ABSTRACT
Miller-Fisher syndrome (MFS) is a rare variant of Guillain–Barré syndrome (GBS) manifesting as the triad of ataxia, areflexia, and ophthalmoplegia. With the extensive 2019 coronavirus disease (COVID-19) immunization program, cases of GBS or MFS following vaccination are increasingly being reported. A 64-y-old Chinese man presented with new-onset paresthesia of the extremities, bilateral abduction limitation, right facial palsy, areflexia of bilateral lower limbs, and left-dominant limb ataxia 12 d after the second dose of inactivated vaccine against COVID-19. Cerebrospinal fluid analysis indicated albumin-cytological dissociation and was positive for anti-GQ1b IgG and anti-GT1b IgG. Nerve conduction studies of limbs showed evidence of axonal neuropathy with reduced sensory amplitudes. Based on the clinical presentations, temporal progression of symptoms, and laboratory findings, the diagnosis of MFS–GBS overlap syndrome was made. The patient was treated with intravenous immunoglobulin and acupuncture and made a complete recovery 54 d after the onset of his initial neurological signs. To the best of our knowledge, we report the first case of MFS–GBS overlap syndrome following the inactivated COVID-19 vaccination. However, a coincidental relationship with this inactivated vaccine cannot be excluded. Although the benefits of COVID-19 vaccination largely outweigh its risk and the prognosis of MFS is generally favorable, a close surveillance of neurological complications post-COVID-19 vaccination is always necessary, considering its potentially disabling and lethal effects on vaccinated populations.
Introduction
Guillain–Barré syndrome (GBS) is an immune-mediated demyelinating polyneuropathy of the peripheral nervous system characterized by symmetrical weakness of the extremities with hyporeflexia or areflexia and sensory disturbances.Citation1 Miller-Fisher syndrome (MFS) is a rare variant of GBS with a prevalence of one to two people per million each year and manifests as the triad of ataxia, areflexia, and ophthalmoplegia. Cases in which MFS coexists with other features of GBS, such as limb weakness, paresthesia, and facial palsy, are considered MFS–GBS overlap syndromes.Citation2
GBS is believed to be a postinfectious disorder, and 2/3 of patients report neurological symptoms after a preceding respiratory or gastrointestinal tract infection.Citation3 Reports from northern China are linked to C. jejuni infections and the acute motor axonal neuropathy phenotype, providing favorable evidences to support an autoantibody-mediated immune process in GBS being triggered by molecular mimicry between structural components of peripheral nerves and the microorganism.Citation1,Citation4 With the extensive 2019 coronavirus disease (COVID-19) immunization program, cases of GBS following vaccination are increasingly being reported.Citation5–7 A study performed a disproportionality analysis using the World Health Organization pharmacovigilance database to investigate associations of GBS with COVID-19 vaccines, indicating that the ChAdOx1 nCoV-19 and two messenger RNA-based COVID-19 vaccines had a higher risk for GBS against the entire database.Citation8 At present, reports of post-COVID-19 vaccination MFS or MFS–GBS overlap syndrome are less frequent, in which most cases received ChAdOx1 nCoV-19 or messenger RNA-based COVID-19 vaccines. Here, we report the first case of a patient with MFS–GBS overlap syndrome following the second dose of inactivated COVID-19 vaccine and conduct a scope review of MFS or its limited forms following COVID-19 vaccines.
Case presentations
A 64-y-old Chinese man complained of mild nasal congestion and runny nose but no fever 10 d after the second dose of the Sinovac-CoronaVac COVID-19 vaccine. He was not treated with any medications. A negative PCR result for COVID-19 infection was confirmed at that time. And the above symptoms were completely relieved on the next day. One day later, the patient experienced new-onset numbness of bilateral lower limbs below the knee joint and numbness of bilateral upper limbs below the elbow joint. His symptoms progressed over the next 10 d to developed double vision, dizziness, nausea, headache, dribbling of saliva, and inability to fully close the right eye. No associated respiratory distress, dysphagia, or urinary or bowel symptoms were reported by him. The patient was admitted to the hospital 15 d after limb paresthesia onset. There was a history of cholecystitis, chronic gastritis, and a surgery for gallstone. The patient was not on any regular medications. He denied a history of smoking, alcohol consumption, or drug abuse. The family history of him was noncontributory.
A complete review of systems was unremarkable. On neurological examination, he was noted to be conscious, alert, and oriented. His speech was clear, with intact naming and repetition. Both pupils were round, equal (right: 3.0 mm and left: 3.0 mm), and slowly reactive to light. Impaired abduction of both eyes (more prominent in the right eye) and right facial diplegia involving the forehead were observed. The other cranial nerves were preserved normally. Gait was normal, with no evidence of muscle weakness, ataxia, or sensory disturbances. Deep-tendon reflexes of bilateral lower limbs were absent.
On the second day of admission, the patients reported unsteadiness and slight difficulty walking. Examination revealed left-dominant limb ataxia and mild ataxic gait.
Investigations
Routine hematological and biochemical analyses were normal, including complete blood count, coagulation profile, blood glucose, glycated hemoglobin, sodium, potassium, and renal and liver function tests. The infectious and immunological examinations were unremarkable, including C-reactive protein, hepatitis series antigens and antibodies, HIV, thyroid function and related antibodies, rheumatoid factor (RF), antinuclear antibody, anti-SS-A antibody, anti-SS-B antibody, anti-Jo-l antibody, anti-PM-Scl antibody, anti-SCl-70 antibody, anti-Ro-52 antibody, anti-Sm antibody, anti-RNP antibody, anti-ds-DNA antibody, antineutrophil cytoplasmic antibody (ANCA), and anticardiolipin antibody (ACA). Tumor marker tests were negative including cancer antigen 125 (CA125), carcinoembryonic antigen (CEA), cancer antigen 199 (CA199), prostate-specific antigen (PSA), and alpha-fetoprotein (AFP). Blood B12/folate, serum iron, ferritin, and transferritin levels were normal. PCR result for COVID-19 infection was negative. Magnetic resonance imaging (MRI) of the brain demonstrated no evidence of an acute infarct (supported by a negative result of diffusion-weighted imaging) or other abnormalities. The cerebrospinal fluid (CSF) analysis showed the following: total protein 691.39 mg/L (normal range: 150–450 mg/L), leukocyte 10/μL (normal range: 0-10/μL), polymorphonuclear leukocytes 0/μL, immunoglobulin G 67.5 ng/L (normal range: 0–34 mg/L), immunoglobulin A 8.22 ng/L (normal range: 0–5 mg/L), and microalbumin 424 ng/L (normal range: 0–350 mg/L). The CSF oligoclonal bands were negative. CSF anti-GQ1b IgG and anti-GT1b IgG were found to be positive. The CSF acid-fast staining, India-ink capsule staining, and culture were negative and CSF cytology was normal. Nerve conduction studies (NCS) of limbs showed evidence of axonal neuropathy with reduced sensory amplitudes. No decremental response to repetitive nerve stimulation was observed, and the result of single-muscle-fiber electromyogram was negative. Brainstem and somatosensory-evoked potential tests were normal.
Treatment and outcomes
The patient was diagnosed with MFS–GBS overlap syndrome according to clinical presentations of ataxia, areflexia, ophthalmoplegia, limb paresthesia, and facial palsy, temporal progression of symptoms, and laboratory findings. He was planned to be treated with 0.4 g/kg per day of intravenous immunoglobulin (IVIG) for 5 d. On d 2 of IVIG administration, the numbness of all four limbs, abduction limitation of both eyes, and ataxia were improved. Due to the high costs of IVIG, the patient refused to continue IVIG treatment and was discharged (22 d after the limb paresthesia onset). After discharge, the patient received acupuncture treatment [once (20–30 minutes) a day for 20 d] and was followed up in the outpatient clinic. Fifty-four days after the onset of his initial neurological signs (limb paresthesia), the symptoms of ataxia, areflexia, ophthalmoplegia, limb paresthesia, and facial palsy were completely resolved.
Discussion
In the present study, we described a male Chinese patient who developed paresthesia in the distal extremities, abductor nerve palsy, facial palsy, areflexia, and ataxia 12 d after the second dose of Sinovac-CoronaVac, consistent with MFS–GBS overlap syndrome, which, to the best of our knowledge, was the first reported case of MFS–GBS overlap syndrome following inactivated COVID-19 vaccine.
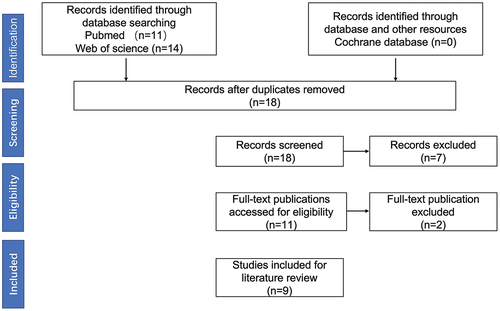
Sinovac-CoronaVac manufactured by the Sinovac Life Sciences Co., Ltd., and adjuvanted (with aluminum hydroxide) to boost the response of the immune system is an (Vero Cell) inactivated vaccine against COVID-19. Recommended schedule is two doses (0.5 mL each) at an interval of 2–4 weeks. Route and site of administration is intramuscular administration, and the preferred site is deltoid muscle. With the widespread implementation of COVID-19 immunization program, a growing concern is vaccine-related side effects. An interim analysis of two clinical trials of inactivated COVID-19 vaccine showed that the degree of local and systemic vaccination-related adverse events following immunization was generally mild.Citation9 However, the incidence of GBS or MFS after the inactivated vaccination had not been reported. Regarding other types of COVID-19 vaccines, seven cases of GBS were reported following BNT162b2 mRNA vaccine among approximately 4 million recipients, and a recent report issued by the UK Health Security Agency concluded that the risk of developing GBS after ChAdOx1vaccine adds 5.6 extra cases of GBS per million doses.Citation10,Citation11 Hence, for detailed description and comparison of the clinical and prognosis information regarding the association between COVID-19 vaccines and MFS, we systematically searched in “PubMed,” “Web of Science,” and “Cochrane” using the keywords“COVID-19” or “SARS-CoV-2,” “vaccination” or “vaccine,” “Miller Fisher syndrome” or “MFS” or “acute ataxic neuropathy” or “acute ophthalmoparesis” from 1 January 2020 to 30 July 2022. The flow diagram of publication identification is listed in . To this end, 25 records were screened and 9 records were finally included in the literature review after identification.
The clinical characteristics and prognosis of MFS following COVID-19 vaccination are listed in . In the 10 cases studied, including the patient in the present case report, the mean age was 63.5 (35.3–72.7) [median (interquartile range)] years old and 80% of patients (8/10) were male. Only one patient had definitive history of preceding respiratory tract infection. Notably, our case showed mild nasal congestion and runny nose before the appearance of neurological symptoms, and we could just rule out the COVID-19 infection of him by PCR test. Whether other respiratory tract infections were present or not was not confirmed. Regarding the vaccine types and number of dose, three patients were with the first-dose BNT162b2, three patients were with the second-dose BNT162b2, two patients were with the first-dose ChAdOx1/S, one patient was with the first-dose inactivated COVID-19 vaccine, and our case was with the second-dose inactivated vaccine. And the time from vaccination to neurological symptom onset was 13.0 (8.0–17.3) d. As for the clinical presentations, the typical symptoms of GBS including limb weakness and paresthesia were observed in 20% (2/10) and 40% (4/10) patients, respectively, indicating the possibility of MFS–GBS overlap syndrome. Facial palsy was observed in 30% (3/10) of cases, and only one patient was observed to have respiratory involvement. Ophthalmoplegia, ataxia, and areflexia, the typical symptoms of MFS, were found in 100% (9/9), 77.8% (7/9), and 66.7% (6/9) of cases. On the relevant auxiliary examinations, CSF albumin-cytological dissociation and anti-ganglioside antibody were observed in 88.9% (8/9) and 62.5% (5/8) of cases. Lines of evidences indicated that the antiganglioside antibodies play a significant role in the pathogenesis of acute autoimmune neuropathies. Anti-GQ1b-IgG is thought to be a key factor in the pathogenesis of MFS, especially for patients with ophthalmoplegia. GQ1b is richly present on paranodal regions of the extramedullary portion of the oculomotor, trochlear, and abducens nerves.Citation18 Inactivated COVID-19 vaccine may also have the GQ1b epitope, which will cause cross-reactivity to vaccine components and peripheral nerves through molecular mimetic mechanisms. To be noted, of these 10 cases, 2 patients reported by Abičić et al. and Kubota et al. manifested as isolated ophthalmoplegia with anti-GQ1b-IgG (+),Citation13,Citation15 which indicated that for patients presenting with isolated ophthalmoplegia and having a history of preceding infection or vaccination, anti-ganglioside antibody test was helpful for accurate diagnosis making. Regarding the treatment and prognosis, immunotherapy was effective in all cases, and most patients had a favorable prognosis, which was consistent with the MFS caused by preceding infections or other vaccination.Citation1,Citation19,Citation20
Table 1. Clinical characteristics and prognosis of published cases of Miller-Fisher syndrome following COVID-19 vaccination.
There are several limitations in the present study. Firstly, as it is well known, preceding respiratory tract infections are important triggers of MFS. Our patients initially presented with mild nasal congestion and runny nose 10 d after the second dose of the vaccine. Although the COVID-19 infection was ruled out at that time, the possibility of respiratory tract infection caused by other microorganisms cannot be excluded. Whether the MFS–GBS overlap syndrome in our case is caused by the COVID-19 vaccination, a precursor respiratory tract infection or a combination effect of vaccine and infection cannot be clearly determined. However, the onset of neurological symptoms was just 1 d after the symptoms of nasal congestion and runny nose, which is not in accordance with the latency period of 7–22 d for infection-induced MFS or GBS reported previously.Citation1 Therefore, it is more likely that the MFS–GBS overlap syndrome in our study was caused by COVID-19 vaccination. Secondly, enhanced MRI was not performed, which made us not obtain related imaging evidence of the oculomotor, abducens, and facial nerves impairments in our case. Thirdly, anti-ganglioside antibodies were tested only in the CSF, which did not allow us to make a comparison of the antibody profiles in the serum and CSF.
Conclusions
We report the first case of MFS–GBS overlap syndrome following the inactivated COVID-19 vaccination. However, a coincidental relationship with this inactivated vaccine cannot be excluded, which made it difficult to conclude a definite cause-and-effect relationship between vaccine against COVID-19 and MFS–GBS overlap syndrome in this time. A close surveillance of neurological complications post-COVID-19 vaccination is always necessary considering its potentially disabling and lethal effects on vaccinated populations, although the prognosis of MFS is generally favorable indicated by the scope review.
Author’s contributions
HL and YBC performed literature review and wrote the original draft of the manuscript. WZ and ZWM revised the manuscript. JL and HC supervised the writing process and revised the manuscript. All authors approved the final version for submission.
Patient consent for publication
Consent obtained directly from patient.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data are available on reasonable request.
Additional information
Funding
References
- Shahrizaila N, Lehmann HC, Kuwabara S. Guillain-Barre syndrome. Lancet. 2021;397:1–5. doi:10.1016/S0140-6736(21)00517-1.
- Sejvar JJ, Kohl KS, Gidudu J, Amato A, Bakshi N, Baxter R, Burwen DR, Cornblath DR, Cleerbout J, Edwards KM, et al. 2011. Guillain-Barre syndrome and Fisher syndrome: case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 29:599–612. doi:10.1016/j.vaccine.2010.06.003.
- van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barre syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2014;10:469–82. doi:10.1038/nrneurol.2014.121.
- Yuki N, Kuwabara S. Axonal Guillain-Barre syndrome: carbohydrate mimicry and pathophysiology. J Peripher Nerv Syst. 2007;12:238–49. doi:10.1111/j.1529-8027.2007.00153.x.
- Assiri SA, Althaqafi RMM, Alswat K, Alghamdi AA, Alomairi NE, Nemenqani DM, Ibrahim ZS, Elkady A. Post COVID-19 vaccination-associated neurological complications. Neuropsychiatr Dis Treat. 2022;18:137–54. doi:10.2147/NDT.S343438.
- Dang YL, Bryson A. Miller-Fisher syndrome and Guillain-Barre syndrome overlap syndrome in a patient post Oxford-AstraZeneca SARS-CoV-2 vaccination. BMJ Case Rep. 2021;14:e246701. doi:10.1136/bcr-2021-246701.
- Nishiguchi Y, Matsuyama H, Maeda K, Shindo A, Tomimoto H. Miller Fisher syndrome following BNT162b2 mRNA coronavirus 2019 vaccination. BMC Neurol. 2021;21:452. doi:10.1186/s12883-021-02489-x.
- Kim JE, Park J, Min YG, Hong YH, Song TJ. Associations of Guillain-Barré syndrome with coronavirus disease 2019 vaccination: disproportionality analysis using the World Health Organization pharmacovigilance database. J Peripher Nerv Syst. 2022;27:206–14. doi:10.1111/jns.12507.
- Parida SP, Sahu DP, Singh AK, Alekhya G, Subba SH, Mishra A, Padhy BM, Patro BK. Adverse events following immunization of COVID-19 (Covaxin) vaccine at a tertiary care center of India. J Med Virol. 2022;94:2453–59. doi:10.1002/jmv.27655.
- Tamborska AA, Singh B, Leonhard SE, Hodel EM, Stowe J, Watson-Fargie T, Fernandes PM, Themistocleous AC, Roelofs J, Brennan K, et al. 2022. Guillain-Barre syndrome following SARS-CoV-2 vaccination in the UK: a prospective surveillance study. BMJ Neurol Open. 4:e000309. doi:10.1136/bmjno-2022-000309.
- Garcia-Grimshaw M, Michel-Chavez A, Vera-Zertuche JM, Galnares-Olalde JA, Hernandez-Vanegas LE, Figueroa-Cucurachi M, Paredes-Ceballos O, Reyes-Teran G, Carbajal-Sandoval G, Ceballos-Liceaga SE, et al. 2021. Guillain-Barre syndrome is infrequent among recipients of the BNT162b2 mRNA COVID-19 vaccine. Clin Immunol. 230:108818. doi:10.1016/j.clim.2021.108818.
- Yamakawa M, Nakahara K, Nakanishi T, Nomura T, Ueda M. Miller Fisher syndrome following vaccination against SARS-CoV-2. Intern Med. 2022;61:1067–69. doi:10.2169/internalmedicine.8851-21.
- Abicic A, Adamec I, Habek M. Miller Fisher syndrome following Pfizer COVID-19 vaccine. Neurol Sci. 2022;43:1495–97. doi:10.1007/s10072-021-05776-0.
- Kim JE, Min YG, Shin JY, Kwon YN, Bae JS, Sung JJ, Hong YH. Guillain-Barre syndrome and variants following COVID-19 vaccination: report of 13 cases. Front Neurol. 2021;12:820723. doi:10.3389/fneur.2021.820723.
- Kubota T, Hasegawa T, Ikeda K, Aoki M. Case report: isolated, unilateral oculomotor palsy with anti-GQ1b antibody following COVID-19 vaccination. F1000res. 2021;10:1142. doi:10.12688/f1000research.74299.1.
- Siddiqi AR, Khan T, Tahir MJ, Asghar MS, Islam MS, Yousaf Z. Miller Fisher syndrome after COVID-19 vaccination: case report and review of literature. Medicine (Baltimore). 2022;101:e29333. doi:10.1097/MD.0000000000029333.
- Michaelson NM, Lam T, Malhotra A, Schiff ND, MacGowan DJL. Miller Fisher syndrome presenting after a second dose of Pfizer-BioNtecH vaccination in a patient with resolved COVID-19: a case report. J Clin Neuromuscul Dis. 2021;23:113–15. doi:10.1097/CND.0000000000000376.
- Chiba A, Kusunoki S, Obata H, Machinami R, Kanazawa I. Serum anti-GQ1b IgG antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain-Barre syndrome: clinical and immunohistochemical studies. Neurology. 1993;43:1911–17. doi:10.1212/WNL.43.10.1911.
- Salmon DA, Proschan M, Forshee R, Gargiullo P, Bleser W, Burwen DR, Cunningham F, Garman P, Greene SK, Lee GM, et al. 2013. Association between Guillain-Barre syndrome and influenza a (H1N1) 2009 monovalent inactivated vaccines in the USA: a meta-analysis. Lancet. 381:1461–68. doi:10.1016/S0140-6736(12)62189-8.
- Prestel J, Volkers P, Mentzer D, Lehmann HC, Hartung HP, Keller-Stanislawski B; Group GBSSRisk of Guillain-Barre syndrome following pandemic influenza A(H1N1) 2009 vaccination in Germany. Pharmacoepidemiol Drug Saf. 2014;23:1192–204. doi:10.1002/pds.3638.