ABSTRACT
Men who have sex with men (MSM) are at high risk of infection with human papillomavirus (HPV). Some countries have incorporated MSM into their HPV vaccination strategies. The acceptance of the HPV vaccine is an important factor affecting vaccine promotion in MSM. This study aims to analyze the factors influencing HPV vaccination willingness among MSM in China. Non-probability sampling was used to recruit MSM in China in June 2021. The information collected included demographic characteristics, HPV knowledge, attitude, behavior, history of sexually transmitted diseases (STDs), and HPV vaccination intention. A structural equation model was used to analyze the data based on the theory of knowledge-attitude-behavior. Among 889 participants, 736 (82.79%) of the MSM were willing to receive the HPV vaccine. The results of the structural equation model showed that knowledge, attitude, behavior, and STD history influenced the vaccination intention, of which knowledge (total effect of .36) and attitude (total effect of .31) had the greatest influence. Since most MSM in China were willing to be vaccinated against HPV, they should be considered for inclusion in the HPV vaccination program. Enhancing HPV awareness and improving risk awareness may be useful in increasing the vaccination willingness of MSM in China.
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted virus worldwide, causing the majority of cervical, oropharyngeal, anal, and vulvar cancers. Research evidence suggests that more than 9000 cases of HPV-related cancers occur in men in the United States annually, accounting for 63% of penile, 91% of anal, and 72% of oropharyngeal cancers.Citation1 HPV-associated oropharyngeal squamous cell cancer is a disease that primarily affects men and has one of the most rapidly rising incidences in high-income countries. The incidence of oropharyngeal squamous cell cancer in men surpassed that of cervical cancer in the UK for the first time in 2016,Citation2 as was the case in the USA in 2015.Citation3 Men who have sex with men (MSM) are at high risk of HPV infection. The overall prevalence of HPV infection is very high among MSM internationally (63.9% in HIV-negative MSM and 92.6% in HIV-infected MSM).Citation4 Numerous studies have reported that MSM have higher oral and anal HPV prevalence than women and heterosexual men.Citation5–7 HPV is far more prevalent among MSM (the prevalence of anal HPV infection is 59.2%), compared with heterosexual men (the overall HPV prevalence is 14.5%) and women (the overall HPV prevalence is 15.6%) in China.Citation6–8 HIV-positive MSM are more likely to be infected with HPV than HIV-negative MSM, and tend to be infected with multiple HPV genotypes.Citation9–11
The HPV vaccine is intended to prevent HPV infection. Three prophylactic HPV vaccines are currently available for the prevention of HPV-related diseases; the 2-valent vaccine is recommended for females, while the 4-valent and 9-valent vaccines are recommended for both males and females.Citation12–15 Several studies have shown that HPV vaccination effectively prevents preventing anal, penile, and oral HPV infection in MSM.Citation16–18 The HPV vaccine is promoted only in women in most countries. Therefore, MSM who do not receive indirect protection from vaccination can only be protected by being vaccinated.Citation19,Citation20 The HPV vaccine is effective even after the first sexual encounter.Citation21,Citation22 Increasing vaccination coverage in the MSM population will ultimately have an important impact on reducing HPV infection in MSM.Citation17,Citation23,Citation24 Therefore, an increasing number of countries, such as Spain, the United Kingdom, the United States, and Australia, are incorporating MSM (aged up to 26 and 45 years in the USA and the UK, respectively) into their HPV vaccination strategies.Citation15,Citation24–26 The HPV vaccine, which was introduced to mainland China in 2016, is promoted only in women. Two types of HPV vaccines (4-valent and 9-valent) are provided to males aged 9 years or more by private physicians in Hong Kong, China.Citation13 However, HPV vaccination rates among MSM are well below the target in some countries where HPV vaccination is recommended for MSM, such as in the USA and France.Citation27,Citation28 The main factors influencing HPV vaccination among MSM include provider recommendation, age, HPV vaccine attitudes, and HPV knowledge.Citation27–30 Therefore, HPV vaccination willingness is an important factor affecting vaccine promotion in MSM,Citation31 and a topic worth studying.
There are few studies on the HPV vaccination willingness of MSM in China. Previous studies on the willingness of women to be vaccinated against HPV showed that 67.25% of women were willing to be vaccinated in China.Citation32 The vaccine acceptance among MSM reported by region varies greatly, ranging from 34.9% to 94.9%.Citation33,Citation34 The factors influencing vaccination willingness mainly include HPV and HPV vaccination knowledge, attitude, sexual behavior, history of sexually transmitted diseases (STDs), and HIV-related services.Citation33–35 HPV knowledge, attitude, and behavior are correlated, but no studies have taken this into account. The knowledge-attitude-behavior (KAB) model is the most commonly used model to explain how individual knowledge and attitudes affect health behavior. It explains that a personʻs knowledge directly affects his/her attitude, and indirectly affects behavior through his/her attitude.Citation36 Therefore, in this study, we applied the KAB model and analyzed the influence of knowledge, attitude, and behavior on HPV vaccination willingness using a structural equation model. The results of this study will be useful in providing recommendations for the future promotion of the HPV vaccine in MSM.
Methods
Subjects and recruitment
In June 2021, MSM were recruited from various cities in China using non-probability sampling. The participants were self-identified gay or bisexual MSM aged 16–45; women and heterosexual men were excluded. In this study, we employed a cross-sectional online survey. Some of the participants were recruited from existing MSM groups (the cohort of “National Science and Technology Major Project 2018ZX10721102-005”), while others were recruited from three nongovernmental organizations (NGOs) through core members of NGOs who were in the existing cohort. Acquired immunodeficiency syndrome (AIDS) voluntary counseling, testing clinic staff and NGOs sent questionnaires to MSM through WeChat. The participants could decide whether to participate in the survey after understanding the purpose, confidentiality, time spent and reward [10 RMB (approximately $1.56)]. The participants had the right to withdraw from the investigation at any time. All of the participantsʻ responses were confidential. This study was approved by the Ethics Committee of Chongqing Medical University (2,019,001).
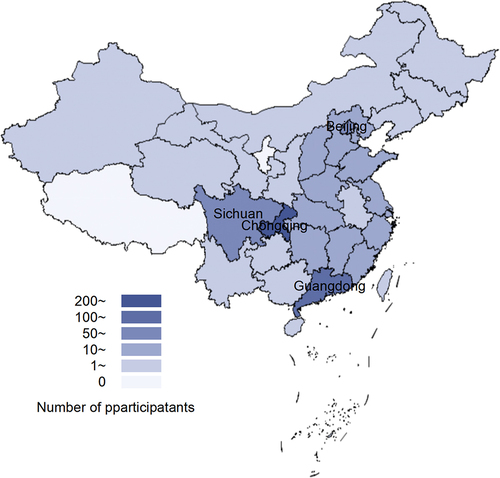
A total of 1,477 participants were recruited. A total of 558 individuals (39.81%) were excluded: those who were of unknown age or older than 45, filled in multiple questionnaires, had problems with logical checks or took less than 2 min to complete the questionnaire (after testing, we assessed that it should have taken participants at least 2 min to complete the questionnaire). The flow chart of the enrollment of participants is shown in The remaining 889 participants met the requirements. The regional distribution of participants was as follows: 283 (31.83%) from Chongqing, 102 (11.471%) from Guangdong, 88 (9.90%) from Sichuan, 65 (7.31%) from Beijing and 351 (39.48%) from 27 other cities. The regional distribution of participants is shown in .
Measurements
The social demographic characteristics included date of birth, household registration, ethnic groups, educational level, employment status, legal marital status (marriage with women), and personal monthly disposable income. Knowledge, attitude and behavior are latent variables that are difficult to measure directly and need to be measured by observed variables. Based on previous literature, 12 observed variables were identified to measure the knowledge of HPV and HPV vaccines.Citation37–39 Attitude was measured using two observed variables: perceived possibility and perceived severity. Seven variables were observed in behavior: the number of male sexual partners, the number of times MSM had sexual intercourse with men, condom use, STD counseling, HIV counseling, STD testing, and HIV testing in the past six months. The initial structural equation model is shown in .
Statistical analysis
Data collation and univariate analysis were performed using SAS version 9.4. Categorical data were described in frequencies and percentages. The chi-squared test was used to compare variables between groups. Mplus version 8.3 (Asparouhov & Muthén, 2019) was used for structural equation modeling and analysis. All the variables used in this study were categorical; thus, a weighted least squares mean and variance adjusted estimator was used to estimate the parameters. The commonly used model-fit indices include the chi-square, comparative fit index (CFI), Tucker-Lewis index (TLI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). The chi-square test is easily affected by other factors (such as degree of freedom and sample size), so this study did not use it as a model fit index. We mainly adopted the suggestions of Hu and Bentle in this study.Citation40 CFI >.95, TLI >.95, SRMR <.08 and RMSEA <.06 indicated that the model was reasonable. The critical values of the model fit index were given by researchers through a simulation study or experience, as there is no consensus on the acceptable levels of these critical values. Therefore, the aforementioned critical values are only for reference.
Results
Sociodemographic characteristics
A total of 889 MSM were eligible for this study. The median age of the participants was 28 years (interquartile range: 23–33), and none of the participants had been vaccinated against HPV. A total of 736 (82.79%) MSM were willing to be vaccinated against HPV. The HPV vaccination willingness varied with education and marital status: MSM with a bachelorʻs degree or higher educational level exhibited the highest willingness (86.21%) to be vaccinated against HPV. Compared with married, divorced or widowed MSM, unmarried MSM were more willing to be vaccinated (84.78%). There was no significant difference in vaccination willingness among MSM of different ages, household registrations, ethnic groups, employment status, and income levels (p > .05) ().
Table 1. Vaccination willingness of MSM with different demographic characteristics (n = 889)
Knowledge, attitude and behavior
The vaccination willingness of MSM with different knowledge, attitudes, behaviors and STD histories is shown in .
Table 2. Vaccination willingness of MSM with different knowledge, attitude, behavior, and STD history (n = 889)
Knowledge of HPV and HPV vaccines
Most MSM had heard of HPV (71.43%), HPV-related diseases (70.98%) and the HPV vaccine (77.95%). MSM who had heard about HPV, HPV-related diseases and the HPV vaccine had a significantly higher willingness to be vaccinated (p < .05). A total of 50.28% of MSM answered incorrectly when presented with the statement “most HPV infections have no visible symptoms.” A total of 40.61% of MSM answered incorrectly when asked if “the HPV vaccine protects against all types of HPV infection;” the MSM who answered incorrectly were more likely to be vaccinated. In terms of other knowledge, the MSM who answered correctly had a higher willingness to be vaccinated than those who answered incorrectly.
Attitude
Only 17.66% of MSM thought they had a high chance of being infected with HPV and 37.80% of MSM thought that HPV posed a great or particularly great threat to them. MSM who thought they were more likely to be infected were more likely to be vaccinated. MSM who perceived a high threat were more willing to be vaccinated than those who perceived a low threat; the difference was statistically significant (p < .05).
Behavior
MSM who had one or more male partners, had sex with men, received STD counseling and testing, or received AIDS counseling and testing within the last six months had higher vaccination willingness. A total of 46.23% of MSM had been tested for STDs. A total of 11.47% of MSM had been diagnosed with STDs in the last sex months. MSM who had been diagnosed with STDs were more likely to be vaccinated. There were significant differences in the aforementioned behaviors between the two groups (p < .05).
Structural equation model
Testing the measurement model
The initial measurement model was tested. The degrees of freedom were 207 (df ≥ 0), which satisfied the t-rule, and the model could be identified. The model fit indices were as follows: CFI = .961, TLI = .957, SRMR = .087, and RMSEA = .068. These model fit indices either reached or were close to the recommended values, making the model acceptable. The factor loading of K12 (whether the HPV vaccine protects against all types of HPV infection) was less than .5, which was lower than the acceptable level; thus, it was deleted. The factor loading of other items was at an acceptable level, and the significance was p < .01.
Structural equation model of HPV vaccination willingness
After deleting the K12 item, the structural equation model of HPV vaccination willingness was constructed. The degrees of freedom were 204 (≥0), which satisfied the t-rule, and the model could be identified. The model-fit indices were as follows: CFI = .959, TLI = .953, SRMR = .084, and RMSEA = .071. The standardized path coefficients of the initial structural equation model of HPV vaccination willingness are shown in . Except for the path from knowledge to behavior, all standardized path coefficients were statistically significant (p < .01). Thus, the model was modified by removing the path from knowledge to behavior.
Table 3. Hypothesis test results (path coefficient) of the initial structural equation model of HPV vaccination willingness
The modified model then fit better, and the improved model fit indices were as follows: CFI = .962, TLI = .957, SRMR = .087, and RMSEA = .068. The standardized path coefficients are shown in The path coefficients of the model were statistically significant (p < .01). A standardized total effect of knowledge on vaccination willingness was .36, with a direct effect of .26 and an indirect effect of .10. A standardized total effect of attitude on vaccination willingness was .31, with a direct effect of .23 and an indirect effect of .08. The direct effect of behavior on vaccination willingness was .17. The direct effect of STD history in the last six months on vaccination willingness was .16.
Discussion
Recommendation of HPV vaccination in MSM
MSM are at high risk of being infected with HPV, as the estimated prevalence of anal HPV among MSM in China is 59.2%.Citation8 However, the HPV vaccine has not been introduced among MSM in China. In 2019, the Chinese National Medical Products Administration approved the first Chinese 2-valent HPV vaccine.Citation41 A previous study in China suggested that the Chinese 2-valent HPV vaccine was more cost-effective for MSM than other imported vaccines.Citation42 In addition, our study showed that 82.79% of MSM were willing to be vaccinated against HPV. This rate was higher than the corresponding rate for women before the HPV vaccine was recommended in China (67.25%) and higher than the international average rate for MSM (50.0%) reported in a 2021 systematic review.Citation32,Citation43 Most MSM would accept to be vaccinated against HPV. Based on the low cost of the Chinese 2-valent HPV vaccine and the high vaccination willingness of MSM, it is important and feasible to include MSM in the HPV vaccine project in China.
Factors influencing HPV vaccination willingness
The structural equation model constructed in this study showed that HPV and HPV vaccine knowledge affected attitude (perceived possibility and perceived threat) and that attitude affected MSM behavior. These results were consistent with the theory of KAB.Citation36 Knowledge, attitude, and behavior influenced the vaccination intention of MSM; knowledge had the greatest impact on inoculation willingness. This was consistent with previous studies, which showed that knowledge has an important impact on vaccination willingness in women, heterosexual men, and MSM.Citation43–45 However, previous studies have not explained exactly how knowledge affects the intent to be vaccinated. The structural equation mode showed that knowledge of HPV and HPV vaccines could help MSM establish correct HPV risk awareness and make them aware of the benefits of HPV vaccination, thereby increasing MSM vaccination willingness. Approximately 30% of the study participants had not heard of HPV prior to being questioned in the context of the present study, thereby indicating a low level of HPV knowledge. HPV-related knowledge can be promoted through the internet, WeChat, social media, and other platforms. At the same time, rigorous fact-checking is necessary as misinformation/disinformation can spread easily through media channels. It is worth noting that a total of 40.61% of MSM thought that the HPV vaccine could prevent all types of HPV infection, and that they were more likely to be vaccinated (87.53%). They had high expectations for the effectiveness of the HPV vaccine. They may be reluctant to get vaccinated after learning that the HPV vaccine only prevents most HPV infections. Therefore, the acceptance of the HPV vaccine in this study may be higher than its true acceptance.
Attitude (perceived possibility and perceived threat) was also an important factor affecting vaccination willingness. MSM with high perceived possibility and high perceived threat were more likely to reduce their risk of HPV infection through vaccination. As mentioned in the protective motivation theory, improving individual awareness in terms of disease severity and susceptibility can enhance individual protective motivation and promote the intention of behavior change.Citation46 When carrying out HPV education, there is a need to emphasize the high incidence and severity of HPV-related diseases to improve the recipientsʻ risk perception.
Behavior affected vaccination intention. MSM with high-risk sexual behavior were more likely to be infected with HPV.Citation47 MSM with high-risk sexual behaviors, including having multiple sexual partners (≥2), having sex with men in the past six months, or not using condoms throughout the course of having sex with other men, were more likely to be vaccinated against HPV. MSM exhibiting high-risk sexual behaviors have a high risk of HPV infection and high acceptance rates of the HPV vaccine; thus, they can be an important target group for HPV vaccination. MSM who underwent STD or HIV counseling and testing were more receptive to the HPV vaccine. This may be because they are exposed to STDs and have a higher risk of infection. It is difficult to reach MSM groups effectively. Hence, bundling HPV vaccination with services related to MSM, such as STDs and HIV counseling and testing, may increase the vaccination rates.
Limitations
The present findings should be interpreted with caution, owing to several limitations. First, convenience sampling was used in this study. We used WeChat to send the questionnaires. MSM who were interested in health-related topics were more likely to complete the questionnaire. Therefore, the acceptance of the HPV vaccine in this study may be higher than its true acceptance, and our results are representative of the MSM population status to a certain extent. Second, we included sensitive topics in this study (such as the number of sexual partners, sexual behaviors, and STD history), which may lead to report bias; hence, participants may not truthfully report this sensitive information. Third, this study did not ask MSM if they found the price of the HPV vaccine to be acceptable or from which institution or organization they would like to be vaccinated against HPV. If the HPV vaccine is to be provided to MSM in the future, the price and the method of access may be important factors affecting the actual vaccination rate of MSM.Citation33,Citation35,Citation48 Therefore, before making the HPV vaccine available to MSM, we need to study the influence of the HPV vaccine price and acquisition method on the acceptance of the vaccine by MSM.
Conclusion
MSM are at high risk of being infected with HPV. In this study, most MSM were willing to be vaccinated against HPV. Therefore, MSM should be considered for inclusion in the HPV vaccination program in China. Knowledge and attitude are important factors influencing the willingness of HPV vaccination in MSM. We should focus on promoting HPV and HPV vaccine knowledge and increasing risk perception to increase vaccination willingness among MSM. HPV vaccination can be bundled with MSM-related services (such as STD counseling and testing) to increase vaccination rates.
Supplemental Material
Download MS Word (17.1 KB)Acknowledgments
The authors would like to express their gratitude to all the participants for their engagement in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available on request from the corresponding authors. The data are not publicly available as they contain sensitive personal behaviors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2038504
Additional information
Funding
References
- Han JJ, Beltran TH, Song JW, Klaric J, Choi YS. Prevalence of genital human papillomavirus infection and human papillomavirus vaccination rates among US adult men: National Health and Nutrition Examination Survey (NHANES) 2013-2014. Jama Oncol. 2017;3(6):810–9. doi:10.1001/jamaoncol.2016.6192.
- Office for National Statistics. Cancer registration statistics, England: first release. 2016. [accessed 2021 Nov 19]. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancerregistrationstatisticsengland/2016
- Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus–Associated cancers — United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2018;67(33):918–24. doi:10.15585/mmwr.mm6733a2.
- Machalek DA, Poynten M, Jin F, Fairley CK, Farnsworth A, Garland SM, Hillman RJ, Petoumenos K, Roberts J, Tabrizi SN, et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol. 2012;13(5):487–500. doi:10.1016/S1470-2045(12)70080-3.
- Sonawane K, Suk R, Chiao EY, Chhatwal J, Qiu P, Wilkin T, Nyitray AG, Sikora AG, Deshmukh AA. Oral human papillomavirus infection: differences in prevalence between sexes and concordance with genital human papilloma virus infection, NHANES 2011 to 2014. Ann Intern Med. 2017;167(10):714–24. doi:10.7326/M17-1363.
- Marra E, Lin C, Clifford GM. Type-Specific anal human papillomavirus prevalence among men, according to sexual preference and HIV status: a systematic literature review and meta-analysis. J Infect Dis. 2019;219(4):590–98. doi:10.1093/infdis/jiy556.
- Ma X, Wang Q, Ong JJ, Fairley CK, Su S, Peng P, Jing J, Wang L, Soe NN, Cheng F, et al. Prevalence of human papillomavirus by geographical regions, sexual orientation and HIV status in China: a systematic review and meta-analysis. Sex Transm Infect. 2018;94(6):434–42. doi:10.1136/sextrans-2017-053412.
- Zhou Y, Lin Y, Gao L, Dai J, Luo G, Li L, Yuan T, Li P, Zhan Y, Gao Y, et al. Human papillomavirus prevalence among men who have sex with men in China: a systematic review and meta-analysis. Eur J Clin Microbiol. 2021;40(7):1357–67. doi:10.1007/s10096-021-04229-y.
- Li X, Li M, Yang Y, Zhong X, Feng B, Xin H, Li Z, Jin Q, Gao L. Anal HPV/HIV co-infection among men who have sex with men: a cross-sectional survey from three cities in China. Sci Rep-Uk. 2016:6. doi:10.1038/srep21368.
- Ming G, Yong-Hong L, Ling-Hua L, Xi-Zi D, Yuan N, Feng L, Feng-Yu H. Prevalence of anal HPV infection among HIV-positive men who have sex with men. J Trop Med. 2019;19:785–88.
- Beliakov I, Senina M, Tyulenev Y, Novoselova E, Surovtsev V, Guschin A. The prevalence of high carcinogenic risk of HPV genotypes among HIV-positive and HIV-negative MSM from Russia. Can J Infect Dis Med Microbiol. 2021;2021:1–6. doi:10.1155/2021/6641888.
- World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017. Wkly Epidemiol Rec. 2017;92:241–68.
- Centre for Health Protection. Consensus statement on the use of human papillomavirus (HPV) vaccine in prevention of cervical cancer. [ accessed 2021 Nov 19]. https://www.chp.gov.hk/files/pdf/consensus_statement_on_the_use_of_hpv_vaccine_in_prevention_of_cervical_cancer.pdf
- Chow EPF, Carter A, Vickers T, Fairley CK, McNulty A, Guy RJ, Regan DG, Grulich AE, Callander D, and Khawar L, et al. Effect on genital warts in Australian female and heterosexual male individuals after introduction of the national human papillomavirus gender-neutral vaccination programme: an analysis of national sentinel surveillance data from 2004–18. Lancet Infect Dis. 2021;10(1016/S1473–3099(21)00071–2):1-13.
- Petrosky E, Bocchini JJA, Hariri S, Chesson H, Curtis CR, Saraiya M, Unger ER, Markowitz LE. Use of 9-Valent Human Papillomavirus (HPV) Vaccine: Updated HPV Vaccination Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2015;64:300–04
- Goldstone SE, Giuliano AR, Palefsky JM, Lazcano-Ponce E, Penny ME, Cabello RE, Moreira ED, Baraldi E, Jessen H, and Ferenczy A, et al. Efficacy, immunogenicity, and safety of a quadrivalent HPV vaccine in men: results of an open-label, long-term extension of a randomised, placebo-controlled, phase 3 trial. Lancet Infect Dis. 2021:1-13. doi:10.1016/S1473-3099(21)00327-3.
- Chow EPF, Tabrizi SN, Fairley CK, Wigan R, Machalek DA, Garland SM, Cornall AM, Atchison S, Hocking JS, Bradshaw CS, et al. Prevalence of human papillomavirus in young men who have sex with men after the implementation of gender-neutral HPV vaccination: a repeated cross-sectional study. Lancet Infect Dis. 2021;21:1448–57. doi:10.1016/S1473-3099(20)30687-3.
- Winer R, Lin J, Querec T, Unger E, Stern J, Rudd J, Golden M, Swanson F, Markowitz L, Meites EJTJ. Effectiveness of human papillomavirus (HPV) vaccination against Penile Hpv infection in men who have sex with men and transgender women. 2021. doi:10.1093/infdis/jiab390.
- Díez-Domingo J, Sánchez-Alonso V, Villanueva R, Acedo L, Tuells J. Impact of a gender-neutral HPV vaccination program in men who have sex with men (MSM). Int J Env Res Pub He. 2021;18(3):963. doi:10.3390/ijerph18030963.
- Ali H, Donovan B, Wand H, Read TRH, Regan DG, Grulich AE, Fairley CK, Guy RJ. Genital warts in young Australians five years into national human papillomavirus vaccination programme: national surveillance data. Bmj. 2013;346:f2032. doi:10.1136/bmj.f2032.
- Tota JE, Giuliano AR, Goldstone SE, Brady D, Alfred S, Alain L, Christine V, and Palefsky JM. Anogenital HPV infection, Seroprevalence, and risk factors for HPV seropositivity among sexually active men enrolled in a Global HPV vaccine trial. Clin Infect Dis. 2021.
- Bogaards JA, Mooij SH, Xiridou M, Schim Van Der Loeff MF, de Sanjosé S. Potential effectiveness of prophylactic HPV immunization for men who have sex with men in the Netherlands: A multi-model approach. PLoS Med. 2019;16(3):e1002756. doi:10.1371/journal.pmed.1002756.
- Goldstein ND, LeVasseur MT, Tran NK, Purtle J, Welles SL, Eppes SC. Modeling HPV vaccination scale-up among urban young men who have sex with men in the context of HIV. Vaccine. 2019;37:3883–91. doi:10.1016/j.vaccine.2019.05.047.
- Martinez-Gomez X, Curran A, Campins M, Alemany L, Rodrigo-Pendas JA, Borruel N, Castellsague X, Diaz-de-Heredia C, Moraga-Llop FA, Del PM, et al. Multidisciplinary, evidence-based consensus guidelines for human papillomavirus (HPV) vaccination in high-risk populations, Spain, 2016. Euro Surveill. 2019;24(7):24. doi:10.2807/1560-7917.ES.2019.24.7.1700857.
- Kirby T. MSM in England to be offered free HPV vaccination. Lancet Oncol. 2018;19:e148. doi:10.1016/S1470-2045(18)30158-X.
- Chow EPF, Danielewski JA, Murray GL, Fehler G, Chen MY, Bradshaw CS, Garland SM, Fairley CK. Anal human papillomavirus infections in young unvaccinated men who have sex with men attending a sexual health clinic for HPV vaccination in Melbourne, Australia. Vaccine. 2019;37:6271–75. doi:10.1016/j.vaccine.2019.08.066.
- Loretan C, Chamberlain AT, Sanchez T, Zlotorzynska M, Jones J. Trends and characteristics associated with human papillomavirus vaccination uptake among men who have sex with men in the United States, 2014–2017. Sex Transm Dis. 2019;46(7):465–73. doi:10.1097/OLQ.0000000000001008.
- Petit B, Epaulard O. Men having sex with men and the HPV vaccine in France: A low vaccine coverage that may be due to its infrequent proposal by physicians. Vaccine. 2020;38:2160–65. doi:10.1016/j.vaccine.2020.01.049.
- Gerend MA, Madkins K, Phillips G, Mustanski B. Predictors of human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2016;43(3):185–91. doi:10.1097/OLQ.0000000000000408.
- Cummings T, Kasting ML, Rosenberger JG, Rosenthal SL, Zimet GD, Stupiansky NW. Catching up or missing out? Human papillomavirus vaccine acceptability among 18- to 26-year-old men who have sex with men in a US National sample. Sex Transm Dis. 2015;42(11):601–06. doi:10.1097/OLQ.0000000000000358.
- Huachun Z, Lin Z, Puifung CE, Lei Z. [Teenage men who have sex with men should be vaccinated against human papillomavirus infection]. Chin J Epidemiol. 2014;35:1072–73.
- Zhang Y, Wang Y, Liu L, Fan Y, Liu Z, Wang Y, Nie S. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. Bmc Public Health. 2016:16. doi:10.1186/s12889-016-2873-8.
- Tian T, Wang D, Papamichael C, Yan Z, Guoyao S, Zhanlin Z, Mahan Y, Xiaoqing T, Zheng G, Jianghong D. HPV vaccination acceptability among men who have sex with men in Urumqi, China. Hum Vaccin Immunother. 2019;15(4):1005–12. doi:10.1080/21645515.2018.1520591.
- Zou H, Meng X, Jia T, Zhu C, Chen X, Li X, Xu J, Ma W, Zhang X. Awareness and acceptance of human papillomavirus (HPV) vaccination among males attending a major sexual health clinic in Wuxi, China: A cross-sectional study. Hum Vacc Immunother. 2016;12:1551–59.
- Nadarzynski T, Smith H, Richardson D, Bremner S, Llewellyn C. Men who have sex with men who do not access sexual health clinics nor disclose sexual orientation are unlikely to receive the HPV vaccine in the UK. Vaccine. 2018;36:5065–70. doi:10.1016/j.vaccine.2018.06.075.
- Jingheng H. Health education, 5th ed. Chongqing, China: Fudan University Press; 2011.
- Li J, Kang L, Li B, Pang Y, Huang R, Qiao Y. Effect of a group educational intervention on rural Chinese womenʻs knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines. Bmc Cancer. 2015:15. doi:10.1186/s12885-015-1682-2.
- Zhang S, Pan X, Wang S, Yang C, Gao X, Wang Z, Li M, Ren Z, Zheng Q, Ma W et al. Knowledge of human papillomavirus vaccination and related factors among parents of young adolescents: a nationwide survey in China. Ann Epidemiol. 2015;25(4):231–35. doi:10.1016/j.annepidem.2014.12.009.
- Chang IJ, Huang R, He W, Zhang SK, Wang SM, Zhao FH, Smith JS, Qiao YL. Effect of an educational intervention on HPV knowledge and vaccine attitudes among urban employed women and female undergraduate students in China: a cross-sectional study. Bmc Public Health. 2013;13(1):916. doi:10.1186/1471-2458-13-916.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6.
- National Medical Products Administration. The first domestic recombinant human papillomavirus vaccine has been licensed. [accessed 2022 Jan 7]. https://www.nmpa.gov.cn/directory/web/nmpa/yaowen/ypjgyw/20191231160701608.html
- Ye Z, Liu Z, Cui S, Chu Z, Jiang Y, Xu J, Hu Q, Shang H. High human papilloma virus vaccine acceptability and cost-effectiveness of the Chinese 2-Valent vaccine among men who have sex with men: a cross-sectional study in Shenyang, China. Front Med. 2021:8. doi:10.3389/fmed.2021.763564.
- Zhao Y, Xin X, Deng H, Xu J, Weng W, Zhang M, Li J, Gao Y, Huang X, Liu C. Improving the acceptability of human papillomavirus vaccines among men who have sex with men according to the associated factors: a systematic review and meta-analysis. Front Pharmacol. 2021:12. doi:10.3389/fphar.2021.600273.
- Sallam M, Al-Mahzoum K, Eid H, Assaf AM, Abdaljaleel M, Al-Abbadi M, Mahafzah A. Attitude towards HPV vaccination and the intention to get vaccinated among female university students in health schools in Jordan. Vaccines. 2021;9:1432. doi:10.3390/vaccines9121432.
- Hu S, Xu X, Zhang Y, Liu Y, Yang C, Wang Y, Wang Y, Yu Y, Hong Y, Zhang X et al. A nationwide post-marketing survey of knowledge, attitude and practice toward human papillomavirus vaccine in general population: Implications for vaccine roll-out in mainland China. Vaccine. 2021;39:35–44. doi:10.1016/j.vaccine.2020.11.029.
- Lin D, Fang X, and Li X. Review of health behavior change theory. Psychol Dev Educ. 2005;04:122–27.
- Zhou Y, Lin Y, Meng X, Duan Q, Wang Z, Yang B, Zheng H, Li P, Li M, Lu Y et al. Anal human papillomavirus among men who have sex with men in three metropolitan cities in southern China: implications for HPV vaccination. Vaccine. 2020;38:2849–58. doi:10.1016/j.vaccine.2020.02.009.
- Nadarzynski T, Smith H, Richardson D, Pollard A, Llewellyn C. Perceptions of HPV and attitudes towards HPV vaccination amongst men who have sex with men: A qualitative analysis. Brit J Health Psych. 2017;22(2):345–61. doi:10.1111/bjhp.12233.