?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
Measles is highly infectious that leads to a high disease burden among the vulnerable population, especially in developing countries, despite the availability of highly effective measles vaccine. Immune amnesia, the resetting of the immune systems of infected patients, has been observed in developed countries. This paper is the first to use various African countries to evaluate the extent of immune amnesia.
Methods
We used two panel datasets from 46 African countries between 1990 and 2018 among children, one is the disease prevalence from Global Burden of Disease, and another is on the measles vaccination coverage from WHO/UNICEF Joint Reporting Form. We used panel regression to estimate the effect of measles prevalence or measles vaccination coverage on other disease prevalence (diarrhea, lower respiratory infection, malaria, meningitis, and tuberculosis).
Results
We found the strong evidence that the increase in the measles prevalence led to an increase in other disease prevalence and mortality. We also found that the increase in the measles vaccination coverage decreased the prevalence of and the mortality due to other diseases.
Discussion and Conclusion
Measles vaccination can have a large impact on children’s health because not only does it reduce the prevalence of measles cases and deaths but also could it potentially reduce the prevalence of and deaths due to other diseases.
KEYWORDS:
Introduction
Measles is a highly infectious disease that kills many people across the globe every year. Despite the availability of measles vaccines, in 2019 alone, the annual number of estimated measles deaths was 207,500 worldwide, 147,900 (over 70%) of which were in African countries.Citation1Approximately 134,200 children are estimated to die due to measles globally in 2015,Citation2 leaving measles a major public health problem.
Measles vaccines are safe, effective, and affordable, as MMR vaccines are 99% effective at preventing measles after the second dose.Citation3 Prior to measles vaccination, African continent had over 1 million cases of measles annually. Measles vaccination program was first introduced in African continents in the mid-1960s and the routine measles control program was established in Africa in the next ten to twenty years from the first introduction. Thanks to the wide distribution of the measles vaccines, the measles cases have been drastic.Citation4,Citation5 Due to measles vaccines, the measles mortality was estimated to reduce by 62% between 2000 and 2019, and Africa observed 57% reduction in the same period of time.Citation1 The coverage of the first dose of measles-containing vaccine (MCV1) in Africa was 69% in 2019. Although this is a considerable improvement from 53% in 2000,Citation1 the coverage is not sufficient for the prevention of endemic transmission of the measles virus, which requires at least 93–95% of population immunity.Citation3
Measles vaccines are not only effective in preventing measles itself but also can they be in preventing other infectious diseases.Citation6–8 Extant studies show that, the immune memory cells will be lost after a measles infection, resetting previously acquired immunity to other pathogens which results in the increased susceptibility to other infectious diseases. This is called “immune amnesia.” Although the mechanism of immune amnesia is not fully understood, Researchers found that 2 to 3 years are necessary to restore protective immune memory.Citation6 Furthermore, it might take up to five years for children to develop immune systems again without measles virus immunesuppression.Citation6 This means that children who contracted with measles virus must be re-vaccinated or re-exposed to all previously infected pathogens to obtain immunity from other diseases again.Citation6,Citation9 In this sense, the long-term impacts of measles infections devastate the continuous efforts of vaccinations of all infectious diseases.
The immune amnesia has been dominantly studied with simulation models and observed in industrial nations such as US, UK, Switzerland, and Denmark.Citation6,Citation10,Citation11 However, studies that examined the impacts of measles vaccines on other infectious diseases are scarce in developing countries, including Africa. A WHO-commissioned review of the effects of the measles vaccine in developing countries such as Guinea-Bissau, Bangladesh, Haiti, Malawi, and Senegal found that the vaccine was associated with a reduction in all-cause child mortality.Citation12 However, the report concluded that their confidence in the effect of the measles vaccine on all-cause mortality is still limited. A study from Democratic Republic of the Congo (DRC)Citation13 looked at the association between past measles infection and the current fever prevalence to find that the fever prevalence was higher among children who were previously contracted with measles. Another study found that measles may have long-term negative impact on vaccine-induced immunity to tetanus in the same country (DRC).Citation14 A study conducted in Samoa also identified the negative effect of the measles induced amnesia on COVID-19 pandemic.Citation15
This paper is the first to conduct a cross-country analysis of the evidence of immune amnesia in African countries. In particular, using the data from 46 African countries, this paper evaluates 1) the extent to which the measles infections lead to the increase of other disease infections and 2) the extent to which the measles vaccination helps reduce the infection of other diseases among children in Africa. We focused on the effect of measles infection and vaccination on five critical infectious diseases in Africa.
Methods
Data
This study uses two sets of data. One is the data on disease prevalence from Global Burden of Disease (GBD) data. The estimates of disease prevalence are based on the simulation model. We focus on the effect of measles on five other diseases: diarrhea, lower respiratory infection (LRI), malaria, meningitis, and tuberculosis (TB). These are main diseases that substantially attribute to the overall prevalence of deaths in African countries. To observe the effect of immune amnesia, we use the same criteria employed by the previous study.Citation6 There are three criteria: 1) the disease generally presents as an acute infection rather than a chronic infection; 2) the disease is present at a standard adequate frequency such that acquired immunity would be expectedly developed within the population; 3) the disease is not the result of an infection due to food poisoning or an animal biting. The previous study also used the fourth criteria: the disease is not a vaccine-preventable cause of death because it could distort results toward an association between mortality and measles if we include one. However, we omit these criteria because our purpose of the study is not to evaluate the accurate association between mortality and measles. The sample is children from 46 sub-Saharan African countries, with ages 1–4 years old and with 5–9 years old, separately. We used the annual data from 1990 to 2019.
Another dataset is the data on the measles vaccination rate from WHO/UNICEF Joint Reporting Form. The data is available annually for 46 sub-Saharan African countries from 1990 to 2018. We focus on the uptake of the first dose of measles vaccine.
Independent variables
To evaluate the effect of the measles prevalence on other diseases prevalence at year t in a country i, the main independent variable is the measles prevalence, which is defined as the average number of measles cases out of 100,000 children between year t and year t-1 in a country i.
To evaluate the effect of the measles vaccination rate on other diseases’ prevalence at year t in a country i, the main independent variable is the measles vaccination rate, which is defined as the average vaccination rate of 1st dose of measles between year t and year t-1 in a country i.
Outcome variables
One set of the primary outcome variable is other disease prevalence. It is defined as the disease prevalence of the following diseases, separately: diarrhea, LRI, malaria, meningitis, and TB. The unit of the variables is the number of disease cases out of 100,000 children in a year.
Another outcome variable is the number of deaths due to other diseases. It is defined as the number of deaths due to other diseases (diarrhea, LRI, malaria, meningitis, and TB) out of 100,000 children in a year.
Estimation Strategy
To address how much the measles infections lead to the increase of other disease infection, we used the following estimation strategy:
where is prevalence or deaths due to other diseases (diarrhea, LRI, malaria, meningitis, and TB) in a country i in year t.
is the measles prevalence as defined above. We included the country and year fixed effects in this panel regression to account for any unobserved cofounding factors which vary by country and over time.
To address how much the measles vaccination coverage helps reduce other disease infection, we used the following estimation strategy:
where is the measles vaccination rate as defined above.
Results
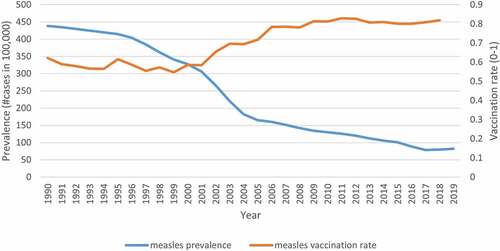
presents the trend of measles prevalence and measles vaccination coverage over time, across 46 African countries, among children aged 1–4 years old. The measles prevalence decreased from 436.7 cases out of 100,000 children to 81.2 cases in 2019. The vaccination coverage increased from 0.58 in 1991 to 0.81 in 2018.
presents the effect of measles prevalence on the prevalence of other diseases. When the measles prevalence increased by one case out of 100,000 children aged 1–4 years, then the prevalence of other diseases increased by the following per 100,000 children: 1.50 (diarrhea), 0.39 (LRI), 20.26 (malaria), 0.33 (meningitis), and 20.29 (TB). Similarly, if the measles prevalence increased by one case out of 100,000 children aged 5–9 years, then the prevalence of other diseases would increase by the following per 100,000 children: 1.24 (diarrhea), 1.35 (LRI), 159.71 (malaria), 3.31 (meningitis), and 159.59 (TB).
Table 1. Effect of measles prevalence on the prevalence of other diseases
presents the effect of measles vaccination coverage on the prevalence of diseases. When the measles coverage increased from 0 (0%) to 1 (100%) among children aged 1–4 years, then the prevalence of diseases decreased by the following per 100,000 children: 611.41 (measles), 924.34 (diarrhea), 277.20 (LRI), 15,078.55 (malaria), 266.74 (meningitis), and 14,311.67 (TB). Similarly, if the measles coverage increased from 0 (0%) to 1 (100%) among children aged 5–9 years, then the prevalence of diseases would decrease by the following per 100,000 children: 79.87 (measles), 118.75 (diarrhea), 127.59 (LRI), 15,493.77 (malaria), 353.71 (meningitis), and 14,573.61 (TB).
Table 2. Effect of measles vaccination on the prevalence of other diseases
presents the effect of measles prevalence on the deaths due to diseases. When the measles prevalence increased by 1 cases out of 100,000 children aged 1–4 years, then the deaths due to diseases increased by the following per 100,000 children: 0.62 (measles), 0.57 (diarrhea), 0.36 (LRI), 0.38 (malaria), 0.10 (meningitis), and 0.08 (TB). Similarly, if the measles prevalence increased by 1 cases out of 100,000 children aged 5–9 years, then the deaths due to diseases would increase by the following per 100,000 children: 0.55 (measles), 0.15 (diarrhea), 0.07 (LRI), 0.10 (malaria), 0.07 (meningitis), and 0.06 (TB).
Table 3. Effect of measles prevalence on deaths due to other diseases
presents the effect of measles vaccination coverage on the deaths due to diseases. When the measles coverage increased from 0 (0%) to 1 (100%) among children aged 1–4 years, then the deaths due to diseases decreased by the following per 100,000 children: 434.94 (measles), 416.70 (diarrhea), 262.50 (LRI), 230.72 (malaria), 70.87 (meningitis), and 59.39 (TB). Similarly, if the measles coverage increased from 0 (0%) to 1 (100%) among children aged 5–9 years, then the deaths due to diseases would decrease by the following per 100,000 children: 50.79 (measles), 14.09 (diarrhea), 7.32 (LRI), 8.19 (malaria), 6.63 (meningitis), and 5.44 (TB).
Table 4. Effect of measles vaccination on deaths due to other diseases
Discussion
This paper evaluates the effect of measles prevalence on other diseases, as well as the effect of measles vaccination coverage on the prevalence of other diseases, among children in 46 African countries between 1990 and 2019.
First, we found that the decline in the measles prevalence was significantly associated with the reduction in other disease prevalence, as well as in the deaths due to these diseases. When the baseline prevalence for a particular disease was high, then the effect size of the measles prevalence on other disease prevalence was also large. For example, when the measles prevalence increased by 1 case out of 100,000 among children aged 1–4, the number of malaria cases increased by 20.26. The effect size is large as compared to other diseases such as LRI (0.39). This is because the malaria prevalence at the baseline in 1990 was also high, 24,567 cases per 100,000, while the prevalence of LRI in 1990 was much lower, 382.61. If we convert the effect size in terms of the percentage to the baseline prevalence, the biggest effect size was 0.10% for LRI and Meningitis, followed by 0.09% for TB, and 0.08% for malaria. These results mean that if the measles prevalence increased by 1 case out of 100,000 among children, the disease cases would increase by 0.10% for LRI and Meningitis, 0.09% for TB, and 0.08% for malaria. The smallest effect size was 0.04% for diarrhea. Overall, these effect sizes in terms of the percentage to the baseline were similar, regardless of the type of disease. Similarly, if we also convert the effect size on the death rate to the percentage to the baseline, here is the percentage increase of the death due to other diseases when the measles prevalence increases by one case out of 100,000: 0.20% (measles), 0.14% (diarrhea, LRI, TB), 0.13% (meningitis), and 0.12% (malaria). The effect should depend on how measles prevalence increases other diseases’ prevalence, as well as on the fatality rate of each disease.
Second, the higher measles vaccination coverage was significantly associated with the reduction in the other diseases prevalence and deaths. The effect size on the disease prevalence when the measles vaccination coverage increased from 0% to 100% in terms of percentage to the baseline was as follows: 80.71% (meningitis), 71.33% (LRI), 65.30% (TB), 61.38% (malaria), and 24.22% (diarrhea). These results mean that when the measles vaccination coverage increased from 0% to 100%, the disease prevalence would increase by the aforementioned percentage of each disease. Similarly, the effect size on the disease mortality when the measles vaccination coverage increased from 0% to 100% in terms of percentage to the baseline was as follows: 142.74% (measles), 105.54% (diarrhea), 100.32% (meningitis), 99.03% (LRI), 96.32% (TB), and 70.56% (malaria).
These results indicate that the increase in the measles vaccination coverage is effective in preventing the prevalence of measles and mortality due to measles the most as compared to other diseases. In addition to that, we also found that, as we hypothesized, the measles vaccination coverage also helped reduce the prevalence and the mortality of other diseases. This result is consistent with findings from the literature that found the evidence of the immune amnesia due to the contraction to measles in developed countriesCitation6,Citation7,Citation11 as well as with studies conducted in developing countriesCitation12–15 which found the correlation between the measles prevalence and the fewer cases of other diseases and overall mortality. Studies which examined the impacts of measles vaccination on the prevalence of other infectious diseases are, however, extremely scarce especially in developing countries.
This paper has an important policy implication. Because we found that measles vaccination not only prevented measles, but also could it potentially prevent other diseases, the effect of the measles vaccination could be underestimated if we do not take into account of its effect on other diseases. Measles vaccine is proven to be highly cost-effective in the existing literature.Citation16,Citation17 For example, supplementary immunization activities (SIAs) have played a vital role in measles control efforts.Citation18 However, existing studies that conducted cost-effectiveness or benefit analyses of SIAs did not include averted disease cases and deaths due to immune amnesia.Citation19,Citation20 Thus, future studies should investigate the cost-effectiveness of the measles vaccination, accounting for the full effect of measles vaccination on other diseases’ prevalence.
Limitation
This paper has several limitations. First, this paper does not address the causal relationship. Because the measles prevalence or measles vaccination coverage is unlikely to be exogenous, the interpretation of results needs caution. Second, we did not differentiate between immunity obtained by vaccination and natural infection through a biological study. Future studies should address this issue. Third, this research analyzed younger children whose ages range from 1–4 and 5–9 years old due to the availability of data. However, it is vital to understand how young infants and older age groups contribute to the measles virus transmission.Citation4 Fourth, we focus on the first dose of measles vaccine in our analysis due to the data availability. When data are available, it is important to evaluate the effect of the full vaccination. Fifth, although we have included the country- and year-fixed effects in the regression specification to control for any unobserved confounding factors, we did not control for other unobserved factors that vary within a country over time. Thus, we should be cautious in interpreting the magnitude of effect size. We expect that the magnitude of impact would be different once we control for such factors.
Conclusion
Measles vaccination can have a large impact on children’s health because not only does it reduce the prevalence of measles cases and deaths but also could it potentially reduce the prevalence of and deaths due to other diseases.
Authors contributions
RS and MH conceived the idea. RS analyzed the data. RS and MH drafted the manuscript. Authors contributed equally to work.
Disclosure statement
No potential conflict of interestwas reported by the authors.
Additional information
Funding
References
- Minal P, Goodson J, Alexander J, Kretsinger J, Samir S, Steulet C, Gacic-Dobo M, Rota P, McFarland J, Menning L, et al. Progress toward regional measles elimination—worldwide, 2000–2019. Morbidity Mortality Weekly Report. 2020;69(45): 1700–05. doi:10.15585/mmwr.mm6945a6.
- World Health Organization. Measles. Regional Office for Africa; 2021 [accessed 2021 Aug 1]. https://www.afro.who.int/health-topics/measles.
- World Health Organization. Measles vaccines: WHO position paper. Weekly Epidemiological Record= Relevé épidémiologique hebdomadaire. 2009;84(35): 349–60.
- Goodson JL, Masresha BG, Wannemuehler K, Uzicanin A, Cochi S. Changing epidemiology of measles in Africa. J Infect Dis. 2011;204(suppl_1): S205–S214. doi:10.1093/infdis/jir129.
- Anderson R, May R. Vaccination and herd immunity to infectious diseases. Nature. 1985;318(6044): 323–29. doi:10.1038/318323a0.
- Mina M, Metcalf J, De Swart R, Osterhaus A, Grenfell B. Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science. 2015;348(6235): 694–99. doi:10.1126/science.aaa3662.
- Mina MJ. Measles, immune suppression and vaccination: direct and indirect nonspecific vaccine benefits. J Infect. 2017;74: S10–S17. doi:10.1016/S0163-4453(17)30185-8.
- Chevalier-Cottin E-P, Ashbaugh H, Brooke N, Gavazzi G, Santillana M, Burlet N, Htar MTT. Communicating benefits from vaccines beyond preventing infectious diseases. Infectious Dis Thera. 2020:9:467-480.
- Mina MJ, Kula T, Leng Y, Mamie L, De Vries RD, Knip M, Siljander H, Rewers M, Choy DF, Wilson MS, et al. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science. 2019;366(6465): 599–606. doi:10.1126/science.aay6485.
- Morales GB, Muñoz MA. Immune amnesia induced by measles and its effects on concurrent epidemics. J Royal Soc Interface. 2021;18(179): 20210153. doi:10.1098/rsif.2021.0153.
- Behrens L, Cherry JD, Heininger U. The susceptibility to other infectious diseases following measles during a three year observation period in Switzerland. Pediatr Infect Dis J. 2020;39(6): 478–82. doi:10.1097/INF.0000000000002599.
- Higgins JPT, Soares-Weiser K, Reingold A. Systematic review of the non-specific effects of BCG, DTP and measles containing vaccines. World Health Organization Report; 2014.
- Ashbaugh H, Cherry J, Hoff N, Doshi R, Alfonso V, Gadoth A, Mukadi P, Higgins S, Budd R, Randall C, et al. Association of previous measles infection with markers of acute infectious disease among 9-to 59-month-old children in the Democratic Republic of The Congo. J Pediatric Infect Dis Soc. 2019;8(6): 531–38. doi:10.1093/jpids/piy099.
- Ashbaugh H, Cherry JD, Sue Gerber SG, Higgins AG, Alfonso VH, Mukadi P, Hoff N, Doshi R, Rimoin AW. Reported history of measles and long-term impact on antibody to tetanus in children 6–59 months of age receiving DTP in the Democratic Republic of Congo. Open Forum Infect Dis. 2017;4(suppl_1): S323–S323. US: Oxford University Press. doi:10.1093/ofid/ofx163.761.
- MacIntyre CR, Costantino V, Heslop DJ. The potential impact of a recent measles epidemic on COVID-19 in Samoa. BMC Infect Dis. 2020;20: 1–6.
- Ozawa S, Mirelman A, Stack ML, Walker DG, Levine OS. Cost-effectiveness and economic benefits of vaccines in low- and middle-income countries: a systematic review. Vaccine. 2012;31(1): 96–108. doi:10.1016/j.vaccine.2012.10.103.
- Kaucley L, Levy P. Cost-effectiveness analysis of routine immunization and supplementary immunization activity for measles in a health district of Benin. Cost Eff Res Allocation. 2015;13(1): 1–12. doi:10.1186/s12962-015-0039-7.
- Khetsuriani N, Deshevoi S, Goel A, Spika J, Martin R, Emiroglu N. Supplementary immunization activities to achieve measles elimination: experience of the European Region. J Infect Dis. 2011;204(suppl_1): S343–S352. doi:10.1093/infdis/jir074.
- Bishai D, Johns B, Nair D, Nabyonga-Orem J, Fiona-Makmot B, Simons E, Dabbagh A. The cost-effectiveness of supplementary immunization activities for measles: a stochastic model for Uganda. J Infect Dis. 2011;204(suppl_1): S107–S115. doi:10.1093/infdis/jir131.
- Hayman DTS. Measles vaccination in an increasingly immunized and developed world. Hum Vaccin Immunother. 2019;15(1): 28–33. doi:10.1080/21645515.2018.1517074.