ABSTRACT
This study aims to assess COVID-19 vaccine acceptance among Muslims in Malaysia. A cross-sectional internet-based survey was to determine acceptance of COVID-19 vaccine. Other influential factors, namely socio-demographics, COVID-19 experience, self-perceived level of religiosity, support in immunization, COVID-19 immunization attitudes, and health fatalistic beliefs (measured using the Helpless Inevitability Subscale of the Religious Health Fatalism Questionnaire, RHFQ-HI) were investigated. The majority reported a definite intent to receive the COVID-19 vaccine (57.3%; 95% CI 55.0–59.6) followed by a probable intent (42.7%; 95% CI 40.4–45.0%). COVID-19 immunization attitudes measured by attitudinal barriers to vaccination scores were found to be the strongest influence of COVID-19 vaccination intent, whereby participants who have lower attitudinal barrier scores reported higher COVID-19 vaccination intent (OR = 6.75 ; 95% 5.20–8.75). Although religious health fatalism was not significantly associated with vaccination intent, a significantly higher proportion of participants with score 4–9 (61.9%) in the RHFQ-HI reported intent to receive COVID-19 vaccine than those with a score of 10–20 (53.5%), p < .001. Intervention for people with skeptical attitudes toward COVID-19 vaccination is warranted.
Introduction
The COVID-19 pandemic poses a great challenge to the population worldwide including the Muslims. An increasing number of Muslim-majority countries across the globe were stricken badly by the outbreak. As of early May 2020, Turkey, Saudi Arabia, Pakistan and Iran were among the hardest-hit Muslim countries by the coronavirus pandemic. Malaysia is a Muslim majority country in the Southeast Asia region that was equally impacted greatly by the COVID-19 outbreak. Malaysia announced the first three cases of COVID-19 on 25 January 2020. On 3 April 2020, Malaysia had the highest number of known infections in Southeast Asia, with 3116 confirmed cases and 50 deaths,Citation1 and a large number of the cases have been linked to a tabligh (religious) gathering.
Vaccine acceptance has always been a challenge in many Muslim countries, and the Muslim religion has been associated with lower vaccination coverage.Citation2 Rejection of immunization on religious grounds is still strong among many Muslims, especially in more conservative Muslim societies. Doubts over the halal (kosher) status of vaccine is well-known to be the major concern of Muslims rejecting immunizations.Citation3,Citation4 Religious health fatalism, the belief that an individual’s health outcome is predetermined or purposed by a higher power and not within the individual’s control, has been a widely used theory in understanding a variety of health and illness-seeking behaviors, as well as an inhibitor to participation in health promotion programmes, health-care utilization and health decision-making.Citation5–8 Muslim, in particular, is a religion with many in the community whose health behaviors are influenced greatly by fatalistic beliefs.Citation9 Studies reported that some Muslims view God as the one who ultimately controls health and illness and believe that God can provide a cure.Citation10,Citation11 Such belief has been reported to greatly influence Muslim health behaviors to the extent that it poses great challenges and ethical dilemmas to health care.Citation12 To the best of our knowledge, religious health fatalism has never been used to investigate vaccine intention among Muslims. Muslims rejecting immunization on religious grounds have been an ongoing concern.Citation13,Citation14 Examining the intersection of religious health fatalism and intention to receive a hypothetical COVID-19 vaccine will provide insights into how these beliefs impact on the Islamic perspective on COVID-19 vaccination.
Malaysia is a Muslim majority country. Prior to the COVID-19 pandemic, the National Immunization Program (NIP) in Malaysia provides free vaccination services to protect Malaysian children from infectious diseases including hepatitis B, poliomyelitis, tuberculosis, Haemophilus influenzae type b, measles, mumps, rubella, Japanese encephalitis (JE) and human papillomavirus (HPV).Citation15 The reported immunization coverage of Malaysia by 2018 was 100% for DPT -HIB (third dose) and polio vaccine (third dose), near 100% for BCG (98.43%) and Hepatitis B (99.16%), and over 80% for MMR (87.75%) and HPV (82.23%).Citation16 As religious affiliation has been known as potential barrier in some Muslim countries,Citation2 uncovering the acceptability of the COVID-19 vaccine is important to inform health policy decisions to improve vaccination coverage in the future. Therefore, the main aim of this study was to assess COVID-19 vaccine acceptance among Muslims in Malaysia. Influential factors of vaccine acceptance, namely socio-demographics, COVID-19 experience, self-perceived level of religiosity, support in immunization, COVID-19 immunization attitudes, and health fatalistic beliefs were explored.
Methods
Study participants and survey design
We commenced a cross-sectional, web-based anonymous survey using an online questionnaire. A website version of the questionnaire was developed using the Google Forms platform. The researchers used the social network platforms of Facebook, Instagram, and WhatsApp to disseminate the Google Forms survey to their network members. Network members were requested to distribute the invitation to all their contacts i.e., snowball distribution of the survey invitation and share on social media. The inclusion criteria were that the respondents were Malaysian Muslim residents who were between 18 and 70 years of age. Taking into consideration that online and mobile users are younger and higher education level, network members were encouraged to disseminate survey link to people of older age and of lower education level to enhance representativeness. The respondents were informed that their participation was voluntary and consent was implied through their completion of the questionnaire. The questionnaire was developed in English and was then translated into Bahasa Malaysia, the national language of Malaysia. A standard forward and back-translation procedure was followed. Questions were presented bilingually in English and Bahasa Malaysia. A panel of experts that consisted of multidisciplinary academicians and researchers validated the content of the questionnaire. Pilot testing was conducted on 20 persons to test the clarity of the items and feasibility of the answer options before the administration of the questionnaire.
Instruments
The questionnaire of the survey, which consists of questions that assessed 1) demographic backgrounds, self-perceived level of religiosity, support in immunization and COVID-19 experience; 2) immunization attitudes; 3) religious health fatalism; and 4) intention to receive a COVID-19 vaccine.
Socio-Demographics, religiosity, support in immunization and COVID-19 experience
Personal details, including age, gender, marital status, occupation, and average monthly household income, were queried. The participants were asked to rate their level of religiosity on a four-point scale (‘not at all’, ‘slightly’, ‘moderately’, ‘very’). Support in immunization was categorized as 1) pro-vaccine (‘You/your child(ren) were vaccinated with all the recommended vaccines in the Malaysian National Immunization Programme at the recommended age-intervals’);Citation17 2) vaccine-hesitant (‘You/your child(ren) were unvaccinated for at least one of the recommended vaccines or you/your child(ren) were not vaccinated at all but were still uncertain about the decision of vaccination’); and 3) anti-vaxxer (‘You/your child(ren) were not vaccinated with all the recommended vaccines at the recommended age-intervals’). The question on COVID-19 experience asked participants whether they have ever been infected with COVID-19 and know of any close acquaintances such as friends, neighbors or colleagues who have been infected with COVID-19.
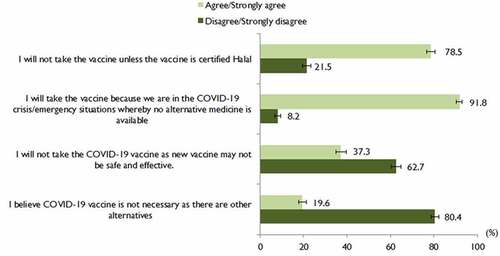
COVID-19 immunization attitudes
COVID-19 immunization attitudes were measured by self-developed attitudinal barriers to COVID-19 vaccination questions (a 4-item rating) that probed the perceived barriers to COVID-19 vaccination. Question 1: ‘I will not take the vaccine unless the vaccine is certified halal’. Question 2: ‘I will take the vaccine because we are in the COVID-19 crisis/emergency situation whereby no alternative medicine is available. Question 3: ‘I will not take the COVID-19 vaccine as the new vaccine may not be safe and effective’. Question 4: ‘I believe the COVID-19 vaccine is not necessary as there are other alternatives’. The response options were ‘strongly agree’, ‘agree’ ‘disagree ‘or ‘strongly disagree’. The question items were scored on a scale from 1 (strongly disagree) to 4 (strongly agree), then summed to create a total scale score. Question 2 was reverse-scored. The possible total attitudinal barriers to vaccination scores ranged from 4 to 16, with higher scores representing higher barriers to COVID-19 vaccination.
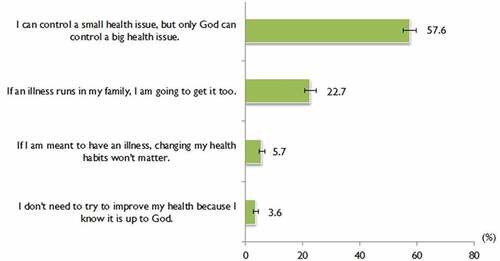
Religious health fatalism
Religious health fatalisms were measured by the Helpless Inevitability Subscale of the Religious Health Fatalism Questionnaire (RHFQ-HI).Citation5,Citation7 The RHFQ-HI is designed to measure the belief that God, not the individual, has control over health outcomes.Citation7 The RHFQ-HI was reported to have a high coefficient alpha (Cronbach alpha reliability coefficient of .89).Citation7 The smaller number of items in the RHFQ-HI is ideal to be used in self-administered online survey to reduce the number of drop-outs. The RHFQ-HI was found to have a Cronbach alpha reliability coefficient The response options were ‘strongly agree’, ‘agree’, ‘neutral’, ‘disagree ‘or ‘strongly disagree’. The question items were scored on a scale from 1 (strongly disagree) to 5 (strongly agree), then summed to create a total scale score. The possible total religious health fatalism score ranged from 4 to 20, with higher scores representing a higher level of religious health fatalism.
Intention to receive a COVID-19 vaccine
The intention to accept a COVID-19 vaccine was measured using a one-item question (If a vaccine against COVID-19 is available on the market, would you take it?) on a four-point scale (‘definitely not’ to ‘yes, definitely’).
All the items in the questionnaire underwent face and content validity by a panel of several experts that consist of academicians, researchers and clinicians to ensure the relevance and clarity of the questions. After amendments, the questionnaire was pilot-tested on randomly sampled lay public who were not included in the study.
Ethical considerations
This study was approved by the University of Malaya Research Ethics Committee (UMREC). Approval code: UM.TNC2/UMREC − 887.
Sample size calculation
The calculated sample size was 385 based on a normal approximation to the binomial distribution with a finite population correction applied,Citation18 assuming an observer proportion of respondents selecting a specific response option of 50%, a 95% confidence level, and a margin of error of 5%, and population size of 17.4 million Muslim in Malaysia.Citation19 The sample size was multiplied by the predicted design effect of two to account for the use of convenience sampling and an online survey.Citation20 Hence, the minimum survey sample size was 770 (385 × 2).
Statistical analysis
The reliability of the self-developed attitudinal barriers to COVID-19 vaccination and RHFQ-HI were evaluated by assessing the internal consistency of the items representing the scores. The four items for attitudinal barriers and the RHFQ-HI scores had a reliability (Cronbach’s α) of .606 and .493, respectively.
Frequency tables, charts and proportions were used for data summarization. The proportion and its respective 95% confidence interval (CI) were calculated. The Pearson chi-square test was used to test whether there were statistically significant differences in vaccination intent and the independent variables in the univariate analyses. We ran multivariable logistic regression analysis to evaluate factors associated with the definite intention to take the COVID-19 vaccine (1= Definitely yes; 0 = Probably yes/probably not/definitely not). The independent variables which have been found to be significant (p < .05) were entered into the multivariable model. The model fit of multivariable logistic regression analysis was assessed using the Hosmer–Lemeshow goodness-of-fit test.Citation21 The Hosmer-Lemeshow statistic indicated a poor fit if the significance value is less than .05. All statistical analyses were performed using the Statistical Package for the Social Sciences, version 20.0 (IBM Corp., Armonk, NY, USA).
Results
Demographics, religiosity, support in immunization and COVID-19 experience
The survey link was disseminated from April 29 to 10 May 2020, and a total of 1,856 complete responses were received and included in the analyses. shows the demographics of our study participants compared with the general adults population in Malaysia.Citation22 Our study population has a slightly higher proportion of females and participants from the bottom 40% (B40) household income range,Citation23 and the Southern region. As shown in the first and second columns of , the study respondents were in the age group of 18 to 30 years old (27.3%) and 31–40 years old (32.5%). The study had a higher representation of females (62.1%), married participants (73.4%), and participants of professional and managerial occupations (56.1%). The proportion of the household income of the study participants was almost equally distributed among all the categories. The study received respondents from all the states in Malaysia, nonetheless, the higher proportion of the participants were from the southern (43.0%) and northern (27.2%) regions. Most of the study participants perceived their level of religiosity to be very religious (66.2%). Only .5% (n = 10) of the study participants reported that they have ever been infected with COVID-19 and 33.9% (n = 629) reported to have close acquaintances who have been infected with COVID-19. A total of 12% (n = 222) identified themselves as vaccine-hesitant (n = 184) and anti-vaxxer (n = 28).
Table 1. Comparison of demographic characteristics of the study population and the general adults population in Malaysia, 2019
Table 2. Demographic characteristics of participants and factors associated with COVID −19 vaccination intent (N = 1856)
COVID-19 immunization attitudes
shows the results of the attitudinal barriers to COVID-19 vaccination. A high proportion (78.5%; 95% CI 76.6–80.4%) reported agree/strongly agree that they will not take the vaccine unless the vaccine is certified halal. A very high proportion (91.8%; 95% CI 90.4–93.0%) reported that they will take the vaccine in the event of an emergency situation where no alternative medicine is available. Only 19.6% (95% CI 17.8–21.4) reported agree/strongly agree that COVID-19 is not necessary as there are other alternatives. The mean and SD for the total attitudinal barriers score was 9.2 (SD ±2.1; range 4 to 16) out of a possible score of 16. The median was 9.0 (IQR 8.0 to 10.0). The attitudinal barriers scores were categorized as a score of 9 to 16 or 4 to 8, based on the median split; as such, a total of 1238 (66.7%; 95% CI 64.5–68.8) were categorized as having a score of 9 to 16 and 618 (33.3%; 95% CI 31.2–35.5) had a score of 4 to 8.
Religious health fatalism
shows the proportion of responses to the RHFQ-HI items. The highest proportion of strongly agree/agree (57.6%; 95% CI 55.3–59.9) was reported for item ‘I can control a small health issue, but only God can control a big health issue’. The lowest proportion of strongly agree/agree (3.6%; 95% CI 2.8–4.6) was reported for the item ‘I don’t need to try to improve my health because I know it is up to God’. The mean and SD for the total RHFQ-HI score was 9.7 (SD ±2.6; range 4 to 20) out of a possible score of 20. The median was 10.0 (IQR 8.0 to 11.0). The RHFQ-HI scores were categorized as a score of 10 to 20 or 4 to 9, based on the median split; as such, a total of 1004 (54.1%; 95% CI 51.8–56.4) were categorized as having a score of 10 to 20 and 852 (45.9%; 95% CI 43.6–48.2) had a score of 4 to 9.
Intention to receive a COVID-19 vaccine
On the whole, a total of 1,747 (94.1%) participants responded yes to COVID-19 vaccine intent, while only 109 (5.8%) responded no. By a more specific breakdown, the majority responded definitely yes (57.3%; 95% CI 55.0–59.6) followed by probably yes (42.7%; 95% CI 40.4–45.0%). Only 1.9% (95% CI 1.4–2.7) responded definitely no and probably no (3.9%; 95% CI 3.1–4.9).
The third and fourth column of shows the univariable and multivariate analyses of factors associated with the definitely yes response to intention to be vaccinated against COVID-19. By demographics, the multivariable analysis finding indicated that the 18‒30 age group reported the highest likelihood of a definite intention to take the COVID-19 vaccine (OR = 1.50; 95% CI 1.03 to 2.20) than the age group above 50 years old. There is a gradual increase in COVID-19 vaccine intent with an increase in income. Participants of income MYR4001–8000 (OR = 1.90; 95% 1.33–2.72) and MYR8001 and above (OR = 1.68; 95% 1.14–2.45) reported significantly higher COVID-19 vaccine intent than those of income MYR2000 and below.
The attitudinal barriers score was found to significantly influence COVID-19 vaccination intent, whereby participants who have lower attitudinal barrier score reported higher COVID-19 vaccination intent (OR = 6.75; 95% 5.20–8.75). Support in immunization also significantly influenced COVID-19 vaccination intent. Participants who were pro-vaccine reported a higher likelihood of intention to be vaccinated against COVID-19 than participants who were vaccine-hesitant/anti-vaxxer (OR = 2.76; 95% 1.97–3.87). Of note, univariate analysis showed that of the total 12% (n = 222) participants that identified themselves as vaccine-hesitant or anti-vaxxer, only 26.6% (n = 59) reported a definite intent to receive the COVID-19 vaccine. Although religious health fatalism was not significantly associated with COVID-19 vaccination intent in the multivariate analysis, in the univariable analysis, a significantly higher proportion of participants with a score of 4–9 (61.9%) in the RHFQ-HI reported intent to receive COVID-19 vaccine than those of score 10–20 (53.5%), p < .001.
Discussion
The acceptance of the vaccine among Muslims warrants urgent research due to long-standing issues surrounding vaccine hesitancy. The Islamic Law states that when faced with emergency circumstances that ‘threaten[s] the life of a nation’ the use of non-halal-certified substances is allowed.Citation24 Of positive note, the vast majority of our study was able to accept a non-halal-certified vaccine when there is a necessity—such as in a desperate and emergency situation and there is no alternative medicine. The process of manufacturing a halal COVID-19 vaccine is likely to take a longer time to materialize. The process and cost of a halal-certified vaccine remain the greatest challenge in its production. In the meantime, religious authority in Muslim countries needs to enlighten the public on the importance of accepting a COVID-19 vaccine, although it may not be halal-certified at the point of its availability. The public may be worried about whether the new COVID-19 vaccine is permissible on religious grounds. It has been suggested that religious leaders should emphasize the fact that not all vaccine contains non-halal materials and if there is any, the amount of the material is insignificant, or almost negligible.Citation4 In addition, the WHO for the Eastern Mediterranean confirmed that the porcine sources used in many vaccines have undergone characteristic changes from impure substances into pure substances (istihalah) that are permissible for use.Citation15 Hence, the Ulama (Muslim religious leaders) and the Fatwa Council members of the country must take a unified stance and inform the public about the Islamic view on the permissibility of COVID-19 so that they could help to alleviate public concern about the vaccine being permissible for Muslims. In consideration of the high global Muslim population, there is potentially a massive global demand for halal COVID-19 vaccines in the near future. The findings of this study highlight the importance of research and production of halal COVID-19 vaccine to serve the needs of the huge global Muslim population to effectively curb the pandemic.
As shown in the results, slightly over one-third expressed reluctance to accept a new vaccine for the new coronavirus based on the safety and effectiveness of a newly developed vaccine. This indicates that people warrant assurance or evidence of the vaccine to be safe and effective before administration. This finding evidences the importance of providing information on the safety and effectiveness of the new COVID-19 vaccine to the public to enhance their acceptance of the new vaccine. This is in line with the WHO recommendations that the development of a COVID-19 vaccine, although it should be accelerated, should not be deployed without sufficient confidence in its safety and efficacy.Citation25
A preference for COVID-19 vaccination alternatives to curb the COVID-19 was evident in this study. A considerably small proportion of the study participants noted that the COVID-19 vaccine is not necessary as there are other alternatives. The alternatives could be pharmacology treatment, other alternative treatments or non-pharmalogical prevention. Unfortunately, the details of the types of COVID-19 vaccination alternatives were not probed in this online survey. Further research is required to understand the preference of COVID-19 vaccination alternatives. In Malaysia, vaccine hesitancy in the national immunization programmes based on reasons other than religious concerns of the halal issue of the vaccine was common. These include beliefs in alternative therapies or treatment, namely traditional medicine and use of food supplement.Citation9
The COVID-19 vaccine acceptance among the Muslim population in this study was high, with 57% reporting a definite intent. By demographic, multivariate analysis found that a higher definite intent to be vaccinated against COVID-19 was associated with younger age and higher income. Systematic reviews similarly found younger age and socio-economic status as important determinants for the uptake of seasonal influenza vaccination.Citation26–28 Immunization attitudes, specifically lower attitudinal barriers were associated with the highest odds ratio for a definite vaccination intent found in this study, implying its strong influence on COVID-19 vaccination intent. Similarly, previous reviews also reported attitudinal barriers inversely influence intention to get vaccinated against influenza.Citation28,Citation29 Therefore, it is recommended that intervention for attitude change toward people who are skeptical about COVID-19 vaccination is of utmost importance. Support in immunization was found as the second most important predictor of COVID-19 vaccine intent. Pro-vaccine people expressed a higher likelihood of having a definite intent to receive the COVID-19 vaccine. This study provides valuable information that shows that despite COVID-19 being highly infectious and a life-threatening illness, the vaccine-hesitant and anti-vaxxer were still skeptical about a COVID-19 vaccine.
In the current study, COVID-19 vaccine acceptance was positively associated with younger age, contrary to studies reporting higher acceptance among older age people in a global survey.Citation30 The reason why the younger age group had higher COVID-19 vaccination acceptance requires further investigation. Similar to other studies,Citation31 this study found less vaccine acceptance among the participants with low income. The finding is of concern because low-income groups are at higher risk of contracting COVID-19 due to reasons such as overcrowded living conditions and more likely to commute using public transportation which limits their social distancing ability.Citation32,Citation33 Therefore, it is important to enhance COVID-19 vaccination willingness in individuals of lower socio-economic classes.
It is also important to note that in this study, although religious health fatalism was not significantly associated with COVID-19 vaccination intent in the multivariate analysis, in the univariable analysis, higher religious health fatalism belief was significantly associated with lower intent to COVID-19 vaccination. This implies that higher religious health fatalism beliefs do have some degree of influence in COVID-19 vaccination. Of note, this study is also the first to reveal that the belief that death is inevitable influences the COVID-19 vaccination intent. Thus, our findings provide the basis for the need for targeted behavioral interventions to decrease perceptions of fatalism among the Muslims. Malaysia is a moderate Muslim country, and to the best of our knowledge, this study is also the first study that examines the helpless inevitability construct of religious health fatalism among Muslims. The median score of 10 out of the highest score of 20, coupled with a total of slightly over half of the participants reporting the higher score of 10–20, implies that the study participants have a moderate level of religious health fatalism measured by the Helpless Ineviability subscale of the Religious Health Fatalism Quesionnaire.Citation5 The RHFQ-HI score in this study was similar to that reported among African-American.Citation7
Some limitations have to be taken into account when the results of this study are interpreted. First, our study adopted a cross-sectional design, so we were able to identify associations between exposure and outcomes but could not infer cause and effect. Second, the non-probability sampling technique using an online web-based questionnaire via a social media platform may lead to selection bias, as reflected in the large sample of females and participants from professional and managerial groups. Nonetheless, the study received responses from all the states and federal territories of Malaysia, although a slightly higher number of responses were from the southern region. Of note, an important limitation associated with the unequal distribution of the number of responses may result in low statistical power in some subgroups. The bivariate screening methods were insufficient to control confounding and could exclude important variables from the multivariable analyses,Citation34 hence resulting in uncontrolled confounding and biased results.Citation35 Another limitation is the low Cronbach’s alpha coefficient for the attitudinal barriers (.606) and the RHFQ-HI (.493) found in this study. Although a Cronbach’s alpha coefficient greater than .70 means an acceptable degree of consistency in exploratory studies its acceptable value is reduced to .50.Citation36–39 The reason for the low Cronbach’s alpha coefficient for the RHFQ-HI in this study is unclear; in contrast, the RHFQ-HI was found to have a Cronbach alpha reliability coefficient of .89 in another study.Citation7 Another disadvantage of online survey research includes uncertainty over the validity of respondents’ inclusion criteria, for instance, whether the responses are genuinely from Muslims, as the online survey was distributed to an unknown audience in the social media. Additionally, self-assessment of religiosity in this study based on a four-point Likert scale may also lead to potential bias. Despite these limitations, we believe our findings provide guidance for public health intervention to enhance COVID-19 vaccine uptake among Muslims in Malaysia as well as globally. Lastly, it is important to note that this study was conducted during the early phase of the COVID-19 pandemic and before the COVID-19 vaccines are available. To date, although COVID-19 vaccination is not compulsory in Malaysia, unvaccinated individuals will lose out on many privileges, including praying at mosques, dining out, and going for Umrah in Saudi Arabia.Citation40 As of January 2022, 78.6% of the population in Malaysia were fully vaccinated against COVID-19.Citation41 The vaccination rate of the adult population of Malaysia is getting closer to 100%, with an approximately 98% having completed their COVID-19 vaccination.Citation42
Conclusions
The introduction of the new coronavirus is anticipated to be accompanied by a variety of challenges, particularly for the Muslim population. Acceptance of the COVID-19 vaccine is high among the Muslims in Malaysia. Important predictors of a definite intention to take the COVID-19 vaccine include positive COVID-19 immunization attitudes and support in immunization. Intervention for attitude change toward people who are skeptical about COVID-19 vaccination to enhance attitudes is needed. Despite COVID-19 being highly infectious and a life-threatening illness, the vaccine-hesitant and anti-vaxxers in this study were still skeptical about the COVID-19 vaccination. An in-depth understanding of how the anti-vaccine Muslim community is responding to the COVID-19 vaccine is important to provide insights for behavioral change intervention. The study also revealed that health fatalistic beliefs also have some degree of influence on COVID-19 vaccination intent, thus warranting the support of religious leaders. Understanding the Islamic perspective on COVID-19 vaccination provides important insights into future immunization policies into increasing vaccination coverage.
Author contributions
L. P.W., Y.L. and Z.H. planned the study. L.P.W., H.A., H.Y.L, S.A.B., I. C., and M.M.A.A.M.H obtained the data. L.P.W. and H.A. performed the data analysis and data summarization. L.P.W. drafted the manuscript. All authors critically reviewed the manuscript; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure statement
The authors declare no conflict of interests.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
Additional information
Funding
References
- World Health Organization (WHO). Coronavirus disease 2019 (COVID-19) situation report – 74; 2020 April 3 [accessed 2021 Aug 4]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200403-sitrep-74-covid-19-mp.pdf?sfvrsn=4e043d03_14
- Costa JC, Weber AM, Darmstadt GL, Abdalla S, Victora CG. Religious affiliation and immunization coverage in 15 countries in Sub-Saharan Africa. Vaccine. 2020;38(5):1160–9. doi:10.1016/j.vaccine.2019.11.024.
- Khoo YS, Ghani AA, Navamukundan AA, Jahis R, Gamil A. Unique product quality considerations in vaccine development, registration and new program implementation in Malaysia. Hum Vaccines Immunother. 2020;16(3):530–38. doi:10.1080/21645515.2019.1667206.
- Wong LP, Wong PF, AbuBakar S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: the way forward for Malaysia, a Southeast Asian country. Hum Vaccines Immunother. 2019. doi:10.1080/21645515.2019.1706935.
- Franklin MD, Schlundt DG, McClellan LH, Kinebrew T, Sheats J, Belue R, Brown A, et al. Religious fatalism and its association with health behaviors and outcomes. Am J Health Behav. 2007;31(6):563–72. doi:10.5993/AJHB.31.6.1.
- Nageeb S, Vu M, Malik S, Quinn MT, Cursio J, Padela AI. Adapting a religious health fatalism measure for use in Muslim populations. PloS One. 2018;13(11):1–12. doi:10.1371/journal.pone.0206898.
- Franklin MD, Schlundt DG, Wallston KA. Development and validation of a religious health fatalism measure for the African-American faith community. J Health Psychol. 2008;13(3):323–35. doi:10.1177/1359105307088137.
- Leyva B, Allen JD, Tom LS, Ospino H, Torres MI, Abraido-Lanza AF. Religion, fatalism, and cancer control: a qualitative study among Hispanic Catholics. Am J Health Behav. 2014;38(6):839–49. doi:10.5993/AJHB.38.6.6.
- Wong LP, Wong PF, Megat Hashim MMAA, Han L, Lin Y, Hu Z, Zhao Q, Zimet GD, et al. Multidimensional social and cultural norms influencing HPV vaccine hesitancy in Asia. Hum Vaccines Immunother. 2020;16(7):1611–22. doi:10.1080/21645515.2020.1756670.
- Johnson JL, Bottorff JL, Balneaves LG, Grewal S, Bhagat R, Hilton BA, Clarke H. South Asian womens’ views on the causes of breast cancer: Images and explanations. Patient Educ Couns. 1999;37(3):243–54. doi:10.1016/s0738-3991(98)00118-9.
- Padela AI, Gunter K, Killawi A, Heisler M. Religious values and healthcare accommodations: voices from the American Muslim community. J Gen Intern Med. 2012;27:708–15. doi:10.1007/s11606-011-1965-5.
- Padela AI, Zaidi D. The Islamic tradition and health inequities: A preliminary conceptual model based on a systematic literature review of Muslim health-care disparities. Avicenna J Med. 2018;8(1):1–13. doi:10.4103/ajm.AJM_134_17.
- Warraich HJ. Religious opposition to polio vaccination.Emerging Infectious Diseases. 2009;15(6):978. doi:10.3201/eid1506.090087.
- Ahmed A, Lee KS, Bukhsh A, Al-Worafi YM, Sarker MM, Ming LC, Khan TM, et al. Outbreak of vaccine-preventable diseases in Muslim majority countries. J Infect Public Health. 2018;11(2):153–55. doi:https://doi.org/10.1016/j.jiph.2017.09.007.
- MYHEALTH Portal Kementerian Kesihatan Malaysia. Immunization Schedule. 2015 [accessed 2021 Aug 3]. http://www.myhealth.gov.my/en/immunization-schedule/
- Ministry of Health Malaysia. Health Facts 2019. [accessed 2021 Aug 3]. https://www.moh.gov.my/moh/resources/Penerbitan/Penerbitan%20Utama/HEALTH%20FACTS/Health%20Facts%202019_Booklet.pdf./
- Kusnin F Immunisation program in Malaysia. [accessed 2021 Aug 3]. https://www.fondation-merieux.org/wp-content/uploads/2017/10/vaccinology-2017-faridah-kusnin.pdf
- Daniel WW. Biostatistics: a foundation for analysis in the health sciences. 7th ed. New York: John Wiley & Sons; 1999.
- Department of Statistics Malaysia. Population distribution and basic demographic characteristic report 2010 (Updated: 05/08/2011). [accessed 2022 Jan 16]. https://www.dosm.gov.my/v1/index.php?r=column/ctheme&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09&bul_id=MDMxdHZjWTk1SjFzTzNkRXYzcVZjdz09#:~:text=The%20total%20population%20was%2028.3,%25)%20and%20Others%20(0.7%25)
- Wejnert C, Pham H, Krishna N, Le B, DiNenno E. Estimating design effect and calculating sample size for respondent-driven sampling studies of injection drug users in the United States. AIDS Behav. 2012;16(4):797–806. doi:https://doi.org/10.1007/s10461-012-0147-8.
- Hosmer JD, Lemeshow S, Sturdivant R. Applied logistic regression. New Jersey: John Wiley & Sons; 2013.
- Deparment of Statistics Malaysia. The 2019 population and housing census of Malaysia. [accessed 2021 Aug 5]. http://pqi.stats.gov.my/result.php?token=ead145b6134eacd515fcbbb52b79fcd1
- Department of Statistics Malaysia. Household income and basic amenities survey report 2019. [accessed 2021 Aug 5]. https://www.dosm.gov.my/v1/uploads/files/1_Articles_By_Themes/Prices/HIES/HIS-Report/HIS-MALAYSIA.pdf
- Zainudin EN, Mohammad KA, Aris A, Shahdan IA. Vaccination: influencing factors and view from an Islamic perspective. IIUM Med J Malaysia. 2018;17:1–8.
- World Health Organization (WHO). WHO solidarity trial – accelerating a safe and effective COVID-19 vaccine. Update on WHO solidarity trial – accelerating a safe and effective COVID-19 vaccine. [accessed 2021 Aug 4]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-trial-accelerating-a-safe-and-effective-covid-19-vaccine
- Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29(38):6472–84. doi:10.1016/j.vaccine.2011.06.107.
- Brien S, Kwong JC, Buckeridge DL. The determinants of 2009 pandemic A/H1N1 influenza vaccination: a systematic review. Vaccine. 2012;30(7):1255–64. doi:10.1016/j.vaccine.2011.12.089.
- Yeung MP, Lam FL, Coker R. Factors associated with the uptake of seasonal influenza vaccination in adults: a systematic review. J Public Health (Bangkok). 2016;38(4):746–53. doi:10.1093/pubmed/fdv194.
- Takahashi O, Noguchi Y, Rahman M, Shimbo T, Goto M, Matsui K, et al. Influence of family on acceptance of influenza vaccination among Japanese patients. Fam Pract. 2003;20(2):162–66. doi:10.1093/fampra/20.2.162.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi:10.1038/s41591-020-1124-9.
- Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, Hasan MT, Sessou P, Ditekemena JD, Amodan BO, Hosseinipour MC et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low-and middle-income countries. Vaccines. 2021;9(5):515. doi:10.3390/vaccines9050515.
- Mein SA. COVID-19 and health disparities: the reality of “the Great Equalizer”. J Gen Intern Med. 2020;35(8):2439–40. doi:10.3390/vaccines9050515.
- Liu L, Miller HJ, Scheff J, Yang C. The impacts of COVID-19 pandemic on public transit demand in the United States. PloS One. 2020;15(11):e0242476. doi:10.1371/journal.pone.0242476.
- Sun GW, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49(8):907–16. doi:10.1016/0895-4356(96)00025-X.
- Sourial N, Vedel I, Le Berre M, Schuster T. Testing group differences for confounder selection in nonrandomized studies: flawed practice. Can Med Assoc J. 2019;191(43):E1189–93. doi:10.1503/cmaj.190085.
- Nunnally J, Bernstein L. Psychometric theory. New York: McGraw-Hill Higher, INC.; 1994.
- Bland J, Altman D. Statistics notes: Cronbach’s alpha. Bmj. 1997;314(7080):275. doi:10.1136/bmj.314.7080.572.
- DeVellis R. Scale development: theory and applications: theory and application. California: Sage; 2003.
- Hinton PR, McMurray I, Brownlow C. SPSS explained. New York: Routledge; 2014 p. 364.
- Independent. Malaysia government tells those who choose not to get Covid vaccine: ‘we will make life very difficult’. [accessed 2022 Jan 16]. https://www.independent.co.uk/asia/southeast-asia/covid-malaysia-unvaccinated-health-ministry-b1940110.html
- Statista. Vaccination rate against COVID-19 Malaysia 2022, by state. [accessed 2022 Jan 16]. https://www.statista.com/statistics/1270638/malaysia-covid-19-vaccination-rate-by-state/
- The Edge Markets. Covid-19: 216,668 vaccine doses dispensed on Jan 7, 32.3% of Malaysian adults boosted. [accessed 2022 Jan 16]. https://www.theedgemarkets.com/article/covid19-216668-vaccine-doses-dispensed-jan-7-323-malaysian-adults-boosted