ABSTRACT
Background
Since 2008, Fujian province provided measles-rubella (MR) vaccine at 8 months followed by measles-mumps-rubella (MMR) vaccine at 18 months a one-dose mumps-containing-vaccine (MuCV) schedule. Several mumps outbreaks have occurred recently in Fujian. Serological surveillance can assess population immunity to mumps and identify risk factors for mumps.
Methods
We conducted a cross-sectional serosurvey of mumps IgG antibodies in the general population of Fujian Province in 2018 and compare results with a similar study conducted in 2009, when the routine schedule had no MuCV. We analyzed changes in mumps epidemiology after implementation of a one-dose MuCV vaccination strategy.
Results
Mumps seroprevalence was 78.6% (95% CI: 77.4–79.8), and the geometric mean concentration (GMC) of mumps antibodies was 245.8 IU/ml (95% CI:237.3–255.1). MuCV vaccination at 18 months resulted in increased seroprevalence and GMCs. Seroprevalence and GMCs varied by age, gender, and number of doses received. Except for children under 18 months, seroprevalence and GMCs were lowest among 10-15-year-olds. Each year after introduction of the one-dose MuCV vaccination policy, the highest incidence of mumps was among 4–6-year-olds and 9–15-year-olds, gradually shifting to older age groups.
Conclusion
A one-dose mumps-containing vaccine schedule does not provide sustained and stable mumps immunity in Fujian. To reduce the risk of mumps, we recommend supplementary vaccination of children without a history of receiving at least one MuCV dose or who are seronegative at 10–15 years of age.
Introduction
Mumps is a common childhood disease caused by mumps virus (MuV) infection.Citation1 MuV infects parotid glands leading to pain and swelling, but can also infect other tissues and organs, resulting in serious complications including encephalitis, meningitis, orchitis, myocarditis, pancreatitis, nephritis, and even death.Citation2 Mumps is frequently reported in China in school-age children younger than 15 years, particularly among 5–9 year-olds.Citation3,Citation4 Mumps is a vaccine-preventable disease, and almost all countries include mumps-containing vaccine (MuCV) in routine vaccination schedules. Widespread use of MuCV has dramatically decreased the incidence of mumps.Citation5 The most commonly used MuCV globally is trivalent live attenuated measles, mumps, and rubella (MMR) vaccine.Citation6 In China, MMR has been included in the national routine program for immunization since 2008.Citation7 MMR was introduced on 1 April 2008 in Fujian province. Subsequent to MMR introduction, children receive one dose of MMR vaccine without charge in a schedule of measles-rubella (MR) vaccine at 8 months followed by MMR vaccine at 18–24 months.Citation3
Mumps surveillance data show that the incidence of mumps in Fujian declined from 2009 to 2010 and then increased and remained high through 2015.Citation8 In spite of high MMR vaccination coverage, approximately 6,000 mumps cases were reported annually in Fujian in the past decade.Citation9–11 Some studies suggest that waning of vaccine-induced immunity is a cause of mumps outbreaks.Citation12,Citation13 Serological surveillance has a valuable role in assessing the level of immunity to mumps and may lead to identification of populations at increased risk for mumps outbreaks.Citation14 To assess population immunity, we conducted a large cross-sectional serosurvey of IgG antibody against MuV in Fujian province in 2018. We compared seroprevalence and antibody levels with seroprevalence and antibody levels from a similar study conducted in 2009, a decade earlier. The aim of our study was to evaluate protection from mumps in an era of a one-dose MuCV schedule and provide a reference for adjustment of vaccination strategy for prevention and control of mumps in China.
Materials and methods
Epidemiological data
Mumps is a class C infectious disease in China, requiring reporting of all diagnosed cases to the National Notifiable Diseases Reporting System (NNDRS) of the Chinese Center for Disease Control and Prevention (China CDC). We obtained all mumps reports from Fujian and used the date of onset of illness as the date of the case. Incidences were calculated as numbers of cases per 100 000 total population per time period, using population data from the National Bureau of Statistics of China.
Serological surveys
In 2009 and 2018, two cross-sectional, population-based sero-surveillance studies were conducted in Fujian using identical sampling methods. Twenty-one counties in 10 cities were chosen at random. Two villages or communities were randomly selected from each county. A systematic sampling method was used to select individuals from each village/community stratifying on age and gender.
Individuals with fever, chronic infectious diseases, or who were immunosuppressed were excluded. In the 2009 serosurvey, 1,967 serum specimens were obtained, and in the 2018 serosurvey, 4,925 specimens were obtained. Subjects were stratified into 18 age groups: 0–7 months, 8–9 months, 10–12 months, 12–17 months, 1.5-year-olds, 2-year-olds, 3-, 4-, 5-, 6-7-, 7-, 8-, 9-, 10–15-, 15–20-, 20–30-, 30–40-, and 40–60-year-olds. MMR vaccination histories were obtained from questionnaires and the Fujian Provincial Vaccine and Immunization information system.
Laboratory assays
Sera were stored at −70°C before testing by Fujian CDC immunization program’s laboratory, which is a World Health Organization measles and rubella reference laboratory. Commercial mumps virus IgG ELISA kits (SERION ELISA classic, InstitutVirion\Serion GmbH, batch number: SAK.BX) were used to detect and quantify mumps specific IgG antibodies. ELISA results were expressed quantitatively as optical density (OD) measurements at 405 nm. IgG antibody concentrations (IU/ml) were calculated using the formula specified by the manufacturer. Concentrations greater than 100 IU/ml were considered positive, concentrations less than 100 IU/ml were considered negative. Samples with titers of between 90 IU/ml and 99 IU/ml were retested twice prior to categorizing as positive or negative.
Statistical analysis
Seroprevalence and geometric mean concentrations (GMCs) and 95% confidence intervals (95% CIs) of mumps IgG antibodies were calculated by region, gender, and age. P-values <0.05 were considered statistically significant. Statistically significant differences in seroprevalence and GMC by age, gender, and number of vaccine doses were assessed with Pearson’s χ2 and non-parametric tests, with significance levels of 0.05. SPSS 20.0 statistical software was used for all analyses.
Ethical review
Approval for the study was obtained from the Medical Ethics Committee of Fujian CDC. Written informed consent was provided by individuals or, for children, by parents. Participants were invited to anonymously fill out a questionnaire that included personal information, such as gender, age or date of birth, and date of sampling. All methods were carried out in accordance with the approved guidelines.
Results
2018 serosurvey
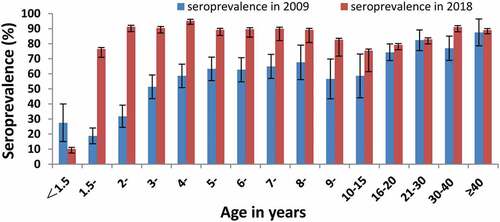
shows results of the 2018 serosurvey. Overall seroprevalence was 78.6% (95% CI:77.4–79.8). The seroprevalence among children <18 months was lowest: less than 10.0% at 8–9 months and 3.4% at 13–17 months. After 18 months (the age of MMR vaccination), seroprevalence increased, and was 95.2% (95% CI:92.8–97.3) at 4 years of age and remained high during the first 5–6 years after vaccination. Seroprevalence decreased to 75.4% (95% CI:71.6–79.4) at 10–15 years of age, and subsequently increase with age. Among individuals﹥20 years, who were born before MuCV introduction, seroprevalence gradually increased from 82.9% (95% CI 79.7–85.7) among 20–30-year-olds to 91.0% (95% CI 87.9–94.1) in the oldest age group.
Table 1. Seroprevalence and GMCs of mumps antibody by age, gender, and number of vaccine doses received in Fujian Province, China, 2018.
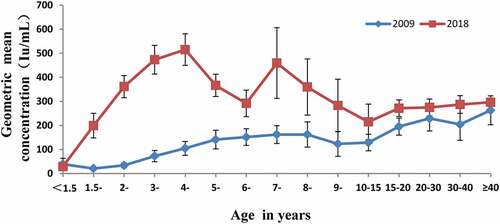
The overall GMC was 245.8 IU/ml (95% CI:237.3–255.1). Age-specific trends in GMC were similar to trends in seroprevalence, with GMCs lowest among children <18 months and highest (515.2 IU/mL) at 4 years, decreasing to 214.8 IU/mL at 10–15 years. GMCs in individuals﹥20 years were stable, ranging between 274.8 IU/mL and 296.5 IU/mL.
Seroprevalence among males was 77.3% (95% CI: 75.6–79.0) and among females was 79.7% (95% CI: 78.0–81.3), with respective GMCs of 235.5 (95% CI: 224.1–247.5) and 255.3 (95% CI: 244.0–267.1). Seroprevalence and GMCs significantly differed by gender (P = 0.039 and P = 0.023).
Among the 4,925 subjects, 50.0% received at least one dose of MuCV, and 37.2% were unaware of their vaccination status (most of whom were over 15 years of age). Among the 12.8% of subjects not vaccinated against mumps, most were not in age groups for whom MuCV was recommended. Seroprevalence and GMC differed significantly by vaccination status. Mumps seroprevalence and GMC of vaccinated cohorts were higher than that of unvaccinated cohorts. Seroprevalence and GMC of two-dose-vaccinated individuals were higher than one-dose-vaccinated individuals. Seroprevalence was 84.4% and the GMC was 274.2 IU/mL among subjects with no information about vaccination status.
Comparison with 2009 serosurvey
Seroprevalence in 2009 and 2018 had similarities and some differences. Children 1.5 to 2 years of age had significantly lower seroprevalence in the 2009 survey compared with the 2018 survey (). Other than children less than 18 months, seroprevalence in each age group was higher in 2018 than in 2009, and differences in seroprevalence narrowed with age, most notably among those over 30 years old. Seroprevalences in the 1.5–15-year age groups were significantly higher in 2018 than in 2009 (P < 0.001): 86.9% in 2018 versus 53.4% in 2009. Increased antibody levels in this age range were associated with the timing of the one-dose MuCV perio
shows GMCs by age group in 2009 and 2018. In 2009, GMCs tended to increase with age, but in 2018, GMC increased rapidly to 515.2 IU/mL, peaking among 4-year-olds, and then decreasing to 291.7 IU/mL among 6-year-olds. GMC increased to 459.2 IU/mL among 7-year-olds and then gradually declined to 214.8 IU/mL among 10-15-year-olds. Above 15 years of age, GMCs gradually increased with age, likely due to natural infection.
Mumps epidemiology from 2005 to 2019
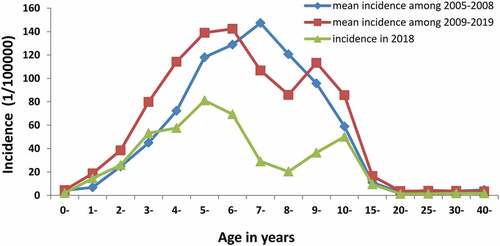
There were 90,922 cases of mumps reported in Fujian from 2005 to 2019 for a mean incidence of 16.3 per 100 000 individuals (). There were no mumps-associated deaths. More than 98% of cases were clinically diagnosed. There were 49,241 male cases and 32,542 female cases. The maximum incidence was 43.2 per 100 000 population in 2011, and the lowest incidence was 7.5 per 100 000 individuals in 2017. After introduction of MMR in 2008, the incidence increased until 2011 and rapidly decreased thereafter. During 2014–2019, the incidence remained around 8.0 per 100 000 individuals.
Table 2. Reported cases and incidence in 2005–2019, Fujian province, China.
Mumps did not vary by region in Fujian. Most of the cases occurred in densely populated areas such as schools and child-care institutions. Preschool children, non-local children, and students (3–15-years old) accounted for approximately 90% of reported cases. From 2005 to 2008, prior to introduction of MMR into EPI, the highest incidences of mumps were among 5–8-year-olds each year. After MMR introduction, two peak incidences were observed: 4–6 years old and 9–15 years old ().
Discussion
Our study showed that the overall seroprevalence of mumps in Fujian Province increased from 56.0% in 2009 to 78.6% in 2018 following the 2008 introduction of mumps vaccine as a component of MMR vaccine. Seroprevalences and GMCs in each age group in 2018 were higher than among corresponding age groups 2009, except for children under 18 months of age – the age at which mumps-containing MMR vaccine was recommended. These results imply that an immune barrier against mumps has been established during the 10 years since the introduction of MMR vaccine in Fujian.
The herd immunity threshold for mumps is 86%–92%, implying the need for very high coverage to prevent epidemics of mumps.Citation15 Mumps population immunity in Fujian is lower than the herd immunity threshold. The annual incidence of mumps in Fujian Province was 16.3 per 100 000 during 2005–2019, higher than the incidence rates in Shanghai and Jiangsu during the same period.Citation1,Citation16 People with low seroprevalence and high incidence of mumps have become a focus of attention in Fujian.
The age group with the lowest mumps seroprevalence was children less than 18 months of age. We found that mumps antibodies among infants declined rapidly after birth, similar to decreases in maternal antibodies to measles and rubella in infants.Citation17 Waaijenborg and colleagues found that maternal antibodies to mumps disappeared by 6–9 months of age.Citation18 Since MMR is administered at 18–24 months in Fujian, approximately 300,000 younger children are at risk for mumps infection. Despite this susceptibility, no mumps outbreaks have been reported in this age group. One likely reason is that after 10 years of routine MuCV vaccination, decreased circulation of mumps virus is indirectly protecting children too young to vaccinate.Citation19 In January 2020, the National Immunization Program updated the routine measles, mumps, rubella schedule to two doses of MMR - one at 8 months and a second dose at 18 months.Citation20 This will further enhance protection of children under 18 months from mumps.
After MMR is given at 18 months of age, mumps antibodies were successfully induced, increasing rapidly until 4 years of age. Subsequently, seroprevalence decreased to 75.4% among 10-15-year-olds. This finding is consistent with a cross-sectional survey of mumps IgG antibodies conducted in Shanghai in 2017.Citation14 In our study, seroprevalence and GMC in 4-year-old children were higher than in 2- and 3-year-olds because some children were not vaccinated with MMR by 2 years of age. Children needed to receive one dose of MMR before entering kindergarten at 3 years old, raising mumps immunity. GMCs in children aged 7–8 years old, as and show, have high seroprevalence and GMCs, which may be attributed to the implementation of vaccination certificate inspection before the admission to primary school and offering MMR to unvaccinated children.Citation1
In unvaccinated, naturally infected cohorts above 30 years of age, GMCs gradually increased with age until becoming stable. Several serological studies have demonstrated that mumps antibody levels decrease with time since vaccination.Citation19,Citation21 Our research is consistent with these observations and likely provides an explanation of frequent mumps outbreaks in children and adolescents.Citation22 The mumps vaccine component of MMR elicits a lower immune response than do the measles and rubella components.Citation23 Studies in Scandinavia document persistence of antibodies in children derived from the Jeryl Lynn mumps strain, with 73% seroconversion in Sweden after a single dose.Citation24 Ferrari and colleagues evaluated persistence of a protective antibody level for mumps among medical students who had been vaccinated during infancy or adolescence in Italy, finding that a significant proportion of the students lacked serological protection from mumps.Citation25
Three highly developed cities in China – Shanghai, Beijing, and Tianjin – have introduced two doses of MMR into their routine immunization program for several years.Citation26 Seroprevalence of zero-dose and one-dose children were significantly lower than among children who received two or three doses, indicating that a two-dose MMR schedule provides better humoral protection against mumps than a one-dose schedule.Citation14 In our study, we found that seroprevalence and GMC among two-dose MMR recipients were higher than among one-dose recipients, but difference in seroprevalence and GMC between the two groups were not statistically significant. Since Fujian used a one-dose MMR vaccination policy, most of the people who received two doses were non-local. Intervals between doses were long and antibody levels may be reduced. Some studies found that the decline of GMCs in the first 1–2 years after the second MMR dose is faster than that after the initial MMR dose.Citation19,Citation27 The global experience had demonstrated that prevention of mumps requires sustained high levels of MuCV coverage with more than one dose of the vaccine.Citation28
We found higher mumps seroprevalences and GMCs in females than in males. A cross-sectional population-based serosurvey in the Netherlands also found significantly higher seroprevalence of mumps antibodies in females.Citation19 Scepanovic and colleagues observed that females exhibited higher rates of seropositivity against most antigens, including mumps, compared with males.Citation29 One potential explanation may be that women have a more robust activation of their immune system, and therefore develop stronger immune responses to antigens.Citation30 This may be a reason why males appear to be more susceptible to mumps virus infection than females.
Comparison of the 2018 and 2009 Fujian serosurveys yielded several interesting results. Children﹤18 months who receive immunity from maternal antibody had rapidly declining antibody levels as the babies got older.Citation17,Citation31 Antibody levels among children﹤18 months in 2018 was significantly lower than among same-age children in 2009. However, this may have been related to the age distribution of the samples collected. More than 80% of the samples collected in 2018 were from infants aged 7–18 months, which have the lowest antibody levels of any age group.Citation19 show that in 2018, children 1.5 years old had a sharp increase in mumps antibodies after vaccination. Both seroprevalence and GMCs remained at high levels in the subsequent age cohorts until four years of age. After that, seroprevalence and GMC began to wane, especially in the 4–9 year group. By comparison, seroprevalence and GMCs increases slowly in these age groups in 2009, showing the effect of natural infection over time instead of vaccination in a discrete and short-time period. This finding also suggests a longer and stable duration of protection induced by natural infection compared vaccination, a phenomenon that was confirmed in an MMR study conducted in Luxembourg.Citation24
Compared with natural infection, vaccination can quickly and effectively reduce the incidence of mumps,Citation1,Citation14 leading to meaningful changes in the epidemiological pattern of mumps. After introduction of one dose of MMR in Fujian, we found two incidence peaks of mumps – at 4–6 years and 9–15 years. The peak incidence tended to gradually shift to older ages. This phenomenon is also being seen in other regions of China.Citation1,Citation17 Several explanations are possible. First, there are lower antibody levels at 5–6 years and 10–15 years age groups due to a one-dose schedule or lack of vaccination as an infant. Second, these age cohorts represent a huge population with very high contact rates in kindergarten, primary school, and senior high school. Such intense exposure may overcome vaccine-induced protection in students and lead to mumps outbreaks.Citation32 Sun and colleagues found that children who received a single dose of MMR vaccine in kindergarten, particularly 2-year-olds in northern Jiangsu province, China, were at high risk of mumps infection.Citation22 Mumps outbreaks occurred in campuses in Fujian Province in 2018, and the cases were mainly among 12–15 year olds.Citation10,Citation11 Finally, MuV has only one serotype but 12 distinct genotypes (A – L).Citation3 The circulating wild type MuV responsible for the recent sustained outbreaks differs from the vaccine genotype. In China, the F genotype is the most common viral strain, whereas the predominant S79 vaccine contains the Jeryl Lynn strain with the A genotype.Citation4 Although antibodies induced by the Jeryl Lynn strain were found to effectively neutralize other genotype strains, antibody levels in general were lower for this wild virus strain compared with the vaccine strain.Citation33 As mumps shifts to an older age groups there may be an increase of serious cases and complications.Citation34 Supplementary vaccination could be considered for children aged 10–15 years to improve protection against mumps and reduce the risk of complications.Citation35 Development of new vaccines against additional MuV genotypes should also be considered.
Our study has some limitations. First, most of the vaccination histories of subjects older than 15 years were unknown, which hindered understanding the relationship between mumps seroprevalence and vaccination. Second, we are unable to correlate sero-epidemiological data with the ages and MMR histories of confirmed mumps cases because more than 90% of the mumps cases were clinically diagnosed, and patient specimens and laboratory information were therefore not available.
Conclusions
Our study showed that immunity against mumps in Fujian is probably sufficient to prevent large outbreaks. Nevertheless, there is persistent lack of protective mumps antibody titers in a substantial percentage of individuals. Both GMCs and seroprevalences in children 10–15 years of age were low and were far less than the herd immunity threshold. Therefore, a one-dose MMR vaccine strategy may not provide effective humoral immunity against mumps. In 2020, the National Immunization Program introduced a two-dose MMR schedule (from the previous MR followed by MMR schedule), changing the schedule from one MuCV dose to two MuCV doses and lowering the initiation of mumps protection to 8 months of age. Based on our findings and additional evidence in the scientific literature, we recommend supplementary vaccination of children who are unable to demonstrate receiving at least one MuCV dose or who are seronegative at 10–15 years of age. Implementing this recommendation may help control mumps among adolescents and younger adults.
Author’s contributions
Weiyi Pan conceived and designed the study. Dong Li, Hairong Zhang, Weiyi Pan, Na You, Zhifei Chen, Xiuhui Yang, Hangsu Zhang, Yong Zhou, and Ningxuan Zheng experimental operation and data analysis. Dong Li and Hairong Zhang wrote the paper. All authors read and approved the manuscript.
Acknowledgments
We would like to express our deepest gratitude for all the unnamed participants in the study. The study is supported by Talent Training Project of Fujian Provincial Health Commission (2021GGB011), and the Fujian Provincial Science and Technology project (2015Y0049).
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- Liu Y, Hu Y, Deng X, Wang Z, Lu P, Ma F, Zhou M, Liu P, Min J. Seroepidemiology of mumps in the general population of Jiangsu province, China after introduction of a one-dose measles-mumps-rubella vaccine. Sci Rep. 2015;5(14660). doi:10.1038/srep14660.
- Su SB, Chang HL, Chen KT. Current status of mumps virus infection: epidemiology, pathogenesis, and vaccine. Int J Mol Sci. 2020;17:1. doi:10.3390/ijerph17051686.
- Cui A, Zhu Z, Hu Y, Deng X, Sun Z, Zhang Y, Mao N, Xu S, Fang X, Gao H, et al. Mumps epidemiology and mumps virus genotypes circulating in mainland China during 2013-2015. Plos One. 2017. doi:10.1371/journal.pone.0169561.
- Cui A, Zhu Z, Chen M, Zheng H, Liu L, Wang Y, Ma Y, Wang C, Fang X, Li P, et al. Epidemiologic and genetic characteristics of mumps viruses isolated in China from 1995 to 2010. Infect Genet Evoln. 2014;21:384–7. doi:10.1016/j.meegid.2013.1012.1005.
- Hviid A, Rubin S. Mühlemann K. Mumps. Lancet. 2008;371(9616):932–944. doi:10.1016/S0140-6736(1008)60419-60415.
- Sasaki H, Fukunaga T, Asano A, Yamanaka K, Oikawa K, Shibata N. Seroprevalence of anti-mumps virus IgG antibody titer and voluntary mumps vaccination coverage in young adults in Japan. Hum Vaccin Immunother. 2021;17(9):3153–3155. doi:10.1080/21645515.2021.1913967.
- Li R, Cheng S, Luo C, Rutherford S, Cao J, Xu Q, Liu X, Liu Y, Xue F, Xu Q, et al. Epidemiological characteristics and spatial-temporal clusters of Mumps in Shandong Province, China, 2005–2014. Scientific Reports. 2017: 7:46328doi: 10.46310.41038/srep46328.
- Dong L, Zhifei C, Xiuhui Y, Weiyi P, Qin W, Suhan Z, Ningxuan Z, Lifang H, Yong Z. Epidemiological and pathogenic characteristics of mumps in Fujian province, 2005-2017. Zhong Hua Liu Xing Bing Xue Za Zhi [Chinese Journal of Epidemiology]. 2018;39(10):1356. doi:10.3760/cma.j.issn.0254-6450.2018.10.013.
- Xiuhui Y, Huiri G, Yanyan S, Aihua H, Hongrong Z, Jiangyan X. Genetic characterization of the mumps virus isolated from an outbreak in Fujian. Chinese J Vaccines Immun. 2013;19:43–46.
- Dong L, Xiuhui Y, Zhifei C, Suhan Z, Ningxuan Z, Hongrong Z, and Yong Z. Pathogenic characteristics of mumps virus isolated from an outbreak in Fujian Province, 2015. Chinese J Vaccines Immun. 2016;22(05):519-524-.
- Dong L, Zhifei C, Danhong C, Weiyi P, Yong Z, Hairong Z, Suhan Z, Ningxuan Z, Xiuhui Y. Etiological identification and genetic characteristics of a mumps outbreak in Fujian province, 2018. Chinese J Vaccines Immun. 2018;24:526–530.
- Hamami D, Cameron R, Kg P, Shankland C. Waning immunity is associated with periodic large outbreaks of mumps: a mathematical modeling study of Scottish Data. Front Physiol. 2017;8(233). doi:10.3389/fphys.2017.00233.
- Lewnard J, Grad Y. Vaccine waning and mumps re-emergence in the United States. Sci Transl Med. 2018;10(433):eaao5945. doi:10.1126/scitranslmed.aao5945.
- Pang H, Zhou Y, Zhao W, Jiang Q. Seroprevalence and determinants associated with mumps antibodies after 20 years of MMR vaccination in urban area of Shanghai, China. Int J Environ Res Public Health. 2018;15(10):2089. doi:10.3390/ijerph15102089.
- Rm A, Rm M. Vaccination and herd immunity to infectious diseases. Nature. 1985; 318(6044):323–329. https://wwwnature.53yu.com/articles/318323a0.
- Pang H, Zhou Y, Zhao W, Jiang Q. Epidemiological changes in mumps infections between 1990 and 2017 in urban area of Shanghai, China. Hum Vaccin Immunother. 2021;17(5):1358–1365. doi:10.1080/21645515.2020.1827610.
- Wang Q, Cheng X, Liu D, Chen C, Yao K. One single-center serological survey on measles, rubella and mumps antibody levels of people in Youyang, China. Hum Vaccin Immunother. 2021;17(11):4203–4209. doi:10.1080/21645515.2021.1924522.
- Waaijenborg S, Sjm H, Mollema L, Smits GP, Berbers GAM, Frmvd K, Hed M, Wallinga J. Waning of maternal antibodies against measles, mumps, rubella, and varicella in communities with contrasting vaccination coverage. J Infect Dis. 2013;208(1):10–16. doi:10.1093/infdis/jit143.
- Smits G, Mollema L, Hahne S, Hd M, Tcherniaeva I, Waaijenborg S, Rv B, Klis FVD, Berbers G. Seroprevalence of mumps in The Netherlands: dynamics over a decade with high vaccination coverage and recent outbreaks. Plos One. 2013;8(3):e58234. doi:10.1371/journal.pone.0058234.
- National Health Commission of the People’s Republic of China. Adjustment on immune procedure of poliomyelitis vaccine and measles-containing vaccine 2020. [accessed 2022 Apr 2022]. http://www.nhc.gov.cn/jkj/s3590/202001/f1b793e053ea49d3b4251fe107ada325.shtml.
- HuaiHo Y, ChiTsai C, WenTsai Y, ChiangWang Y, YienLin T, JenLee D, JungChen C. Humoral immunity to mumps in a highly vaccinated population in Taiwan. J Microbiol Immunol Infect. 2019;52(3):379–385. doi:10.1016/j.jmii.2017.09.001.
- Sun X, Tang F, Hu Y, Deng X, Wang Z, Zhou M, Liu Y. High risk of mumps infection in children who received one dose of mumps-containing vaccine: waning immunity to mumps in children aged 2-5 years from kindergartens in Jiangsu Province, China. Human Vaccines Immunotherapeutics. 2020;16(7):1738–1742. doi:10.1080/21645515.2019.1708162.
- Mossong J, Putz L, Schneider F. Seroprevalence of measles, mumps and rubella antibodies in Luxembourg: results from a national cross-sectional study. Epidemiol Infect. 2004;132(1):11–18. doi:10.1017/S0950268803001584.
- Kristina B, Abreu E, Arneborn M, Böttiger M. Immunity to mumps before and after MMR vaccination at 12 years of age in the first generation offered the two-dose immunization programme. Vaccine. 1998;16(2–3):323–327. doi:10.1016/S0264-410X(97)88332-6.
- Ferrari C, Aurilio MT, Mazza A, Pietroiusti A, Magrini A, Balbi O, Bolcato M, Coppeta L. Evaluation of immunity for mumps among vaccinated medical students. Vaccines. 2021;9(599). doi:10.3390/vaccines9060599.
- Su QR, Liu J, Ma C, Fan CX, Wen N, Luo HM, Wang HQ, Li L, Hao LX. Epidemic profile of mumps in China during 2004-2013. Zhonghua Yu Fang Yi Xue Za Zhi. 2016;6(50):611–614. doi:10.3760/cma.j.issn.0253-9624.2016.07.009.
- Angela D, Núria T, Jesús C, Joan B, Pere G, Marcela G, Dolors C, Joan C, Cristina R, Maria J. Mumps vaccine effectiveness in highly immunized populations. Vaccine. 2010;28(20):3567–3570. doi:10.1016/j.vaccine.2010.02.107.
- WHO. Mumps virus vaccines. Wkly Epidemiol Rec. 2007;82(7):51–60. Available online.
- Scepanovic P, Alanio C, Hammer C, Hodel F, Bergstedt J, Patin E, Thorball CW, Chaturvedi N, Charbit B, Abel L, et al. Human genetic variants and age are the strongest predictors of humoral immune responses to common pathogens and vaccines. Genome Med. 2018;10(59). doi:10.1186/s13073-13018-10568-13078.
- Lklein S, Jedlicka A, Pekosz A. The Xs and Y of immune responses to viral vaccines. Lancet Infect Dis. 2010;10(11):338–349. doi:10.1016/S1473-3099(10)70049-9.
- Meng Q, Liu Y, Yu J, Li L, Shi W, Shen Y, Li L, Zhan S, Yang F, Wang Y, et al. Seroprevalence of maternal and cord antibodies specific for diphtheria, tetanus, pertussis, measles, mumps and rubella in Shunyi, Beijing. Sci Rep. 2018;8(1):13021. doi:10.1038/s41598-018-31283-y.
- Katie G, Jane W, Ewout F, Marjon B, Koen H, Kioe B, Corien S, Tjibbe D, Binnendijk R, Melker H, et al. Mumps outbreak among vaccinated university students associated with a large party, the Netherlands, 2010. Vaccine. 2012;30(29):4676–4680. doi:10.1016/j.vaccine.2012.04.083.
- Rubin S, Link M, Sauder C, Zhang C, Ngo L, Rima B, Duprex W. Recent mumps outbreaks in vaccinated populations: no evidence of immune escape. J Virol. 2012;86(1):615–620. doi:10.1128/JVI.06125-11.
- WHO. Mumps. Vaccine Position Papers. 2007 [accessed 2022 Mar 27]. http://www.who.int/immunization/documents/positionpapers/en.
- Li YT, Luo XQ, Zhong XB, Cai LM, Zhu LP, Chen XQ, Wang KC, Chen ZG. Seroprevalences of antibodies against pertussis, diphtheria, tetanus, measles, mumps and rubella: A, cross-sectional study in children following vaccination procedure in Guangzhou, China. Vaccine. 2020;38(23):3960–3967. doi:10.1016/j.vaccine.2020.03.056.