- Li M, Dai ZJ, Zhang C, Wei DH, Li YJ, Wei Y. Investigation and analysis on cognition of HPV vaccine among college students in Liuzhou city. Med Dietotherapy Health. 2020;7:183–85.
- Wei ZS, Lv YM. Knowledge and intention of students in a university regarding human papillomavirus and its vaccine. Chin J Sch Doctor. 2018;32:890–94.
- Yu X. Analysis of factors influencing university students’ willing to inject HPV vaccine in Nanchang based on the model of TAM&TPB [dissertation]. Nanchang (China): Nanchang University; 2019.
- Liu KY, Guo WW, Liu SM. Investigation and analysis on awareness and willingness of HPV vaccine among nursing students in Ningxia. Health Vocational Educ. 2020;38:104–06.
- Yan TF, Lin X, Li R. Investigation on the awareness of cervical cancer prevention and HPV vaccine among female college students. Occup Health. 2020;36(10):1399–401. doi:10.13329/j.cnki.zyyjk.2020.0371.
- Liu YH, Rui P, Dou ZD, Zhang GJ. Investigation and analysis of the awareness, attitudes and practice on HPV vaccine among female college students. J Qiqihar Med Univ. 2019;40(23):2988–91. doi:10.3969/j.1002-1256.2019.23.035.
- Song QQ, Zhang YJ, Yang CQ, Fang JY, Chang JF, Li SP, Wei FX, Su YY, Wu T. Investigation on awareness and willingness of HPV vaccination among college students in Xiamen city. Chin J Health Educ. 2019;35(8):705–10. doi:10.16168/j.cnki.1002-9982.2019.08.007.
- Li YF, Ma HS, Li RX, Lin HZ, Xiao WW, Huang MM, Huang SJ, Wu T, Su YY. Awareness, willingness and influencing factors of HPV vaccination among male college students in Xiamen. Chin J Sch Health. 2019;40(12):1880–83. doi:10.16835/j.cnki.1000-9817.2019.12.032.
- Lu J, Mou W, Jiang MB, Zhang GH, Wang J, Yan L, He JX. Investigation on the cognition of HPV and HPV vaccine among college students in Shanghai. Shanghai J Prev Med. 2015;27:762–66.
- Pan D, Yang JJ, Yang JY, Tao GX. Investigation on the cognition and acceptance of HPV vaccine among some people in Taizhou city. Chin J Matern Child Health J. 2019;30(5):570–73. doi:10.3969/j.1673-5293.2019.05.010.
- Pan D, Wang LJ, Cheng AH, Ying LX. Investigation on awareness of HPV vaccine among female college students in Taizhou city and influencing factors of vaccination intention. Prac Prev Med. 2020;27(5):595–97. doi:10.3969/j.1006-3110.2020.05.023.
- Yang J, Xu LJ, Xu L, Yu M, Cheng YM, Nie N. Awareness of HPV and HPV vaccine among non-medical college students in Xi’an. Chin J Matern Child Health J. 2016;27(8):923–25. doi:10.3969/j.1673-5293.2016.08.007.
- Ma D, Wei Y, Li O, Wang WC. Study on medical student knowledge and attitudes regarding HPV and its vaccine. Matern Child Health Care Chin. 2013;28:4699–701. doi:10.7620/zgfybj.j.1001-4411.2013.28.42.
- Jiang SF, Liu M. Investigation on awareness of HPV vaccine among college students in Zhejiang province: based on comparative analysis between Ningbo and Taizhou. Mod Bus Trade Ind. 2020;15:56–58. doi:10.19311/j.cnki.1672-3198.2020.15.026.
- Zeng XM, Ren ZF, Wei XL, Lin W, Qiao YL. Investigation on cognition of HPV and vaccine among undergraduates in Sun Yat sen University. Mod Preventive Med. 2015;42:1822–25.
- Fu SL. Research on cognition and attitude of Chinese mainland population on HPV preventive vaccine [dissertation]. Beijing (China): Peking Union Medical College; 2019.
- Wang SM, Zhang SK, Pan XF, Ren ZF, Yang CX, Wang ZZ, Gao XH, Li M, Zheng QQ, Ma W, et al. Human papillomavirus vaccine awareness, acceptability, and decision-making factors among Chinese college students. Asian Pac J Cancer Prev. 2014;15(7):3239–45. doi:10.7314/APJCP.2014.15.7.3239.
- Liu A, Ho FK, Chan LKL, Ng JYW, Li SL, Chan GCF, Leung TF, Ip P. Chinese medical students’ knowledge, attitude and practice towards human papillomavirus vaccination and their intention to recommend the vaccine. J Paediatr Child Health. 2018;54(3):302–10. doi:10.1111/jpc.13693.
- Chiang VCL, Wong HT, Yeung PCA, Choi YK, Fok MSY, Mak OI, Wong HY, Wong KH, Wong SY, Wong YS, et al. Attitude, acceptability and knowledge of HPV vaccination among local university students in Hong Kong. Int J Environ Res Public Health. 2016;13(5):486. doi:10.3390/ijerph13050486.
- Choi EPH, Wong JYH, Lau AYY, Fong DYT. Gender and sexual orientation differences in Human Papillomavirus (HPV) vaccine uptake among Chinese young adults. Int J Environ Res Public Health. 2018;15(6):1099. doi:10.3390/ijerph15061099.
- Ouyang LC, Wang SQ, Hu ML, Gong YL. Investigation on cognition and vaccination willingness of female medical students of Jianghan University on HPV and HPV vaccine. J Jianghan Univ (Nat Sci Ed). 2020;48(5):47–54. doi:10.16389/j.cnki.cn42-1737/n.2020.05.006.
- Cocchio S, Bertoncello C, Baldovin T, Fonzo M, Bennici SE, Buja A, Majori S, Baldo V. Awareness of HPV and drivers of HPV vaccine uptake among university students: a quantitative, cross-sectional study. Health Soc Care Community. 2020:1–11. doi:10.1111/hsc.12974.
- Rashid S, Labani S, Das BC. Knowledge, awareness and attitude on HPV, HPV vaccine and cervical cancer among the college students in India. Plos One. 2016;11(1):e0166713. doi:10.1371/journal.pone.0166713.
- Oz M, Cetinkaya N, Apaydin A, Korkmaz E, Bas S, Ozgu E, Gungor T. Awareness and knowledge levels of Turkish college students about human papilloma virus infection and vaccine acceptance. J Cancer Educ. 2016;33(2):260–68. doi:10.1007/s13187-016-1116-0.
- Chanprasertpinyo W, Rerkswattavorn C. Human Papillomavirus (HPV) vaccine status and knowledge of students at a university in rural Thailand. Heliyon. 2020;6(8):e04625. doi:10.1016/j.heliyon.2020.e04625.
- Ratanasiripong NT, Cheng AL, Enriquezc M. What college women know, think, and do about Human Papillomavirus (HPV) and HPV vaccine. Vaccine. 2013;31(11):1370–76. doi:10.1016/j.vaccine.2013.01.001.
- Giede C, McFadden LL, Komonoski P, Agrawal A, Stauffer A, Pierson R. The acceptability of HPV vaccination among women attending the university of Saskatchewan student health services. Gynecol Oncol. 2010;116(3):679–86. doi:10.1016/j.ygyno.2009.10.036.
- Kang HY, Kim JS. Knowledge, attitudes of human papillomavirus vaccine, and intention to obtain vaccine among Korean female undergraduate students. Women Health. 2011;51(8):759–76. doi:10.1080/03630242.2011.627091.
- Borlu A, Gunay O, Balcı E, Sagıroglu M. Knowledge and attitudes of medical and non-medical Turkish university students about cervical cancer and HPV vaccination. Asian Pac J Cancer Prev. 2016;17(1):299–303. doi:10.7314/APJCP.2016.17.1.299.
- Gantz L, Calvo A, Hess-Holtz M, et al. Predictors of HPV knowledge and HPV vaccine awareness among women in Panama city, Panama. World Med Health Policy. 2019;11(1):95–118. doi:10.1002/wmh3.293.
- Chido-Amajuoyi OG, Jackson I, Yu R, Shete S. Declining awareness of HPV and HPV vaccine within the general US population. Hum Vaccin Immunother. 2020:7. doi:10.1080/21645515.2020.1783952.
- McCusker SM, Macqueen I, Lough G, MacDonald AI, Campbell C, Graham SV. Gaps in detailed knowledge of Human Papillomavirus (HPV) and the HPV vaccine among medical students in Scotland. BMC Public Health. 2013;13:264. doi:10.1186/1471-2458-13-264.
- Bettinghaus EP. Health promotion and the knowledge-attitude-behavior continuum. Prev Med. 1986;15(5):475–91. doi:10.1016/0091-7435(86)90025-3.
- Zhao FH, Qiao YL. Cervical cancer prevention in China: a key to cancer control. Lancet. 2019;393(10175):969–70. doi:10.1016/S0140-6736(18)32849-6.
- Canfell K. Towards the global elimination of cervical cancer. Papillomavirus Res. 2019;8:100170. doi:10.1016/j.pvr.2019.100170.
- Wang WZ, Lyu JL, Li MT, Zhang YJ, Xu ZH, Chen YY, Zhou JJ, Wang SF. Quality evaluation of HPV vaccine-related online messages in China: a cross-sectional study. Hum Vaccin Immunother. 2020:9. doi:10.1080/21645515.2020.1814095.
- Kester LM, Shedd-Steele RB, Dotson-Roberts CA, Smith J, Zimet GD. The effects of a brief educational intervention on human papillomavirus knowledge and intention to initiate HPV vaccination in 18–26 year old young adults. Gynecol Oncol. 2014;132:S9–12. doi:10.1016/j.ygyno.2013.12.033.
Appendix A.
Search strategy
The last search date was October 8, 2020.
1. Web of Science, WOS
2. PubMed
Query: (“vaccine”[Title] OR “vaccination”[Title]) AND (“HPV”[Title] OR “human papillomavirus”[Title])
Results: 5,727
3. Science of Direct, SOD
Query: Title: (HPV OR human papillomavirus) AND (vaccine OR vaccination)
Results: 2,373
4. EBSCO
Query: TI (HPV OR human papillomavirus) AND TI (vaccine OR vaccination)
Results: 21,028
5. China National Knowledge Infrastructure, CNKI
Query: (TI = ‘HPV’ OR TI = ‘human papillomavirus’ OR TI = ‘人乳头瘤病毒’) AND (TI = ‘疫苗’ OR TI = ‘接种’ OR TI = ‘免疫’ OR TI = ‘vaccine’ OR TI = ‘vaccination’)
Results: 12,238
6. Wanfang Data
Query: (题名:(HPV) OR 题名:(human papillomavirus) OR 题名:(人乳头瘤病毒)) AND (题名:(疫苗) OR 题名:(接种) OR 题名:(免疫) OR 题名:(vaccine) OR 题名:(vaccination))
Results: 7,632