How I became a researcher
 After graduating from school, I was certain that I wanted to continue my studies, and my choice was between dentistry and medicine. Both educations were offered at the Karolinska Institutet in Stockholm. My father, who was a dentist, advised me to choose medicine. He told me that it would offer so manydifferent paths once I passed the first semester. And my mother, a correspondent and icon painter, helped me once I started with the tedious German anatomy of Rauber Kopsch: Anatomie des Menschen, the facts of which are still true. During the second year in medical school – which was mainly chemistry – I became impatient and tried to enroll with Prof. George Klein for a research project. At the time, he was a pioneer of tumor biology for which he had recently established a whole building of fervent activity, the Tumor Biology department. He immediately sent me to his second in charge, Olle Sjögren, who enthusiastically welcomed me to his group. This was the only procedure needed to register for PhD studies at the Karolinska Institutet in 1960. It was done in less than one hour.
After graduating from school, I was certain that I wanted to continue my studies, and my choice was between dentistry and medicine. Both educations were offered at the Karolinska Institutet in Stockholm. My father, who was a dentist, advised me to choose medicine. He told me that it would offer so manydifferent paths once I passed the first semester. And my mother, a correspondent and icon painter, helped me once I started with the tedious German anatomy of Rauber Kopsch: Anatomie des Menschen, the facts of which are still true. During the second year in medical school – which was mainly chemistry – I became impatient and tried to enroll with Prof. George Klein for a research project. At the time, he was a pioneer of tumor biology for which he had recently established a whole building of fervent activity, the Tumor Biology department. He immediately sent me to his second in charge, Olle Sjögren, who enthusiastically welcomed me to his group. This was the only procedure needed to register for PhD studies at the Karolinska Institutet in 1960. It was done in less than one hour.
It was amazing how quickly and effortlessly scientists at KI welcomed students, introduced us to their laboratory work and took us to informal seminars with world renowned international visitors. In this environment I learnt about the most fascinating discoveries. I read the book “Oncogenic viruses” by Ludwik Gross on filtered entities from enlarged spleens of the AK mouse strain that spontaneously develops leukemia. The Gross virus was first isolated in 1951 and found to induce lymphatic leukemia when inoculated into newborn mice of non-leukemic strains.
I became immensely fascinated by this tumor virus and started right away in their projects to dissect mice and collect lymph nodes and spleens. The use of these cells to immunize other mice resulted in my first scientific article in 1962.
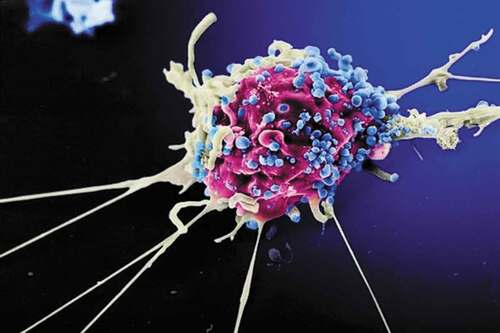
My first visual experience with the variable world of viruses was made together with Sten Jakobsson at the electron microscope at the Sabbatsberg Hospital in 1964. We subjected Gross leukemic cells to the cytotoxic antibodies I had made in mice. In the presence of complement, we could observe swollen or broken cell membranes at regular distances, with more severely damaged cell membranes in other cells or even disorganized dying cells. The Gross virus buds through the cell membrane, and here we had discovered the initial mechanisms for killing virus-infected cells through cytotoxic antibodies induced by the vaccinations.
George Klein and his wife Eva then went to the US and left me with two rooms containing 160 cages of mice of various strains to breed and to do experiments on. Six generations later the mice were still cautiously inbred, and I had discovered that the lymphoma cells contain antigens related to the Gross virus. The tumor cells had new virus-induced cellular antigens caused by the virus, and these antigens could be used for immunization against the virus but also to protect against development of tumors and lymphomas. Curiously, immunization with the virus or the virus-infected cells could also delay or prevent the development of the hereditary leukemia of the AK mouse strain. I realized a virus-specific antigen must be present in both the endogenous and transplanted leukemic cells.
My fellow student Hans Wigzell, who later became the head of the Immunology department, studied the mechanism of cytotoxic cell killing. He gave me some tubes of Friend virus, before he too departed for a US visit. I discovered that the Friend leukemia could be inhibited both by immunizing the mother of tumor-prone pups or by passive immunization by antibody or lymphoid cells. My leukemia-virus findings were revealed in parallel with the findings on polyoma virus-induced antigens that could inhibit development of multiple tumors, studies performed by George and Eva Klein and Olle Sjögren.
One day during our coffee seminar, the Nobel prize of Watson and Crick was announced, and we then understood much more about nucleic acid replication. I could formally show that both the Gross virus and the Friend virus were RNA viruses. The next big enlightenment came when Baltimore and Temin (1965) received the Nobel prize for RNA virus replication through DNA and reverse transcriptase. These findings helped to understand the eternal presence of retroviruses in cells. Imagine my chagrin when I visited Renato Dulbecco in Boston in 1966 and admired his invention of cultivating polio virus in cell culture. To be polite I asked: Have you ever been to Stockholm? Yes, he said, when I received the Nobel Prize last year …
In 2008 Harald zur Hausen received the Nobel Prize for identifying the HPV as origin of cancer in humans, but he had thought about and published thoughts on virus-induction of human tumors already in the 1970s. Effective vaccines against malignant HPV types have been developed that inhibit both virus infection and the resulting cervical cancers. There are now up to 20 tumorigenic HPV types, and a vaccine that is 9-valent. Today, the vaccines directed against human papilloma virus particles are the most effective preventive vaccines for cervical cancer. But there is as yet no vaccine against established transformed tumor cells. Five common human tumor types are induced by viruses from the retroviral- herpes-, papilloma- and hepatitis viral families and do carry oncoviral antigens.
I presented my PhD in 1966 with a thesis that described immunity against virally induced tumors. As the most competent opponents I had Erling Norrby, professor of Virology, and Göran Möller, professor of Immunology. I was quite nervous the day before my thesis defense. On the morning of the thesis presentation, my considerate husband Patrik therefore fed me two chocolate bars and a small piece of Valium. Thus, I was not nervous anymore, but somewhat lethargic in my responses. I was awarded the highest of honors which meant that I automatically got the title of associate professor.
It wasn’t long after my PhD thesis before I was supervising my own research students. My first student, Marta Granström, studied the role of lipoproteins in blood during hematopoiesis. To obtain some human samples, she was sent out of the laboratory to have a fatty lunch on bacon, lard-strips and fried eggs. Imagine our reaction to her venous blood being neither red nor blue, but solid white! With only 10 ml at hand, we had lots of material for her study on low-density lipoproteins.
Infectious diseases and oncology
Before my medical studies were finished, I was recruited by Jerzy Einhorn to the clinical Oncology department, Radiumhemmet. Professor Einhorn had built an experimental laboratory beside the clinic and recruited young researchers from the Karolinska Institutet Campus to help develop clinical science associated to patient care, a system not found in Europe at the time. For me, this resulted in interesting work both as a clinical oncologist and in parallel diagnosing viral diseases at the National Bacteriological Laboratories, later re-named the Swedish Institute for Infectious Disease Control.
In the oncology clinic I became interested in tumor-associated antigens of testicular cancer. Most interesting were the hormonal/enzymatic proteins that gave clues to the differentiation and pathogenicity of the tumor and indicated whether occult metastasis occurred. We discovered isoenzymes of the placental alkaline phosphatase produced by seminoma cells in 1977, and also introduced several tumor antigens to the hospital laboratories, to be used for serological monitoring of tumor load.
We made several attempts to immunize against alpha fetoprotein (AFP) or carcinoembryonic antigen (CEA), which were considered the tumor antigens most characteristic of malignancies, although of endogenous origin. Through a collaboration with Håkan Mellstedt we immunized individuals who were tumor free after radical operation, but had a high probability to develop metastasis due to their stage of primary colorectal cancer. Although cellular immune responses against CEA were induced, there was no decreased proportion of recurrencies either in time or in frequency. I wish that we had had at our disposal, one of the checkpoint inhibitor monoclonal antibodies, for a combinatorial therapeutic approach. Later, combinations with monoclonals interfering with T-cell immune checkpoints have shown better immunization results. Immunolocalization studies with labeled anti-CEA antibody were also performed in patients with colon cancer and tumors were localized by emission computed tomography. The accurate localization was 70–75% and we detected a few previously unknown tumors.
HIV vaccine development
The disease of AIDS – a severe immunodeficiency – started to appear in the 1980s. About this disease I said: To do research on AIDS you will have to go to the US. The first meeting in Belgium was horrific, a new disease caused by a virus, the transmission unclear, we were all afraid. In the first patients that appeared in Sweden, we discovered that the specific cell-mediated immune response was usually absent at a time when other lymphocyte responses appeared normal or near normal. This defect is a major factor in patients´ incapacity to combat the latent virus. It was clear that vaccines should be made that could stop this disease.
From collaborating with Astra/Medivir on antiviral agents, we proceeded to make a vaccine by the novel technology of DNA immunization. During this time and later I have had a great collaboration with Margaret Liu, who had discovered that cellular cytotoxicity can be induced by genetic immunization.
My students at the time participated in the design of HIV-DNA plasmid vaccines and the readout in multiple animal systems. Preclinical HIV-1 vaccine protocols were assessed for efficacy in an experimental murine model we had developed for this purpose. We showed that priming with the HIV-DNA plasmids followed by a protein or vector boost was the most effective to protect these animals from HIV infectious challenge. We sought the optimal combination of antigens to inhibit viral replication and ended up with seven HIV-DNA plasmids for our first clinical trials in 1996.
Gerald Voss took us to Rixensart in Belgium, the large complex of vaccine production of GlaxoSmithKline in Europe. He told us that such a complex medicine/vaccine could never make it into humans. It has, however, been launched in several clinical trials performed in Sweden with collaborators Eric Sandström and Gunnel Biberfeld, as well as in Italy, Tanzania, and Mozambique. The DNA plasmids appeared to be very effective in priming for immune responses against a variety of HIV strains since they stimulated both innate, humoral, and cell-mediated immunities.
During this period, I collaborated with Dr Annika Linde to improve viral detection by polymerase chain reaction, PCR, at the Beijing Children’s Hospital in China, one of the largest pediatric hospitals worldwide. I also collaborated with David Goldenberg at Immunomedics in New Jersey for synthesizing novel cell surface-acting antiviral drugs, and with researchers at Karolinska Institutet, Pontus Blomberg and Katrin Markland at Vecura for creative production and safety instructions on DNA vaccine production and all the time with Jorma Hinkula, Kalle Ljungberg and Maria Isaguliants, who provided ingenious experimental ideas and clever company.
We found that immunodeficient children respond better to HIV vaccine immunotherapy than infected adults. Therefore, the Epiical project is the most exciting one of all. Children who are HIV-infected at birth and receive antiretroviral compounds will be repeatedly immunized with the seven HIV-DNA plasmids and an HIV vector boost. In children who are HIV-infected at birth, the general immune system is usually intact, and their virus level is very low. By vaccination, it might thus be possible to further diminish or perhaps even eradicate HIV. The prime-boost HIV vaccine schedule was developed in a collaboration with Merlin Robb at the Henry Jackson Foundation and Paolo Rossi from the European Pediatric foundation PENTA. This NIH supported R01 project was initiated in 2017 and is anticipated to have results in 2023.
National and international teaching
I have been involved as a teacher of medical subjects during my whole career. Through the years, there have been around 50 PhD students under my direct tuition. I am still in contact with many, although now they are supervising me. My philosophy as supervisor is based on my own experience from the period as research student – to be given the chance to work independently, while at the same time having access to colleagues who work with similar issues, possibly from different viewpoints. It is also important to be disciplined, and I admit that I was not very disciplined when young. I learned the importance of discipline in the clinic.
The European research consortia provide an excellent opportunity for courses on HIV vaccinology. Joan Joseph in Barcelona, Barbara Ensoli in Rome and Robin Shattock in London lent support to the AVIP, Europrise and EAVI2020 PhD schools. During the vaccine courses students spend time together at a laboratory with intensive teaching, seminars, study visits and group meetings. They train to present scientific articles, and to discuss scientific results. Finally, the students end up as teachers and take leading roles in discussions and presentations.
A place where it was easy to teach students was the Keystone Conference in Colorado. Each winter I took several virology students to the conference centers and mountains. It was amazing how fast we learned about both virally induced diseases and downhill skiing!
We have acquired what I found so compelling during the first year in medical school – that you can obtain creative moments during interaction in an informal and simple way close to books, computers, and lecture tables, often with some good food. In the pediatric course, we had Italian professor and friend Paolo Palma cooking pasta in my home together with 20 students and teachers from different universities around the world!
Finally
Throughout my career, I have worked with viruses and the work has led to diagnostic methods, antiviral drugs, and novel experimental vaccines against cancer and HIV. Working to develop vaccines for humans has led me to become more of an inventor than discoverer. My collaborators and research students are working to develop the HIV vaccine further.
During the last two years, I am a voluntary senior scientist. I am amazed by how rapidly known and yet new technologies were applied to sequence the strains of Sars-Cov-2 virus, and how very rapidly many laboratory scientists and companies collaborate to provide novel vaccines.
The only vaccine that has eradicated a disease is the smallpox vaccine. The last smallpox virus outbreak in Sweden occurred during my course in infectious diseases. Twenty-seven people got infected from a sailor traveling from Australia through Indonesia and India. Not until three virus transfer generations later was the disease correctly diagnosed and could be traced and stopped after seven generations of transmission. We students had to sit outside of the clinic on the lawn at Roslagstull Hospital in Stockholm. I had the privilege of spending many days with photographer Lennart Nilsson to visualize the vaccinia pox virus routes of infection of cells. Pox viruses can actually be seen by ordinary light microscopy and were comparatively easy to monitor. Photo: Lennart Nilsson.
Disclosure statement
No potential conflict of interest was reported by the author.
Additional information
Funding
Notes on contributors
Britta Wahren
Britta Wahren was born in Dalecarlia, Sweden in 1938. She was married to engineer Patrik and has two daughters Marie and Emilie, both in the medical field. She became professor of Clinical Virology in 1992 at the Karolinska Institutet in Stockholm, where she graduated both for an MD and a PhD and made scientific and clinical careers. Until 2005 she was head of Dept of Virology at the Swedish Institute for Infectious Disease Control, and then at the Department of Microbiology, Tumor and Cell Biology at Karolinska Institutet. In 2000, she conceived and initiated the new Dept of Virology at Karolinska Institutet Huddinge Hospital. Her specialities include Virology and Clinical Oncology. She is presently professor emerita at Karolinska Institutet and collaborates at the WiKiKi.se documentation site.
Dr. Wahren has been on the boards of several research committees, such as the Swedish Medical Research Council, the Swedish Cancer Foundation, the Globvac program for the Research Council of Norway, and served as scientific advisor to committees of the European Council, the Erasmus Medical Center in the Netherlands, the US National Institutes of Health and the US National Cancer Institute. She contributed to the initiation of and was a member of the Swedish governmental board for Gene Technology. She has organised national and international meetings and conferences, such as a Nobel Conference on Genes that induce Immunity in 1996, and the International conferences on AIDS in Stockholm 1988 and Vancouver in 1996. Together with Patrik Wahren she wrote Framtidens farliga smitta in 2007, a book on future infectious pandemics.
She has been the tutor of over 50 doctoral students for their PhDs at the Karolinska Institutet. She was also examiner/opponent for PhD students at universities in Europe and Africa 1965-2020. She has served as director of European PhD research schools, the latest one in the EU Horizon program EAVI2020. In 2014 she received the Cancer and Allergy foundation prize for developing a cancer vaccine and in 2015 the Karolinska Institutet Silver Medal for outstanding research on HIV. Her portrait was posted at the Swedish Medical Society in 2018.
Since 1962 until today, Britta Wahren has published over 600 scientific articles in the subjects of virology and oncology and contributed to chapters in books on the same subjects. In her research she discovered viral and tumor immunogenicity of murine leukaemia viruses and identified human organ-specific fetal and tumor antigens. These markers were established as diagnostic and research tools in the clinical setting. She has discovered the family spread of herpes viruses and studied antiviral mechanisms against herpesviruses and HIV. Her laboratory introduced antiviral assays and established national clinical networks. As a member of the board, she was involved in establishing and monitoring the European and Developing Countries Clinical Trial Program – EDCTP, a European–African partnership supported by the European Union to develop HIV, Tuberculosis, and Malaria treatments for developing countries.
Britta Wahren has designed HIV-DNA vaccines for several European Community research programs, with the aims to design and produce vaccines and to perform clinical trials of HIV vaccines. The HIV vaccines that she and her group designed and produced were used in phases 1 and 2 clinical trials in Europe and Africa. A pediatric program, RV534 Epiical, is ongoing, with her DNA-based HIV vaccine acting as a prime for boosting the immune response of children born with HIV infection. Her present research interest is devoted to genetic vaccines, expression of single viral genes and induction of immunity to the gene products.