ABSTRACT
On the basis of their training, medical students are considered “the best case scenario” among university students in knowledge of the human papillomavirus (HPV). We evaluated differences in knowledge of HPV, HPV vaccine, and head and neck cancer (HNC) among medical students. A previously validated questionnaire was completed by 247 medical students at a Midwestern university. Outcomes of interest were knowledge score for HPV and HPV vaccine, and HNC, derived from combining questionnaire items to form HPV knowledge and HNC scores, and analyzed using multivariate linear regression. Mean scores for HPV knowledge were 19.4 out of 26, and 7.2 out of 12 for HNC knowledge. In the final multivariate linear regression model, sex, race, and year of study were independently associated with HPV and HPV vaccine knowledge. Males had significantly lower HPV vaccine knowledge than females (β = −1.53; 95% CI: −2.53, −0.52), as did nonwhite students (β = −1.05; 95% CI: −2.07, −0.03). There was a gradient in HPV vaccine knowledge based on the year of study, highest among fourth year students (β = 6.75; 95% CI: 5.17, 8.33). Results were similar for factors associated with HNC knowledge, except for sex. HNC knowledge similarly increased based on year of study, highest for fourth year students (β = 2.50; 95% CI: 1.72, 3.29). Among medical students, gaps remain in knowledge of HPV, HPV vaccine, and HPV-linked HNC. Male medical students have significantly lower knowledge of HPV. This highlights the need to increase medical student knowledge of HPV and HPV-linked HNC.
Introduction
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection in the United States.Citation1 In addition to several anogenital and second primary malignancies,Citation2–4 HPV is linked to at least 72% of oropharyngeal cancer cases, a subset of head and neck cancer (HNC).Citation5 HPV-associated oropharyngeal cancer has increased in incidence between 57% and 225% in the last three decades and has now exceeded cervical cancer as the most common HPV-associated cancer in the United States.Citation6–8 All approved vaccines are effective against HPV 16 and 18 which together are responsible for about 95% of HPV-associated oropharyngeal cancer.Citation7 Five years after the initial recommendation for adolescent girls, the HPV vaccine recommendation was expanded to include boys by the Advisory Committee on Immunization Practices in 2011 with the goal of preventing HPV-associated cancer. Furthermore, indications for the HPV vaccine were recently expanded to include prevention of HPV-associated oropharyngeal cancer.Citation6,Citation9
Although the HPV vaccine is safe and effective,Citation10,Citation11 it has had limited uptake in the United States, especially in the eligible young adult population.Citation12–15 There is strong evidence that poor provider knowledge of HPV and inadequate physician vaccine recommendations are contributors.Citation16–20 Clinician knowledge, communication ability, and comfort in providing strong recommendations are critical to effective recommendation of the vaccine.Citation16,Citation17,Citation19,Citation20
The medical student population is a unique population in the context of HPV. They comprise the next generation of pediatricians, family medicine physicians, and other primary care clinicians who will lead conversations about the HPV vaccine. However, they are also personally connected to the HPV vaccine discourse as they are eligible for the vaccine themselves. In fact, they often fall within the highest-risk age group for HPV infection, an age group in which individuals are more likely to experiment with oral sex, a primary risk factor for oral HPV.Citation21–24 Therefore, it is important to characterize medical students’ understanding of HPV and its sequelae. However, there remains a paucity of research investigating or characterizing the gaps in HPV knowledge in this population, particularly regarding HNC.
Most of the HPV-related literature on medical and college students in general has focused on knowledge and attitudes about HPV and HPV vaccines without assessing knowledge of HPV-associated HNC.Citation25–28 Studies that focused on HNC had limited study populations and sociodemographic analyses.Citation29,Citation30 Building on these previous studies, we aimed to (1) characterize knowledge of HPV, HPV vaccine, and HPV-associated HNC among medical students, and (2) determine demographic and educational factors associated with differences in knowledge.
Materials and methods
A cross-sectional study was conducted at a medical school in the Midwest using a previously validated questionnaire designed to elicit sociodemographic information and data regarding HPV, the HPV vaccine, and HNC. This was administered via Qualtrics, a secure, web-based application designed for data capture in research studies.Citation31,Citation32 The survey was distributed online to all medical students 26 years or younger. The age range was selected based on eligibility for HPV vaccination at the time of survey, when recommendations for the HPV vaccine were limited to the age of 26 years. Also, previous studies have evaluated HPV vaccination with this age cutoff.Citation20,Citation33 Participants were informed of the study objectives, and informed consent was obtained. Responses to the questionnaire were recorded anonymously. Participation was non-mandatory, but monetary compensation (20.00 USD) was offered to those who completed the survey and elected to receive compensation. The questionnaire was administered to 311 medical students. Of these, 247 completed the survey, yielding a response rate of 79%. This study was approved by the university’s institutional review board.
Measures
The outcome measures were (1) knowledge about HPV and the HPV vaccine, and (2) knowledge about HPV-associated HNC. Knowledge about HPV and the HPV vaccine was assessed with 26 questions. Survey answers were scored as 1 for correct responses and 0 for incorrect responses. Scores were then summed to derive an HPV and HPV vaccine knowledge score, for which the maximum score was 26 and the minimum was 0. HPV-associated HNC knowledge was measured using 12 questions. These responses were scored as 1 for correct responses and as 0 for incorrect responses. Scores were summed to create an HPV-associated HNC knowledge score, which ranged from 0 to 12. For both outcome measures, a higher score represented higher knowledge. In addition, specific knowledge questions regarding HPV’s association with HNC and HPV’s association with cervical cancer (dichotomized as yes/no) were analyzed.
The independent variables included year of study (first, second, third, or fourth year), age, sex (male, female), race (white, nonwhite [combining low-frequency responses]), marital status (married, single but dating, single, and not dating), and number of lifetime oral partners and number of lifetime vaginal partners (zero, one, ≥ two), physician recommendation of HPV vaccine (yes, no), HPV vaccine initiation (recipient of at least one dose), HPV vaccine completion (recipient of at least three doses), and specialty of interest (pediatrics, family medicine, internal medicine, surgery, other specialties).
Statistical analysis
Descriptive statistics were used to analyze the characteristics of the respondents. Sociodemographic characteristics and sexual behavioral risk factors were compared by year of study using Pearson’s chi-square for categorical variables and one-way ANOVA for continuous variables. Two multivariable linear regression models were used to examine the association between the two outcomes (HPV and HPV vaccine knowledge and HPV-associated HNC knowledge) and sociodemographic and sexual behavioral risk factors including year of study, sex, race, marital status, number of oral sexual partners, and number of vaginal sexual partners. Age was not included in the adjusted model because it was highly correlated with year of study. Adjusted β coefficients with corresponding 95% confidence intervals were reported for each variable. In addition, two multivariable logistic regression models were used to examine associations between knowledge of HPV’s association with HNC or cervical cancer, and the same sociodemographic and sexual behavioral risk factors listed above. Analyses were performed using SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC). All statistical analyses were two-tailed and used an alpha level of 0.05 to determine statistical significance.
Results
Sample characteristics
A summary of the characteristics of the respondents in the study sample is provided in . A total of 247 medical students completed the questionnaire, of which 36.4% were first-years, 26.7% were second-years, 24.7% were third-years, and 12.2% were fourth-years. The mean (SD) age of respondents was 24.0 (1.3), and the range was 23.0 (1.2) to 25.5 (0.6). More than half of study respondents were female (56.1%, n = 139) and white (60.1%, n = 149). Almost half 48.0% (n = 119) were married, 53% (n = 130) had multiple oral sexual partners, and 39% (n = 96) had multiple vaginal sexual partners. There was a statistically significant difference in marital status (p = .0026), and provider recommendation to receive HPV vaccine (p = .0336), based on year of study. There was no statistical difference observed in sex, race, number of oral sexual partners, number of vaginal sexual partners, initiation of the HPV vaccine series, completion of the HPV vaccine series, or specialty choice by year of study.
Table 1. Sample characteristics.
HPV and HPV vaccine knowledge
The mean (SD) HPV and HPV vaccine knowledge score was 19.4 (4.6) (). There was a gradient in HPV and HPV vaccine knowledge score based on year of study: first-years had score of 16.2 (4.6) and fourth-years had the highest score of 23.3 (1.6) (). This was a statistically significant difference (p < .001) (). There was no difference in HPV and HPV vaccine knowledge by choice of specialty (). A summary of the adjusted linear regression results estimating HPV and HPV vaccine knowledge is presented in . Compared with first-year students, the second year (β = 2.62; 95% CI: 1.42, 3.82), third-year (β = 6.19; 95% CI: 4.96, 7.41) and fourth-year (β = 6.75; 95% CI: 5.17, 8.33) students had higher HPV and HPV vaccine knowledge. Males (β = −1.53; 95% CI: −2.53, −0.52) and nonwhite (β = −1.05; 95% CI: −2.07, −0.03) medical students had lower HPV and HPV vaccine knowledge in comparison to their female and white counterparts. Marital status, number of oral sexual partners, and number of vaginal sexual partners had no significant association with HPV and HPV vaccine knowledge.
Figure 1. The average (a) HPV and HPV vaccine knowledge (b) HPV-associated HNC knowledge by year of study (n = 247).
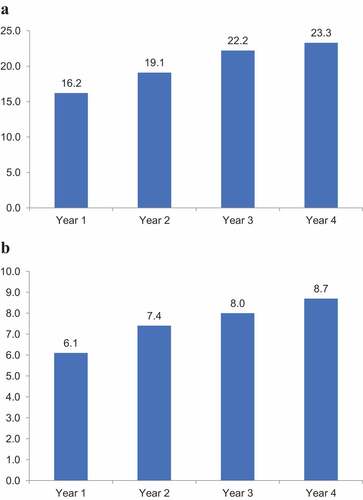
Table 2. HPV and the vaccine knowledge, HPV-associated HNC cancer knowledge, and specific knowledge questions assessing HPV’s association with HNC or cervical cancer by specialty.
Table 3. Linear regression estimating relative risks of HPV and the vaccine, and HPV-associated HNC cancer knowledge.
HPV-associated HNC knowledge
The mean (SD) HPV-associated HNC knowledge was 7.2 (2.1) out of a maximum score of 12 (). There was a statistically significant difference in HPV and HPV vaccine knowledge (p < .001) (). First-year students had the lowest mean score at 6.0 (1.9), while fourth-year students had the highest at 8.7 (1.9) (). There was no difference in HPV-associated HNC knowledge by choice of specialty (). A summary of the adjusted linear regression results estimating HPV-associated HNC knowledge is presented in . In the multivariable analyses, second-year (β = 1.37; 95% CI: 0.78, 1.96), third-year (β = 1.84; 95% CI: 1.24, 2.45), and fourth-year (β = 2.50; 95% CI: 1.72, 3.29) students had higher HPV-associated HNC knowledge compared with first-year students. Nonwhite medical students had lower HPV-associated HNC knowledge (β = −0.86; 95% CI: −1.37, −0.36) compared with whites. There was no difference observed in HPV-associated HNC knowledge by sex, marital status, number of lifetime oral sexual partners, and number of lifetime vaginal sexual partners.
HPV association specific knowledge questions
Similar to the two aggregate knowledge scores, specific questions assessing knowledge of HPV’s association with HNC and HPV’s association with cervical cancer exhibited increased rate of correct responses with increasing year of study (p < .001) (). There were no significant differences in either knowledge by specialty choice (). summarizes logistic regression results of individual knowledge questions regarding HPV’s association with HNC or cervical cancer. No statistically significant differences were observed by any covariate analyzed, with the exception that first-year students show a decreased odds as compared to fourth year students of identifying either HPV’s association with HNC or HPV’s association with cervical cancer (aOR = 0.11; 95% CI: 0.03, 0.36; aOR = 0.29; 95% CI: 0.10, 0.83, respectively).
Table 4. Logistic regression estimating odds ratio of individual knowledge questions regarding HPV’s association with HNC or cervical cancer.
Discussion
This study aimed to identify differences in knowledge of HPV, HPV vaccine, and head HNC among medical students. Our results indicate that there are gaps in knowledge of both HPV vaccine and HPV-associated HNC among medical students. While we observed a pattern of increased knowledge levels with increasing training from first year to fourth, we also observed differences in HPV vaccine knowledge based on sex and race and differences in knowledge of HPV’s association with HNC based on race. Our results provide some evidence that, as primary stakeholders in HPV vaccine communication, education, and uptake,Citation18 this next generation of clinical providers may need more education about the HPV vaccine themselves.
The current literature regarding prevention and outcomes of HPV-associated cancer is rapidly evolving. In the current study, the mean score for HPV and HPV vaccine knowledge was 19.4 out of 24, and knowledge HPV-associated HNC was 7.2 out of 12. In a previous study of university students, 81% had less than average knowledge scores. However, participants were university without a medical background.Citation34 In another survey of medical students in Alabama, participants had similar knowledge levels as the current study, but the study focused mainly on knowledge of HPV and HPV vaccine, not HPV’s association with HNC.Citation26 We found in the current study that medical student knowledge of both outcome measures remained inadequate, even among senior (4th year) medical students.
We observed a “dose–response” association between year of study and both HPV and HPV vaccine knowledge and HPV-associated HNC knowledge. Second, third- and fourth-year medical students had higher knowledge scores than first-year students. Similar associations between HPV knowledge, HPV vaccine knowledge, and medical school year of study have been described in recent literature.Citation26 Likewise, the differences in HPV-associated HNC knowledge by year of study in this report are supported by a recent study reporting that medical students identify incorrect HPV oncological associations as often as its correct association with HNC.Citation29 Unlike the current study, however, a recent survey of 10 medical schools in New York reported similar knowledge levels between third- and fourth-year medical students regarding HNC.Citation35 Taken together, our findings from the Midwest, the study from Alabama,Citation26 a report from New York,Citation35 as well as a national survey of medical trainees (medical students and residents),Citation29 all suggest that there might be an opportunity to improve the medical school curricula with regard to HPV, HPV vaccine, and HPV’s association with HNC. It seems at present that medical students may be not be adequately prepared to address an issue like HPV vaccine uptake, which is a national imperative.Citation36 Given the poor rate of HPV vaccine uptake and increasing incidence of HPV-related cancers, we suggest that providing adequate knowledge about HPV, HPV-related cancers, and the HPV vaccine should be addressed in medical school curricula across the United States.
This study revealed lower HPV and HPV vaccine knowledge in male medical students. These results were contrast with the observations made in a previous study, which did not find any difference in knowledge based on sex.Citation26 Studies have consistently shown that despite a higher incidence of HNC in men, they have both lower HPV vaccine uptake, and HPV vaccination knowledge than women.Citation37–42 Many men consider HPV to be a female issue as public health vaccination campaigns have largely highlighted the vaccine as a preventive measure for cervical cancer. In addition to differences in sex, we also found a gap in knowledge by race, and nonwhite medical students had significantly lower knowledge of HPV, HPV vaccine, and HPV’s association with HNC. While differences in HPV-associated HNC knowledge by race have been shown in the general population, this trend has not been investigated in the medical student population.Citation37–39–Citation43,Citation44 This is important because minorities are less likely to receive HPV vaccine recommendations from providers despite more often relying on primary care provider as a primary source of health information.Citation45–47 It is important to recognize these differences in knowledge by race and sex in developing interventions for these groups, and in improving the medical curricula. It is particularly important as a physician’s recommendation of the HPV vaccine remains one of the most important predictors of uptake,Citation18 and patient-physician racial concordance is associated with improved patients’ communication and overall satisfaction with care provided.Citation48,Citation49 Thus, it is important that future healthcare providers that are from minority racial background receive training that equips them to engage in conversations that would increase HPV vaccine uptake, especially when they provide care for racially concordant patients. This might help mitigate the racial inequality in HPV vaccine uptake.Citation45,Citation46
Limitations and strengths
This study has several limitations. First, as the sample includes medical students from a single Midwestern academic institution, generalizability is limited regarding medical students across the United States. However, two national surveys reported overall similar results, which supports the external validity of our conclusions.Citation19,Citation29 Second, the cross-sectional study design precludes causal conclusions. There is also a limited sample size of fourth-year medical students due to the inclusion criteria of a maximum age of 26 years. Recently, with increased enrollment of non-traditional medical students, the average age of medical students has risen. The increasing number of medical students over 26 years is not included in our study; however, we believe their exclusion should not affect our findings as a majority of medical students as our cutoff age of 26 years falls within the average of matriculating into medical school in the United States within the last two decades.Citation50 Lastly, our physician recommendation of HPV vaccine assessment may not be reliable as it is possible that a subset of respondents to this question may have been vaccinated as children.
Despite these limitations, our study is one of few to examine HPV-associated HNC knowledge in the medical student population, in addition to knowledge of HPV and HPV vaccine. The study included comparable numbers of both male and female participants, which contrasts with most previous studies which included only females.
Implications
HPV vaccination for all below the age of 26 years and for those between 27 and 45 years with certain risk factors, based on a patient-physician shared decision-making. Thus, there is a need for provider knowledge and recommendation of the vaccine. Evidence is growing regarding inadequate physician communication and recommendation of the HPV vaccine.Citation21–24 Knowledge of HPV’s link to oropharyngeal cancer is particularly important as HPV-associated oropharyngeal cancer has surpassed cervical cancer as the leading HPV-associated cancer in the United States.Citation51 Citation35Unlike cervical cancer, HPV vaccine is the only primary prevention for oropharyngeal cancer, and the Food and Drug Administration only recently extended the indications for HPV vaccination to include preventing oropharyngeal cancer.Citation6 However, more individuals may be aware of the link between HPV and cervical cancer than the link between HPV and HNC.Citation38 There are several reasons driving this lack of knowledge of HPV’s link to HNC relative to cervical cancer. For example, the natural history of cervical cancer is more understood than oropharyngeal cancer. Also, the HPV vaccine was first approved and heavily marketed toward females for preventing cervical cancer, and it was not until 2011 that the vaccine was approved for use among males. Thus, it might be that even among medical students, there may still be some lingering perception of HPV being primarily an issue for women.
Thus, there is a need for improved knowledge regarding HPV-related associations and interventions in healthcare providers today. Our study showed that there are inadequate HPV knowledge levels among medical students. Improving gaps in HPV vaccine coverage, reducing HPV infection rates, and advancing primary prevention of HPV-associated oropharyngeal cancer all rely on new and robust educational interventions that begin with medical students, especially in males and racial/ethnic minorities.
Conclusion
Our study shows that medical students have low knowledge of HPV, the HPV vaccine, and the association between HPV and HNC. There are pronounced disparities in knowledge by medical school year, sex, and race. Educational interventions must address medical student knowledge to improve HPV vaccine coverage and address the increasing incidence of HPV-associated oropharyngeal cancer.
Disclosure statement
Dr Osazuwa-Peters is a scientific advisor to Navigating Cancer.
Additional information
Funding
References
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, Su J, Xu F, Weinstock H. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013 Mar;40(3):1–8. doi:10.1097/OLQ.0b013e318286bb53.
- Adjei Boakye E, Buchanan P, Hinyard L, Osazuwa-Peters N, Schootman M, Piccirillo JF. Incidence and risk of second primary malignant neoplasm after a first head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2018 Aug 1;144(8);727–737. doi:10.1001/jamaoto.2018.0993.
- Adjei Boakye E, Grubb L, Peterson CE, Osazuwa-Peters N, Grabosch S, Ladage HD, Huh WK. Risk of second primary cancers among survivors of gynecological cancers. Gynecol Oncol. 2020 Sep;158(3):719–726. doi:10.1016/j.ygyno.2020.06.492.
- Wang M, Sharma A, Osazuwa-Peters N, Simpson MC, Schootman M, Piccirillo JF, Huh WK, Adjei Boakye E. Risk of subsequent malignant neoplasms after an index potentially-human papillomavirus (HPV)-associated cancers. Cancer Epidemiol. 2020;64:101649. doi:10.1016/j.canep.2019.101649.
- Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer. 2008;113(S10):3036–3046. doi:10.1002/cncr.23764.
- Osazuwa-Peters N, Graboyes EM, Khariwala SS. Expanding indications for the human papillomavirus vaccine: one small step for the prevention of head and neck cancer, but one giant leap remains. JAMA Otolaryngol Head Neck Surg. 2020 Dec 1;146(12);1099–1101. doi:10.1001/jamaoto.2020.4068.
- Pytynia KB, Dahlstrom KR, Sturgis EM. Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol. 2014 May;50(5):380–386. doi:10.1016/j.oraloncology.2013.12.019.
- Osazuwa-Peters N, Simpson MC, Massa ST, Adjei Boakye E, Antisdel JL, Varvares MA. 40-Year incidence trends for oropharyngeal squamous cell carcinoma in the United States. Oral Oncol. 2017 Nov 1;74(Supplement C):90–97. doi:10.1016/j.oraloncology.2017.09.015.
- Chaturvedi AK, Graubard BI, Broutian T, Pickard RKL, Tong Z-Y, Xiao W, Kahle L, Gillison ML. Effect of prophylactic human papillomavirus (HPV) vaccination on oral HPV infections among young adults in the United States. J Clin Oncol. 2018 Jan 20;36(3):262–267. doi:10.1200/jco.2017.75.0141.
- Osazuwa-Peters N, Rohde RL, Boakye EA. HPV vaccination is safe-you don’t have to whisper it. JAMA Network Open. 2021 Sep 1;4(9):e2125124. doi:10.1001/jamanetworkopen.2021.25124.
- Sonawane K, Lin YY, Damgacioglu H, et al. Trends in human papillomavirus vaccine safety concerns and adverse event reporting in the United States. JAMA Network Open. 2021 Sep 1;4(9):e2124502. doi:10.1001/jamanetworkopen.2021.24502.
- Adjei Boakye E, Lew D, Muthukrishnan M, Tobo BB, Rohde RL, Varvares MA, Osazuwa-Peters N. Correlates of human papillomavirus (HPV) vaccination initiation and completion among 18–26 year olds in the United States. Human Vaccines Immunotherapeutics. 2018;14(8):2016–2024. doi:10.1080/21645515.2018.1467203.
- Adjei Boakye E, Zeng W, Governor S, Nagendra S, Tobo BB, Simpson MC, Osazuwa-Peters N. Differences in human papillomavirus (HPV) vaccine uptake by nativity status among men aged 18–34 years. Prev Med Rep. 2019 Dec;16:101010. doi:10.1016/j.pmedr.2019.101010.
- Barnard M, George P, Perryman ML, Wolff LA, De Groot AS. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: implications from the precaution adoption process model. PloS One. 2017;12(8):e0182266. doi:10.1371/journal.pone.0182266.
- Thompson EL, Vamos CA, Vázquez-Otero C, Logan R, Griner S, Daley EM. Trends and predictors of HPV vaccination among U.S. College women and men. Prev Med. 2016 May;86:92–98. doi:10.1016/j.ypmed.2016.02.003.
- Dempsey AF, Pyrzanowski J, Campagna EJ, Lockhart S, O’Leary ST. Parent report of provider HPV vaccine communication strategies used during a randomized, controlled trial of a provider communication intervention. Vaccine. 2019 Feb 28;37(10):1307–1312. doi:10.1016/j.vaccine.2019.01.051.
- Dempsey AF, Pyrznawoski J, Lockhart S, Barnard J, Campagna EJ, Garrett K, Fisher A, Dickinson LM, O’Leary ST. Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: a cluster randomized clinical trial. JAMA Pediatr. 2018 May 7;172(5):e180016. doi:10.1001/jamapediatrics.2018.0016.
- Mohammed KA, Geneus CJ, Osazuwa-Peters N, Adjei Boakye E, Tobo BB, Burroughs TE. Disparities in provider recommendation of human papillomavirus vaccination for U.S. adolescents. J Adolesc Health. 2016 Nov;59(5):592–598. doi:10.1016/j.jadohealth.2016.06.005.
- Schnaith AM, Evans EM, Vogt C, Tinsay AM, Schmidt TE, Tessier KM, Erickson BK. An innovative medical school curriculum to address human papillomavirus vaccine hesitancy. Vaccine. 2018 Jun 18;36(26):3830–3835. doi:10.1016/j.vaccine.2018.05.014.
- Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19-26: Importance of a physician’s recommendation. Vaccine. 2011 Jan 29;29(5):890–895. doi:10.1016/j.vaccine.2009.12.063.
- Oshman LD, Davis AM. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices (ACIP). JAMA. 2020 Feb 4;323(5):468–469. doi:10.1001/jama.2019.18411.
- Burger EA, Kim JJ, Sy S, Castle PE. Age of acquiring causal human papillomavirus (HPV) infections: leveraging simulation models to explore the natural history of HPV-induced cervical cancer. Clin Infect Dis. 2017 Sep 15;65(6):893–899. doi:10.1093/cid/cix475.
- Chen J, Gopala K, Akarsh PK, Struyf F, Rosillon D. Prevalence and incidence of human papillomavirus (HPV) infection before and after pregnancy: pooled analysis of the control arms of efficacy trials of HPV-16/18 AS04-adjuvanted vaccine. Open Forum Infect Dis. 2019 Dec;6(12):ofz486. doi:10.1093/ofid/ofz486.
- Habel MA, Leichliter JS, Dittus PJ, Spicknall IH, Aral SO. Heterosexual anal and oral sex in adolescents and adults in the United States, 2011-2015. Sex Transm Dis. 2018 Dec;45(12):775–782. doi:10.1097/olq.0000000000000889.
- Afonso NM, Kavanagh MJ, Swanberg SM, Schulte JM, Wunderlich T, Lucia VC. Will they lead by example? Assessment of vaccination rates and attitudes to human papilloma virus in millennial medical students. BMC Public Health. 2017 Jan 6;17(1):35. doi:10.1186/s12889-016-3969-x.
- Daniel CL, McLendon L, Green CL, Anderson KJ, Pierce JY, Perkins A, Beasley M. HPV and HPV vaccination knowledge and attitudes among medical students in Alabama. J Cancer Educ. 2021 Feb;36(1):168–177. doi:10.1007/s13187-019-01613-3.
- Tung WC, Lu M, Qiu X, Ervin S. Human papillomavirus knowledge, attitudes, and vaccination among Chinese college students in the United States. Vaccine. 2019 May 27;37(24):3199–3204. doi:10.1016/j.vaccine.2019.04.084.
- Franca MC, Boyer VE, Gerend MA, Lee M, Whittington KD, McKinney SL, Collins SK, McKinnies RC, Adjei Boakye E. College students’ awareness of the link between human papillomavirus (HPV) and HPV-associated cancers. J Cancer Educ. 2022 Apr 22. doi:10.1007/s13187-022-02172-w.
- Laitman BM, Ronner L, Oliver K, Genden E. US medical trainees’ knowledge of human papilloma virus and head and neck cancer. Otolaryngol Head Neck Surg. 2020 Jan;162(1):56–59. doi:10.1177/0194599819886117.
- Evans L, Matley E, Oberbillig M, Margetts E, Darrow L. HPV knowledge and attitudes among medical and professional students at a Nevada university: a focus on oropharyngeal cancer and mandating the vaccine. J Cancer Educ. 2020 Aug;35(4):774–781. doi:10.1007/s13187-019-01529-y.
- Cruz GD, Le Geros RZ, Ostroff JS, Hay JL, Kenigsberg H, Franklin DM. Oral cancer knowledge, risk factors and characteristics of subjects in a large oral cancer screening program. J Am Dent Assoc. 2002 Aug;133(8):1064–71; quiz 1094. doi:10.14219/jada.archive.2002.0330.
- Lambert EC. College students’ knowledge of human papillomavirus and effectiveness of a brief educational intervention. J Am Board Fam Pract. 2001 May-Jun;14(3):178–183.
- Wilson AR, Hashibe M, Bodson J, Gren LH, Taylor BA, Greenwood J, Jackson BR, She R, Egger MJ, Kepka D, et al. Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: An observational study. BMC Womens Health. 2016 Jul 22;16(1):41. doi:10.1186/s12905-016-0323-5.
- Osazuwa-Peters N, Tutlam NT. Knowledge and risk perception of oral cavity and oropharyngeal cancer among non-medical university students. J Otolaryngol - Head Neck Surg = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale. 2016 Jan 28;45(1):5. doi:10.1186/s40463-016-0120-z.
- Laitman BM, Oliver K, Genden E. Medical student knowledge of human papillomavirus–positive head and neck cancer. JAMA Otolaryngology–Head Neck Surg. 2018;144(4):380–382. doi:10.1001/jamaoto.2017.3089.
- U.S. Department of Health and Human Services. Healthy people 2020 topics & objectives: Immunization and infectious diseases. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
- Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Human Vaccines Immunotherapeutics. 2017 Nov 2;13(11):2713–2722. doi:10.1080/21645515.2017.1363133.
- Osazuwa-Peters N, Adjei Boakye E, Mohammed KA, Tobo BB, Geneus CJ, Schootman M. Not just a woman’s business! Understanding men and women’s knowledge of HPV, the HPV vaccine, and HPV-associated cancers. Prev Med. 2017 Jun;99:299–304. doi:10.1016/j.ypmed.2017.03.014.
- Osazuwa-Peters N, Hu A, Rohde RL, Tobo BB, Geneus CJ, Mohammed KA, Adjei Boakye E. Sociodemographic predictors of the human papillomavirus (HPV) and HPV vaccine knowledge and awareness among Americans who use the internet as their primary source of health information. J Consum Health Internet. 2018;22(3):199–216. doi:10.1080/15398285.2018.1509258.
- Daley EM, Vamos CA, Zimet GD, Rosberger Z, Thompson EL, Merrell L. The feminization of HPV: reversing gender biases in US human papillomavirus vaccine policy. Am J Public Health. 2016 Jun;106(6):983–984. doi:10.2105/ajph.2016.303122.
- Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Human Vaccines Immunotherapeutics. 2016 Jun 2;12(6):1519–1527. doi:10.1080/21645515.2016.1157673.
- Adjei Boakye E, Babatunde OA, Wang M, Osazuwa-Peters N, Jenkins W, Lee M, Kim M. Geographic variation in human papillomavirus vaccination initiation and completion among young adults in the U.S. Am J Prev Med. 2021 Mar;60(3):387–396. doi:10.1016/j.amepre.2020.09.005.
- Osazuwa-Peters N, Adjei Boakye E, Chen BY, Clancy J, Vallot PL, Su JL, Beck GE, Varvares MA. Sociodemographic factors associated with knowledge and risk perception of human papillomavirus and human papillomavirus–associated oropharyngeal squamous cell carcinoma among a predominantly black population. JAMA Otolaryngol–Head Neck Surg. 2017 Feb 1;143(2):117–124. doi:10.1001/jamaoto.2016.2784.
- Osazuwa-Peters N, Adjei Boakye E, Hussaini AS, et al. Characteristics and predictors of oral cancer knowledge in a predominantly African American community. PloS One. 2017;12(5):e0177787. doi:10.1371/journal.pone.0177787.
- Daniel-Ulloa J, Gilbert PA, Parker EA. Human papillomavirus vaccination in the UNIted States: uneven uptake by gender, race/ethnicity, and sexual orientation. Am J Public Health. 2016 Apr;106(4):746–747. doi:10.2105/ajph.2015.303039.
- Burdette AM, Webb NS, Hill TD, Jokinen-Gordon H. Race-Specific trends in HPV vaccinations and provider recommendations: Persistent disparities or social progress? Public Health. 2017 Jan;142:167–176. doi:10.1016/j.puhe.2016.07.009.
- Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US national immunization survey. Am J Public Health. 2013 Jan;103(1):164–169. doi:10.2105/ajph.2011.300600.
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004. doi:10.1001/archinte.159.9.997.
- Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, Bylund CL. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethnic Health Disparities. 2018 Feb;5(1):117–140. doi:10.1007/s40615-017-0350-4.
- Zhang D, Li G, Mu L, Thapa J, Li Y, Chen Z, Shi L, Su D, Son H, Pagan JA, et al. Trends in medical school application and matriculation rates across the United States from 2001 to 2015: implications for health disparities. Acad Med. 2021 Jun 1;96(6):885–893. doi:10.1097/acm.0000000000004033.
- Osazuwa-Peters N, Massa ST, Simpson MC, Adjei Boakye E, Varvares MA. Survival of human papillomavirus-associated cancers: filling in the gaps. Cancer. 2018 Jan 1;124(1):18–20. doi:10.1002/cncr.30945.
