ABSTRACT
Human Papillomavirus (HPV) is one of the most common sexually transmitted infections associated with a wide range of diseases and cancers that may affect both genders. Since 2007, the Spanish National Immunization Program includes HPV vaccination, and currently it only targets 12-year-old girls. The objective of our study is to assess differences in the knowledge of HPV and HPV vaccine acceptability according to different factors, and to identify the role of different sources of information. A cross-sectional, multicenter survey research was carried out in twenty-four pediatric offices in Spain, and included parents of children aged 9 to 14 years old. 1,405 valid survey-responses were considered for the analysis. Parental awareness of HPV and HPV vaccine, as well as vaccine acceptability, are still strongly associated with child gender (girls) and age (12–14 years old). HPV knowledge and HPV vaccine acceptability are related to parental gender, HPV vaccination status and having at least one daughter. Parents who consulted a healthcare source to obtain further information about HPV had greater HPV and HPV vaccine knowledge and acceptability. HPV and HPV vaccine awareness and acceptability are strongly associated with child gender and age, which correlates with the current immunization program.
Introduction
Human Papillomavirus (HPV) is one of the most common sexually transmitted infections: it is estimated that between 75% and 80% of sexually active individuals will come into contact with the virus.Citation1 Although most infections are cleared by the immune system within a few months, about 5%-10% of them may persist.Citation2 The persistence of HPV infection can cause diseases such as genital warts, precancerous lesions, and certain cancers such as cervical, vulvar, vaginal, anal, penile and head and neck cancers.Citation3 The prevention of HPV infections through vaccination is the most promising and efficacious strategy against such a common sexually transmitted infection.Citation2 Currently, there are three vaccines available in Spain: the tetravalent and the bivalent vaccine that are available since 2007, and the nonavalent vaccine that is available since 2017.Citation4
In Spain, the National Immunization Program (NIP) commenced in 2007 and currently targets only 12-year-old girls. According to the latest data available, the average vaccination coverage rate in girls in 2019 was 79.0% for the 2-dose schedule.Citation5 However, since 2018, the Spanish Association of Pediatricians (AEP) recommends HPV vaccination for boys and girls at the age of 12 years, although vaccination for boys is not funded yet.Citation6
Over these years, the Spanish studies that evaluated knowledge of HPV, vaccine acceptability and drivers of HPV vaccination had focused exclusively on female or adult populations and were performed in specific regions across Spain, not being representative of the entire country.Citation7–9 Therefore, in 2019–2020, we conducted the KAPPAS study: Knowledge and Acceptability of Papillomavirus Vaccines in Parents of Adolescents in Spain. It is the first national, cross-sectional, multicenter survey research to assess HPV knowledge and vaccine acceptability among the parents of adolescents in Spain.Citation10 Recruitment and analysis performed in this study, offer an innovative approach to obtain relevant insights about current HPV vaccination knowledge and acceptability that will be also useful for a future implementation for a gender-neutral vaccination program in the country.
Recommendations on HPV vaccination are widespread across the WHO (World Health Organization) European Region, and the number of countries that have introduced gender-neutral vaccination (GNV) programs, targeting girls and boys, has increased in recent years.Citation11 A recent targeted literature review highlights that 28% of WHO European countries were providing fully- or partially funded HPV vaccination programs for both genders, girls and boys, by 2018–2019.Citation9 In those countries where HPV GNV programs have been implemented, vaccine coverage rates reach similar percentages among boys and girls.Citation12
The factors associated with HPV knowledge and vaccine acceptability in adolescents and their parents in countries where HPV vaccine is licensed had been studied in the literature.Citation13–15 According to a previous systematic literature review that examined seventy non-interventional studies conducted in 16 European countries, the main factors associated with HPV knowledge were female gender, higher education and higher-income group.Citation13 The factors associated with HPV vaccine acceptability were female gender and younger age of the responding parents, female gender of the child, having received previous vaccinations during the childhood and previous confidence in vaccine efficacy.Citation13 In addition, other publications found significant correlations between an increased acceptability of HPV vaccine and the improvement of awareness and knowledge of HPV infection and vaccination.Citation16 Despite all the previous studies, vaccination coverage rates are still suboptimal, and a deeper understanding of factors influencing parental HPV vaccination knowledge and acceptability is critical to ensure the successful implementation of HPV vaccination programs.Citation17–20
Moreover, vaccine misinformation and infodemia are increasing threats during the SARS-CoV2 (Severe acute respiratory syndrome coronavirus 2) pandemic.Citation21,Citation22 The WHO recently published a guide on misinformation management which also underscores the importance of promoting informed health decisions based on accurate and scientific information.Citation23 Information sources are a critical factor to overcome these threats and few studies have assessing their impact among parents of adolescents for HPV vaccination.Citation24,Citation25
The results of the primary objective of the KAPPAS, assessing HPV knowledge and vaccine acceptability in general, are subject of a separate publication and have been already presented elsewhere.Citation8 Here, we address the results of the secondary objectives of the KAPPAS study, focused on assessing the factors influencing HPV knowledge and vaccine acceptability in parents of adolescent children.
Materials and methods
Study design and setting
This study is an analysis of secondary outcomes of the KAPPAS study: a cross-sectional, multicenter survey research study. Twenty-four (24) sites (public and private) across Spain participated in the study. Recruitment was performed through pediatricians and targeted the fathers, mothers or legal tutors of children (girls and/or boys) aged 9 to 14 years who had been living in Spain for the last 12 months at least.
The study secured the approval of the reference Investigational Ethical Committee (IEC) on January 8, 2019. Other local IEC also approved the protocol when necessary.
Survey development
A structured survey was developed to collect epidemiological variables as well as knowledge- and acceptance-related measurements. The questionnaire was developed on the basis of a previous systematic literature reviewCitation13 carried out by our group to identify published studies and items used to evaluate parental and/or adolescent HPV knowledge and/or HPV vaccination acceptability. The draft questionnaire was then validated by an Expert Committee comprised of 4 expert pediatricians in HPV and adolescents. It was subsequently tested by means of a cognitive debriefing methodology on a representative sample of 12 parents following the adjustment of wording and comprehensiveness according to the participants’ suggestions. The final version of the questionnaire was validated by the Expert Committee.
The survey (included in the Supplementary material) included five sections: 1) sociodemographic characteristics (15 items); 2) knowledge of HPV (9 items); 3) knowledge of vaccines and their acceptability in general (5 items); 4) HPV vaccination knowledge (8 items); 5) HPV vaccine acceptability (7 items). The points were summated to create a total score. The Degree of HPV knowledge total score ranged from 0 to 40, the Degree of HPV vaccine acceptability ranged from 0 to 5, the Degree of HPV vaccination knowledge ranged from 0 to 21 and the Degree of knowledge of vaccines and their acceptability in general ranged from −10 to 10. All questions were either open- or closed using the appropriate response scale depending on the specific question (yes/no, yes/no/not sure, ordinal scale of level of agreement or specific response options, when needed).
Data collection
The parents were invited to complete the study survey (either online or in a paper-and-pen format) by the investigator following the order generated by a randomization tool and according to stratification quotas defined to ensure population representativeness.
An active recall recruitment process was designed to avoid any selection bias, since chronically ill patients may attend pediatrician offices more frequently than healthy children. All children between 9 and 14 years old were identified through investigator databases or medical records and were divided into stratification quotas based on gender (male/female), age (9–11 y.o./12-14 y.o.) and HPV vaccine coverage rate (VCR) in the region (high/low). Parents had to complete the study survey exclusively for the selected son or daughter. All the participants gave their consent before filling in the survey.
Statistical analysis
The potential factors assessed that might influence HPV knowledge and HPV vaccine acceptability were: HPV vaccination status (yes/no); gender (boys/girls), age (9–11 y.o./ 12–14 y.o.); HPV VCR in the region (since the mean national VCR was 77.8% in 2016, latest data available when the protocol was approved, regions with a VCR of ≤77.8% and >77.8% were regarded as low- and high-VCR regions, respectively); the gender of the respondent parent (male/female); region; province; location (urban, semi-urban, rural); type of center (private vs. public); parent’s age; educational level; work status; nationality; marital status; parent’s vaccination status; number of children; gender of the children in the family (proportion of daughters ≥50% or <50%) and having at least one daughter over the age of 9.
The t-test for independent samples was considered when mean differences associated with dichotomous variables were analyzed. The one-way ANOVA for independent measures was chosen for polytomous questions. Tukey HSD (Honest Significant Difference) pairwise comparisons were considered. Chi-square tests were computed to measure the association between qualitative variables.
Two regression analyses were performed to evaluate the effect of the different variables on knowledge of HPV and the acceptability of the HPV vaccine. For this purpose, ordinary least squares regression analyses were carried out with best subsets regression as an exploratory model for building regression analyses. A random forest algorithm was considered due to problems with collinearity and link function with the linear regression model when explaining the degree of acceptability of the HPV vaccine.
Results
A total of 3,110 participants were selected and contacted, 1,071 of whom did not answer and 55 declined to participate. After the invalid survey responses had been excluded (n = 79) 1,405 surveys were considered valid for the analysis (1,116 online and 289 paper-based) (see reasons for invalid surveys in Figure S1). The parents’ sociodemographic profile is provided in the Supplementary Material (Table S1), most of them were mothers (86.19%) aged between 40 and 49 years (69.11%). 52.38% of the children on whom the survey was completed were girls. The mean age of these children was 11.49 years, and 27.83% of them were vaccinated against HPV. Among the vaccinated ones, 87.98% were girls and 12.02% were boys.
Factors determining HPV knowledge and HPV vaccine knowledge and acceptability
Factors related to the child for whom the survey was completed
Child gender
Parental knowledge and acceptability of HPV vaccine was significantly higher when the parents´ answers refers to a girl compared to a boy (p < .001) (). Mean estimations are obtained based on the responses to the items of the questionnaire, as described in the Supplementary material.
Figure 1. Child-related factors influencing HPV knowledge and HPV vaccine acceptability. (a) Child gender. (b) Child age. (c) Child vaccination status. Boxplot representations of scores for, from left to right, HPV knowledge (score range: 0 to 40), knowledge and acceptance of vaccines in general (score range: −10 to 10), HPV vaccine knowledge (score range: 0 to 21) and HPV vaccine acceptability (score range: 0 to 5). The line inside the box represents the median. The lower and upper boundaries of each box indicate Q1 and Q3, respectively.
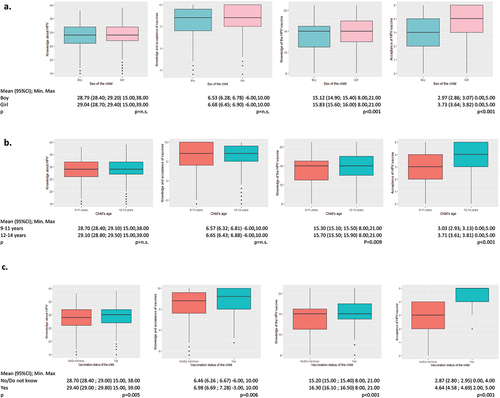
Total scores for the sections “HPV knowledge” and “knowledge and acceptance of vaccines in general” do not differ significantly by the child gender. ().
Child age
The parents who responded the survey about a child aged 12–14 years old obtained slightly but significantly higher mean scores regarding knowledge and acceptability of HPV vaccine compared to parents with a child aged 9–11 years (knowledge of HPV vaccine: p = .009; acceptability of HPV vaccine: p = .001) (). There were no significant differences when comparing both child age groups regarding HPV knowledge and knowledge and acceptance of vaccines in general ().
Child’s HPV vaccination status
Parents of vaccinated children obtained significantly higher mean scores in all 4 knowledge and acceptability variables compared to those who did not know their child’s vaccination status or whose child was not vaccinated (knowledge of HPV: p = .005; knowledge and acceptance of vaccines in general: p = .006; knowledge of HPV vaccine: p < .0001; acceptability of HPV vaccine: p < .001) ().
Factors related to family/parental characteristics
Parent gender
Mothers obtained significantly higher mean scores than fathers in knowledge of HPV (p < .001), knowledge of HPV vaccine (p < .001) and acceptability of the HPV vaccine (p = .001) (). There were no differences in parent gender with regard to knowledge and acceptability of vaccines in general ().
Figure 2. Factors related to family/parental characteristics influencing HPV knowledge and HPV vaccine acceptability. (a) Parent gender. (b) Parental HPV vaccination status. (c) Having at least one daughter. (d) Number of daughters in the family. (e) Having at least one daughter of vaccination age (≥9 y.o.). Boxplot representations of scores for, from left to right, HPV knowledge (score range: 0 to 40), knowledge and acceptance of vaccines in general (score range: −10 to 10), HPV vaccine knowledge (score range: 0 to 21) and HPV vaccine acceptability (score range: 0 to 5). The line inside the box represents the median. The lower and upper boundaries of each box indicate Q1 and Q3, respectively.
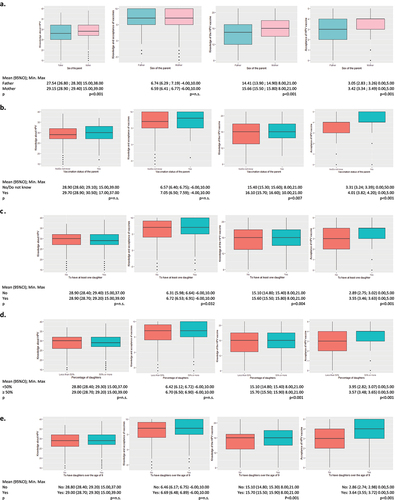
Parental HPV vaccination status
Parents who reported to be vaccinated against HPV evinced greater knowledge of HPV vaccine (p = .007) and greater acceptability of HPV vaccine (p < .001) (). However, no differences were found for HPV knowledge or acceptability of vaccines in general ().
Parental age
The acceptability of the HPV vaccine was not statistically different among groups of parents according to age. However, mean HPV vaccine knowledge was lower in parents aged 30–39 years compared to parents over 40 years (p < .001). Regarding HPV knowledge, parents aged 40–49 years obtained significantly higher mean total scores than those aged 30–39 years (p = .002). Finally, parents aged 50 or older obtained higher means in knowledge and acceptability of vaccines in general (p = .028).
Parental educational level
The average level of knowledge of HPV, HPV vaccine and knowledge and acceptance of vaccines in general increased significantly as the educational level of the parents increased (p < .001 all variables), although no differences were found in their level of acceptability of HPV vaccine.
Having at least one daughter
Having at least one daughter was associated with significantly greater knowledge (p = .004); and acceptability of HPV vaccine (p < .001). No differences were observed for HPV knowledge ().
Number of daughters in the family
The mean HPV vaccine knowledge score was significantly higher among families in whom less than 50% of the children were daughters vs. ≥50% being daughters; p < .001. In contrast, the acceptability of HPV vaccine was significantly higher among parents with a lower proportion of daughters in the family (<50% daughters vs. ≥50% daughters; p < .001). No significant differences between the proportion of daughters in the family and the knowledge of HPV and knowledge and acceptance of vaccines in general were found ().
Having at least 1 daughter of vaccination age (≥9 years old)
The results showed that having at least one ≥9-year-old daughter was associated with significantly higher scores in HPV vaccine knowledge (p < .001) and acceptability (p < .001). However, no differences were found for HPV knowledge or knowledge and acceptability of vaccines in general ().
Other parental or family factors
No significant differences were observed with regard to knowledge of HPV, knowledge of HPV vaccine and acceptability of HPV vaccine when the groups were compared according to: parent’s employment status (unemployed vs. part-time vs. full-time), nationality (Spanish vs. other), marital status (married vs. not married) and number of children (1 vs. 2 vs. 3 vs. 4 or more) [data not shown].
Other sociodemographic factors
Region vaccine coverage rate
Statistically significant differences were found when parental knowledge scores in regions with different VCR were compared, although no differences were observed regarding HPV vaccine acceptability (knowledge of HPV (range 0–40): high VCR: 29.35 vs. low VCR: 28.59; p < .001; knowledge and acceptance of vaccines in general (range −10 to 10): high VCR: 6.41 vs. low VCR: 6.77; p = .038; knowledge of HPV vaccine (range 0–21): high VCR: 15.72 vs. low VCR: 15.31; p = .009).
Province, place of residence and type of center
Mean scores in HPV knowledge were not statistically different according to the place of residence. Results considering whether the type of center was public or private did not show significant differences, except for the knowledge and acceptance of vaccines in general (range −10 to 10), which was higher among parents recruited from private centers (public, 6.19 vs. private, 7.50; p < .001).
Multivariate analysis
Knowledge of HPV
After 11 independent variables that were significantly associated with the degree of knowledge about HPV according to a bivariate t-test analysis had been identified, the multivariate regression model revealed that the most relevant variables for explaining the degree of knowledge of HPV were 1) knowledge of HPV vaccine, 2) consulting a healthcare source about HPV infection. This model accounts for 51.1% of the variance of the knowledge of HPV ().
Table 1. Multivariate models for HPV knowledge and acceptability of HPV vaccine
Acceptability of HPV vaccine
The individual bivariate analysis identified 13 independent variables that were significantly associated with the degree of acceptability of the HPV vaccine. The multivariate model for the acceptability of HPV vaccine based on a Random Forest algorithm included the following variables: 1) child’s vaccination status, 2) total score in knowledge of HPV vaccine, 3) total score in knowledge and acceptability of vaccines in general, 4) healthcare source consulted about HPV vaccine, 5) total score in knowledge of HPV and 6) parent’s vaccination status. The model accounts for 53.1% of the variance of the acceptability of the HPV vaccine ().
Impact of the sources of information consulted and knowledge of HPV, HPV vaccine and its acceptability
Specific analyses were carried out considering the type of source consulted by parents. A distinction was made between healthcare sources, which included pediatricians, general physicians, gynecologists, urologists, nurses, pharmacists and other healthcare professionals; and non-healthcare sources, such as school, family and friends, press, radio/TV, the Internet/social media, amongst others. The results showed that parents who consulted healthcare sources about HPV infection achieved a higher mean knowledge of HPV, knowledge of HPV vaccine and acceptability of HPV vaccine (all of them p < .001), although no differences were observed with regard to knowledge and acceptance of vaccines in general (p = .525) (). Similarly, parents who consulted a healthcare source about HPV vaccine had a significantly higher mean score in all 4 main variables: knowledge of HPV (p < .001), knowledge of HPV vaccine (p < .001), acceptability of HPV vaccine (p < .001) and knowledge and acceptance of vaccines in general (p = .003) ().
Figure 3. Influence of consulting healthcare sources about HPV infection (a) or HPV vaccine (b) on HPV knowledge and HPV vaccine acceptability. Boxplot representations of scores for, from left to right, HPV knowledge (score range: 0 to 40), knowledge and acceptance of vaccines in general (score range: −10 to 10), HPV vaccine knowledge (score range: 0 to 21) and HPV vaccine acceptability (score range: 0 to 5). The line inside the box represents the median. The lower and upper boundaries of each box indicate Q1 and Q3, respectively.
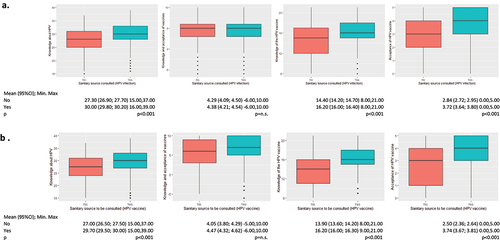
The differences in total scores when the specific healthcare source consulted was considered showed that gynecologists and pediatricians may provide more accurate information to parents. Parents who consulted other healthcare sources tended to obtain lower scores in terms of knowledge of HPV and HPV vaccine and acceptability (). Knowledge means were also higher when parents consulted the Internet or radio/TV, although their HPV vaccine acceptability was significantly lower. In general, consulting other sources led to lower mean scores in knowledge and acceptability of HPV vaccine ().
Table 2. Knowledge and acceptability scores according to whether or not respondents had consulted each healthcare source
Table 3. Knowledge and acceptability scores according to whether or not respondents had consulted other non-healthcare sources
Further information sources
In line with the results of the sources consulted, parents who stated that they would consult a healthcare source to get information about HPV infection or HPV vaccine also obtained significantly higher mean scores in HPV and HPV vaccine knowledge and HPV vaccine acceptability (p < .05 in all three variables, data not shown).
Discussion
KAPPAS preliminary findings showed that the degree of knowledge of HPV in Spain is still modest despite high vaccine acceptability.Citation8 The specific results of the secondary objectives of the study, reported here, suggests that parental awareness of HPV infection and vaccination, as well as HPV vaccine acceptability, are still strongly associated with their children’s gender and age, probably influenced by the Spanish NIP, which currently targets only 12-year-old girls. HPV vaccine awareness is greater among parents with children who match the profile currently funded by the NIP. In line with our findings, previous research showed that the acceptability of HPV vaccination among the male population was diminished by a lack of awareness and knowledge and a general perception of lower benefits of HPV vaccination for males.Citation26
Furthermore, an association was found between HPV knowledge and HPV vaccine acceptability and parent gender, which was higher among mothers than fathers. These results are in line with the findings of Mortensen et al., 2015, who described that one of the main variables related to HPV knowledge and vaccine acceptability is parent gender.Citation27 Nevertheless, it is important to mention that the percentage of fathers who answered the KAPPAS survey was 13.81%, which constitutes a small sample size.
Some of the explanatory factors observed in this study were also considered as significant variables when the correlation with the degree of acceptability of the HPV vaccine was explained or studied in previous works.Citation15,Citation28–30 In our study, some of the most relevant variables for explaining the degree of knowledge of HPV and HPV vaccine acceptability proved to be the degree of knowledge of HPV vaccine and consulting a healthcare source about HPV infection.
Previous research has found that the potential predictors of HPV vaccine acceptability are previous knowledge of HPV,Citation31 and one of the main predictors is advice from healthcare personnel.Citation6 The role of vaccination status (of parent or child) has been also reported in the literature.Citation6,Citation32,Citation33 As our group already found, acceptability of the HPV vaccine is a more complex multifaceted construct reflecting the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or previous responses to the intervention.Citation13 Providing the population with evidence-based scientific data is beneficial and crucial, although it does not necessarily lead individuals to understand or interpret such information correctly.Citation34 Although poor health literacy is regarded as a cause of vaccine hesitancy, it is rarely considered when this subject is discussed. The association between health literacy skills and vaccine acceptability has been shown to be uneven when general measures are used, and also depends on population characteristics and the type of vaccine in question. Vaccine literacy has been constructed upon the same idea of health literacy, although very few specific measuring tools have been developed hitherto. More of these instruments need to be validated and used extensively with the ultimate aim of assessing vaccine literacy skills and defining interventions geared toward improving them.Citation35
With regard to HPV-related information, and in line with the findings reported in the literature,Citation36 our results showed that the degree of knowledge of HPV and the acceptability of the HPV vaccine tended to increase slightly as the number of sources consulted increased.
Healthcare sources of information (pediatrician, gynecologist, family doctor, etc.) played an important role in providing precise and accurate information about HPV and its vaccine, according to our results. Parents tended to be more aware of HPV- and HPV vaccine-related questions, and their acceptability was higher if they consulted a healthcare source, particularly if it was a pediatrician or a gynecologist. In Spain, pediatricians play a very relevant role in providing advice and recommendations about vaccine in children. On the other hand, gynecologists have traditionally been involved in managing HPV-related diseases, and relevant scientific societies in this field recommend individual-based HPV vaccine recommendation.
Our results underline the need to encourage other groups of healthcare professionals (HCPs) besides pediatricians or gynecologists, such as nurses, urologists and specialists in sexually transmitted diseases, to contribute and to join forces in raising awareness of HPV and the benefits of vaccinating against it, among the population at large. Facilitating HCP-initiated discussions and providing clear information about HPV vaccines is key to increasing vaccine acceptability among boys as well.Citation26 Johnson et al. reported that providing a recommendation for vaccination was the strongest predictor of vaccination in both genders.Citation37
The Internet also plays a very important role in conveying information about HPV and HPV vaccine. It was one of the most common sources of information and was associated with greater knowledge, although this did not translate into higher HPV vaccine acceptability. These findings were similar to those reported by McRee et al.Citation38 These results highlight the importance of the specific online sources consulted, since Moran et al. emphasized that anti-vaccine websites contain a considerable amount of misinformation.Citation33 In this regard, targeted, balanced and high-quality information should be provided to the relevant population through the appropriate channels that help to improve the acceptability of HPV vaccination and to achieve the goal of eliminating HPV-related diseases.
Given the changing situation toward HPV GNV programs, coordinated efforts should be made to provide balanced information for evidence-based decision-making about HPV vaccination, as it has also been reinforced through studies in other European countries.Citation15,Citation38 These efforts should focus on raising awareness about the importance of HPV vaccination, not only in girls but also on scaling up to the male population. Currently, there is solid evidence about the role of HPV in other diseases besides cervical cancer: genital warts, precancerous lesions and anal, penile and oropharyngeal cancersCitation39 Implementing GNV programs seeks not only to protect the male population from the burden of HPV, but also to contribute to extend herd protection to unvaccinated women and also mitigate the impact of an unexpected potential reduction in coverage.Citation40 Therefore, HPV vaccination in both genders would contribute to the resilience of the vaccination programs, which is key to reach the elimination of HPV-related diseases.Citation39,Citation40 In addition, training HCPs and improving the quality of the information available on the Internet or alternative channels are key to increasing HPV vaccine uptake.
Some limitations derived from the nature of this study should be considered. Firstly, parent-reported information is subjective and may be affected by social desirability, inaccuracy or mistakes. In addition, multiple testing can lead to spurious relationships showing statistically significant results. Nevertheless, the high consistency of results among bivariate and multivariate statistical analysis is a proof of its robustness. It also should be remembered that individual healthcare professional attitudes may influence parents’ perceptions in terms of knowledge of HPV and acceptability of HPV vaccine. In addition, some predictor factors of HPV vaccine knowledge and acceptability could be missing in the survey. However, this risk is very limited, due to the performance of a previous systematic literature review that was used for the development of the survey. In addition, some factors like income level of families, can be extrapolated by the answers provided to other questions such as employment status and level of studies.
In conclusion, HPV infection and vaccine awareness and acceptability are strongly associated with child gender and age, which correlates with the current NIP in Spain, where only 12-year-old girls are targeted. Our study highlights the role of HCPs as a source of information, meaning that parents who had learnt about the HPV vaccine when consulting a healthcare source had greater HPV and HPV vaccine knowledge and acceptability, thereby helping to achieve and maintain high coverage rates and to reach the elimination of HPV-related diseases.
List of abbreviations
Supplemental Material
Download MS Word (1.9 MB)Acknowledgments
Investigators of the KAPPAS study: Magdalena Aga (CS Repélega); Inés Cabeza (CS de Galdakao); Isabel Cañabate (CS Churriana); Patricia Company (CS el Pla-Elx); Cynthia Crespo (CAP Montclar); Auxiliadora Fernandez (IHP Sevilla); Mara Garcés (CS Nazaret); Gema Belén López (IHP Córdoba); Josep Mares (Mares Riera); María Martín (CS La Cala de Mijas); Reyes Mazas (CS de Gama); Ana María Nocea (CS Condes de Barcelona); Lizeth Peña (CS Pla Vinalopó); Victoria Planelles (CS Paiporta); Elena Taborga (CS Villalegre); Isabel Úbeda (CS L’Eliana). Editorial assistance and medical writing support were provided by Esther Tapia, PhD and Adelphi Targis, SL.
Disclosure statement
NL, AJR, MC are full-time employees of MSD Spain. ISdlC has received grants and/or honoraria as a consultant/advisor or attending conferences and practical courses from GlaxoSmithKline, Sanofi Pasteur, MSD and Pfizer. EV, ESV, AS, AL and MPS have received honoraria from MSD as an investigator for this study. MGS has received honoraria from MSD as an investigator for this study and honoraria from MSD Spain and GlaxoSmithKline outside the submitted work.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.2024065
Additional information
Funding
References
- Weaver BA. Epidemiology and natural history of genital human papillomavirus infection. J Am Osteopath Assoc. 2006;106:S2–11.
- Bosch FX, Broker TR, Forman D, Moscicki AB, Gillison ML, Doorbar J, Stern PL, Stanley M, Arbyn M, Poljak M, et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine. 2013;31(Suppl 7):H1–31. doi:10.1016/j.vaccine.2013.10.003.
- Schiffman M, Doorbar J, Wentzensen N, de Sanjose S, Fakhry C, Monk BJ, Stanley MA, Franceschi S. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers. 2016;2:16086. doi:10.1038/nrdp.2016.86.
- Asociación Española de Pediatría. Calendario de vacunaciones de la AEP. Razones y bases de las recomendaciones 2021. [accessed 2021 Apr 7]. https://vacunasaep.org/sites/vacunasaep.org/files/cav-aep_calendario-2021_v.2_01ene2021.pdf .
- Ministerio de Sanidad Servicios Sociales e Igualdad. Revisión del calendario de vacunación 2016. [accessed 2021 22 March]. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/docs/Revision_CalendarioVacunacion.pdf
- Alvarez Garcia FJ, Cilleruelo Ortega MJ, Alvarez Aldean J, Garces-Sanchez M, Garcia Sanchez N, Garrote Llanos E, Merino ÁH, de Arce AI, Melián AM, Gómez ML, et al. Immunisation schedule of the Spanish Association of Paediatrics: 2020 recommendations. An Pediatr (Barc). 2020;92(1):52 e51–52 e10.
- Navarro-Illana P, Navarro-Illana E, Vila-Candel R, Diez-Domingo J. Drivers for human papillomavirus vaccination in Valencia (Spain). Gac Sanit. 2018;32(5):454–58. doi:10.1016/j.gaceta.2017.05.008.
- Navarro-Illana P, Caballero P, Tuells J, Puig-Barbera J, Diez-Domingo J. Acceptability of human papillomavirus vaccine in mothers from Valencia (Spain). An Pediatr (Barc). 2015;83(5):318–27. doi:10.1016/j.anpedi.2014.11.018.
- Caballero-Perez P, Tuells J, Rementeria J, Nolasco A, Navarro-Lopez V, Aristegui J. Acceptability of the HPV vaccine among Spanish university students in the pre-vaccine era: a cross-sectional study. Rev Esp Quimioter. 2015;28:21–28.
- Lopez N, Garces, M, Panizo M, Salamanca De la Cueva I, Cotarelo M. Parental knowledge of HPV and vaccine acceptability in Spain: results from KAPPAS survey EUROGIN Congress 2021 Abstract #1714 35; Toronto, Canada.
- Bonanni P, Faivre P, Lopalco PL, Joura EA, Bergroth T, Varga S, Gemayel N, Drury R. The status of human papillomavirus vaccination recommendation, funding, and coverage in WHO Europe countries (2018-2019). Expert Rev Vaccines. 2020;19(11):1073–83. doi:10.1080/14760584.2020.1858057.
- Bruni L, Saura-Lazaro A, Montoliu A, Brotons M, Alemany L, Diallo MS, Afsar OZ, LaMontagne DS, Mosina L, Contreras M, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev Med. 2021;144:106399. doi:10.1016/j.ypmed.2020.106399.
- Lopez N, Garces-Sanchez M, Panizo MB, de la Cueva IS, Artes MT, Ramos B, Cotarelo M. HPV knowledge and vaccine acceptance among European adolescents and their parents: a systematic literature review. Public Health Rev. 2020;41:10. doi:10.1186/s40985-020-00126-5.
- Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: a systematic review. Prev Med. 2017;95:26–37. doi:10.1016/j.ypmed.2016.11.019.
- Loke AY, Kwan ML, Wong YT, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8(4):349–62. doi:10.1177/2150131917742299.
- Sitaresmi MN, Rozanti NM, Simangunsong LB, Wahab A. Improvement of Parent’s awareness, knowledge, perception, and acceptability of human papillomavirus vaccination after a structured-educational intervention. BMC Public Health. 2020;20(1):1836. doi:10.1186/s12889-020-09962-1.
- Allen JD, Othus MK, Shelton RC, Li Y, Norman N, Tom L, Del Carmen MG. Parental decision making about the HPV vaccine. Cancer Epidemiol Biomarkers Prev. 2010;19(9):2187–98. doi:10.1158/1055-9965.EPI-10-0217.
- Krawczyk A, Perez S, King L, Vivion M, Dube E, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: II. Qualitative results. Hum Vaccin Immunother. 2015;11(2):330–36. doi:10.4161/21645515.2014.980708.
- Krawczyk A, Knauper B, Gilca V, Dube E, Perez S, Joyal-Desmarais K, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: i. Quantitative results. Hum Vaccin Immunother. 2015;11(2):322–29. doi:10.1080/21645515.2014.1004030.
- Trim K, Nagji N, Elit L, Roy KPK. Attitudes, and behaviours towards human papillomavirus vaccination for their children: a systematic review from 2001 to 2011. Obstet Gynecol Int. 2012;2012:921236. doi:10.1155/2012/921236.
- Larson HJ. A call to arms: helping family, friends and communities navigate the COVID-19 infodemic. Nat Rev Immunol. 2020;20(8):449–50. doi:10.1038/s41577-020-0380-8.
- Horton RO. Managing the COVID-19 vaccine infodemic. Lancet. 2020;396(10261):1474. doi:10.1016/S0140-6736(20)32315-1.
- UNICEF. Vaccine misinformation management field guide. 2020 [accessed 2021 Jun 10]. https://www.unicef.org/mena/reports/vaccine-misinformation-management-field-guide .
- Underwood NL, Gargano LM, Jacobs S, Seib K, Morfaw C, Murray D, Hughes JM, Sales JM. Influence of sources of information and parental attitudes on human papillomavirus vaccine uptake among adolescents. J Pediatr Adolesc Gynecol. 2016;29(6):617–22. doi:10.1016/j.jpag.2016.05.003.
- Lai D, Bodson J, Davis FA, Lee D, Tavake-Pasi F, Napia E, Villalta J, Mukundente V, Mooney R, Coulter H, et al. Diverse families’ experiences with HPV vaccine information sources: a community-based participatory approach. J Community Health. 2017;42(2):400–12. doi:10.1007/s10900-016-0269-4.
- Lacombe-Duncan A, Newman PA, Baiden P. Human papillomavirus vaccine acceptability and decision-making among adolescent boys and parents: a meta-ethnography of qualitative studies. Vaccine. 2018;36(19):2545–58. doi:10.1016/j.vaccine.2018.02.079.
- Mortensen G AM L, Idtaleb L. Parental attitudes towards male human papillomavirus vaccination: a pan-European cross-sectional survey infectious disease epidemiology. BMC Public Health. 2015;15:1–10. doi:10.1186/s12889-015-1863-6.
- Friedman AL. SHEtk, attitudes, beliefs, and communication preferences of the general public regarding HPV: findings from CDC focus group research and implications for practice. Heal Educ Behav. 2007;22:1–15. doi:10.1177/1090198106292022.
- Brabin L, Roberts SA, Farzaneh F, Kitchener HC. Future acceptance of adolescent human papillomavirus vaccination: a survey of parental attitudes. Vaccine. 2006;24(16):3087–94. doi:10.1016/j.vaccine.2006.01.048.
- Olshen E, Woods ER, Austin SB, Luskin M, Bauchner H. Parental acceptance of the human papillomavirus vaccine. J Adolesc Health. 2005;37(3):248–51. doi:10.1016/j.jadohealth.2005.05.016.
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–14. doi:10.1016/j.ypmed.2007.05.013.
- Grandahl M, Tyden T, Westerling R, Neveus T, Rosenblad A, Hedin E, Oscarsson M. To consent or decline HPV vaccination: a pilot study at the start of the national school-based vaccination program in Sweden. J Sch Health. 2017;87(1):62–70. doi:10.1111/josh.12470.
- Lm MMB, Everhart K, Morgan A, Prickett E. What makes anti-vaccine websites persuasive? A content analysis of techniques used by anti-vaccine websites to engender anti-vaccine sentiment. J Commun Healthc. 2016;2:151–63. doi:10.1080/17538068.2016.1235531.
- Biasio LR, Bonaccorsi G, Lorini C, Pecorelli S. Assessing COVID-19 vaccine literacy: a preliminary online survey. Hum Vaccin Immunother. 2021;17(5):1304–12. doi:10.1080/21645515.2020.1829315.
- Biasio LR. Vaccine literacy is undervalued. Hum Vaccin Immunother. 2019;15(11):2552–53. doi:10.1080/21645515.2019.1609850.
- Giambi C, D’Ancona F, Del Manso M, De Mei B, Giovannelli I, Cattaneo C, Possenti V, Declich S. Exploring reasons for non-vaccination against human papillomavirus in Italy. BMC Infect Dis. 2014;14:545. doi:10.1186/s12879-014-0545-9.
- Lm JKL, Cabral H, Kazis LE, Katz IT. Variation in human papillomavirus vaccine uptake and acceptability between female and male adolescents and their caregivers. J Community Health. 2017;42:522–32. doi:10.1007/s10900-016-0284-5.
- Rp MA-L, Brewer NT. Parents’ Internet use for information about HPV vaccine. Vaccine. 2013;30:3757–62. doi:10.1016/j.vaccine.2011.11.113.
- European Cancer Organisation. Viral protection: achieving the possible. A four step plan for eliminating HPV cancers in Europe. [accessed 2021 Jun 15]. https://www.europeancancer.org/resources/159:viral-protection-achievingthe-possible-a-four-step-plan-for-eliminating-hpv-cancers-in-europe.html
- Elfstrom KM, Lazzarato F, Franceschi S, Dillner J, Baussano I. Human papillomavirus vaccination of boys and extended catch-up vaccination: effects on the resilience of programs. J Infect Dis. 2016;213(2):199–205. doi:10.1093/infdis/jiv368.
