ABSTRACT
Given increased global concern about vaccine hesitancy, this study estimates coverage of mandatory vs non-mandatory vaccines in children, and assesses whether vaccine hesitancy among young parents relates to their childʻs eventual vaccination status in Shanghai, China. In a cohort study within Shanghai, China, we ascertained vaccine hesitancy among parents of young infants, and later abstracted their childʻs electronic immunization records. We measure full coverage of vaccines on the mandatory, and publicly funded Expanded Program on Immunization (EPI). Non-EPI vaccines included pneumococcal conjugate vaccine, Haemophilus influenzae type b vaccine, and rotavirus vaccine. Vaccine hesitancy was linked to vaccine uptake through mixed effects logistic regression models. Among 972 children, full coverage of all EPI vaccines by 15 months was 95%, compared to dose 1 coverage of pneumococcal conjugate vaccine at 13%, Haemophilus influenzae type b vaccine at 68%, and rotavirus vaccine at 52%. Vaccine hesitancy was not significantly linked with full coverage of all EPI vaccines (OR: 1.55, 95% CI: .89, 2.72), but coverage in the vaccine hesitant was lower for pneumococcal conjugate vaccine dose 1 (OR: .70, 95% CI: .53, .91), and rotavirus vaccine dose 1 (OR: .69, 95% CI: .56, .86). Disparities by education level were not significant for EPI vaccines, but were for dose 1 of pneumococcal conjugate vaccine rotavirus vaccine. Overall, vaccine hesitancy was related to lower uptake of non-EPI, but not EPI vaccines. Shanghai has a robust system for insurance equitable access to EPI vaccines, but if vaccine hesitancy grows, it could reduce coverage of non-EPI vaccines.
Introduction
Uptake of vaccines that protect against many deadly childhood infectious diseases has been dramatically increased since the establishment of the Expanded Programme on Immunization (EPI) by the WHO in 1974.Citation1 Thanks to the program, global coverage of some EPI vaccines, such as the measles vaccine, polio vaccine, and diphtheria-tetanus-pertussis vaccine (DTP) has reached 80%, resulting in a significant reduction in deaths and hospitalization from measles and neonatal tetanus.Citation2 Despite this success, gaps in vaccination still exist. In 2019, 13.8 million children worldwide did not receive the first dose of DTP, and the number of unvaccinated children has remained stubbornly high in Africa and the Western Pacific regions.Citation2
In recent years, the WHO has added in recommendations for the EPI to include vaccines to protect against other diseases, such as pneumonia, diarrhea, and human papillomavirus.Citation3 Globally, two of the leading causes of death in children under 5 years are pneumonia and diarrhea, which can be prevented in part by relatively new vaccines like the pneumococcal conjugate vaccine (PCV), Haemophilus influenzae type b vaccine (Hib), or rotavirus vaccine (RVV). Worldwide coverage of these vaccines varies but is relatively low.Citation2 For example, in China, PCV, Hib, and RVV are not included in the publicly funded EPI program but require self-payment,Citation4 and, in contrast to EPI vaccines, are not mandatory for school entry, leading to low uptake.Citation5
The burden of disease that could be prevented by these vaccines is significant in China. The WHO estimates that China accounts for 12% of worldwide cases of invasive pneumococcal disease (IPD), and 14% of Hib cases.Citation6,Citation7 It is estimated that 30,000 children <5 years of age in China die from IPD in China each year.Citation6 Additionally, about one-fourth to one-third of the pneumonia cases might be caused by Hib.Citation8 Rotavirus is a significant cause of severe and mild diarrheal disease in Chinese children, and may cause around 40% and 30% of diarrhea-related hospitalizations and outpatient visits among children <5 years of age in China.Citation9
In the absence of a mandatory and publicly funded vaccination program, an individual familyʻs decision on whether or not to obtain a non-EPI vaccine is dependent on many factors, including availability, cost of the vaccine, and perception of vaccine benefits.Citation10 Parents may also have hesitancy or concerns about vaccines in general.Citation11,Citation12 The WHO defines vaccine hesitancy as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services.”Citation12 The definition of vaccine hesitancy is in flux and could also be considered to include concepts of complacency or confidence in vaccination services.Citation13 A previous study in China found that many parents were unwilling to pay for vaccines such as Hib, PCV, and rotavirus vaccine,Citation14 but it is unclear how vaccine hesitancy could play into these decisions. In China, EPI vaccines are mandatory for school entry, with very strict oversight over any vaccine waiver. Although mandating vaccinations could prove to be successful interventions to increase vaccine uptake,Citation15 the effect of vaccine hesitancy on receipt of non-mandatory, non-EPI vaccines are still unclear. In addition, urbanicity has been found associated with vaccination inequality. Studies found the vaccination coverage in several provinces of China was lower in urban areas and in migrant children compared to rural areas and local children.Citation16,Citation17 However, few studies have occurred within a large metropolitan area in China, like Shanghai. The analysis could shed light on the complexities and heterogeneity of vaccination coverage, and ultimately reduce the coverage gap between rural and urban areas in an area expressing rapid urbanization. In a cohort study within Shanghai, China, we ascertained vaccine hesitancy among parents of young infants at baseline,Citation18 and later abstracted their childʻs electronic immunization records. This study aims to estimate coverage of EPI vs non-EPI vaccines in children, and assesses whether vaccine hesitancy among young parents relates with their childʻs eventual vaccination status.
Methods
Study population
This is a cohort study, with baseline survey data collected between May and September 2017, and vaccination status ascertained from electronic immunization records in summer 2020. Details of the survey data collected in 2017 are described elsewhere.Citation18 Forty townships were first selected based on the size of their population according to the 2010 Census. All districts in Shanghai, were eligible except Chongming island, a less-populated island district relatively distant from the city. Within each township, a governmental primary care clinic was randomly selected, and then a convenience sample of parents attending the clinic were selected. Our sample size was based on a desire to estimate prospective relationships between vaccine hesitancy and vaccine uptake. Based on pilot data, we expected a pneumococcal vaccination uptake to be 13.9% and 5.5% in those without and with vaccine hesitancy. With 80% power and an alpha of .05, we would need at least 191 individuals with and without vaccine hesitancy. Given an estimated intra-cluster coefficient of .02389 using pilot data, we would need to enroll at least 647 individuals. The sample size was further inflated to conduct two separate discrete choice experiments in the sample.Citation19,Citation20 The inclusion criteria included being a parent, grandparent, or guardian of an infant ≤3 months, and being ≥18 years old.
Vaccination outcomes
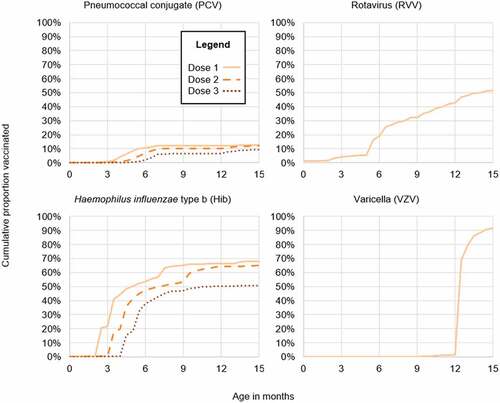
In August 2020, participantsʻ immunization records were abstracted from the Shanghai Immunization Program Information System, which records vaccination information from each community health center in the municipality. We extracted records of the date of administration for a variety of EPI and non-EPI vaccines (see ). We did not include bacillus Calmette-Guérin in the analysis. For this analysis, we focused on vaccinations occurring ≤1 year of age, and so calculated the cumulative incidence of vaccination by 15 months of age (~3 months after 1 year of age) in order to adequately measure vaccinations recommended for administration at 12 months. Additionally, we report two measures of full vaccination. Full coverage of early series vaccines refers to three doses of polio, HepB, and DTP vaccines, because these are vaccines with 3 doses recommended by 6 months of age. We also measure full coverage of all EPI vaccines (the early series plus 2 doses MCV, and 1 dose each of measles, JEV, and VZV). As a standard measurement, we estimated full coverage if all the vaccines in the measure were administered by 15 months. For non-EPI vaccines (PCV, Hib, RVV), we only report dose 1 coverage.
Table 1. Schedule and coverage of vaccines offered to infants ≤12 months a in Shanghai (2017-2020, N=972)
Vaccine hesitancy
There is not a standard measurement for vaccine hesitancy.Citation21 Vaccine hesitancy was measured through a 10-item scale, originally developed the WHO SAGE Working Group on Vaccine Hesitancy.Citation22 The scale was developed through systemic peer-reviewed literatures and tested through global pilot test.Citation22 Descriptive results from the scale are presented elsewhere,Citation18 and in Supplementary Appendix 1. We collapsed the scale into a dichotomous outcome in a previously validated way for a similar scale.Citation23 In brief, the scale contains 10 items, with each item having a 5-point Likert response. We summed the items so that the scale ranged in possibility from 10 to 50, and then dichotomized at 25. Higher numbers represented those vaccine hesitant, and lower numbers those not vaccine hesitant.
Control variables
Other sociodemographic variables are used as control variables in a multivariable analysis, including gender of the child, the relationship of the participant to the child (mother, father, or other), monthly family income, education, and residency. Residency refers to the familyʻs official residency documents. The options include locals (those with an official residency within Shanghai), urban non-locals (those from an urban area outside of Shanghai), and rural non-locals (those from a rural area outside of Shanghai). Individuals with non-local residency may have difficulty obtaining certain social services from the government,Citation24 however, EPI vaccines are offered for free to children regardless of their residency status.
Statistical analysis
We present cumulative incidence curves of several different EPI and non-EPI vaccine series, along with the estimated proportion of children vaccinated by 15 months of age. The all-course coverage of EPI vaccines was calculated by kids who have vaccinated the 3rd dose of polio, 3rd dose of HepB, 3rd dose of DTP, 2nd dose of MCV, measles, and JEV divided by all participants. The relationship between sociodemographic variables and four measures of vaccination coverage (full EPI coverage, PCV1, Hib1, and RVV1) was assessed through a Pearsonʻs chi-square test. Subsequently, we regressed the four measures of vaccination coverage onto vaccine hesitancy, controlling for sociodemographic characteristics. We excluded grandparents from this analysis due to small cell sizes. These models used a mixed effects logistic regression framework, with a random intercept at the township level to account for clustering of the survey sample. We used sampling weights in our analysis. The sampling weights were derived from the inverse probability of selection for each participant given the complex sampling scheme, and make the study population generalizable to the population of parents of young infants in Shanghai. The data were analyzed in SAS version 9.4 (SAS Institute, Cary, NC).
Ethical approval
The study protocol was approved by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (#HUM00125379) and an ethical review committee from the Shanghai Centers for Disease Control and Prevention (#2017–2). Participants gave written informed consistent prior to data collection.
Results
In 2017, 1,188 participants were originally interviewed, and the vaccine records were accessed in 2020 (). Differences between those still in the sample and those lost to follow up (n = 216) are shown in Supplementary Appendix 2. We had a final sample size of 972 (82%). About two-thirds (66%) were mothers of the children, with the rest fathers (30%), or others (4%). About half (54%) were locals, with the remainder being urban non-locals (14%) or rural non-locals (32%).
Table 2. Demographic characteristics of study population, Shanghai, 2017-2020 (N=972)
Cumulative vaccination coverage by 15 months after birth is shown in . The complete series of doses recommended by ≤12 months are over 90% for all EPI vaccines. For example, 99% of children have 3 doses of DTP, 100% 3 doses of polio, and 98% 1 dose of measles. Slightly fewer children, 92%, had 1 dose VZV administered, which was only added to the EPI on 1 August 2018. Full coverage of early series vaccines (3 doses polio, HepB, and DTP) was 98%, and all course coverage of all EPI vaccines was 95%. Voluntary, non-EPI vaccines had lower coverage. The proportion of children at 15 months who had 1 dose of Hib was 68%, 1 dose of PCV was 13% and 1 dose of RVV was 52%.
shows the timing of vaccination uptake for EPI vaccines. In general, there is rapid uptake of vaccines around the time of administration. For example, for polio dose 1, which is recommended at 2 months, uptake of the vaccine is <2% just before 2 months, 90% at 2.5 months, and 96% by the end of the 2nd month. Uptake of non-EPI vaccines is lower and occurs more slowly (). For example, coverage of Hib dose 1, recommended at the same age as polio dose 1, increases from under 1% before the 2nd month to 22% by the end of the 2nd month.
Figure 1. Cumulative proportion of children in Shanghai receiving a vaccine included in the Expanded Program on Immunization, 2017-2020.
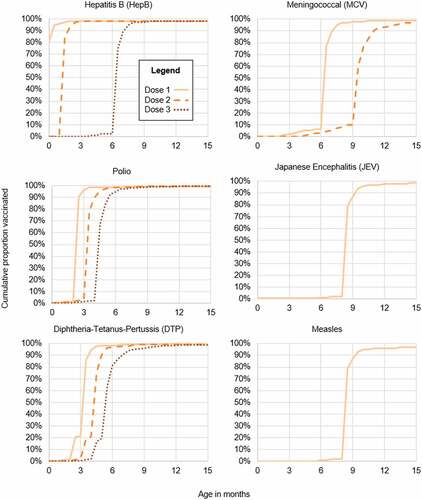
Figure 2. Cumulative proportion of children in Shanghai receiving a vaccine not included in the Expanded Program on Immunization, 2017-2020. VZV was added into the EPI on August 1, 2018.
The vaccination rates of several self-paying vaccines stratified by demographic characteristics were shown in . In regard to full coverage of all EPI vaccines, there were no significant differences by gender of child, relationship of survey participation to child, education status, or residency. For the non-EPI vaccines, there were more disparities by educational status and residency. For example, PCV1 coverage was 20% among those who had a parent with some college or more, versus 3% among those with a high school education (P < .0001), and similarly for Hib1, vaccination coverage was higher for those with some college (71%) vs not (59%) (P = .0182).
Table 3. Relationship of sociodemographic status to coverage of vaccines on and not on the Expanded Program on Immunization (EPI) by 15 months age in Shanghai, China, N=972, 2017-2020
The relationship of vaccine hesitancy to coverage of EPI- and non-EPI vaccines is shown in . Vaccine hesitancy was not significantly linked with full coverage of all EPI vaccines, but coverage in the vaccine hesitant was lower for PCV1 (OR: .66, 95% CI: .50, .88), and RVV1 (OR: .77, 95% CI: .62, .96). Similar to the bivariate analysis, uptake of vaccines was lower among rural non-locals compared to locals for PCV1 and RVV1, but not for EPI vaccines. By education, there was not a difference for full coverage of all EPI vaccines, but those with a college education had 5.16 times higher odds of giving their child PCV1 (95% CI: 3.07, 8.68), and 1.86 times higher odds of giving their child RVV1 (95% CI: 1.45, 2.38).
Table 4. Relationship of vaccine hesitancy to coverage of vaccines on and not on the Expanded Program on Immunization (EPI) by 15 months age in Shanghai, China, N=957, 2017-2020
Discussion
Worldwide, parents may express a range of concerns over what vaccines are recommended or mandated for their children. Few prospective, empirical studies exist that examine the relationship between vaccine hesitancy and actual vaccination status. Our study fills in the gap by relating childrenʻs vaccination records with parentsʻ attitudes toward vaccines shortly after their childʻs birth. Our focus is on understanding if mandating vaccination can reduce disparities and mitigate vaccine hesitancy. We found that there were more sociodemographic disparities in uptake for EPI vaccines (i.e., mandated and publicly funded vaccines) than non-EPI vaccines (i.e. optional vaccines requiring payment), and we found vaccine hesitancy to be related to lower uptake of non-EPI, but not EPI vaccines.
Vaccine hesitancy and vaccination coverage
Studying the relationship between hesitancy and uptake of mandated vaccines allows us to understand how governmental regulations can impact vaccination coverage, even with the existence of widespread hesitancy. By comparing the impact of vaccine hesitancy in EPI and non-EPI vaccines, we can see if adding the vaccines into the EPI list mitigates the impact of parentsʻ hesitancy. This could necessitate expanding the EPI list to include vaccine-preventable diseases with high burden but low uptake rate in the future. We found that vaccine hesitancy related to uptake of non-EPI but not EPI vaccines. Worldwide there is widespread, consistent support for mandatory vaccines.Citation25 As expected for this study, mandating vaccination such as requiring vaccines for school entry did mitigate the impact of vaccine hesitancy for EPI-vaccines. Our results indicate that even if individuals are vaccine hesitant, they will receive these vaccines, even if they opt out of non-mandatory vaccines like PCV1 and RVV1. This pattern would seem to indicate that future inclusion of vaccines onto the EPI list could increase their coverage, even among vaccine hesitant parents. However, we acknowledge that parents in Shanghai express strong preferences about having fewer vaccines given to their children at young ages,Citation19,Citation26 and co-administration of vaccines is relatively low,Citation27 especially compared to the vaccine schedule in countries like the United States.Citation28
Hib, pneumococcal, and rotavirus vaccination are relatively recent additions to the list of the WHOʻs recommended vaccinations for public funding,Citation3 but they are not yet publicly funded within China. Calls to do so have focused on the high burden of disease that could be protected against by these vaccines.Citation29 However, the high cost for some of these vaccines made by international pharmaceutical companies, particularly PCV, could be problematic for public funds.Citation4,Citation29 Moreover, public funding for vaccines in China typically occurs only for vaccines produced by domestic companies.Citation30 There have been domestically produced monovalent RVV and Hib vaccines for several years, with a Chinese- made PCV released only in April 2020.Citation31 At the same time, the immunization schedule in Shanghai has undergone several changes recently. Shanghai made a shift to adding in inactivated polio vaccine (IPV) doses in May 2016Citation30 (as of October 2020, there is a full 4 dose IPV schedule), and publicly funding VZV starting 1 August 2018. Nationally, though, VZV is still a non-EPI vaccine. Cost-effectiveness studies have found PCVCitation32 and HibCitation33 to be cost-effective, but due to its lower cost and longer time being produced domestically, the Hib vaccine may be more likely to be included in the Shanghai EPI at an earlier date. Interestingly, within our study, vaccine hesitancy did not substantially impact the uptake of Hib vaccine. This might be due to Hib vaccine being a relatively low cost vaccine, that is made domestically, but determinants of parents acceptance of the Hib vaccine need to be further studied.
Disparities in vaccination uptake
Across all vaccination outcomes considered, we did observe lower coverage among non-locals, and especially rural non-locals, compared to locals. As China rapidly urbanizes, more and more families move into cities, and, although vaccine services are offered to residents without regard to their residency status, there could be other reasons driving reduced vaccination coverage in non-locals. For example, a study from Hangzhou, another city in eastern China close to Shanghai, found that lower vaccination uptake in non-locals was associated with larger family sizes, lower family income, and the family living in the area for a shorter period of time.Citation34
Besides residency status, however, there were relatively fewer disparities for EPI vaccines compared to non-EPI vaccines. For example, those with a higher educational level were more likely to have their child receive PCV1 or Hib1, whereas the proportions were comparable for full coverage of all EPI vaccines. This indicates that there has been an equitable push for vaccines on the EPI schedule. This push was present in earlier programs and funding streams, including a project to fund HepB vaccination from Gavi, the Vaccine Alliance.Citation35 Previous research has shown high vaccination coverage of EPI vaccines across the country.Citation36 That gaps by socioeconomic status are larger for non-EPI vaccines speak to the lack of public funding,Citation5,Citation34 and also a lack of trust or knowledge or less perceived need for these vaccines.Citation37,Citation38
Strengths and limitations
A strength of this study was that it is a cohort study. We originally sampled the parents and asked their attitudes toward the pediatric vaccines in 2017, when their infants were very young, and we pulled out the vaccination records of these children in 2020, through which we can see if the actual vaccination results corresponded with parentsʻ stated attitudes. We will further follow up these parents to see how their attitudes toward pediatric vaccines change over time. Additionally, we included a representative sample of parents throughout almost all districts in Shanghai, excluding one district far away from the downtown area. However, this sample may be biased since parents formed a convenience sample of those attending a vaccination clinic. Thus, these selected parents might be already less vaccine hesitant than those who would never attend a vaccination clinic. The first survey sampled caregivers of infants younger than 3 months old in order to limit the exposure parents had to pediatric vaccination or childhood disease. However, most infants received some doses of vaccine before this point, and so the parents would have already had some impression of vaccinations prior to the baseline survey. In addition, we removed 216 children who had moved out of Shanghai by the date of retrieving the vaccination records. This may overestimate vaccination coverage, since a large proportion of people lost to follow up were non-locals.
Conclusions
In a cohort study from Shanghai, China, we identified how coverage of publicly funded EPI vaccines differed from non-EPI vaccines (including vaccines for rotavirus, Hib, and pneumococcus, which carry strong recommendations from the WHO). Coverage of non-EPI vaccines was lower, less timely, and incurred more of a disparity by education level and between those vaccine hesitant or not. As more vaccines are added onto the EPI in Shanghai, it will be important to gauge the general populationʻs attitude toward these new vaccines.
Supplemental Material
Download MS Word (26.5 KB)Acknowledgements
We appreciate the work of the technicians at the Shanghai Immunization Program Information System for the help obtaining the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available upon reasonable request from the corresponding author.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2043025
Additional information
Funding
References
- Greenwood B. The contribution of vaccination to global health: past, present and future. Philos Trans R Soc Lond B Biol Sci. 2014;369(1645):20130433. doi:10.1098/rstb.2013.0433.
- Chard AN, Gacic-Dobo M, Diallo MS, Sodha SV, Wallace AS. Routine vaccination coverage — worldwide, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1706–8. doi:10.15585/mmwr.mm6945a7.
- World Health Organization. Summary of WHO position papers - recommendations for routine immunization (updated: April 2019) [Internet]. 2019 [cited 2019 Nov 1]. Available from: https://www.who.int/immunization/policy/Immunization_routine_table1.pdf
- Zhuang J-L, Wagner AL, Laffoon M, Lu Y-H, Jiang Q-W. Procurement of category 2 vaccines in China. Vaccines (Basel). 2019;7(3):97. doi:10.3390/vaccines7030097.
- Wagner AL, Sun X, Montgomery JP, Huang Z, Boulton ML, Xu J. The impact of residency and urbanicity on Haemophilus influenzae type b and pneumococcal immunization in Shanghai children: a retrospective cohort study. PLoS One. 2014;9(5):e97800. doi:10.1371/journal.pone.0097800.
- Oʻ-Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902. doi:10.1016/S0140-6736(09)61204-6.
- Watt JP, Wolfson LJ, Oʻ-Brien KL, Henkle E, Deloria-Knoll M, McCall N, Lee E, Levine OS, Hajjeh R, Mulholland K, et al. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Lancet. 2009;374(9693):903–11. doi:10.1016/S0140-6736(09)61203-4.
- Yang Y, Shen X, Jiang Z, Liu X, Leng Z, Lu D, Rao J, Liu J, Chang L. Study on Haemophilus influenzae type b diseases in China: the past, present and future. Pediatr Infect Dis J. 1998;17(Supplement):S159–65. doi:10.1097/00006454-199809001-00013.
- Wu D, Yen C, Yin Z-D, Y-X L, Liu N, Liu Y-M, Wang H-Q, Cui F-Q, Gregory CJ, Tate JE, et al. The public health burden of rotavirus disease in children <5 years of age and considerations for rotavirus vaccine introduction in China. Pediatr Infect Dis J. 2016;35(12):e392. doi:10.1097/INF.0000000000001327.
- Thomson A, Robinson K, Vallée-Tourangeau G. The 5as: A practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34:1018–24. doi:10.1016/j.vaccine.2015.11.065.
- World Health Organization. Ten Threats to global health in 2019 [Internet]. 2019 [accessed 2019 Jan 22]. Available from: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019
- The Strategic Advisory Group of Experts (SAGE). Report of the SAGE working group on vaccine hesitancy [Internet]. 2014 [cited 2018 Jun 14]; Available from: http://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf
- MacDonald N, Dubé E, Butler R. Vaccine hesitancy terminology: A response to Bedford et al. Vaccine. 2017;37(30):3947–48. doi:10.1016/j.vaccine.2017.11.060.
- Hou Z, Chang J, Yue D, Fang H, Meng Q, Zhang Y. Determinants of willingness to pay for self-paid vaccines in China. Vaccine. 2014;32:4471–77. doi:10.1016/j.vaccine.2014.06.047.
- Jarrett C, Wilson R, Oʻ-Leary M, Eckersberger E, Larson HJ. Strategies for addressing vaccine hesitancy – a systematic review. Vaccine. 2015;33:4180–90. doi:10.1016/j.vaccine.2015.04.040.
- Lv M, Fang R, Wu J, Pang X, Deng Y, Lei T, Xie Z. The free vaccination policy of influenza in Beijing, China: the vaccine coverage and its associated factors. Vaccine. 2016;34:2135–40. doi:10.1016/j.vaccine.2016.02.032.
- Zhang X, Syeda ZI, Jing Z, Xu Q, Sun L, Xu L, Zhou C. Rural-Urban disparity in category II vaccination among children under five years of age: evidence from a survey in Shandong, China. Int J Equity Heal. 2018;17:1–8.
- Ren J, Wagner AL, Zheng A, Sun X, Boulton ML, Huang Z, Zikmund-Fisher BJ, Angelillo IF. The demographics of vaccine hesitancy in Shanghai, China. PLoS One. 2018;13(12):e0209117. doi:10.1371/journal.pone.0209117.
- Huang Z, Wagner AL, Lin M, Sun X, Zikmund-Fisher BJ, Boulton ML, Ren J, Prosser LA. Preferences for vaccination program attributes among parents of young infants in Shanghai, China. Hum Vaccines Immunother. 2020;16(8):1905–10. doi:10.1080/21645515.2020.1712937.
- Sun X, Wagner AL, Ji J, Huang Z, Zikmund-Fisher BJ, Boulton ML, Ren J, and Prosser LA. A conjoint analysis of stated vaccine preferences in Shanghai, China. Vaccine. 2020;36(6):1520–25.
- Cella P, Voglino G, Barberis I, Alagna E, Alessandroni C, Cuda A, Dʻ-Aloisio F, Dallagiacoma G, Nitto SDE, Gaspare FDI, et al. Resources for assessing parents' vaccine hesitancy: a systematic review of the literature. J Prev Med Hyg. 2020;61(3):E340–73. doi:10.15167/2421-4248/jpmh2020.61.3.1448.
- Larson HJ, Jarrett C, Schulz W, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33:4165–75. doi:10.1016/j.vaccine.2015.04.037.
- Akel KB, Masters NB, Shih S-F, Lu Y, Wagner AL. Modification of a vaccine hesitancy scale for use in adult vaccinations in the United States and China. Hum Vaccin Immunother. 2021;17(8):2639–46. doi:10.1080/21645515.2021.1884476.
- Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in China. Lancet. 2012;379(9818):843–52. doi:10.1016/S0140-6736(11)61878-3.
- Gualano MR, Olivero E, Voglino G, Corezzi M, Rossello P, Vicentini C, Bert F, Siliquini R. Knowledge, attitudes and beliefs towards compulsory vaccination: a systematic review. Hum Vaccin Immunother. 2019;15(4):918–31. doi:10.1080/21645515.2018.1564437.
- Wagner AL, Boulton ML, Sun X, Huang Z, Harmsen IA, Ren J, Zikmund-Fisher BJ. Parentsʻ concerns about vaccine scheduling in Shanghai, China. Vaccine. 2017;35:4362–67. doi:10.1016/j.vaccine.2017.06.077.
- Wagner AL, Sun X, Huang Z, Boulton ML. Co-Administration of paediatric vaccines in Shanghai, China. Public Health. 2016;131:52–55. doi:10.1016/j.puhe.2016.08.017.
- Wodi AP, Ault K, Hunter P, McNally V, Szilagyi PG, Bernstein H. Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger — United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(6):189–92. doi:10.15585/mmwr.mm7006a1.
- Yu H, Yang W, Varma JK. To save childrenʻs lives, China should adopt an initiative to speed introduction of pneumonia vaccines. Heal Aff. 2012;31(11):2545–53. doi:10.1377/hlthaff.2011.1272.
- Ghosh P. Human vaccines industry in China, 2019: Part—I. MGM J Med Sci. 2020;7(1):35. doi:10.4103/mgmj.MGMJ_27_20.
- Sohu News. Guó chǎn yì miáo jìn kǒu tì dài jìn xíng shí : zhōng guó shǒu gè zì yán 13 jià fèi yán jié hé yì miáo (wò ān xīn) huò pī [Internet]. 2020 [cited 2021 Sep 1]; Available from: https://www.sohu.com/a/388546646_114778
- Maurer KA, Chen H-F, Wagner AL, Hegde ST, Patel T, Boulton ML, Hutton DW. Cost-Effectiveness analysis of pneumococcal vaccination for infants in China. Vaccine. 2016;34:6343–49. doi:10.1016/j.vaccine.2016.10.051.
- Zhang H, Garcia C, Yu W, Knoll MD, Lai X, Xu T, Jing R, Qin Y, Yin Z, Wahl B, et al. National and provincial impact and cost-effectiveness of Haemophilus influenzae type b conjugate vaccine in China: a modeling analysis. BMC Med. 2021;19(1):1–14. doi:10.1186/s12916-021-02049-7.
- Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J. Comparative assessment of immunization coverage of migrant children between national immunization program vaccines and non-national immunization program vaccines in East China. Hum Vaccin Immunother. 2015;11(3):761–68. doi:10.1080/21645515.2015.1012015.
- Cui F, Liang X, Gong X, Chen Y, Wang F, Zheng H, Wu Z, Miao N, Hadler SC, Hutin YJ, et al. Preventing hepatitis B though universal vaccination: reduction of inequalities through the GAVI China project. Vaccine. 2013;31:J29–35. doi:10.1016/j.vaccine.2012.07.048.
- Cao L, Wang H-Q, Zheng J-S, Yuan P, Cao L-S, Zhang G-M, and Jiang K-Y. National immunization coverage survey in China after integrated more vaccines into EPI since 2008. Chin J Vaccine Immun. 2012;18:419–24.
- de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396:898–908.
- Wagner AL, Boulton ML, Sun X, Mukherjee B, Huang Z, Harmsen IA, Ren J, Zikmund-Fisher BJ. Perceptions of measles, pneumonia, and meningitis vaccines among caregivers in Shanghai, China, and the health belief model: a cross-sectional study. BMC Pediatr. 2017;17(1):143. doi:10.1186/s12887-017-0900-2.
