ABSTRACT
This study aimed to estimate the disease burden and health-related quality of life (HRQOL) among patients with severe hand, foot, and mouth disease (HFMD) in Jiangsu Province, China. We analyzed the surveillance data of HFMD cases in Jiangsu Province from 2009 to 2020. Moreover, a cross-sectional study was conducted in Nanjing and Suzhou, China, between January 2017 and May 2018. Patients with severe HFMD and their parents were recruited from selected hospitals. Questionnaires and hospital management systems were used to collect data on direct economic burden. The HRQOL of children was assessed using the TNO-AZL Preschool Quality of Life (TAPQOL) scale. A total of 1,348,737 confirmed cases of HFMD were reported to the NNDRS in Jiangsu province during 2009–2020. Of these, 9,622 were severe cases, with 62 (.64%) of these being fatal. From January 2017 to May 2018, data was collected from 362 severe HFMD cases using a structured questionnaire. The median per capita direct economic burden was RMB 16142.88, and was associated with the region and length of hospital stay (P < .05). The direct economic burden for all cases of severe HFMD in Jiangsu province between 2017 and 2018 was approximately RMB 16.64 million. Finally, the median (IQR) of the TAPQOL scale for children with severe HFMD was 69.23 (56.20, 82.27). Severe HFMD infection is a relatively large burden for individuals, and the burden of EV-A71 infection was seen to be even greater for the population. Prevention of severe HFMD should strengthen hygiene habits and targeted measures for EV-A71 vaccination.
Introduction
Hand, foot, and mouth disease (HFMD) is a common infectious disease that predominantly affects children younger than 5 years of age. It is mainly caused by enterovirus 71 (EV-A71) and Coxsackie virus A16 (CV-A16).Citation1 However, some patients may become severely ill, with neurological or cardiopulmonary complications, and even death.Citation2,Citation3 In the past few decades, the largest outbreaks of HFMD have occurred in the Asian-Pacific region, including countries such as Malaysia, Singapore, and Vietnam.Citation4-8 In China, since HFMD was included in the management of Category C statutory infectious diseases in May 2008, its incidence rate and the number of confirmed cases have been the first among statutory reported infectious diseases.Citation9 Moreover, the EV-A71 vaccine launched in 2016 seems to have varying degrees of impact on the prevalence and pathogenic composition of HFMD.Citation10-13 One study indicated that a dramatic decrease in EV-A71 cases was observed, although the total cases remained high.Citation12 Overall, HFMD has caused serious economic and social burdens and has become an important public health problem that cannot be ignored.
From 2008 to 2018, a total of 157, 065 cases of severe HFMD were reported in China, with a severe case proportion of .76% and a severity-fatality rate of 2.34%.Citation14 Meanwhile, one study has pointed out that patients with severe HFMD are more likely to have a lower socioeconomic status and suffer a heavy economic burden.Citation15 Living with severe HFMD can carry a huge financial burden on individuals and families. In addition, severe HFMD can adversely affect the physical and mental health, as well as the quality of life among children. However, most of the existing studies focus on the analysis of epidemiological characteristics and related factors, such as the incidence of HFMD, or evaluate vaccine effectieness.Citation10,Citation14,Citation16,Citation17 Only a few studies have assessed the economic burden and health-related quality of life (HRQOL) among children with severe HFMD from 2011 to 2013.Citation18,Citation19 These studies indicated that higher economic burden and loss of disability-adjusted life years (DALYs) were associated with EV-A71 infection and longer disease duration.Citation18,Citation19 Studies on the disease burden of severe HFMD, especially economic burden, and studies regarding HRQOL among children with severe HFMD are insufficient.
Therefore, this study aimed to (1) analyze the incidence trend of HFMD and the pathogenic composition of severe HFMD in Jiangsu Province from 2009 to 2020; (2) estimate the economic burden of severe HFMD and the sociodemographic factors associated with the economic burden; and (3) assess the HRQOL among children with severe HFMD and the sociodemographic factors associated with HRQOL. We hope to provide a scientific basis for the rational allocation of medical resources, and prevention and control strategy establishment for HFMD.
Materials and methods
Case definitions
The clinical diagnostic criteria for severe HFMD were based on the “Guidelines for the Diagnosis and Treatment of Hand, Foot, and Mouth Disease (2010 Edition)” by the Ministry of Health of China.Citation20 Patients with severe HFMD mainly suffered from neurological damage, respiratory function involvement, circulatory dysfunction, and other symptoms. The diagnostic criteria for laboratory-confirmed cases were: (1) Enterovirus (CV-A16, EV-A71, etcetera.) specific nucleic acid test was positive; (2) Enterovirus was isolated and identified as EV-A71, CV-A16, or another enterovirus that can cause HFMD.
Epidemiological, economical, and health-related quality of life data collection
Data on HFMD cases from 2009 to 2020 were obtained from the National Noticeable Disease Reporting System (NNDRS) established by the Chinese Center for Disease Control and Prevention. Basic demographic and diagnostic information and etiological results of HFMD cases were collected via the NNDRS.
Data was collected from patients with severe HFMD who were treated at Nanjing Children’s Hospital and Suzhou Children’s Hospital in Jiangsu Province from January 2017 to May 2018. The data collected referred to economic burden and related to quality of life through retrospective and prospective investigations. Information regarding direct non-medical costs, including accommodation and diet, transportation, and nutrition costs, were collected in detail. The HRQOL of patients with severe HFMD was assessed using the TAPQOL scale. The TAPQOL scale not only has acceptable reliability and validity, but has also been previously used in other countries,Citation21-23 as well as in ChinaCitation24 Moreover, the TAPQOL scale consists of 43 items and covers the 12 dimensions of sleep, appetite, lungs, stomach, skin, motor functioning, communication, social functioning, problem behavior, anxiety, positive mood, and vitality. Items in each dimension were assigned points according to the answer selection. The sum of the score of each dimension was finally transformed linearly to a 0–100 domain score, in which a higher score meant a better HRQOL.Citation21 Investigations were conducted through patient telephone follow-ups or face-to-face surveys.
This study was approved by the Ethics Committee of the Jiangsu Provincial Center for Disease Control and Prevention (JSJK2016-B008-01).
Quality control and statistical analysis
Data from the questionnaires were entered into EpiData 3.1 software, and all data were entered twice. The missing data were completed using multiple imputation methods.Citation25 The proportion of missing data for variables ranged from .55%–14.09%. Sensitivity analysis revealed no statistically significant differences. The annual economic burden of the patients with HFMD in this study was converted to the 2018 level at a discount rate of 5%.Citation26 Descriptive analysis was performed using the mean and standard deviation (SD), median and interquartile range (IQR), and composition ratio.
In univariate analysis, the Wilcoxon rank sum test was used to compare two groups of non-normally distributed data, and the Kruskal–Wallis H test was used for the comparison of multiple groups. Multivariate analysis was performed using multiple linear stepwise regression analysis. The independent variables included gender, age, region, and the number of days in hospital. The specific assignment of each independent variable is presented in . The (β) coefficient and its 95% confidence interval (CI) of each variable were estimated to identify the influencing factors of direct economic burden and the total score of the TAPQOL scale, respectively. As described in a previous study,Citation27 the sampling distribution of the sample mean approximated a normal distribution when the sample size was sufficient (>30). Therefore, the population mean was roughly replaced by the sample mean to estimate the total economic burden.
Table 1. Assignment of independent variables
All statistical analyses were performed using Excel 2016, SPSS software, and R software. A two-sided P value of <.05 was considered statistically significant.
Results
The incidence of HFMD cases in Jiangsu Province
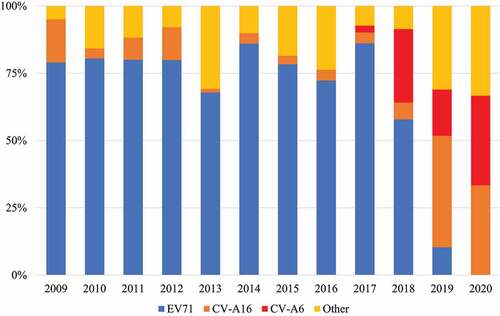
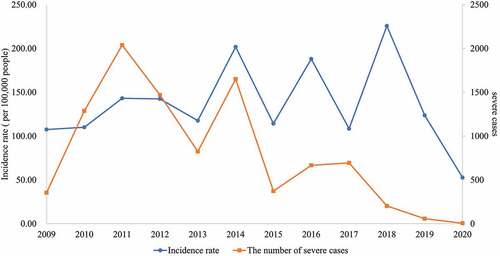
A total of 1,348,737 confirmed cases of HFMD were reported to the NNDRS in Jiangsu province during 2009–2020. Of these, 9,622 were severe cases. Among the severe cases, 62 (.64%) were fatal. During the 12 years, the incidence rate of HFMD remained relatively stable overall, except for a sharp decline in 2020. However, the number of severe HFMD cases was relatively high between 2010 and 2014. In contrast, a gradual decline in the number of severe HFMD cases have seen since 2015. It is particularly worth mentioning that the number of severe HFMD cases fell below 60 during 2019–2020. In addition, the number of deaths from HFMD was relatively small in the Jiangsu Province (, Supplementary 1).
Figure 1. Trends in the incidence rate and the number of severe cases of hand, foot, and mouth disease in Jiangsu Province from 2009 to 2020.
The primary pathogen type causing severe HFMD was the EV-A71 pathogen from 2009 to 2018 (). The EV-A71 pathogen had suddenly decreased since 2018, with the proportion being zero in 2020. Furthermore, the Coxsackie virus A6 (CV-A6) pathogen appeared in severe HFMD cases in 2017, and the proportion was gradually increased. The CV-A16 pathogen has always been one of the pathogens causing severe HFMD, and together with the CV-A6 pathogen, they gradually became the main types of pathogens causing severe HFMD from 2019 to 2020.
Direct economic burden of severe HFMD and influencing factors
Direct economic burden of severe HFMD
A total of 362 of the patients with severe HFMD were included in the analysis between January 2017 and May 2018 (, Supplementary 1). There were no deaths. The direct economic burden totaled RMB 6713946.39, of which 83.16% were direct medical costs and 16.84% were direct non-medical costs ( and ). The median of per capita direct economic burden was RMB 16142.88. Meanwhile, the reimbursed costs were RMB 3461690.64, which accounted for 61.96% of the direct medical costs. Drug costs accounted for the largest costs in direct medical costs (40.40%), while accommodation and diet costs accounted for the largest costs in direct non-medical costs (45.25%) (Supplement 1). In addition, all patients were hospitalized for a total of 3960 days, with a median of 10.00 days, The median of hospitalization cost per capita was RMB 1324.19 per day.
Figure 3. The composition of direct economic burden of patients with severe hand, foot, and mouth disease in Nanjing and Suzhou.
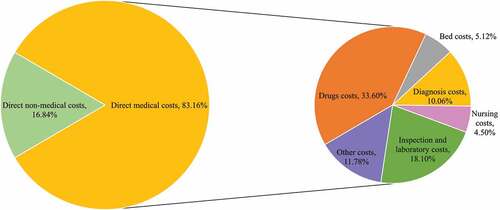
Table 2. The cost of patients with severe hand, foot, and mouth disease in Nanjing and Suzhou from January 2017 to May 2018 (RMB)
The comparisons between the groups demonstrated that the differences in gender and age of direct medical costs, direct non-medical costs, and direct economic burden were not statistically significant (P > .05). However, the direct medical costs, direct non-medical costs, and direct economic burden in Nanjing were significantly higher (P < .001) than those in Suzhou ().
Influencing factors of direct economic burden
Since the direct economic burden data did not conform to the normal distribution (P < .001) and was heavily positively skewed, the 1/x transformation was adopted for data conversion. Then the normality test results showed that P = .211. Subsequently, multivariate analysis was performed on the direct economic burden of severe HFMD patients using multiple linear stepwise regression analysis. Gender, age, region, and number of days in the hospital were analyzed in the regression model. However, only the variable of the region (β=−.45, P < .001) and the number of days in the hospital (β=−.15, P = .003) had statistically significant effects on the direct economic burden of patients with severe HFMD. The regression model was statistically significant (F = 78.76, adjusted R2 = .582). The specific results are shown in .
Table 3. Multi-Factor analysis of direct economic burden of patients with severe hand, foot, and mouth disease
The estimated direct economic burden of Jiangsu Province from 2017 to 2018
There were 897 cases of severe HFMD in Jiangsu Province between 2017 and 2018 (Supplementary 1). The mean and standard deviation (SD) of the direct economic burden, direct medical costs, and direct non-medical costs of 362 cases of severe HFMD were RMB 18546.81 ± 8674.94, RMB 15423.68 ± 7614.43, and RMB 3123.13 ± 2623.68, respectively. According to the estimation method described in the Statistical Analysis section, the overall average of the economic burden of severe HFMD was estimated to be RMB 18546.81, RMB 15423.68, and RMB 3123.13, respectively. Thus, the direct economic burden, direct medical costs, and direct non-medical costs of 897 severe cases in Jiangsu Province between 2017 and 2018 were approximately RMB 16.64 million, RMB 13.84 million, and RMB 2.8 million, respectively.
Health-related quality of life among patients with severe HFMD
As shown in , the median of the TAPQOL scale for patients with severe HFMD was 69.23, and the interquartile range was (56.20, 82.27). The highest median score in each dimension of the scale were “lungs” and “anxiety” (100.00) and the lowest were “social functioning” and “liveliness” (50.00).
Table 4. The TAPQOL scale score of patients with severe hand, foot, and mouth disease
The comparisons between the groups revealed that the differences in gender and age of the scale and the score of each dimension were not statistically significant (P > .05). There were statistically significant differences in the region of the score of some dimensions as follows: “appetite,” “lungs,” “stomach,” “skin,” and “motor functioning” (P < .05).
Discussion
This study found that the number of severe cases of HFMD showed a downward trend, especially from 2016 to 2020. The main pathogen causing severe HFMD changed from EV-A71 between 2009 and 2016 to non-EV-A71 (CV-A16, CV-A6, etc.) from 2017 to 2020. The direct economic burden, direct medical costs, and direct non-medical costs of severe HFMD were RMB 6713946.39, RMB 5583372.18, and 1130574.21, respectively. Meanwhile, the direct economic burden, direct medical costs, and direct non-medical costs of children with severe HFMD in Nanjing were higher than those in Suzhou. It was further estimated the direct economic burden, direct medical costs, and direct non-medical costs for 897 cases of severe HFMD in Jiangsu province between 2017 and 2018 were approximately RMB 16.64 million, RMB 13.84 million, and RMB 2.8 million, respectively. Finally, the median (IQR) of the total score of the TAPQOL scale for children with severe HFMD was 69.23 (56.20, 82.27). The total TAPQOL score was not statistically related to age, gender, and region.
Numerous studies revealed that EV-A71 was the main pathogen causing severe HFMD.Citation1,Citation2,Citation5,Citation28,Citation29 The epidemic of EV-A71 cases presented a certain periodicity, with an epidemic peak every 2–3 years.Citation14 Similar results were shown before 2016. However, after 2016, the predominant serotype of the pathogen causing severe HFMD in Jiangsu Province has changed, and this epidemic pattern is no longer present. This change may be due to the administration of the EV-71 vaccine. Since 2016, Jiangsu Province began administering EV-A71 vaccinations, and the overall vaccination rate for children in the birth cohort reached 19.63–28.63% from 2016 to 2019 (Supplement 1). This greatly reduced the prevalence of EV-A71 and the incidence of severe HFMD.Citation30 On the other hand, this may be due to the natural law of different conversion of the dominant serotypes of enteroviruses in susceptible populations. In addition, there was a significant decrease in the incidence rate of HFMD in 2020. Such a significant change was more attributable to the increase in public awareness of the prevention and control of infectious diseases due to the impact of the coronavirus disease 2019 (COVID-19) epidemic.Citation31,Citation32 Basic prevention and control measures such as frequent hand washing, wearing masks, and maintaining a certain degree of social distancing led to a reduction in the number of reported cases of common HFMD and severe HFMD in 2020.
Information on the economic burden of HFMD can support decision-makers in formulating and implementing intervention strategies, especially those regarding vaccine resources. The results of this study showed that the direct economic burden of 362 patients with HFMD was RMB 613943.39. The median of the per capita direct economic burden was RMB 16142.88, accounting for 27.22% (RMB 59308 in NanjingCitation33 and 25.43% (RMB 63481 in SuzhouCitation33 of the disposable income of local residents in 2018, respectively, which was higher than the direct economic burden of patients with severe HFMD previously reported in Xi’an and Shanghai.Citation34,Citation35 However, it was comparable to the direct economic burden reported by Nanjing and Qingdao.Citation36,Citation37 Moreover, the study revealed that longer the hospital stay leads to higher direct economic burden, direct medical costs, and direct non-medical costs in patients. This was not only in line with our outcome predictions but also consistent with the conclusions of other studies.Citation19 The direct economic burden, direct medical costs, and direct non-medical costs of patients in Nanjing were higher than those of patients in Suzhou. This may be related to the different factors that affect economic burden, such as economic development, consumption level, and price level of the region where the patients with severe HFMD were located. Meanwhile, direct medical costs (83.16%), drug costs (40.40%), and accommodation and diet costs (45.25%) accounted for the largest proportions of direct economic burden, direct medical costs, and direct non-medical costs, respectively. Severe HFMD has caused serious economic burdens on society and families of patients, especially relating to direct medical costs. A previous study revealed that the socioeconomic status of the families of patients with severe HFMD may be lower, and that they may suffer a heavy economic burden.Citation15 Poor families are therefore more likely to suffer a heavier burden of disease. In addition, the results also indicated that reimbursement costs accounted for 61.96% of hospitalization costs. This reminds us that in addition to implementing effective measures for the prevention and control of HFMD, more attention should be devoted to establishing scientific and effective medical insurance systems to effectively reduce the burden of disease for patient and their families.
The results of this study indicated that children with severe HFMD had lower TAPQOL scores. Except for “lungs”, “motor functioning”, and “anxiety”, the other scores were lower than those of healthy children observed in previous studies.Citation24 In a Chinese study, which also used the TAPQOL scale, the scores of children with CV-A16 infection were also lower than those of healthy children.Citation24 In previous studies on the HRQOL among patients with HFMD, the indicators used were DALYs or quality-adjusted life years (QALY).Citation18,Citation19 Due to different measurement methods and indicators, our results are not directly comparable to previous study results. However, it can be inferred that HFMD severely impairs quality of life among patients. Moreover, children with severe HFMD had the poorest HRQOL in the “social functioning” and “vitality” domains (50.00). We speculated that the severe illness causes children to lose their past vitality. Direct changes in child vitality were noticed by parents as seen in the information gathered. The study also found that the HRQOL among patients with severe HFMD was not related to gender and age, and was only slightly different in the region. It may be that the age of onset among children was generally low. The exposure conditions of the surrounding environment were similar, and the subjective feelings of the parents toward their children were also similar. Overall, this study emphasizes the adverse effects of severe HFMD to HRQOL among children. More attention should be paid to restoring quality of life and the improving of mental health.
This study had some limitations that should be considered when interpreting the findings. Firstly, this study was based on a questionnaire survey of HFMD cases conducted in hospitals, and other cases may have been missed. Incomplete investigations could lead to biased estimates of disease burden. Secondly, the comparison can be made only when the same discount rate is converted into the cost simultaneously. The cost of this study was only a rough comparison compared to the cost of other studies in order to provide a reasonable basis for inference. Thirdly, in this study, indirect costs and intangible costs were not calculated, and the assessment of the economic burden of severe HFMD had its own limitations. Follow-up studies should conduct a systematic investigation to comprehensively evaluate the heavy economic burden of severe HFMD. Fourthly, the collection of information on influencing factors such as sociodemographic and clinical symptoms of the cases was not comprehensive enough. Therefore, the analysis of the influencing factors in this paper is not sufficiently in-depth enough, and follow-up research needs to be supplemented and improved. Fifthly, the “motor functioning,” “social functioning,” and “communication” dimensions of the TAPQOL scale were only appropriate for children aged 18 months and older, while the rest of the nine scales were still applicable to children younger than 18 months.Citation38 Therefore, the assessment of HRQOL for patients younger than 18 months of age may be biased. Sixthly, the TAPQOL scale was completed by the parents of children infected with severe HFMD rather than the children themselves. There were a few differences between the views of the children and their parents. As some point, parents were unclear about their child’s illness and related circumstances. Therefore, the quality of the investigation may have been affected. However, for children who could not complete the scale independently, parents were still regarded as a good source of information. Finally, more effort is needed in sampling‐size selection and survey methods.
Conclusion
The burden of severe hand, foot, and mouse disease in Jiangsu Province is significant, and the health-related quality of life among patients is poor. Therefore, basic prevention and control measures such as frequent hand washing, wearing masks, and maintaining a certain social distance, as well as targeted measures for vaccination, should be vigorously promoted. Moreover, scientific and effective medical subsidies and reimbursement policies should be established to reduce the financial burden on patients. Finally, efforts should be made to improve the health-related quality of life among children.
Author contributions
XFZ and Hui Jin designed the study. YH, Hong Ji, and WQS conducted the literature search and review. WQS, LLC, HH, ZZ, and HMS collected and extracted the data. YH, CXD, and TTC analyzed the data. Hui Jin, XFZ, YH, and Hong Ji interpreted the results. All authors critically revised the manuscript for important intellectual content.
Informed consent statement
Informed consent was obtained from all participants.
Supplemental Material
Download MS Word (438.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2049168
Additional information
Funding
References
- Xing W, Liao Q, Viboud C, Zhang J, Sun J, Wu JT, Chang Z, Liu F, Fang VJ, Zheng Y, et al. Hand, foot, and mouth disease in China, 2008–12: an epidemiological study. Lancet Infect Dis. 2014;14:308–7. doi:10.1016/S1473-3099(13)70342-6.
- Huang CC, Liu CC, Chang YC, Chen CY, Wang ST, Yeh TF. Neurologic complications in children with enterovirus 71 infection. N Engl J Med. 1999;341:936–42. doi:10.1056/NEJM199909233411302.
- Ooi MH, Wong SC, Lewthwaite P, Cardosa MJ, Solomon T. Clinical features, diagnosis, and management of enterovirus 71. Lancet Neurol. 2010;9:1097–105. doi:10.1016/S1474-4422(10)70209-X.
- Sabanathan S, Tan le V, Thwaites L, Wills B, Qui PT, Rogier van Doorn H. Enterovirus 71 related severe hand, foot and mouth disease outbreaks in South-East Asia: current situation and ongoing challenges. J Epidemiol Community Health. 2014;68:500–02. doi:10.1136/jech-2014-203836.
- Solomon T, Lewthwaite P, Perera D, Cardosa MJ, McMinn P, Ooi MH. Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis. 2010;10:778–90. doi:10.1016/S1473-3099(10)70194-8.
- Chan LG, Parashar UD, Lye MS, Ong FG, Zaki SR, Alexander JP, Ho KK, Han LL, Pallansch MA, Suleiman AB, et al. Deaths of children during an outbreak of hand, foot, and mouth disease in sarawak, malaysia: clinical and pathological characteristics of the disease. for the Outbreak Study Group. Clin Infect Dis. 2000;31:678–83. doi:10.1086/314032.
- Chan KP, Goh KT, Chong CY, Teo ES, Lau G, Ling AE. Epidemic hand, foot and mouth disease caused by human enterovirus 71, Singapore. Emerg Infect Dis. 2003;9:78–85. doi:10.3201/eid1301.020112.
- Khanh TH, Sabanathan S, Thanh TT, Thoa le PK, Thuong TC, Hang V, Farrar J, Hien TT, Chau NVV, van Doorn HR, et al. Enterovirus 71–associated hand, foot, and mouth disease, Southern Vietnam, 2011. Emerg Infect Dis. 2012;18:2002–05. doi:10.3201/eid1812.120929.
- Ji H, Fan H, Lu PX, Zhang XF, Ai J, Shi C, Huo X, Bao C-J, Shan J, Jin Y, et al. Surveillance for severe hand, foot, and mouth disease from 2009 to 2015 in Jiangsu province: epidemiology, etiology, and disease burden. BMC Infect Dis. 2019;19:79. doi:10.1186/s12879-018-3659-7.
- Wang J, Jiang L, Zhang C, He W, Tan Y, Ning C. The changes in the epidemiology of hand, foot, and mouth disease after the introduction of the EV-A71 vaccine. Vaccine. 2021;39:3319–23. doi:10.1016/j.vaccine.2021.05.009.
- Du Z, Huang Y, Lawrence WR, Xu J, Yang Z, Lu J, Zhang Z, Hao Y. Leading enterovirus genotypes causing hand, foot, and mouth disease in Guangzhou, China: relationship with climate and vaccination against EV71. Int J Environ Res Public Health. 2021;18:292. doi:10.3390/ijerph18010292.
- Meng XD, Tong Y, Wei ZN, Wang L, Mai JY, Wu Y, Luo Z-Y, Li S, Li M, Wang S, et al. Epidemical and etiological study on hand, foot and mouth disease following EV-A71 vaccination in Xiangyang, China. Sci Rep. 2020;10:20909. doi:10.1038/s41598-020-77768-7.
- Han Y, Chen Z, Zheng K, Li X, Kong J, Duan X, et al. Epidemiology of hand, foot, and mouth disease before and after the introduction of enterovirus 71 vaccines in Chengdu, China, 2009-2018. Pediatr Infect Dis J. 2020;39:969–78.
- Ren M, Cui J, Nie T, Liu F, Sun J, Zhang Y, Chang Z. Epidemiological characteristics of severe cases of hand, foot, and mouth disease in China, 2008-2018. Chin J Epidemiol. 2020;41:1802–07.
- Wang K, Wang F, Li Y, Liang L, Cui P, Han S, et al. Association of clinical severity with family affluence-based socioeconomic status among hospitalized pediatric hand, foot, and mouth disease patients in Henan, China: a single hospital-based case series study. Open Forum Infect Dis. 2021;8:ofab150.
- Jiang L, Jiang H, Tian X, Xia X, Huang T. Epidemiological characteristics of hand, foot, and mouth disease in Yunnan Province, China, 2008-2019. BMC Infect Dis. 2021;21:751.
- Huang R, Wei J, Li Z, Gao Z, Mahe M, Cao W. Spatial-Temporal mapping and risk factors for hand foot and mouth disease in northwestern inland China. PLoS Negl Trop Dis. 2021;15:e0009210.
- Gan ZK, Jin H, Li JX, Yao XJ, Zhou Y, Zhang XF, et al. Disease burden of enterovirus 71 in rural central China: a community-based survey. Hum Vaccin Immunother. 2015;11:2400–05.
- Zheng Y, Jit M, Wu JT, Yang J, Leung K, Liao Q, et al. Economic costs and health-related quality of life for hand, foot and mouth disease (HFMD) patients in China. PLoS One. 2017;12:e0184266.
- China MoHotPsRo. Hand, foot, and mouth disease diagnosis and treatment guidelines (2010 edition). Chin Pract J Rural Doctors. 2012;19:9–11.
- Fekkes M, Theunissen NC, Brugman E, Veen S, Verrips EG, Koopman HM, et al. Development and psychometric evaluation of the TAPQOL: a health-related quality of life instrument for 1-5-year-old children. Qual Life Res. 2000;9:961–72.
- Lee CF, Chien LY, Ko YL, Chou YH, Tai CJ, Liou YM. Development and psychometric properties of the Chinese language version of the TAPQOL: a health-related quality of life instrument for preschool children. Int J Nurs Stud. 2005;42:457–65.
- Rajmil L, Abad S, Sardon O, Morera G, Pérez-Yarza EG, Moreno A, et al. Reliability and validity of the Spanish version of the TAPQOL: a health-related quality of life (HRQOL) instrument for 1- to 5-year-old children. Int J Nurs Stud. 2011;48:549–56.
- Yao Xuejun LJ, Jin P, Zhang X, Zhu F. Analysis of the reliability and validity of TNO-AZL preschool children quality of life. Jiangsu J Prev Med. 2018;29:151-153+230.
- van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011 Dec;45:1-67.
- Phillips M, Shepard DS, Lerman SJ, Cash RA, Whitesell PH. Estimating costs for cost-effectiveness analysis. Guidelines for managers of diarrhoeal diseases control programmes. 1988.
- Cui T, Zhang X, Wang Q, Yue N, Zheng M, Wang D, et al. Disease burden concerning hepatitis E-infected inpatients in Jiangsu province, China. Vaccine. 2020;38:673–79.
- Liu SL, Pan H, Liu P, Amer S, Chan TC, Zhan J, et al. Comparative epidemiology and virology of fatal and nonfatal cases of hand, foot and mouth disease in mainland China from 2008 to 2014. Rev Med Virol. 2015;25:115–28.
- Wang Y, Feng Z, Yang Y, Self S, Gao Y, Longini IM, et al. Hand, foot, and mouth disease in China: patterns of spread and transmissibility. Epidemiology. 2011;22:781–92.
- Head JR, Collender PA, Lewnard JA, Skaff NK, Li L, Cheng Q, et al. Early evidence of inactivated enterovirus 71 vaccine impact against hand, foot, and mouth disease in a major center of ongoing transmission in China, 2011-2018: a longitudinal surveillance study. Clin Infect Dis. 2020;71:3088–95.
- Sun X, Xu Y, Zhu Y, Tang F. Impact of non-pharmaceutical interventions on the incidences of vaccine-preventable diseases during the COVID-19 pandemic in the eastern of China. Hum Vaccin Immunother. 2021;17:4083-4089.
- Kataoka SY, Kataoka Y, Tochitani K, Miyakoshi C, Yamamoto Y. Influence of anti-COVID-19 policies on 10 pediatric infectious diseases. Pediatr Int. 2021.doi:10.1111/ped.14958.
- Jiangsu Provincial Bureau of Statistics. Jiangsu statistical yearbook. [accessed 2022 Jan 16]. http://tj.jiangsu.gov.cn/col/col76362/index.html.
- Bai YW, Yang F, Chen Z, Chen B. Research on economic burden and influencing factors of hand-foot-mouth disease in Xi’An, 2018. Chin J Sch Health. 2020;41:1384–87.
- Wang ZL, Xia AM, Li YF, Su HL, Zhan LW, Chen YP, et al. Socioeconomic burden of hand, foot and mouth disease in children in Shanghai, China. Epidemiol Infect. 2016;144:138–43.
- Shl H-L-L, Qin X-H. Investigation on economic burden among families of 90 children with severe hand, foot and mouth disease. Guangxi Med J. 2020;42:357–59.
- Jia J, Sd P, Xian-Jun W, Xia W, Fa-Chun J. Investigation on economic burden caused by severe hand-foot-mouth disease in Qingdao,2014. Disease Surveillance. 2016;31:703–06.
- Tan LT, Nathan AM, Jayanath S, Eg KP, Thavagnanam S, Lum LCS, et al. Health-Related quality of life and developmental outcome of children on home mechanical ventilation in a developing country: a cross-sectional study. Pediatr Pulmonol. 2020;55:3477–86.