ABSTRACT
Traditionally, the management of active relapsing remitting MS was based on the, so-called, maintenance therapy, which is characterized by continuous treatment with particular disease modifying therapy (DMT), and a return of disease activity when the drug is discontinued. Another approach is characterized by a short treatment course of a DMT, which is hypothesized to act as an immune reconstitution therapy (IRT), with the potential to protect against relapses for years after a short course of treatment. Introduction of monoclonal antibodies in the treatment of MS has revolutionized MS treatment in the last decade. However, given the increasingly complex landscape of DMTs approved for MS, people with MS and neurologists are constantly faced with the question which DMT is the most appropriate for the given patient, a question we still do not have an answer to. In this product review, we will discuss the first DMT that acts as IRT, an anti-CD52 monoclonal antibody alemtuzumab and an anti CD20 monoclonal antibody, ocrelizumab that has the potential to act as an IRT, but is administered continuously. Special emphasis will be given on safety in the context of COVID-19 pandemics and vaccination strategies.
Introduction
Multiple sclerosis (MS) is a lifelong immune-mediated inflammatory and neurodegenerative disease of the central nervous system (CNS) that according to 2020 data affects nearly 2.8 million people worldwide.Citation1,Citation2
Although the exact cause of the disease remains unknown, the pathophysiological process engages environmental and genetic factors as well as altered immunological response. The pathological hallmark of these interactions in MS are inflammation, demyelination, axonal damage, gliosis, and remyelination.Citation3
MS is categorized into three major clinical subtypes: relapsing-remitting MS (RRMS), affecting 85% of patients, that over time in part of the subjects proceeds to secondary progressive MS (SPMS), characterized by worsening disability. At the beginning of the disease 10–15% of MS patients are diagnosed with primary progressive MS (PPMS), a distinct clinical phenotype characterized by continuous clinical deterioration leading to impairment of ambulation.Citation4
In recent years, following the rising knowledge about MS immunology, there has been an increase in available disease modifying therapies (DMT). Although these drugs have a marked impact on the reduction of inflammatory disease activity, the influence on disability progression is less pronounced.Citation5 The treatment of progressive forms of MS continues to be a challenge with, at the moment, limited treatment options.
Treatment approaches in multiple sclerosis
Traditionally, the management of active RRMS is based on the, so-called, maintenance therapy, which is characterized by continuous treatment with particular DMT, and a return of disease activity when the drug is discontinued.Citation6 In the event of occurrence of disease activity (in the form of relapses or new T2 or Gd+ lesions), a DMT with higher efficacy is usually initiated (). This approach in sequencing of different DMTs depending on their efficacy/safety profile is called the escalation approach.
Figure 1. The management of active RRMS is based on the disease activity and prognostic factors. (A) Following the diagnosis of RRMS, treatment with disease modifying therapy (DMT) with moderate efficacy and good safety profile is initiated. In the event of occurrence of disease activity (in the form of relapses or new T2 or Gd+ lesions), a DMT with higher efficacy is usually initiated. This approach in sequencing of different DMTs depending on their efficacy/safety profile is called the escalation approach. (B) If the patient has highly active RRMS or poor prognostic factors, treatment with high-efficacy DMTs is started from the diagnosis of RRMS. Monoclonal antibodies which have the potential to act as an immune reconstitution therapy (alemtuzumab and ocrelizumab) are frequently used in this situation.
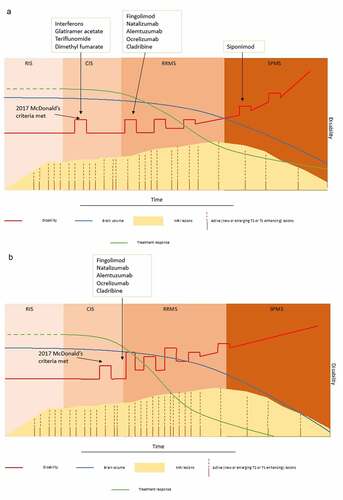
Another approach is characterized by a short treatment course of a DMT, which is hypothesized to act as an immune reconstitution therapy (IRT), with the potential to protect against relapses for years after a short course of treatment ().Citation6
In this product review we will discuss monoclonal antibodies which have the potential to act as an IRT: an anti-CD52 monoclonal antibody alemtuzumab indicated for the treatment of RRMS and an anti-CD20 monoclonal antibody ocrelizumab indicated for the treatment of RRMS and PPMS.
Alemtuzumab
Alemtuzumab (Lemtrada®) is a genetically engineered, humanized, IgG1 kappa monoclonal antibody with specific binding propensity toward CD52, a human cell surface antigen.Citation7 Although the exact role of CD52 in immune response is not fully elucidated, there is evidence that it is an important contributor in T-cell costimulation and migration.Citation8 CD52 antigen is highly expressed on T and B lymphocytes with low or no expression on cellular component of the innate immune system such as monocytes, macrophages, natural killer (NK) cells, neutrophils, bone marrow stem cells, or plasma cells.Citation9 Thus, by depleting T and B lymphocytes, predominantly by mechanisms of antibody dependent cell-mediated cytolysis (ADCC), complement-dependent cytolysis (CDC), and induction of apoptosis,Citation10–12 it mostly leaves effectors of innate immune system intact.
Alemtuzumab was approved by the European Medicines Agency (EMA) under the name Lemtrada® for use in treatment of active relapsing-remitting multiple sclerosis (RRMS) in 2013Citation13 based on results of 3 core clinical trials, one 3-year phase 2 (CAMMS223)Citation14 and two 2-year phase 3 trials (CARE-MS I)Citation15 and (CARE-MS II).Citation16 However, the drug was previously in use under name Campath® and MabCampath® following its approval in 2001 by the US Food and Drug Administration (FDA) and the EMA for the treatment of B-cell chronic lymphocytic leukemia (B-CLL).Citation17 Currently, alemtuzumab is used in conditioning protocol prior to tissue transplantation, in prevention of transplant rejection and graft versus host reaction and in various hematological malignancies.Citation18 Since November 2019, due to EMA restriction, alemtuzumab is used to treat patients with highly active RRMS, defined as highly active disease despite prior DMT use or rapidly evolving severe disease.Citation19 Treatment regime includes 2 treatment courses with recommended dose of 12 mg/day administered by intravenous (IV) infusion. For the first course it is used for 5 consecutive days and 12 months thereafter the second course is administered for 3 consecutive days. In patients who after two treatment courses have breakthrough disease activity, it is possible to apply third and fourth course, each administered for 3 consecutive days and after at least 12 months from the previous one.
Mechanism of action
Mechanism of action of alemtuzumab in MS is not fully explained, but it is considered that the drug expresses its immunomodulatory effect through depletion and subsequent repopulation of T and B lymphocytes. Pharmacokinetics of alemtuzumab, considering data from phase 2 and 3 clinical trials for dose of 12 mg /day, indicate that serum concentrations increase with each consecutive dose and the mean maximum serum concentration (Cmax) is accomplished after the last infusion in a treatment course.Citation7 The assumed metabolic pathway is protein catabolism,Citation20 and serum concentrations generally become below the Limit of Quantitation (BLQ) within approximately 30 days following each treatment course.Citation7 Elimination of alemtuzumab is dependent on lymphocyte count with lower count decreasing clearance of alemtuzumab and is also dependent on presence of anti-drug antibodies (ADA).Citation7 In CARE-MS I and CARE-MS II, 85.2% of the study population receiving 12 mg was positive for ADA at any time point during the 2-year treatment course and 92.2% developed inhibitory ADA. Presence of ADA was associated with slower clearance of alemtuzumab from circulation but had no significant impact on the pharmacodynamics.
It is considered that therapeutic effect of alemtuzumab is achieved by rebalancing of the immune system with repopulation of different lymphocytes subsets in various proportions, numbers, and time periods. Total lymphocyte counts return to baseline levels in the majority (80%) of patients after 12 months.Citation9 After initial depletion, B lymphocytes repopulate to baseline levels by 6 months while T cell counts do not reach baseline levels by 12 months.Citation21
B-cell reconstitution following alemtuzumab occurs in a manner of hyperpopulation. In a study including 78 patients with RRMS who participated in Phase II trials, after their return to baseline, B cells continued to rise, reaching 165% of baseline by 12 months.Citation22 Also, the authors suggested that B-lymphocyte repopulation after alemtuzumab treatment resulted in a B-cell subtypes tending toward immature phenotypes, driven by increased serum levels of BAFF, and that prolonged memory B-cell depletion may contribute to the efficacy of alemtuzumab in MS.Citation22 On the other hand, it was also suggested that hyperrepopulation of immature B cells in the absence of regulatory T cells may be one of the contributors in development of secondary B cell autoimmunity following alemtuzumab treatment.Citation21
Based on the studies evaluating patterns of reconstitution of T cell subsets after alemtuzumab treatment, it is speculated that CD4 + T cell repopulation is responsible for remission or resumed disease activity.Citation23,Citation24 Regulatory T-cells (Treg) are important mediators in the maintenance of peripheral immune tolerance by suppressing potentially auto-aggressive conventional CD4 + T-cells (Tcon) subtype. During immunological reconstitution CD4+ CD25+ CD127 low Treg cell expand,Citation25 and percentage of CD4+ CD25+ CD127lowTreg cell which produce TGF-b1–, IL-10–, and IL-4 is highest at month 3.Citation23 In another study significant increase in Treg cell percentage was observed at month 24 that was accompanied by an increase in Treg cell suppressive activity against myelin basic protein (MBP)-specific Th1 and Th17 cells which could explain the long-lasting therapeutic benefit of alemtuzumab in RRMS.Citation26 However, there is a recent study suggesting that Treg are not spared from alemtuzumab-mediate depletion and that enhanced inhibitory effect of Treg following alemtuzumab is due to altered composition and reactivity of postdepletional Tcon.Citation27
Although, CD52 antigen is far less expressed on cellular component of innate immune system such as dendritic cells (DC), monocytes, macrophages, natural killer (NK) cells, neutrophils, bone marrow stem cells, or plasma cells, it has been demonstrated that 6 months after alemtuzumab treatment, specific DC subsets were reduced, while CD56bright NK cells expanded in patients with MS.Citation28 Even though, increased number and function of the CD56bright NK-cell subset was associated with beneficial effects of daclizumab, a humanized monoclonal antibody directed against the IL-2 receptor chain,Citation29 increased numbers of CD56bright NK cells have also been noticed in several autoimmune disorders, one of them being Hashimoto thyroiditis,Citation30 very common side effect of alemtuzumab treatment. So, remodeling of the innate immune compartment may play a role in both efficacy of alemtuzumab but also in development of side effects, in particular secondary autoimmunity.
Efficacy of alemtuzumab
Evidence from core clinical trials
Core clinical trials in which efficacy of alemtuzumab in active RRMS was assessed included one 3-year phase 2 clinical trial (CAMMS223)Citation14 and two confirmatory 2-year phase 3 trials (CAMMS323/CARE-MS ICitation15 and CAMMS324/CARE-MS IICitation16).
Treatment naïve patients were enrolled into CAMMS223 and CARE-MS I, whilst CARE-MS II enrolled patients who failed previous interferon (IFN) β-1a or glatiramer acetate therapy. Alemtuzumab significantly reduced the annual relapse rare (ARR) versus IFNβ-1a in all three clinical trials (). Subgroup analysis of patients from CARE-MS studies who fulfilled criteria for highly active RRMS showed similar findings (0.26 in the alemtuzumab group vs 0.51 in the IFNβ-1a; p < .001). In CARE-MS I studies alemtuzumab did not significantly reduced 6-month SAD versus interferon, while in CARE- MS II significantly less patient experienced SAD in alemtuzumab cohort ().
Table 1. Main outcomes of core clinical trials with alemtuzumab in RRMS and ocrelizumab in RRMS and PPMS
Regarding the MRI outcomes, no difference was observed between treatment groups in median change in volume of T2-hyperintense lesions in both CARE-MS I and II trials. However, in both trials, significantly less patients in alemtuzumab cohort had gadolinium-enhancing and new or enlarging T2-hyperintense lesions at 24 months. Median change in brain parenchymal fraction significantly differed between groups (–0.867% in the alemtuzumab group vs – 1.488% in the IFNβ-1a; p <.0001 in CARE-MS I and – 0.615% in the alemtuzumab group vs – 0.810% in the IFNβ-1a; p <.01 in CARE-MS II).
Finally, statistically significant improvements from baseline with alemtuzumab were observed health related quality of life (HR-QOL) at the earliest postbaseline assessment and sustained through Year 2.Citation31
Evidence from extension studies
Long-term extension studies CAMMS03409 and TOPAZ evaluated long-term effectiveness and safety of alemtuzumab.Citation32,Citation33 Participants who were previously on SC IFNβ-1a were switched to alemtuzumab. Participants previously treated with alemtuzumab could receive additional course of alemtuzumab 12 mg for 3 consecutive days if they had documented evidence of resumed disease activity.
For participants from CAMMS223 12-year follow-up,Citation34 and for participants from CAMMS323 and 324, 5-year follow-up data were reported.Citation35,Citation36 Effectiveness data are summarized in . In CAMMS223, no evidence of disease activity (NEDA) from years 7 to 12 was accomplished in 34% participants.Citation34 NEDA in years 3, 4, and 5 was achieved in 61.7%, 60.2%, and 62.4% of participants from CAMMS323, respectively.Citation35 In years 3, 4, and 5, proportions of participants with NEDA were 52.9%, 54.2%, and 58.2% for participants from CAMMS324, respectively.Citation36
Table 2. Main outcomes of extension studies with alemtuzumab in RRMS
A post-hoc analysis of CARE-MS study population investigated alemtuzumab outcomes by baseline age (≥18 to ≤25, >25 to ≤35, >35 to ≤45, >45 to ≤55 years) in 8 year follow up to find that alemtuzumab had greater efficacy than SC IFNB-1a over 2 years across comparable age groups, with no significant differences between alemtuzumab-treated age groups.Citation37
Several other post-hoc analyses mainly investigated long-term effectiveness in participants with highly active disease,Citation33 and in participants who experience relapse in between 1st and 2nd cycles,Citation38 or after 2nd cycle of alemtuzumab.Citation39 In all three analyses, alemtuzumab showed low ARR, high percentage of patients who were free of 6-month CDW and favorable MRI outcomes. Of 742 CARE-MS patients who entered the CARE-MS extension, 396 (53%) received no more than two courses over 8 years, 201 (27%) received three courses, 94 (13%) received four courses, and 51 (<7%) received five or more courses over 8 years.Citation39
Evidence from real-world studies
There are limited real world data on effectiveness of alemtuzumab (). A retrospective study using data from 8 Italian centers in which 322 patients were switching from other DMT (reason for switch was relapse-rate (41.3%), MRI activity (22.8%), JCV+ (18.2%), EDDS progression (4.9%), other (12.8%)) to alemtuzumab showed that ARR decreased independently of previous DMT (prealemtuzumab ARR was 0.99 and ARR during alemtuzumab was 0.13, p < .001). Additional finding of this study was that relapses between treatment courses were associated with higher disease activity during follow-up.Citation40 Four studies showed high variation in percentage of pwMS treated with alemtuzumab who achieve NEDA-3, ranging from 29.2 to 66.7%.Citation41–44 Nevertheless, the effectiveness of alemtuzumab seems to be higher if administered as first line therapy.Citation45,Citation46
Table 3. Main outcomes from real-world studies with alemtuzumab in RRMS and ocrelizumab in RRMS and PPMS
Of special interest are studies investigating comparative effectiveness of high-efficacy DMTs. A comparison between the effectiveness and safety of autologous hematopoietic stem cell transplant (aHSCT) (n = 25) and alemtuzumab (n = 32) in aggressive RRMS during 24 months of follow-up showed that NEDA-3 was more frequently achieved in aHSCT cohort than in alemtuzumab-treated patients (75% vs 56% p = .023).Citation47 In an international, observational study that compared effectiveness of alemtuzumab (n = 189), natalizumab (n = 1160), IFNβ-1a (n = 2155), and fingolimod (n = 828) over ≥ 5 years’ treatment, alemtuzumab, and natalizumab had similar effects on ARR but alemtuzumab seemed to be superior to fingolimod (0.15 vs 0.34, p < .0001) and interferon beta (0.19 vs 0.53, p < .0001). Natalizumab was superior to alemtuzumab in enabling recovery from disability.Citation48 On the other hand, another observational study that compared effectiveness of alemtuzumab and natalizumab showed that after 12 months of treatment, the EDSS score of RRMS patients treated with natalizumab was significantly lower compared with the patients treated with alemtuzumab (1.23 vs 2.56, p < .05).Citation49 A small observational study including 16 patients switching from natalizumab to alemtuzumab due to high risk of progressive multifocal leukoencephalopathy (PML) showed that clinical evaluation performed at 6 and 12 months showed stability, in particular neither relapses nor an increase in EDSS were observed.Citation50 Similar finding were obtained from a study on pediatric population in which after median of 3.9 years of follow-up NEDA-3 was sustained.Citation51 In a larger, single-center Italian study with mean follow up of 27 months, involving 90 patients with RRMS who started alemtuzumab treatment either due to highly aggressive disease or high risk of PML, 43.7% of patients achieved NEDA-3. EDSS was reduced after the treatment with alemtuzumab (from a median of 2.5 (IQR 1.5–4) before to 2.0 (IQR 1.5–3.5) after, p = .025).Citation52
On the other hand, several studies have shown that therapy switch from fingolimod to alemtuzumab was highly effective in reducing clinical and MRI disease activity.Citation53–55 Unfortunately, there are no studies yet investigating comparative effectiveness of alemtuzumab with ocrelizumab or cladribine.
Finally, observational studies showed that alemtuzumab stabilized overall cognitive functioning in active RRMS and positively affected cognitive processing speed,Citation56 and also to improved patient-reported outcomes in the observational PRO-ACT,Citation57 and PROMiS studies.Citation58
Safety of alemtuzumab
The most common adverse events (AEs) in clinical trials were rash, headache, fever and respiratory tract infections.Citation13,Citation15,Citation16 The AEs of special interest in follow-up were infusion associated reactions (IARs), secondary autoimmunity and infections. The length of the time period from alemtuzumab administration and occurrence of AEs defines subgroups of AEs into: (i) immediate comprising of IARs, (ii) periinfusional AEs including infections and cardiovascular, cerebral, gastrointestinal, and pulmonary complication, and (iii) late, such as secondary autoimmune disorder ().
Table 4. Adverse events associated with alemtuzumab and ocrelizumab
Infusion associated reactions
Most common AEs (experienced by 90.1% of patient) in CARE-MS program were IARs considered to be consequence of cytokine release associated with alemtuzumab-induced lymphocyte lysis.Citation15,Citation16 Most IARs were mild-to-moderate in severity while serious IARs such as fever, nausea, headache, urticaria, hypotension, tachycardia, atrial fibrillation, and chest discomfort were experienced in 3.1%. Treatment discontinuation due to IARs was low; one (0.03%) patient discontinued treatment in CARE-MS I study due to allergic dermatitis and five (1.1%) discontinued treatment in CARE-MS II due to noncardiac chest pain and dyspnea in one patient, and pharyngeal edema, rash, purpura, and urticaria each in one patient. Mitigation strategies for prevention of IARs are shown in .Citation59,Citation60
Periinfusional AEs
The most common periinfusional AEs associated with alemtuzumab are infections, which are predominantly (>95%) mild to moderate and include upper respiratory tract infections, urinary tract infections, and mucocutaneous herpetic infections. Infections occur more frequently with alemtuzumab than SC IFNB-1a during Years 1 (58.7% vs 41.3%) and 2 (52.6% vs 37.7%), but declined for alemtuzumab-treated patients in Years 3 (46.6%), 4 (42.8%), 5 (40.9%), and 6 (38.1%). Serious infections were not frequent (1.0%–1.9% per year) and most commonly included pneumonia, gastroenteritis, varicella zoster and appendicitis. Frequency of opportunistic infections was even lower and accounted 0.8% of participants who received alemtuzumab and included herpes infections (n = 3; varicella zoster meningitis, varicella zoster, multidermatomal varicella zoster), candidiasis (n = 4), cytomegalovirus infection (n = 1), and acute disseminated tuberculosis (n = 1). Lymphocyte counts after alemtuzumab therapy did not predict infection risk.Citation61 Occasional cases from post-marketing setting have shown serious opportunistic infections in alemtuzumab treated patients such as Listeria monocytogenes, Cytomegalovirus, Pneumocystis jiroveci, and Nocardia spp.Citation62 Recommended preventive measures are shown in .Citation13
In postmarketing setting rare cases of acute acalculous cholecystitis developing during of shortly after alemtuzumab administration were described, and the underlying mechanism may be similar to infusion-associated reactions mediated by a systemic inflammatory response.Citation63
During postmarketing pharmacovigilance in April 2019, EMA issued an assessment report based on marketing authorization holder’s (MAH) safety database searched from September 2013 through 31 March 2019 with 55,431 patient-years (PY) of exposure. Two cases of myocardial ischemia, 27 cases of myocardial infarction, 22 cases of potential myocardial ischemia or myocardial infarction, 25 cases of cerebrovascular accidents, including 6 cases of arterial dissection, 7 cases of pulmonary hemorrhage, 20 cases of pulmonary embolism, and 68 cases of immediate nonimmune-mediated thrombocytopenia were identified as risks in close temporal (≤ 30 days) association with the infusion of alemtuzumab.Citation19 The mechanism of these rare AEs is still unclear, but may be related to increased cytokine release following alemtuzumab infusion.
Secondary autoimmunity
Secondary autoimmunity in alemtuzumab-treated patients is not fully elucidated but one of the hypothesis is that CD52+ cells depletion followed by the rapid repopulation of B cells in the relative absence of T-cell regulatory mechanisms that promote immune tolerance may account for the secondary B-cell mediated autoimmunities.Citation64 Additionally, secondary autoimmunity may appear when homeostatic proliferation predominates thymopoiesis in repopulation of T cells.Citation65 Alemtuzumab is considered to increase risk of thyroid disorders, immune thrombocytopenic purpura (ITP), nephropathies, and autoimmune hepatitis.Citation19 Furthermore, cases of severely exacerbated central nervous system (CNS) inflammation have been described,Citation66–68 as well as systemic erythematosus lupus (SLE),Citation69 cytopenias,Citation70 and acquired hemophilia A.Citation71
The most common autoimmune AEs, experienced by 42% of patients are thyroid AEs such as hyperthyroidism (including Graves’ disease), hypothyroidism, thyroiditis, and goiter. The rate of thyroid AEs peaks in Year 3 and subsequently declines. Most thyroid disorders associated with alemtuzumab are mild or moderate and no deaths occurred as a result of thyroid events.Citation72 A systematic review and meta-analysis including 1362 MS patients from seven studies treated with alemtuzumab found that prevalence of newly diagnosed thyroid adverse events was 33%. Graves’ disease was the most represented (63% of cases), followed by Hashimoto thyroiditis (15%). Spontaneous remission was observed in 12% of patients with Graves’ disease, 56% were treated with antithyroid drugs only but 22% (95% CI 13–32%) needed additional radioiodine. Definitive surgery was performed in 11% of patients with Graves’ disease.Citation73
In the clinical development program over a median of 6.1 years of follow-up 33 (2.2%) patients treated with alemtuzumab developed ITP.Citation74 Corticosteroids, platelets, and/or intravenous immunoglobulins are used as first line treatment for ITP. ITP incidence in postmarketing setting is considered to be 0.72%.Citation74
Autoimmune nephropathies associated with alemtuzumab include antiglomerular basement membrane (anti-GBM) disease, membranous glomerulonephropathy and serum anti-GBM antibody without typical anti-GBM disease. The incidence of autoimmune nephropathies within clinical trials was 0.34% (5/1485 patients) and 0.05% in the postmarketing setting. The five cases from clinical trials were identified early, responded to conventional therapy (where needed), and had favorable outcomes. All anti-GBM disease cases with documented urinalysis demonstrated prior microscopic hematuria.Citation75
Autoimmune hepatitis (AIH) was found in a total of 40 unique case reports in the MAH’s database but only 9 cases had enough information and no known concomitant conditions/events/medications. The nine cases of AIH in alemtuzumab-treated patients translate into a reporting rate of 16 cases per 100,000 person-years.Citation19 Additionally, 9 out of 11 cases with biopsy proven AIH had preexisting or had developed autoimmune thyroid conditions prior to the development of AIH suggesting that autoimmune propensity and the potential for poly-autoimmunity are important factors to take into account for minimizing the risk of autoimmune conditions associated with alemtuzumab. In addition, a new signal was identified and analyzed in this procedure and that were cases of acquired hemophilia A (antifactor VIII antibodies) that have been reported in both clinical trial and postmarketing setting. In addition, 13 cases of autoimmune-mediated CNS disease and 10 cases of Guillain-Barre Syndrome (GBS). Hemophagocytic lymphohistiocytosis in 11 cases, 2 with fatal outcome. Overall mortality rate in the postmarketing setting is 0.42% for EU patients. Finally, Epstein-Barr virus (EBV) hepatitis, another opportunistic infection, was described.Citation19
Therapeutic indication, dosage, administration, and monitoring
Alemtuzumab is indicated in treatment of adults with highly active RRMS either in patients with highly active disease despite a full and adequate course of treatment with at least one DMT or in patients with rapidly evolving severe RRMS defined by two or more disabling relapses in one year, and with one or more Gadolinium enhancing lesions on brain MRI or a significant increase in T2 lesion load as compared to a previous recent MRI. Treatment should only be initiated and supervised by a neurologist experienced in the treatment of patients with MS in a hospital with ready access to intensive care. Contraindication for alemtuzumab are: hypersensitivity to the active substance or to any of the excipients, HIV infection, severe active infection until complete resolution, uncontrolled hypertension, history of arterial dissection of the cervicocephalic arteries, history of stroke, history of angina pectoris or myocardial infarction, known coagulopathy, on antiplatelet or anticoagulant therapy and other concomitant autoimmune diseases (besides MS). The recommended dose of alemtuzumab is 12 mg/day administered by intravenous infusion (duration of each infusion should be approximately 4 hours) for two initial treatment courses, with up to two additional treatment courses if needed. For the first course alemtuzumab is administered for 5 consecutive days and 12 months thereafter the second course is administered for 3 consecutive days. Each additional course should be 12 months after the previous one and the drug is administered for 3 consecutive days. Immediately prior to each alemtuzumab infusion patients should be pre-treated with corticosteroids each of the first 3 days of any treatment course. Pretreatment with antihistamines and/or antipyretics prior to alemtuzumab administration may also be considered. Oral prophylaxis for herpes infection should be administered to all patients starting on the first day of each treatment course and continuing for a minimum of 1 month following treatment. In addition, prior to each infusion a baseline ECG and heart rate and blood pressure measurement should be obtained. At least every hour during infusion monitoring of heart rate, blood pressure and overall clinical status of the patients should be performed. Observation for infusion reactions is recommended for a minimum of 2 hours after infusion. Platelet count should be obtained immediately after infusion on days 3 and 5 of the first infusion course, as well as immediately after infusion on day 3 of any subsequent course. Complete blood count with differential, serum transaminases, serum creatinine levels and urine analysis should be performed at monthly intervals at least 48 months following the last treatment and thyroid stimulating hormone level should be obtained every 3 months for the same time period. Before initiation of therapy, all patients must be evaluated for both active or inactive (“latent”) tuberculosis infection, according to local guidelines. To reduce the risk of listeriosis/listeria meningitis, patients should avoid ingestion of uncooked or undercooked meats, soft cheeses and unpasteurized dairy products 2 weeks prior to, during, and for at least 1 month after alemtuzumab infusion. If compliance with Listeria-free diet cannot be achieved than cotrimoxazole 960 mg three times a week for 1 month after each cycle of alemtuzumab should be administered. It is recommended that HPV screening be completed annually for female patients.Citation76
Alemtuzumab and pregnancy
Data from the use of alemtuzumab in pregnant women are limited. It is not known whether alemtuzumab can cause fetal harm when administered to pregnant women or whether it can affect reproductive capacity. Serum concentrations generally fall below the limit of quantitation (BLQ) within approximately 30 days following each treatment course,Citation7 and women of childbearing potential have to use effective contraception when receiving a course of treatment with alemtuzumab and up to 4 months after each treatment course.Citation76 A report of pregnancy outcomes in alemtuzumab-treated women from the phase 2 and 3 clinical development program over 16 years found 264 pregnancies in 160 alemtuzumab-treated women, with a mean age at conception of 32.6 years, and mean time from last alemtuzumab dose to conception of 35.9 months. Of the 264 pregnancies 16 (6%) conceptions occurred within 4 months, and 5 conceptions within 1 month of the last alemtuzumab dose. Of the 233 completed pregnancies with known outcomes, there were 155 (67%) live births with no congenital abnormalities or birth defects, 52 (22%) spontaneous abortions, 25 (11%) elective abortions, and 1 (0.4%) stillbirth. Maternal age was associated with an increased risk of spontaneous abortion and the risk was not increased neither in women with pregnancy onset within 4 months of alemtuzumab exposure nor in women having autoimmune thyroid AEs.Citation77 Breast-feeding should be discontinued during each treatment course and for 4 months following the last infusion of each treatment course.Citation76
Alemtuzumab and COVID-19
COVID-19 is the pandemic disease caused by severe acute respiratory syndrome (SARS) coronavirus 2 (SARS-CoV-2) infection.Citation78 Considering significant infectious risks with alemtuzumab especially in the first two years of treatment initially it was speculated that the risk of COVID19 may be higher in patients treated with alemtuzumab.Citation79 However, there are cases reported even with a short time period between last alemtuzumab infusion and SARS-CoV-2 infection with favorable clinical outcome,Citation80 and also there is a report of a patient who acquired COVID-19 only 3 months after the last cycle of alemtuzumab and was able to produce SARS-CoV-2 antibodies.Citation81 A study involving 565 MS patients with suspected SARS-CoV-2 infection and 279 MS patients with confirmed SARS-CoV-2 infection from 85 Italian MS centers found that progressive MS course, higher EDSS, higher body mass index (BMI), comorbidities, and recent methylprednisolone use as well as therapy with an anti‐CD20 agent (ocrelizumab or rituximab) was significantly associated (odds ratio [OR] = 2.37, 95% confidence interval [CI] = 1.18–4.74, p = .015) with increased risk of severe COVID‐19. No warning signal for alemtuzumab has been reported in this cohort.Citation82 A recent systematic review that included 2493 MS patients and 37 neuromyelitis optica spectrum disorder (NMOSD) patients with COVID-19 from 84 studies found 37 reported patients on alemtuzumab and COVID-19. Most of them had a benign course and recovered completely, and none of them died. Of all MS patients included in this review 46 (1.8%) had fatal outcomes.Citation83
Vaccination and alemtuzumab treatment
Although vaccinations are safe and effective for the vast majority of pwMS, some specific considerations should be kept in mind when planning vaccination strategies before, during and after receiving alemtuzumab.Citation84 Live attenuated vaccines are contraindicated during treatment with alemtuzumab. However, pwMS who have been treated with an immune reconstitution therapy like alemtuzumab in the past and have reconstituted their peripheral immune systems should be able to respond to any vaccine (including live attenuated vaccines). If an individual had an incomplete immune reconstitution, they may still consider having a COVID-19 vaccine with the potential for a blunted immune response, as studies have shown that vaccination within 6 months of treatment with alemtuzumab results in a smaller proportion of vaccine responders.Citation85 Although some of the vaccines used for COVID-19 are live attenuated vaccines, the adenovirus genes required for viral replication are disabled. Thus, the adenovirus vector used in these vaccines is not able to cause adenoviral infection, making it highly likely to be safe for people with MS using any DMT, including alemtuzumab.Citation86
Ocrelizumab
Ocrelizumab (Ocrevus®) is a recombinant humanized monoclonal antibody that targets CD20-expressing B cells. Although MS was previously considered to be a predominantly T cell-mediated autoimmune disease, in the last decade, especially with the introduction of B-cell depleting therapies for other immunological diseases, it became obvious that B cells have a major contribution to MS pathogenesis.Citation87
The era of B-cell depletion therapy started in 1997, when rituximab, a chimeric monoclonal antibody was approved by the European Medical Agency (EMA) and the US Food and Drug Administration (FDA) for the oncologic treatment of B-cell non-Hodgkin’s lymphoma.Citation88 Rituximab was later used in the treatment of various autoimmune diseases, most commonly in the treatment of rheumatoid arthritis and systemic lupus erythematosus.Citation89 Following the pathological basis of therapeutic effects in autoimmune diseases, rituximab was also introduced in MS treatment. In 2008, the results of phase II of randomized double-blinded clinical trial HERMES conducted on pwRRMS were published, showing that rituximab reduces inflammatory lesions on MRI, as well as the proportion of relapses.Citation90 Positive results of rituximab treatment in MS encouraged investigators to evaluate other anti-CD20 antibodies in the treatment of MS and today we have 4 available anti CD20 treatment. The aim of this review was to evaluate the role of ocrelizumab, the second developed monoclonal antibody, in the treatment of relapsing-remitting and primary progressive forms of MS.
Mechanism of action
B cells originate from hematopoietic stem cell precursors in the bone marrow and their development consists of the maturation, selection, and differentiation process that takes place within the bone marrow, as well as in the secondary lymphoid organs.Citation91 During the development process, B cells are expressing different CD markers and for ocrelizumab treatment consideration the most important marker is CD20. This marker is not expressed on stem cell precursors, antibody-secreting plasmablasts, and plasma cells, but it is present on immature, naive, and memory B-cells.Citation92
Initial evidence of B-cell involvement in MS came with the identification of specific IgG fraction in the cerebrospinal fluid analysis (CSF).Citation93 These fractions are known as oligoclonal bands and exhibit the activity of clonally expanded B cells within the intrathecal space. Oligoclonal bands are present in almost 90% of all patients with MS and they can substitute dissemination in time according to the 2017 diagnostic criteria for MS.Citation94,Citation95
Within the CSF of pwMS polyclonal B cell response to measles, rubella, and varicella-zoster virus (MRZ reaction) is found, and it is considered to be a highly specific laboratory marker of MS.Citation96
Another important contribution to the proof of B-cell presence in the CNS was discovered in 2004 when ectopic lymphoid follicle-like structures containing CD20 + B cells as well as CD138+ plasma cells and follicular dendritic cells were found in the leptomeninges of SPMS patients.Citation97 Immunohistochemical analysis of brain specimens obtain from RRMS and PPMS patient revealed signs of pathologic meningeal aggregates of CD20 + B cells and CD3 + T cells that correlated with cortical demyelination.Citation98,Citation99 In PPMS patients meningeal infiltration was associated with a more severe clinical course and younger age of death.Citation99
Selective depletion of CD20 B cells in ocrelizumab-treated patients is achieved through 4 mechanisms: ADCP, ADCC, CDC, and apoptosis. Innate immunity and the T-cell are not affected in ocrelizumab treated patients. Due to the fact that stem cells, pro-B cells, and plasma cells do not express CD20, the capacity of B-cell reconstitution and antibody production is retained.Citation100,Citation101
In phase III studies on people with RRMS, ocrelizumab demonstrated to completely decrease the CD19 + B-cell count (equivalent in an assay measuring CD20+ cells) in blood after 2 weeks of treatment.Citation102
The median time to B-cell repletion after the last infusion of ocrelizumab in the phase II study was 72 weeks.Citation103 Ocrelizumab displays dose-dependent depletion of B cells. Patients with mild renal and hepatic impairment were also included in clinical trials and no change in the pharmacokinetics was observed. Ocrelizumab is cleared primarily via catabolism and degrades into smaller peptides and amino acids and its half-life is 26 days.Citation101
Pooled analysis from RRMS and PPMS studies demonstrated the correlation between the B-cell depletion in blood with higher ocrelizumab exposure and body weight.Citation104 Another study supporting these findings showed that patients with fast repopulation rate of B cells had higher BMI.Citation105
Efficacy of ocrelizumab
Evidence from core clinical trials – RRMS
The safety and efficacy of ocrelizumab in people with RRMS was tested in one phase II,Citation103 and two identical phase III studies OPERA I and II ().Citation102 Results of the phase II study
demonstrated in both dosing regimen of ocrelizumab (600 and 2000 mg) significant reduction in the number of gadolinium-enhancing T1 lesions at weeks 12, 16, 20, and 24 in comparison to placebo and INF beta 1a i.m.Citation103 Similar efficacy on MRI parameters was demonstrated in phase III studies.Citation102 Additionally, 46 and 47% relative reduction in ARR in OPERA I and II, respectively, and 40% lower risk of 12-week (p < .001) and 24-week confirmed disability progression (p = .003) in pooled analysis of both studies was seen.
Evidence from extension studies – RRMS
Long term data from open label ocrelizumab extension in RRMS patients demonstrated that earlier and continuous ocrelizumab treatment up to 5 years provides sustained benefit on clinical and MRI measures of inflammatory disease activity. The beneficial effect was also observed in a smaller percentage of patients with disease progression as well as in a slower rate of brain volume loss.Citation106
Evidence from core clinical trials – PPMS
In 2009 the results of the OLYMPUS trial were published in which rituximab was evaluated in people with PPMS (pwPPMS). Although this trial failed to demonstrate the efficacy of rituximab in pwPPMS, a subgroup analysis demonstrated delayed disability progression in participants who were <51 years of age and had signs of the inflammatory activity of the disease.Citation107
The results provided in a subset of patients from OLYMPUS trial were the rationale for the design of ORATORIO, a phase III randomized, double-blind, placebo-controlled trial, in which ocrelizumab was investigated in pwPPMS ().Citation108 The percentage of patients with 12-week disability progression was significantly lower in ocrelizumab treated pwPPMS compared to participants receiving placebo. Statistically significant results in favor of ocrelizumab were demonstrated in following secondary outcomes: decrease in disability progression at 6 months, 25-foot walk (T25FW) change at 120 weeks, the percentage change in total T2-weighted lesions, the number of new or enlarging T2 lesions and the percentage of brain volume loss.
Evidence from extension studies – PPMS
After completion of the double-blind period in the ORATORIO study, participants were offered to enter an open-label extension phase in which they continued ocrelizumab or were switched from placebo to ocrelizumab.Citation109 All included patients were followed during the period of the at least 6.5 study years out of which 3.5 study years were in the open-label extension.
Out of 732 subjects included in the ORATORIO study, 451 participants were included in the open-label extension. At the last available analysis, disability measures (24-week confirmed disability progression, 9HPT, composite progression, and confirmed time to requiring a wheelchair) and MRI parameters (percentage change from baseline for T2 lesion volume and T1 hypointense lesion volume) were in favor of patients who were treated from the beginning in the ocrelizumab arm.
Evidence from real-world studies
Only a couple of studies investigated the effectiveness of ocrelizumab in a real-world setting ().Citation110,Citation111 In pwRRMS NEDA-3 was achieved in >90% of participants in both studies. Furthermore, in pwPPMS disease progression ranged from 4.7 to 37.5%. However, these data are limited by short follow-up and real-world studies of longer duration are needed. No new safety signals were identified.
Safety of ocrelizumab
More than 80% participants in OPERA 1 and more than 85% of OPERA 2 in both treatment arm reported AE,Citation102 while serious AE were present in 1.3% of ocrelizumab and in 2.9% of the IFN-beta-1a sc. group. In the ORATORIO trial, 95.1% of patients in the ocrelizumab group and 90% in the placebo group reported at least one AE while 20.4% in ocrelizumab and 22.2% in the placebo-treated arm had serious AE.Citation109 The most common AEs in the ocrelizumab treated group in both studies were IRR and infections while side effects of special interest were malignant diseases ().
Infusion associated reactions
In core clinical trials for both RRMS and PPMS, IARs occurred in 34.3 and 39.9% of participants, respectively.Citation102,Citation108 Most of them were mild to moderate with exception of one life-threatening episode of bronchospasm in pwRRMS and two treatment discontinuation in pwPPMS. The most frequent ocrelizumab IRR presentations were pruritus, rash, throat irritation, and flushing. (102, 108) Short infusion period of 2 hours in comparison with 3.5 hours did not increase the risk of IRRs.Citation112
Infections
In OPERA trials the most common infections (≥10% in both trials and treatment groups) were upper respiratory tract infection, nasopharyngitis, and urinary tract infection. There were no reports of opportunistic infections during the trials. Herpesvirus-associated infections were reported in 5.9% of the ocrelizumab and 3.4% of the INF group and were classified as mild or moderate with the exception of one ocrelizumab treated patient with severe genital herpes simplex infection.
In ORATORIO trial the percentage of any reported infection was 71.4% in the ocrelizumab and 69.9% in the placebo-treated group. The most common infections were nasopharyngitis, urinary tract infection, influenza, and upper respiratory tract infection. Upper respiratory tract infections were more common in ocrelizumab than in the placebo arm (10.9% vs. 5.9%). The percentage of serious infections (SI) according to system organ class was without significant difference, 6.2% with ocrelizumab and 5.9% with placebo. Herpesvirus-related infections were detected in 4.7% of ocrelizumab and 3.3% of placebo-treated patients, among which oral herpes was more common with mild to moderate clinical features.
In a recent systematic review of ocrelizumab associated AEs, that included reports of 7000 ocrelizumab treated patients, authors found that 61% of ocrelizumab-treated subjects had at least one AE, with the most common being infection (39%) and IRR (26%).Citation113 The most commonly reported infections were nasopharyngitis, upper respiratory tract infections, urinary tract infections as well as skin reactions. PPMS patients in comparison with RRMS patients had higher prevalence of AE,Citation102,Citation108 but it is important to note that PPMS patients in clinical trials were 8 years older on average in comparison with RRMS.
According to published data, there were in total 10 cases of PML in ocrelizumab treated patients. Out of 10 PML cases, 9 were considered to be carryover due to previous exposure to either natalizumab or fingolimod, and 1 case was observed in 78-year-old patient with lymphopenia grade 2 and no prior DMD exposure.Citation114,Citation115
In the ocrelizumab all-exposure treated population the most common serious infections (SI) were urinary tract infection, pneumonia and cellulitis. More than 95% of SI resolved without treatment discontinuation. There were no reports of new SI or new patterns of SI than those reported previously. As in clinical trials, SI were more prevalent in PPMS patients in comparison with RRMS phenotype.Citation116 Moreover, it was demonstrated that a decreased level of serum immunoglobulins, particularly IgG levels are related to increased risk of SI.Citation117
After 7 years of follow-up a reduction in serum IgG levels at an approximate mean rate of 3–4% per year was observed, but the profile of SIs verified during the hypogammaglobulinemia did not differ from patients with normal levels of IgG.Citation116 Due to the fact that ocrelizumab administration can cause reactivation of latent hepatitis B virus (HBV) infection,Citation118 HBV screening is mandatory before ocrelizumab introduction. Active HBV infection is a contraindication for ocrelizumab treatment while in cases of HB core antibody or surface antigen positivity consultation of a hepatologist is warranted.
Neoplasms
In OPERA trials, four neoplasms (0.5% of patients) occurred in the ocrelizumab group (two cases of invasive ductal breast carcinoma, one case of renal cell carcinoma, and one case of malignant melanoma), and two occurred (0.2%) in the INF group (mantle-cell lymphoma and squamous-cell carcinoma in the chest). In the open-label extension study, during which all participants were treated with ocrelizumab, five additional cases of neoplasm (two cases of breast cancer, two cases of basal-cell skin carcinoma, and one case of malignant melanoma) were reported.Citation102
In core clinical trials there were three deaths, one death in the ocrelizumab group (suicide in the OPERA II trial) and two in the INF group (one suicide in the OPERA I trial, and one death due to mechanical ileus in the OPERA II trial).Citation102
Neoplasms were reported in ORATORIO trial in 11 out of 486 patients (2.3%) in the ocrelizumab group (breast cancer in 4 patients, basal-cell carcinoma in 3, endometrial adenocarcinoma, anaplastic large-cell lymphoma, malignant fibrous histiocytoma, and pancreatic carcinoma) and in 2 of 239 patients (0.8%) in the placebo group (cervical adenocarcinoma in situ and basal-cell carcinoma).
In total five deaths were reported: four (0.8%) in the ocrelizumab arm due to pulmonary embolism, pneumonia, pancreatic carcinoma, and aspiration pneumonia and one (0.4%) in the placebo arm owing to a road-traffic accident.Citation108
In long term follow up that included all exposureocrelizumab treated patients yearly crude incidence of all malignancies (breast cancer and non-melanoma skin cancer included) remained stable over time. There was a higher number of breast cancers in ocrelizumab-treated patients in clinical trials but in long-term follow-up the age-standardized incidence of female breast cancer remained within epidemiological references.Citation119
In data that included clinical trials and open-label extensions of ocrelizumab-treated patients, there was no increase in fatalities and no pattern of fatalities was observed in the ocrelizumab-treated patients.Citation120
Less common side effects
In 2020 the first case of ocrelizumab-induced colitis was described,Citation121 followed by case of severe colitis,Citation122 and ocrelizumab-induced colitis and esophagitis.Citation123 Pathophysiologically, this could be explained with regulatory B-cell depletion that was found to be associated with colitis in animal models and found also in specimens of intestinal tissue in patients with ulcerative colitis.Citation124
Due to the fact that colitis was described with rituximab treatment,Citation124 medical professionals prescribing ocrelizumab need to be vigilant in treated patients presenting with new onset gastrointestinal symptoms.
Our group published the case of acute pancreatitis in a patient without risk factors that occurred four months after second ocrelizumab cycle. Patient had mild clinical presentation and recovered completely.Citation125 In clinical trials five cases of pancreatitis were described and third patients had hepatobiliary risk factors.Citation126
A case of fulminant hepatitis induced by Echovirus 25 during ocrelizumab monotherapy was published as well and resulted in liver failure that was treated with liver transplantation. Several Echovirus cases causing fulminant hepatitis were confirmed in rituximab-treated patients as well.Citation127
Late onset neutropenia is defined as decrease of neutrophils <1.5 × 109 more than 4 weeks after ocrelizumab exposure in a person with previously normal neutrophil count.Citation128
Similar cases were described in rituximab,Citation129 and only a few so far in ocrelizumab-treated patients.Citation130 Neutropenia can occur weeks to months after ocrelizumab treatment and it could be caused by alterations in growth factors that affect B-cell production at the level of bone marrow.Citation130
Therapeutic indication, dosage, administration, and monitoring
Ocrelizumab is indicated in the treatment of adult patients with relapsing or primary progressive forms of MS.Citation131 European indication limits the use of Ocrelizumab in patients with relapsing forms of MS with active disease defined by clinical or imaging features and early PPMS in terms of disease duration and level of disability, and with imaging features characteristic of inflammatory activity.Citation101
The starting ocrelizumab dose is 300 mg in 250 mL 0.9% NaCl, followed by a second infusion after 2 weeks, and thereafter every 6 months of 600 mg in 500 mL 0.9% NaCl, IV administered. Duration of the two 300 mg infusions should be approximately 2.5 hours. In order to avoid IRR, patients are at least 30–60 min prior to administration of ocrelizumab premedicated with 100 mg methylprednisolone (or an equivalent) and an antihistamine. Some centers in addition use paracetamol as well in premedication protocols. In subsequent cycles, two-hour infusion protocol can be applied in case patients did not experience any previous serious IRR. Patients are monitored at the infusion center for at least 60 min following ocrelizumab infusion.Citation101
In our center, before every ocrelizumab cycle, we perform analysis of complete blood count and biochemistry including liver enzymes, lgM, IgG, and IgA levels, and absolute number of CD4 lymphocytes. Ocrelizumab is not administered in the following cases: number of absolute lymphocytes < 800, number of CD4 lymphocytes < 250, liver enzymes > 5× of upper normal level and when the level of any evaluated immunoglobulin is < 50% of the lower normal level.
Ocrelizumab and pregnancy
Rituximab and ocrelizumab are class of IgG1 antibodies and the placental transfer of these immunoglobulins occurs in a linear fashion with minimal transport in the first trimester, and maximal transport during the third trimester. Therefore, minimal fetal exposure is expected during the early stages of pregnancy while an increasing rate can occur during the third trimester.Citation132,Citation133 There are limited data regarding the usage of B cell treatment during pregnancy; however, several publications evaluated the safety and effectiveness of rituximab administration in patients with NMOSD and MS as well as other immunological, rheumatological, and hemato-oncological diagnosis before and during pregnancy. Results of these studies demonstrated no major safety signals.Citation134,Citation135
A small number of studies evaluated ocrelizumab exposure and pregnancy outcomes. A cohort study from Germany evaluated pregnancy outcomes and disease activity in women with NMOSD and MS that were treated with ocrelizumab or rituximab.Citation136 The study cohort included 68 known outcomes of 88 pregnancies from 81 women. Significantly more preterm births occurred in women with exposure during pregnancy and 2 major congenital abnormalities were observed in the same group of treated patients. Other evaluated pregnancy outcomes were similar between groups. Out of the whole cohort, three women had SI during pregnancy, and SI leading to hospitalization occurred in 3 newborns. There were no relapses during pregnancy in women with MS, one relapse occurred in the NMOSD group. Postpartum relapse occurred in 17.2% of RRMS and 8.3% of NMOSD women.Citation136 Most neonates had normal B-cell counts and for those with decreased B cell count recovery was complete at the age of 5 months with no observed increase of SI.
A study presented at ECTRIMS 2019 reported 118 pregnancies in women with MS exposed to ocrelizumab in utero with 54 known pregnancy outcomes and demonstrated the results that are not suggestive of an increased risk of adverse pregnancy or fetal outcomes.Citation137
The concentration of rituximab in breast milk was also shown to be minimal with no signs of developmental delay or SI in the follow-up period.Citation138
Because of the potential fetal B-cell depletion, decrease immunoglobulin levels and the possibility of SI the current label proposes discontinuation of anti-CD20 treatment at least 6 (FDA)Citation131 to 12 months (EMA)Citation101 before planned pregnancy.
Ocrelizumab and COVID-19
Recently published data that included SARS-CoV-2 positive patients treated with ocrelizumab during clinical trials, postmarketing safety database data and real-world data indicate similar rates of hospitalization, invasive ventilation and death in the ocrelizumab-treated and nonocrelizumab-treated patients.Citation139
More severe clinical features of SARS-CoV-2 infection, in ocrelizumab-treated patients as well as in general population, was associated with advanced age, male sex and the presence of comorbidities.Citation140
According to data presented in Hughes et al. dataset, COVID-19 in ocrelizumab-treated subjects was predominantly mild to moderate in severity what is in accordance with the reported general population and MS datasets.Citation139
On the other hand, data presented from the Italian group demonstrated that besides progressive MS course and comorbidities, recent methylprednisolone use as well as therapy with an anti-CD20 agent (ocrelizumab or rituximab) was significantly associated (odds ratio [OR] = 2.37, 95% confidence interval [95% CI] = 1.18–4.74, p = .015) with increased risk of severe COVID-19.Citation82
North American Registry of Patients with MS evaluated the clinical outcome in 1626 patients with SARS-CoV-2 infection. Increased disability and older age were each independently correlated with increased odds of all evaluated clinical severity levels. Among specific MS treatment rituximab and recent treatment with corticosteroids were associated with worse COVID-19 clinical severity.Citation141
Due to COVID-19 pandemic and lockdown measures that were in place in many countries a delay in ocrelizumab infusions may have occurred. However, real-world data demonstrated that delaying ocrelizumab infusions up to three months had no impact on disease activity as measured by relapses with the number of previous ocrelizumab cycles being a significant predictor of peripheral B cells (CD19+) count.Citation142
Vaccination and ocrelizumab treatment
Preventing infections by vaccination is one of the most important parts of a comprehensive medical approach to patients with MS, even more so during COVID-19 pandemic.
In general, patients with MS should receive vaccinations in accordance with the local or national vaccination schedule. Special consideration exists regarding the administration of live and live-attenuated vaccines that are not recommended for MS patients taking a DMT.Citation143
Another specific consideration is related to the type of DMT and its mechanism of action.
Although treatment with ocrelizumab leads to a continuous depletion of CD20+ cells the capacity of B-cell reconstitution, as well as preexisting humoral immunity, should remain intact. In order to assess the influence of ocrelizumab administration on the humoral response on most commonly administered vaccines, VELOCE (Phase IIIb) study was conducted in pwRRMS.Citation144 Results of the study demonstrated attenuation of humoral responses at all time points in ocrelizumab treated patients but with antibody titers that are still expected to be protective. Based on these results, it would be advisable to administer all vaccines at least 6 weeks before ocrelizumab introduction.Citation101,Citation144 Taking into account data from the VELOCE study, a similar response with diminished immunogenicity to COVID-19 vaccine may be anticipated in ocrelizumab treated patients. In a recently published case report authors presented vaccine failure in an ocrelizumab treated patient who developed symptomatic COVID-19 infection 19 days after the last dose of COVID-19 mRNA vaccine.Citation145 First dose of the vaccine was given within 3 weeks from last ocrelizumab infusion and this may have affected antibody development. It is worth mentioning that the patient was treated with casirivimab and imdevimab, monoclonal antibodies that are FDA approved in mild to moderate COVID-19 patients who are at high risk for progressing to severe COVID-19.Citation146
Taken all this into account, it has been suggested that dose interruption will be needed to allow effective vaccination against SARS-CoV-2, without the effect on inflammatory disease control.Citation147
Conclusions
Introduction of monoclonal antibodies in the treatment of MS have revolutionized the MS treatment landscape in the last decade. With the introduction of alemtuzumab into clinical practice, we have witnessed the first immune reconstitution therapeutic approach in MS, with a potential of long lasting remission after only two cycles of therapy. Similarly, with the introduction of ocrelizumab we have witnessed a first DMT having a positive effect on delaying progression in pwPPMS. With the increasingly complex landscape of DMTs approved for MS, people with MS and neurologists are constantly faced with the question which DMT is the most appropriate for the given patient. There are two important fact that one has to bear in mind in this decision process: (i) DMTs should be commenced within a year from the disease onset to reduce the risk of disability accumulation over the long termCitation148 and (ii) initial treatment with higher efficacy DMTs is associated with a lower risk of conversion to SP MS vs initial treatment with lower efficacy DMTs.Citation149 Further clinical and real-world studies are needed to obtain long-term efficacy and safety evidence and comparative effectiveness for these therapies. Furthermore, personalized approach to MS treatment and management is warranted and studies investigating potential biomarkers of treatment response are of utmost importance.
Disclosure of potential conflicts of interests
TG: Participated as a clinical investigator and/or received consultation and/or speaker fees from: Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals, TG Pharmaceuticals.
BB: Participated as a clinical investigator and/or received consultation and/or speaker fees from: Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals.
IA: Participated as a clinical investigator and/or received consultation and/or speaker fees from: Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals, TG Pharmaceuticals.
MKS: received consultation and/or speaker fees from: Sanofi Genzyme, Roche.
MH: Participated as a clinical investigator and/or received consultation and/or speaker fees from: Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals, TG Pharmaceuticals.
Authors’ contributions
Study concept and design: Habek. Acquisition of data: Gabelić, Barun, Adamec, Krbot Skorić, Habek. Analysis and interpretation of data: Gabelić, Barun, Adamec, Krbot Skorić, Habek. Drafting of the manuscript: Gabelić, Barun. Critical revision of the manuscript for important intellectual content: Gabelić, Barun, Adamec, Krbot Skorić, Habek. Administrative, technical, and material support: Gabelić, Barun, Adamec, Krbot Skorić, Habek.
References
- Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, Robertson N, La RN, Uitdehaag B, van der Mei I, et al. Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult Scler. 2020;26:1816–21. doi:10.1177/1352458520970841.
- Dargahi N, Katsara M, Tselios T, Androutsou ME, De Courten M, Matsoukas J. Apostolopoulos V. Multiple sclerosis: immunopathology and treatment update. Brain Sci. 2017;7:78. doi:10.3390/brainsci7070078.
- Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG. Multiple sclerosis. N Engl J Med. 2000;343:938–52. doi:10.1056/NEJM200009283431307.
- Kantarci OH. Phases and phenotypes of multiple sclerosis. Continuum (Minneap Minn). 2019;25:636–54.
- Amato MP, Fonderico M, Portaccio E, Pastò L, Razzolini L, Prestipino E, Bellinvia A, Tudisco L, Fratangelo R, Comi G, et al. Disease-modifying drugs can reduce disability progression in relapsing multiple sclerosis. Brain. 2020;143:3013–24. doi:10.1093/brain/awaa251.
- AlSharoqi IA, Aljumah M, Bohlega S, Boz C, Daif A, El-Koussa S, Inshasi J, Kurtuncu M, Müller T, Retief C, et al. Immune reconstitution therapy or continuous immunosuppression for the management of active relapsing-remitting multiple sclerosis patients? A narrative review. Neurol Ther. 2020;9:55–66. doi:10.1007/s40120-020-00187-3.
- Li Z, Richards S, Surks HK, Jacobs A, Panzara MA. Clinical pharmacology of alemtuzumab, an anti-CD52 immunomodulator, in multiple sclerosis. Clin Exp Immunol. 2018;194:295–314. doi:10.1111/cei.13208.
- Watanabe T, Masuyama J, Sohma Y, Inazawa H, Horie K, Kojima K, Uemura Y, Aoki Y, Kaga S, Minota S, et al. CD52 is a novel costimulatory molecule for induction of CD4+ regulatory T cells. Clin Immunol. 2006;120:247–59. doi:10.1016/j.clim.2006.05.006.
- Freedman MS, Kaplan JM, Markovic-Plese S. Insights into the mechanisms of the therapeutic efficacy of alemtuzumab in multiple sclerosis. J Clin Cell Immunol. 2013;4:1000152. doi:10.4172/2155-9899.1000152.
- Hu Y, Turner MJ, Shields J, Gale MS, Hutto E, Roberts BL, Siders WM, Kaplan JM. Investigation of the mechanism of action of alemtuzumab in a human CD52 transgenic mouse model. Immunology. 2009;128:260–70. doi:10.1111/j.1365-2567.2009.03115.x.
- Bindon CI, Hale G, Waldmann H. Importance of antigen specificity for complement-mediated lysis by monoclonal antibodies. Eur J Immunol. 1988;18:1507–14. doi:10.1002/eji.1830181006.
- Stanglmaier M, Reis S, Hallek M. Rituximab and alemtuzumab induce a nonclassic, caspase-independent apoptotic pathway in B-lymphoid cell lines and in chronic lymphocytic leukemia cells. Ann Hematol. 2004;83:634–45. doi:10.1007/s00277-004-0917-0.
- European Medicines Agency. Lemtrada 12 mg concentrate for solution for infusion: EU summary of product characteristics. 2019. [accessed 25 Feb 2021]. https://www.ema.europa.eu/ .
- Coles AJ, Compston DA, Selmaj KW, Lake SL, Moran S, Margolin DH, Norris K, Tandon PK, CAMMS223 Trial Investigators. Alemtuzumab vs. interferon beta-1a in early multiple sclerosis. N Engl J Med. 2008;359:1786–801.
- Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung HP, Havrdova E, Selmaj KW, Weiner HL, Fisher E, et al. CARE-MS I investigators. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet. 2012;380:1819–28. doi:10.1016/S0140-6736(12)61769-3.
- Coles AJ, Twyman CL, Arnold DL, Cohen JA, Confavreux C, Fox EJ, Hartung HP, Havrdova E, Selmaj KW, Weiner HL, et al. CARE-MS II investigators. Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled phase 3 trial. Lancet. 2012;380:1829–39. doi:10.1016/S0140-6736(12)61768-1.
- Hale G. The CD52 antigen and development of the CAMPATH antibodies. Cytotherapy. 2001;3:137–43. doi:10.1080/146532401753174098.
- Gribben JG, Hallek M. Rediscovering alemtuzumab: current and emerging therapeutic roles. Br J Haematol. 2009;144:818–31. doi:10.1111/j.1365-2141.2008.07557.x.
- European Medicines Agency. Lemtrada assessment report: procedure under article 20 of regulation (EC) No 726/2004 resulting from pharmacovigilance data. 2019. [accessed 25 Feb 2021]. https://www.ema.europa.eu/ .
- Syed YY. Alemtuzumab: a review in relapsing remitting multiple sclerosis. Drugs. 2021;81:157–68. doi:10.1007/s40265-020-01437-2.
- Baker D, Herrod SS, Alvarez-Gonzalez C, Giovannoni G, Schmierer K. Interpreting lymphocyte reconstitution data from the pivotal phase 3 Trials of Alemtuzumab. JAMA Neurol. 2017;74:961–69. doi:10.1001/jamaneurol.2017.0676.
- Thompson SA, Jones JL, Cox AL, Compston DA, Coles AJ. B-cell reconstitution and BAFF after alemtuzumab (Campath-1H) treatment of multiple sclerosis. J Clin Immunol. 2010;30:99–105. doi:10.1007/s10875-009-9327-3.
- Zhang X, Tao Y, Chopra M, Ahn M, Marcus KL, Choudhary N, Zhu H, Markovic-Plese S. Differential reconstitution of T cell subsets following immunodepleting treatment with alemtuzumab (anti-CD52 monoclonal antibody) in patients with relapsing-remitting multiple sclerosis. J Immunol. 2013;191:5867–74. doi:10.4049/jimmunol.1301926.
- Rolla S, De Mercanti SF, Bardina V, Horakova D, Habek M, Adamec I, Cocco E, Annovazzi P, Vladic A, Novelli F, et al. Lack of CD4+ T cell percent decrease in alemtuzumab-treated multiple sclerosis patients with persistent relapses. J Neuroimmunol. 2017;313:89–91. doi:10.1016/j.jneuroim.2017.10.009.
- Cox AL, Thompson SA, Jones JL, Robertson VH, Hale G, Waldmann H, Compston DA, Coles AJ. Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol. 2005;35:3332–42. doi:10.1002/eji.200535075.
- De Mercanti S, Rolla S, Cucci A, Bardina V, Cocco E, Vladic A, Soldo-Butkovic S, Habek M, Adamec I, Horakova D, et al. Alemtuzumab long-term immunologic effect: treg suppressor function increases up to 24 months. Neurol Neuroimmunol Neuroinflamm. 2016;3:e194. doi:10.1212/NXI.0000000000000194.
- Haas J, Würthwein C, Korporal-Kuhnke M, Viehoever A, Jarius S, Ruck T, Pfeuffer S, Meuth SG, Wildemann B. Alemtuzumab in multiple sclerosis: short- and long-term effects of immunodepletion on the peripheral treg compartment. Front Immunol. 2019;10:1204. doi:10.3389/fimmu.2019.01204.
- Gross CC, Ahmetspahic D, Ruck T, Schulte-Mecklenbeck A, Schwarte K, Jörgens S, Scheu S, Windhagen S, Graefe B, Melzer N, et al. Alemtuzumab treatment alters circulating innate immune cells in multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016;3:e289. doi:10.1212/NXI.0000000000000289.
- Bielekova B, Catalfamo M, Reichert-Scrivner S, Packer A, Cerna M, Waldmann TA, McFarland H, Henkart PA, Martin R. Regulatory CD56(bright) natural killer cells mediate immunomodulatory effects of IL-2Ralpha-targeted therapy (daclizumab) in multiple sclerosis. Proc Natl Acad Sci U S A. 2006;103:5941–46. doi:10.1073/pnas.0601335103.
- Rizzo R, Zatelli MC, Rotola A, Cassai E, Degli Uberti E, Di Luca D, Caselli E. Increase in peripheral CD3-CD56brightCD16- Natural killer cells in Hashimoto’s thyroiditis associated with HHV-6 infection. Adv Exp Med Biol. 2016;897:113–20.
- Arroyo González R, Kita M, Crayton H, Havrdova E, Margolin DH, Lake SL, Giovannoni G, CARE-MS I and II Investigators. Alemtuzumab improves quality-of-life outcomes compared with subcutaneous interferon beta-1a in patients with active relapsing-remitting multiple sclerosis. Mult Scler. 2017;23:1367–76. doi:10.1177/1352458516677589.
- An extension protocol for multiple sclerosis patients who participated in genzyme-sponsored studies of alemtuzumab. [ accessed 1 Mar 2021]. https://clinicaltrials.gov/ct2/show/NCT00930553 .
- Ziemssen T, Bass AD, Berkovich R, Comi G, Eichau S, Hobart J, Hunter SF, LaGanke C, Limmroth V, Pelletier D, et al. CARE-MS I, CARE-MS II, CAMMS03409, and TOPAZ investigators. Efficacy and safety of alemtuzumab through 9 years of follow-up in patients with highly active disease: post Hoc analysis of CARE-MS I and II patients in the TOPAZ extension study. CNS Drugs. 2020;34:973–88. doi:10.1007/s40263-020-00749-x.
- Steingo B, Al Malik Y, Bass AD, Berkovich R, Carraro M, Fernández Ó, Ionete C, Massacesi L, Meuth SG, Mitsikostas DD, et al. CAMMS223, CAMMS03409, and TOPAZ Investigators. Long-term efficacy and safety of alemtuzumab in patients with RRMS: 12-year follow-up of CAMMS223. J Neurol. 2020;267:3343–53. doi:10.1007/s00415-020-09983-1.
- Havrdova E, Arnold DL, Cohen JA, Hartung HP, Fox EJ, Giovannoni G, Schippling S, Selmaj KW, Traboulsee A, Compston DAS, et al. CARE-MS I and CAMMS03409 Investigators. Alemtuzumab CARE-MS I 5-year follow-up: durable efficacy in the absence of continuous MS therapy. Neurology. 2017;89:1107–16. doi:10.1212/WNL.0000000000004313.
- Coles AJ, Cohen JA, Fox EJ, Giovannoni G, Hartung HP, Havrdova E, Schippling S, Selmaj KW, Traboulsee A, Compston DAS, et al. CARE-MS II and CAMMS03409 Investigators. Alemtuzumab CARE-MS II 5-year follow-up: efficacy and safety findings. Neurology. 2017;89:1117–26. doi:10.1212/WNL.0000000000004354.
- Bass AD, Arroyo R, Boster AL, Boyko AN, Eichau S, Ionete C, Limmroth V, Navas C, Pelletier D, Pozzilli C, et al. CARE-MS I, CARE-MS II, CAMMS03409, and TOPAZ investigators. Alemtuzumab outcomes by age: post hoc analysis from the randomized CARE-MS studies over 8 years. Mult Scler Relat Disord. 2021;49:102717. doi:10.1016/j.msard.2020.102717.
- Van Wijmeersch B, Singer BA, Boster A, Broadley S, Ó F, Freedman MS, Izquierdo G, Lycke J, Pozzilli C, Sharrack B, et al. Efficacy of alemtuzumab over 6 years in relapsing-remitting multiple sclerosis patients who relapsed between courses 1 and 2: post hoc analysis of the CARE-MS studies. Mult Scler. 2020;26:1719–28. doi:10.1177/1352458519881759.
- Comi G, Alroughani R, Boster AL, Bass AD, Berkovich R, Fernández Ó, Kim HJ, Limmroth V, Lycke J, Macdonell RA, et al. CARE-MS I, CARE-MS II, CAMMS03409, and TOPAZ Investigators. Efficacy of alemtuzumab in relapsing-remitting MS patients who received additional courses after the initial two courses: pooled analysis of the CARE-MS, extension, and TOPAZ studies. Mult Scler. 2020;26:1866–76. doi:10.1177/1352458519888610.
- Sacca F, Russo CV, Frau J, Annovazzi P, Signoriello E, Bonavita S, Grasso R, Clerico M, Cordioli C, Laroni A, et al. A real-world study of alemtuzumab in a cohort of Italian patients. ECTRIMS 2019 Online Library Sep 13, 2019; 278628, p. 1428S.
- di Ioia M, Di SV, Farina D, Di TV, Travaglini D, Pietrolongo E, Sensi SL, Onofrj M, De LG. Alemtuzumab treatment of multiple sclerosis in real-world clinical practice: a report from a single Italian center. Mult Scler Relat Disord. 2020;38:101504. doi:10.1016/j.msard.2019.101504.
- Italian Alemtuzumab Study Group. Prosperini L, Annovazzi P, Boffa L, Buscarinu MC, Gallo A, Matta M, Moiola L, Musu L, Perini P, Avolio C, et al. No evidence of disease activity (NEDA-3) and disability improvement after alemtuzumab treatment for multiple sclerosis: a 36-month real-world study. J Neurol. 2018;265:2851–60. doi:10.1007/s00415-018-9070-x.
- Brecl Jakob G, Barun B, Gomezelj S, Gabelić T, Šega Jazbec S, Adamec I, Horvat Ledinek A, Rot U, Krbot Skorić M, Habek M. Effectiveness and safety of alemtuzumab in the treatment of active relapsing-remitting multiple sclerosis: a multicenter, observational study. Neurol Sci. 2021. doi:10.1007/s10072-021-05145-x.
- Moiola L, Zanetta C, Di Cristinzi M, Rinaldi F, Brambilla L, Frau J, Malucchi S, Annovazzi P, Puorro G, Bianco A. Italian prospective multicenter observational study conducted in daily clinical practice in patients affected by RRMS with highly active disease, naïve to therapies, who start a treatment with alemtuzumab (ALEM-NAIVE). ECTRIMS online library. Oct 11, 2018; 228739:896.
- Rigoni E, Singh-Curry V, Nandoskar A, Malik O, Dorsey R, Bergamaschi R, Muraro P, Nicholas R, Scalfari A Alemtuzumab as induction versus escalation therapy: efficacy and adverse events in the real-world. ECTRIMS online library. ECTRIMS 2019. Sep 13, 2019; 1398.
- Ziemssen T, White R, Kern R, Engelmann U, Haase R, Guikema B, Akgün K, TREAT-MS Study Group. TREAT-MS study of real-world effectiveness of alemtuzumab in RRMS patients in Germany: subgroup analysis by number of prior disease-modifying therapies. ECTRIMS 2019 online library. Sep 12, 2019; 279348, p. 988.
- Boffa G, Lapucci C, Sbragia E, Varaldo R, Raiola AM, Currò D, Roccatagliata L, Capello E, Laroni A, Mikulska M, et al. Aggressive multiple sclerosis: a single-centre, real-world treatment experience with autologous haematopoietic stem cell transplantation and alemtuzumab. Eur J Neurol. 2020;27:2047–55. doi:10.1111/ene.14324.
- MSBase Study Group. Kalincik T, Jwl B, Robertson N, Willis M, Scolding N, Cm R, Wilkins A, Pearson O, Ziemssen T, Hutchinson M, et al. Treatment effectiveness of alemtuzumab compared with natalizumab, fingolimod, and interferon beta in relapsing-remitting multiple sclerosis: a cohort study. Lancet Neurol. 2017;16:271–81. doi:10.1016/S1474-4422(17)30007-8.
- Wang L, Qi CH, Zhong R, Yuan C, Zhong QY. Efficacy of alemtuzumab and natalizumab in the treatment of different stages of multiple sclerosis patients. Medicine (Baltimore). 2018;97:e9908. doi:10.1097/MD.0000000000009908.
- Malucchi S, Capobianco M, Lo RM, Malentacchi M, di Sapio A, Matta M, Sperli F, Bertolotto A. High-risk PML patients switching from natalizumab to alemtuzumab: an observational study. Neurol Ther. 2017;6:145–52. doi:10.1007/s40120-016-0058-0.
- Margoni M, Rinaldi F, Miante S, Franciotta S, Perini P, Gallo P. Alemtuzumab following natalizumab in highly active paediatric-onset multiple sclerosis. Mult Scler J Exp Transl Clin. 2019;5:2055217319875471.
- Frau J, Coghe G, Lorefice L, Fenu G, Musu L, Cocco E. Efficacy and safety of alemtuzumab in a real-life cohort of patients with multiple sclerosis. J Neurol. 2019;266:1405–11. doi:10.1007/s00415-019-09272-6.
- i-MuST study group. Frau J, Saccà F, Signori A, Baroncini D, Fenu G, Annovazzi P, Capobianco M, Signoriello E, Laroni A, La Gioia S, et al. Outcomes after fingolimod to alemtuzumab treatment shift in relapsing-remitting MS patients: a multicentre cohort study. J Neurol. 2019;266:2440–46. doi:10.1007/s00415-019-09424-8.
- Huhn K, Bayas A, Doerck S, Frank B, Gerbershagen K, Hellwig K, Kallmann B, Kleinschnitz C, Kleiter I, Lee DH, et al. Alemtuzumab as rescue therapy in a cohort of 50 relapsing-remitting MS patients with breakthrough disease on fingolimod: a multi-center observational study. J Neurol. 2018;265:1521–27. doi:10.1007/s00415-018-8871-2.
- Alcalá C, Gascón F, Pérez-Miralles F, Domínguez JA, Gil-Perotín S, Casanova B. Treatment with alemtuzumab or rituximab after fingolimod withdrawal in relapsing-remitting multiple sclerosis is effective and safe. J Neurol. 2019;266:726–34. doi:10.1007/s00415-019-09195-2.
- Riepl E, Pfeuffer S, Ruck T, Lohmann H, Wiendl H, Meuth SG, Johnen A. Alemtuzumab improves cognitive processing speed in active multiple sclerosis-A longitudinal observational study. Front Neurol. 2018;8:730.
- Wray D, Jacques F, Miller TA, Nicholas J, Mozzicato S, Fanelli MJ, Korideck H, Kappler M, Daizadeh N, Mitchell C, et al. Treatment sequencing and satisfaction with alemtuzumab in relapsing multiple sclerosis patients: interim results of the real-world PRO-ACT study [abstract no P3.2-097]. Neurology 2019;92(Suppl):15.
- Khatri BO, Morawski J, Chung L, Poole E, Hashemi L, Bury D. Significant and clinically meaningful health-related quality of life improvements with alemtuzumab in RRMS patients in clinical practice: interim results from a prospective, non-interventional, real-world study (PROMiS) [abstract no. P3.2-098 plus poster]. Neurology. 2019;92:15.
- Šega-Jazbec S, Barun B, Horvat Ledinek A, Fabekovac V, Krbot Skorić M, Habek M. Management of infusion related reactions associated with alemtuzumab in patients with multiple sclerosis. Mult Scler Relat Disord. 2017;17:151–53. doi:10.1016/j.msard.2017.07.019.
- Vukusic S, Brassat D, de Seze J, Izquierdo G, Lysandropoulos A, Moll W, Vanopdenbosch L, Arque MJ, Kertous M, Rufi P, et al. Single-arm study to assess comprehensive infusion guidance for the prevention and management of the infusion associated reactions (IARs) in relapsing-remitting multiple sclerosis (RRMS) patients treated with alemtuzumab (EMERALD). Mult Scler Relat Disord. 2019;29:7–14. doi:10.1016/j.msard.2019.01.019.
- Wray S, Havrdova E, Snydman DR, Arnold DL, Cohen JA, Coles AJ, Hartung HP, Selmaj KW, Weiner HL, Daizadeh N, et al. Infection risk with alemtuzumab decreases over time: pooled analysis of 6-year data from the CAMMS223, CARE-MS I, and CARE-MS II studies and the CAMMS03409 extension study. Mult Scler. 2019;25:1605–17. doi:10.1177/1352458518796675.
- Buonomo AR, Zappulo E, Viceconte G, Scotto R, Borgia G, Gentile I. Risk of opportunistic infections in patients treated with alemtuzumab for multiple sclerosis. Expert Opin Drug Saf. 2018;17:709–17. doi:10.1080/14740338.2018.1483330.
- Croteau D, Flowers C, Kulick CG, Brinker A, Kortepeter CM. Acute acalculous cholecystitis: a new safety risk for patients with MS treated with alemtuzumab. Neurology. 2018;90:e1548–e1552. doi:10.1212/WNL.0000000000005422.
- von Kutzleben S, Pryce G, Giovannoni G, Baker D. Depletion of CD52-positive cells inhibits the development of central nervous system autoimmune disease, but deletes an immune-tolerance promoting CD8 T-cell population. Implications for secondary autoimmunity of alemtuzumab in multiple sclerosis. Immunology. 2017;150:444–55. doi:10.1111/imm.12696.
- Jones JL, Thompson SA, Loh P, Davies JL, Tuohy OC, Curry AJ, Azzopardi L, Hill-Cawthorne G, Fahey MT, Compston A, et al. Human autoimmunity after lymphocyte depletion is caused by homeostatic T-cell proliferation. Proc Natl Acad Sci USA. 2013;110:20200–05. doi:10.1073/pnas.1313654110.
- Haghikia A, Dendrou CA, Schneider R, Grüter T, Postert T, Matzke M, Stephanik H, Fugger L, Gold R. Severe B-cell-mediated CNS disease secondary to alemtuzumab therapy. Lancet Neurol. 2017;16:104–06. doi:10.1016/S1474-4422(16)30382-9.
- Barton J, Hardy TA, Riminton S, Reddel SW, Barnett Y, Coles A, Barnett MH. Tumefactive demyelination following treatment for relapsing multiple sclerosis with alemtuzumab. Neurology. 2017;88:1004–06. doi:10.1212/WNL.0000000000003694.
- Wehrum T, Beume LA, Stich O, Mader I, Mäurer M, Czaplinski A, Weiller C, Rauer S. Activation of disease during therapy with alemtuzumab in 3 patients with multiple sclerosis. Neurology. 2018;90:e601–e605. doi:10.1212/WNL.0000000000004950.
- Adamec I, Mayer M, Ćorić M, Ruška B, Habek M. Systemic erythematosus lupus after treatment of multiple sclerosis with alemtuzumab. Mult Scler Relat Disord. 2020;46:102589. doi:10.1016/j.msard.2020.102589.
- Maniscalco GT, Cerillo I, Servillo G, Napolitano M, Guarcello G, Abate V, Improta G, Florio C Early neutropenia with thrombocytopenia following alemtuzumab treatment for multiple sclerosis: case report and review of literature. Clin Neurol Neurosurg. 2018;175:134–36.
- Gounder K, Batt T, Dreyer M. Two case reports of acquired haemophilia A as complications of alemtuzumab treatment for multiple sclerosis. BMJ Neurol Open. 2021;3(1):e000095. doi:10.1136/bmjno-2020-000095.
- Cuker A, Bass AD, Nadj C, Agius MA, Steingo B, Selmaj KW, Thoits T, Guerreiro A, Van Wijmeersch B, Ziemssen T, et al. Immune thrombocytopenia in alemtuzumab-treated MS patients: incidence, detection, and management. Mult Scler. 2020;26:48–56. doi:10.1177/1352458518816612.
- Dayan C, Cuker A, LaGanke C, Fernández O, Hupperts R, Sharrack B, Singer B, Vermersch P, Margolin D, Twyman C. Autoimmunity in patients treated with alemtuzumab for relapsing-remitting multiple sclerosis: 6-year follow-up of the CARE-MS studies. Mult Scler. 2016;22:168.
- Scappaticcio L, Castellana M, Virili C, Bellastella G, Centanni M, Cannavò S, Campennì A, Ruggeri RM, Giovanella L, Trimboli P. Alemtuzumab-induced thyroid events in multiple sclerosis: a systematic review and meta-analysis. J Endocrinol Invest. 2020;43:219–29. doi:10.1007/s40618-019-01105-7.
- Phelps R, Winston JA, Wynn D, Habek M, Hartung HP, Havrdová EK, Markowitz GS, Margolin DH, Rodriguez CE, Baker DP, et al. Incidence, management, and outcomes of autoimmune nephropathies following alemtuzumab treatment in patients with multiple sclerosis. Mult Scler. 2019;25:1273–88. doi:10.1177/1352458519841829.
- European Medicines Agency. Product information Lemtrada 2019. [ accessed 5 Mar 2021]. www.ema.europa.eu/en/documents/product-information/lemtrada-epar-product-information_en.pdf .
- Oh J, Achiron A, Celius EG, Chambers C, Derwenskus J, Devonshire V, Hellwig K, Hutton GJ, McCombe P, Moore M, et al. CAMMS223, CARE-MS I, CARE-MS II, CAMMS03409, and TOPAZ Investigators. Pregnancy outcomes and postpartum relapse rates in women with RRMS treated with alemtuzumab in the phase 2 and 3 clinical development program over 16 years. Mult Scler Relat Disord. 2020;43:102146. doi:10.1016/j.msard.2020.102146.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–73. doi:10.1038/s41586-020-2012-7.
- Giovannoni G, Hawkes C, Lechner-Scott J, Levy M, Waubant E, The GJ. COVID-19 pandemic and the use of MS disease-modifying therapies. Mult Scler Relat Disord. 2020;39:102073. doi:10.1016/j.msard.2020.102073.
- Fernández-Díaz E, Gracia-Gil J, García-García JG, Palao M, Romero-Sánchez CM, Segura T. COVID-19 and multiple sclerosis: a description of two cases on alemtuzumab. Mult Scler Relat Disord. 2020;45:102402. doi:10.1016/j.msard.2020.102402.
- Fiorella C, Lorna G. COVID-19 in a multiple sclerosis (MS) patient treated with alemtuzumab: insight to the immune response after COVID. Mult Scler Relat Disord. 2020;46:102447. doi:10.1016/j.msard.2020.102447.
- Sormani MP, De Rossi N, Schiavetti I, Carmisciano L, Cordioli C, Moiola L, Radaelli M, Immovilli P, Capobianco M, Trojano M, et al. Disease-modifying therapies and coronavirus disease 2019 severity in multiple sclerosis. Ann Neurol. 2021;89:780–89. doi:10.1002/ana.26028.
- Sharifian-Dorche M, Sahraian MA, Fadda G, Osherov M, Sharifian-Dorche A, Karaminia M, Saveriano AW, La Piana R, Antel JP, Giacomini PS. COVID-19 and disease-modifying therapies in patients with demyelinating diseases of the central nervous system: a systematic review. Mult Scler Relat Disord. 2021;50:102800. doi:10.1016/j.msard.2021.102800.
- Reyes S, Ramsay M, Ladhani S, Amirthalingam G, Singh N, Cores C, Mathews J, Lambourne J, Marta M, Turner B, et al. Protecting people with multiple sclerosis through vaccination. Pract Neurol. 2020;20:435–45. doi:10.1136/practneurol-2020-002527.
- McCarthy CL, Tuohy O, Compston DAS, Kumararatne DS, Coles AJ, Jones JL. Immune competence after alemtuzumab treatment of multiple sclerosis. Neurology. 2013;81:872–76. doi:10.1212/WNL.0b013e3182a35215.
- [ accessed 22 Apr 2021]. https://practicalneurology.com/articles/2021-jan/ms-minute-the-covid-19-vaccine-vaccine-readiness-in-ms/pdf .
- Sabatino JJ Jr, Pröbstel AK, Zamvil SS. B cells in autoimmune and neurodegenerative central nervous system diseases. Nat Rev Neurosci. 2019;20:728–45.
- Looney RJ. B cells as a therapeutic target in autoimmune diseases other than rheumatoid arthritis. Rheumatology (Oxford). 2005;44(Suppl 2):ii13–ii17. doi:10.1093/rheumatology/keh618.
- Browning JL. B cells move to centre stage: novel opportunities for autoimmune disease treatment. Nat Rev Drug Discov. 2006;5:564–76. doi:10.1038/nrd2085.
- Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, Bar-Or A, Panzara M, Sarkar N, Agarwal S, et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med. 2008;358:676–88. doi:10.1056/NEJMoa0706383.
- Seifert M, Küppers R. Human memory B cells. Leukemia. 2016 Dec;30(12):2283–92. doi:10.1038/leu.2016.226.
- Pavlasova G, Mraz M. The regulation and function of CD20: an “enigma” of B-cell biology and targeted therapy. Haematologica. 2020;105:1494–506. doi:10.3324/haematol.2019.243543.
- Yahr MD, Goldensohn SS, Kabat EA. Further studies on the gamma globulin content of cerebrospinal fluid in multiple sclerosis and other neurological diseases. Ann N Y Acad Sci. 1954;58:613–24. doi:10.1111/j.1749-6632.1954.tb54099.x.
- Dobson R, Ramagopalan S, Davis A, Giovannoni G. Cerebrospinal fluid oligoclonal bands in multiple sclerosis and clinically isolated syndromes: a meta-analysis of prevalence, prognosis and effect of latitude. J Neurol Neurosurg Psychiatry. 2013;84:909–14. doi:10.1136/jnnp-2012-304695.
- Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, Fazekas F, Filippi M, Freedman MS, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17:162–73. doi:10.1016/S1474-4422(17)30470-2.
- Jarius S, Eichhorn P, Franciotta D, Petereit HF, Akman-Demir G, Wick M, The WB. MRZ reaction as a highly specific marker of multiple sclerosis: re-evaluation and structured review of the literature. J Neurol. 2017;264:453–66. doi:10.1007/s00415-016-8360-4.
- Serafini B, Rosicarelli B, Magliozzi R, Stigliano E, Aloisi F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 2004;14:164–74. doi:10.1111/j.1750-3639.2004.tb00049.x.
- Lucchinetti CF, Popescu BF, Bunyan RF, Moll NM, Roemer SF, Lassmann H, Brück W, Parisi JE, Scheithauer BW, Giannini C, et al. Inflammatory cortical demyelination in early multiple sclerosis. N Engl J Med. 2011;365:2188–97. doi:10.1056/NEJMoa1100648.
- Choi SR, Howell OW, Carassiti D, Magliozzi R, Gveric D, Muraro PA, Nicholas R, Roncaroli F, Reynolds R. Meningeal inflammation plays a role in the pathology of primary progressive multiple sclerosis. Brain. 2012;135(Pt 10):2925–37. doi:10.1093/brain/aws189.
- Laurent S, Michel B, Wu H, Eggers E, Demuth S, Strauli N, Wilson MR, Sirota M, Herman A, von Buedingen HC. Effect of ocrelizumab on B and T cell immune repertoires in patients with relapsing multiple sclerosis [abstract no P693]. Mult Scler J 2017;23:337.
- [ accessed 27 Feb 2021] https://www.ema.europa.eu/en/documents/product-information/ocrevus-epar-product-information_en.pdf.
- Hauser SL, Bar-Or A, Comi G, Giovannoni G, Hartung HP, Hemmer B, Lublin F, Montalban X, Rammohan KW, Selmaj K, et al. Ocrelizumab versus Interferon Beta-1a in relapsing multiple sclerosis. N Engl J Med. 2017;376:221–34. doi:10.1056/NEJMoa1601277.
- Kappos L, Li D, Calabresi PA, O’Connor P, Bar-Or A, Barkhof F, Yin M, Leppert D, Glanzman R, Tinbergen J, et al. Ocrelizumab in relapsing-remitting multiple sclerosis: a phase 2, randomised, placebo-controlled, multicentre trial. Lancet. 2011;378:1779–87. doi:10.1016/S0140-6736(11)61649-8.
- Gibiansky E, Petry C, Mercier F, Günther A, Herman A, Kappos L, Hauser S, Yamamoto Y, Wang Q, Model F, et al. Ocrelizumab in relapsing and primary progressive multiple sclerosis: pharmacokinetic and pharmacodynamic analyses of OPERA I, OPERA II and ORATORIO. Br J Clin Pharmacol. 2020. doi:10.1111/bcp.14658.
- Signoriello E, Bonavita S, Di Pietro A, Abbadessa G, Rossi F, Miele G, Casertano S, Lus G. BMI influences CD20 kinetics in multiple sclerosis patients treated with ocrelizumab. Mult Scler Relat Disord. 2020;43:102186. doi:10.1016/j.msard.2020.102186.
- Hauser SL, Kappos L, Arnold DL, Bar-Or A, Brochet B, Naismith RT, Traboulsee A, Wolinsky JS, Belachew S, Koendgen H, et al. Five years of ocrelizumab in relapsing multiple sclerosis: OPERA studies open-label extension. Neurology. 2020;95:e1854–e1867. doi:10.1212/WNL.0000000000010376.
- Hawker K, O’Connor P, Freedman MS, Calabresi PA, Antel J, Simon J, Hauser S, Waubant E, Vollmer T, Panitch H, et al. Rituximab in patients with primary progressive multiple sclerosis: results of a randomized double-blind placebo-controlled multicenter trial. Ann Neurol. 2009;66:460–71. doi:10.1002/ana.21867.
- Montalban X, Hauser SL, Kappos L, Arnold DL, Bar-Or A, Comi G, de Seze J, Giovannoni G, Hartung HP, Hemmer B, et al. Ocrelizumab versus placebo in primary progressive multiple sclerosis. N Engl J Med. 2017;376:209–20. doi:10.1056/NEJMoa1606468.
- Wolinsky JS, Arnold DL, Brochet B, Hartung HP, Montalban X, Naismith RT, Manfrini M, Overell J, Koendgen H, Sauter A, et al. Long-term follow-up from the ORATORIO trial of ocrelizumab for primary progressive multiple sclerosis: a post-hoc analysis from the ongoing open-label extension of the randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2020;19:998–1009. doi:10.1016/S1474-4422(20)30342-2.
- Sempere AP, Berenguer-Ruiz L, Borrego-Soriano I, Burgos-San Jose A, Concepcion-Aramendia L, Volar L, Aragones M, Palazón-Bru A. Ocrelizumab in multiple sclerosis: a real-world study from Spain. Front Neurol. 2021;11:592304. doi:10.3389/fneur.2020.592304.
- Fernandez-Diaz E, Perez-Vicente JA, Villaverde-Gonzalez R, Berenguer-Ruiz L, Candeliere Merlicco A, Martinez-Navarro ML, Gracia Gil J, Romero-Sanchez CM, Alfaro-Saez A, Diaz I, et al. Real-world experience of ocrelizumab in multiple sclerosis in a Spanish population. Ann Clin Transl Neurol. 2021;8:385–94. doi:10.1002/acn3.51282.
- Hartung HP. ENSEMBLE Steering Committee members and study investigators. Ocrelizumab shorter infusion: primary results from the ENSEMBLE PLUS substudy in patients with MS. Neurol Neuroimmunol Neuroinflamm. 2020;7:e807. doi:10.1212/NXI.0000000000000807.
- Ng HS, Rosenbult CL, Tremlett H. Safety profile of ocrelizumab for the treatment of multiple sclerosis: a systematic review. Expert Opin Drug Saf. 2020;19:1069–94. doi:10.1080/14740338.2020.1807002.
- F. Hoffmann La-Roche Ltd. Ocrelizumab and PML. 2020. [ accessed 15 Apr 2021]. https://www.ocrelizumabinfo.com/content/dam/gene/ocrelizumabinfo/pdfs/progressive-multifocal-leukoencephalopathy.pdf.
- Patel A, Sul J, Gordon ML, Steinklein J, Sanguinetti S, Pramanik B, Purohit D, Haroutunian V, Williamson A, Koralnik I, et al. Progressive multifocal leukoencephalopathy in a patient with progressive multiple sclerosis treated with ocrelizumab monotherapy. JAMA Neurol. 2021;78:736–740. doi: 10.1001/jamaneurol.2021.0627.
- F. Hoffmann La-Roche Ltd.Ocrelizumab and infections.2020. [ accessed 15 Apr 2021]. https://www.ocrelizumabinfo.com/content/dam/gene/ocrelizumabinfo/pdfs/infections.pdf .
- Derfuss T, Weber MS, Hughes R, Wang Q, Sauter A, Koendgen H, Hauser SL, Bar-Or A, Hartung HP Serum immunoglobulin levels and risk of serious infections in the pivotal phase III trials of ocrelizumab in multiple sclerosis and their open-label extensions. ECTRIMS Online Library. Sep 11, 2019; 279399; 65.
- Ciardi MR, Iannetta M, Zingaropoli MA, Salpini R, Aragri M, Annecca R, Pontecorvo S, Altieri M, Russo G, Svicher V, et al. Reactivation of hepatitis B virus with immune-escape mutations after ocrelizumab treatment for multiple sclerosis. Open Forum Infect Dis. 2018;6:ofy356. doi:10.1093/ofid/ofy356.
- F. Hoffmann La-Roche Ltd. Ocrelizumab and malignancies. 2020. https://www.ocrelizumabinfo.com/content/dam/gene/ocrelizumabinfo/pdfs/malignancies.pdf .
- F. Hoffmann La-Roche Ltd. Ocrelizumab and fatalities. 2020. [ accessed 15 Apr 2021]. https://www.ocrelizumabinfo.com/content/dam/gene/ocrelizumabinfo/pdfs/fatalities.pdf;
- Sunjaya DB, Taborda C, Obeng R, Dhere T. First case of refractory colitis caused by ocrelizumab. Inflamm Bowel Dis. 2020;26:e49. doi:10.1093/ibd/izaa057.
- Lee HH, Sritharan N, Bermingham D, Strey G. Ocrelizumab-induced severe colitis. Case Rep Gastrointest Med. 2020;2020:8858378.
- Barnes A, Hofman D, Hall LA, Klebe S, Mountifield R. Ocrelizumab-induced inflammatory bowel disease-like illness characterized by esophagitis and colitis. Ann Gastroenterol. 2021;35:1–2.
- Eckmann JD, Chedid V, Quinn KP, Bonthu N, Nehra V, Raffals LE. De novo colitis associated with rituximab in 21 patients at a tertiary center. Clin Gastroenterol Hepatol. 2020;18:252–53. doi:10.1016/j.cgh.2019.03.027.
- Adamec I, Reiner Ž, Pećin I, Šućur N, Godan Hauptman A, Barun B, Gabelić T, Habek M. Acute pancreatitis after ocrelizumab treatment for relapsing remitting multiple sclerosis. Mult Scler Relat Disord. 2020;45:102381. doi:10.1016/j.msard.2020.102381.
- [ accessed 15 Apr 2021]. https://www.ema.europa.eu/en/documents/assessment-report/ocrevus-epar-public-assessment-report_en.pdf .
- Nicolini LA, Canepa P, Caligiuri P, Mikulska M, Novi G, Viscoli C, Uccelli A. Fulminant hepatitis associated with Echovirus 25 during treatment with ocrelizumab for multiple sclerosis. JAMA Neurol. 2019;76:866–67. doi:10.1001/jamaneurol.2019.0522.
- Zanetta C, Robotti M, Nozzolillo A, Sangalli F, Liberatore G, Nobile-Orazio E, Filippi M, Moiola L Late onset absolute neutropenia associated with ocrelizumab treatment in multiple sclerosis: a case report and review of the literature. J Neurol Sci. 2020;409:116603.
- Wolach O, Bairey O, Lahav M. Late-onset neutropenia after rituximab treatment: case series and comprehensive review of the literature. Medicine (Baltimore). 2010;89:308–18. doi:10.1097/MD.0b013e3181f2caef.
- Baird-Gunning J, Yun J, Stevenson W, Ng K. Severe delayed-onset neutropenia induced by ocrelizumab. Neurohospitalist. 2021;11:59–61. doi:10.1177/1941874420936438.
- [ accessed 15 Apr 2021]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761053lbl.pdf .
- Kane SV, Acquah LA. Placental transport of immunoglobulins: a clinical review for gastroenterologists who prescribe therapeutic monoclonal antibodies to women during conception and pregnancy. Am J Gastroenterol. 2009;104:228–33. doi:10.1038/ajg.2008.71.
- DeSesso JM, Williams AL, Ahuja A, Bowman CJ, Hurtt ME. The placenta, transfer of immunoglobulins, and safety assessment of biopharmaceuticals in pregnancy. Crit Rev Toxicol. 2012;42:185–210. doi:10.3109/10408444.2011.653487.
- Das G, Damotte V, Gelfand JM, Bevan C, Cree BAC, Do L, Green AJ, Hauser SL, Bove R. Rituximab before and during pregnancy. A systematic review, and a case series in MS and NMOSD. Neurol Neuroimmunol Neuroinflamm. 2018;5:e453. doi:10.1212/NXI.0000000000000453.
- Smith JB, Hellwig K, Katharina Fink DJ, Lyell FP, Langer-Gould A. Rituximab, MS, and pregnancy. Neurol Neuroimmunol Neuroinflamm. 2020;7:e734. doi:10.1212/NXI.0000000000000734.
- Kümpfel T, Thiel S, Meinl I, Ciplea AI, Bayas A, Hoffmann F, Hofstadt-van OU, Hoshi M, Kluge J, Ringelstein M, et al. Anti-CD20 therapies and pregnancy in neuroimmunologic disorders: a cohort study from Germany. Neurol Neuroimmunol Neuroinflamm. 2020;8:e913. doi:10.1212/NXI.0000000000000913.
- Oreja-Guevara C, Wray S, Buffels R, Zecevic D, Vukusic S Pregnancy outcomes in patients treated with ocrelizumab. ECTRIMS Online Library. Sep 12, 2019; 279140; 780.
- LaHue SC, Anderson A, Krysko KM, Rutatangwa A, Dorsey MJ, Hale T, Mahadevan U, Rogers EE, Rosenstein MG, Bove R. Transfer of monoclonal antibodies into breastmilk in neurologic and non-neurologic diseases. Neurol Neuroimmunol Neuroinflamm. 2020;7:e769. doi:10.1212/NXI.0000000000000769.
- Hughes R, Whitley L, Fitovski K, Schneble HM, Muros E, Sauter A, Craveiro L, Dillon P, Bonati U, Jessop N, et al. COVID-19 in ocrelizumab-treated people with multiple sclerosis. Mult Scler Relat Disord. 2020;49:102725. doi:10.1016/j.msard.2020.102725.
- Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–36. doi:10.1038/s41586-020-2521-4.
- Salter A, Fox RJ, Newsome SD, Halper J, Li DKB, Kanellis P, Costello K, Bebo B, Rammohan K, Cutter GR, et al. Outcomes and risk factors associated with SARS-CoV-2 infection in a North American registry of patients with multiple sclerosis. JAMA Neurol. 2021;78:699–708. doi:10.1001/jamaneurol.2021.0688.
- Barun B, Gabelić T, Adamec I, Babić A, Lalić H, Batinić D, Krbot Skorić M, Habek M. Influence of delaying ocrelizumab dosing in multiple sclerosis due to COVID-19 pandemics on clinical and laboratory effectiveness. Mult Scler Relat Disord. 2020;48:102704. doi:10.1016/j.msard.2020.102704.
- Otero-Romero S, Ascherio A, Lebrun-Frénay C. Vaccinations in multiple sclerosis patients receiving disease-modifying drugs. Curr Opin Neurol. 2021;34:322–28. doi:10.1097/WCO.0000000000000929.
- Bar-Or A, Calkwood JC, Chognot C, Evershed J, Fox EJ, Herman A, Manfrini M, McNamara J, Robertson DS, Stokmaier D, et al. Effect of ocrelizumab on vaccine responses in patients with multiple sclerosis: the VELOCE study. Neurology. 2020;95:e1999–e2008. doi:10.1212/WNL.0000000000010380.
- Chilimuri S, Mantri N, Gongati S, Zahid M, Sun H. COVID-19 vaccine failure in a patient with multiple sclerosis on ocrelizumab. Vaccines (Basel). 2021;9:219. doi:10.3390/vaccines9030219.
- [ accessed 15 Apr 2021]. https://www.fda.gov/media/143892/download .
- Baker D, Roberts CAK, Pryce G, Kang AS, Marta M, Reyes S, Schmierer K, Giovannoni G, Amor S. COVID-19 vaccine-readiness for anti-CD20-depleting therapy in autoimmune diseases. Clin Exp Immunol. 2020;202:149–61. doi:10.1111/cei.13495.
- Iaffaldano P, Lucisano G, Butzkueven H, Hillert J, Hyde R, Koch-Henriksen N, Magyari M, Pellegrini F, Spelman T, Sørensen PS, et al. Early treatment delays long-term disability accrual in RRMS: results from the BMSD network. Mult Scler. 2021;135245852110101. doi:10.1177/13524585211010128.
- Brown JWL, Coles A, Horakova D, Havrdova E, Izquierdo G, Prat A, Girard M, Duquette P, Trojano M, Lugaresi A, et al. Association of initial disease-modifying therapy with later conversion to secondary progressive multiple sclerosis. JAMA. 2019;321:175–87. doi:10.1001/jama.2018.20588.
