ABSTRACT
Human papillomavirus (HPV) vaccine uptake remains low in China, especially among girls. Recently, China has initiated a pilot program on HPV immunization for girls aged 9–14 years. We conducted a cross-sectional online survey in Minhang district of Shanghai, a pilot region for the program, to investigate HPV vaccination status among mothers and their daughters 9–14. A total of 1031 parents and 1122 daughters 9–14 were included. Of them, 18.6% of mothers and 4.5% of daughters had been vaccinated with HPV vaccines or made an appointment; additionally, 62.7% and 78.4% intended to receive vaccination but did not make an appointment. Notably, 6.2% of parents did not intend to receive vaccination for themselves (or their wives) but intended to vaccinate their daughters. Moreover, we calculated parental knowledge and awareness scores toward HPV infection and vaccination. Both scores were significantly higher among the parents who had received HPV vaccination than those who intended to across mothers’ vaccination status (P < .001 for knowledge and P = .019 for awareness), whereas similar between the two groups across daughters’ vaccination status (P = .694 and P = .737). Parents believed mothers had a significantly higher susceptibility to HPV infection and lower health consequences, compared to daughters 9–12 (P = .002 and P < .001) or those 13–14 (both P < .001). In conclusion, HPV vaccine uptake remains a discrepancy between mothers and their daughters 9–14. However, their intents to receive HPV vaccination were both high. Parental knowledge and awareness may improve vaccination intent for daughters 9–14 in China. It warrants a certain health education toward susceptibility to HPV infection and health consequences.
Introduction
Human papillomavirus (HPV) is currently considered to be the most common sexually transmitted infection. Persistent HPV infection can cause a variety of diseases, such as genital warts, cervical cancer, vaginal cancer, and oropharyngeal cancer.Citation1 The overall infection rate of high-risk HPV is approximately 19.0% in Chinese women.Citation2 The World Health Organization (WHO) recommends HPV vaccination as the primary prevention for cervical cancer,Citation3 especially for girls aged 9–13.Citation4 The Advisory Committee on Immunization Practices (ACIP) recommends girls get their first dose of HPV vaccine at the age of 11–12.Citation5 Multiple studies have shown that HPV vaccination for girls aged 9–14 prevents more cervical cancer deaths and is more cost-effective.Citation6,Citation7
After the United States licensure in 2006, the first bivalent HPV vaccine was approved in China in 2016,Citation8,Citation9 Currently, bivalent HPV vaccine is for female aged 9–45 years, quadrivalent HPV vaccine is for female 20–45, and 9-valent HPV vaccine is for 16–26 in China’s mainland.Citation10 However, due to the late introduction and self-payment of HPV vaccines, the uptake rate is very low among girls aged 9–14.Citation11 Safety and effectiveness of HPV vaccine are the main concerns for Chinese parents.Citation12 In addition, Chinese parental knowledge of HPV and HPV vaccines remains lacking, resulting in a neglected need for HPV vaccination for girls.Citation12 It has been documented that parents with better education and higher income tend to be more willing to have their daughters vaccinated against HPV.Citation9 Moreover, parents traditionally play a key role in vaccine decisions for their children. Parental attitudes may influence adolescent attitudes to HPV vaccines, and maternal vaccine hesitancy may increase the number of unvaccinated daughters.Citation13,Citation14
In 2021, the National Health Commission of the People’s Republic of China has launched a pilot expanded program on HPV immunization for local girls aged 9–14 in selected cities and regions.Citation15 Minhang district of Shanghai is a pilot region and is currently preparing an HPV vaccination strategy for girls 9–14. In contrast, current vaccination strategy in Shanghai allows local females (those with local household registration or residence permit) to make appointments for HPV vaccination in community health centers and pay in full by themselves.Citation16 Thus, we designed a cross-sectional study to investigate the vaccination status of HPV vaccines among mothers and daughters aged 9–14, and determine the association of parental HPV-related knowledge and awareness with the vaccination status, which would provide direct and prompt evidence for improving HPV vaccination among girls aged 9–14.
Materials and methods
Study design
We designed a cross-sectional study among the parents (mother or father) with daughter(s) aged 9–14 in Minhang district of Shanghai, which is a pilot region for national expanded program on HPV immunization in China, between January and February 2022.
An online questionnaire was used to investigate the HPV vaccine uptake and intent. Based on the previous studies,Citation17 we designed a questionnaire, including the questions on the HPV vaccination status stratified for mothers and daughters, general knowledge and awareness toward HPV and HPV vaccination, in addition to demographics such as age, educational level, and monthly household income (supplementary file).
Participants
Inclusion criteria of participants were as follows: a) parents have at least one daughter aged 9–14; b) those who voluntarily participated in this survey. Those who did not complete the questionnaire were excluded from the study.
The online questionnaire was supported by www.wjx.com. Using a convenient sampling strategy, a quick response (QR) code was dispersed to the students’ parents in 10 primary schools and 10 middle schools in Minhang district of Shanghai. When the parents clicked on the online questionnaire link, they first read the informed consent; only those who clicked “agree” to the consent could further fill the questionnaire.
Measurement
We investigated the HPV vaccination status (uptake and intent) among mothers and daughters and prepared four responses, including “had been vaccinated,” “had not been vaccinated but had made an appointment,” “intend to receive vaccination but did not make an appointment,” and “not intend to receive vaccination.”
Moreover, we prepared a total of five questions on the knowledge of HPV infection (HPV types, diseases caused by HPV, risk of infection, transmission routes, and typical symptoms) and four questions on HPV vaccines (valency, vaccination schedule, vaccination age, and vaccine-preventable diseases). Parental knowledge score was calculated using the following strategy: 3 points for each correct answer, 0 point for incorrect answers, and 1 point for stating they did not know or by selecting a partially correct answer. In addition, for multiple-choice questions, 1 point was given for each correct answer. Then, the scores were added together as the knowledge score. The reliability of these questions has been validated with a Cronbach’s α = 0.812, suggesting a strong reliability.
We also prepared a total of 24 statements measuring the awareness toward risk and severity of HPV infection, effect and safety of HPV vaccines, and cost and convenience of HPV vaccination. Among them, six statements were designed for both parents and their daughters. A 5-point Likert scale was utilized to assess the awareness, including strongly agree (5 points), agree (4 points), neutral (3 points), disagree (2 points), and strongly disagree (1 point). For negative attitude statements, 6 points were subtracted from the statements’ scores so that all items had scores in the same direction. Then, the scores were added together as the awareness score. The reliability analysis for this set of 24 statements was strong with a Cronbach’s α = 0.968.
Statistical analysis
Descriptive methods were used to present the characteristics of parents in the study. Considering the parents may have two or more daughters aged 9–14, we prepared the analysis strategy as follows: each parent was counted once when we presented their characteristics; furthermore, they were repeatedly counted in the statistical analysis for their daughters.
Kappa test was utilized to determine the agreement between the vaccination status among mothers and daughters. Chi-square test was used to compare HPV vaccination status among daughters across parents’ characteristics. Furthermore, generalized linear models were used to determine the association between parental knowledge and awareness scores with HPV vaccination status among mothers and daughters in two age groups. In the models, we controlled for factors such as parental age, educational level, monthly household income, and number of children as confounders. The two age groups were stratified by daughters’ age, 9–12 and 13–14, based on the primary schools and middle schools. This study used IBM SPSS Statistics 23.0 (Armonk, NY, USA) to perform statistical analysis. A P value of <0.05 was considered statistically significant.
Ethical approval
This study was approved by the Institutional Review Board of the Fudan University School of Public Health (IRB 00002408 and FWA 00002399) under IRB #2021-09-0919. When the parents entered the online questionnaire, they first read the informed consent; only those who clicked “agree” to the consent could further complete the questionnaire. Thus, it was considered they had provided the informed consent to the study. In addition, we did not collect any personal identifier in the questionnaire.
Results
Characteristics of parents in the study
A total of 1046 questionnaires were collected, of which 15 were completed by parents who had daughters outside 9–14 years. Thus, 1031 questionnaires were included in our study. The parents had an average age of 43.09 years (standard deviation, 4.04 years). Of them, 63.6% had a bachelor’s degree and above. In addition, those who had monthly income less than CNY 20,000 (approximately USD 3000) (31.7%) and higher than CNY 20,000 (33.4%) were similar.
Notably, the majority of these parents were mothers (80.1%). More than half (59.1%) had a single daughter aged 9–14 years, and 7.0% had two or more daughters 9–14. Furthermore, 21.4% had one daughter 9–14 and son(s) regardless of age, 10.8% had one daughter 9–14 and other daughter(s) outside 9–14. In addition, the remaining respondents (1.7%) had two daughters 9–14 and another daughter (outside 9–14) or son. Accordingly, a total of 1122 daughters 9–14 were included in the analysis.
HPV vaccination status among mothers and daughters
Among the parents, 18.6% of themselves (respondents were mothers) or their wives (respondents were fathers) had been vaccinated with HPV vaccines or had made an appointment, 62.7% intended to receive vaccination but did not make an appointment, and 18.7% did not intend to receive vaccination. In contrast, the majority of their daughters (78.4%) had not been vaccinated but intended to, in addition to the minority (4.5%) had been vaccinated/made an appointment.
We compared the uptake and intent between mothers and daughters, stratified by two age groups of 9–12 and 13–14. It showed both poor agreement in these two groups with Kappa values of 0.371 (age of 9–12) and 0.412 (age of 13–14) (P < .001) (). Notably, in these two groups, 16.6% and 15.6% of parents who (or whose wives) had been vaccinated/made an appointment intended to vaccinate their daughters, respectively; in contrast, 6.0% and 6.4% of those who (or whose wives) did not intend to receive vaccination for themselves intended to vaccinate their daughters, respectively.
Table 1. HPV vaccination status between mothers and daughters aged 9–12.
Table 2. HPV vaccination status between mothers and daughters aged 13–14.
Moreover, HPV vaccine uptake and parental intent among the daughters differed significantly by parental sex, age, educational level, monthly household income, and number of children (). Parents who were mother, younger, had higher educational level, higher income, and single daughter were more likely to receive HPV vaccination for their daughters (each P < .01). Similarly, those who were mother, younger, and had higher income were more likely to have received HPV vaccination or intend to receive for themselves or their wives (each P < .01; data not shown).
Table 3. HPV vaccination status among daughters aged 9–14 across parents’ characteristics.
Parental knowledge and awareness across HPV vaccination status
Parental knowledge scores toward HPV infection and vaccination were similar between the parents with daughters 9–12 and 13–14 (P = .257 across vaccination status among daughters and P = .762 across vaccination status among mothers) (). Furthermore, parental awareness scores toward HPV infection and vaccination for daughters were also similar between those with daughters 9–12 and 13–14 across vaccination status among daughters (P = .314); however, their awareness scores for mothers differed significantly across vaccination status among mothers (P = .006).
Table 4. Parental knowledge and awareness across HPV vaccination status (scores, average ± standard deviation).
In addition, both knowledge and awareness scores were lowest among the parents who did not intend to receive HPV vaccination for themselves (or their wives) or their daughters, regardless of daughters’ age (each P < .001) (). Furthermore, across vaccination status among mothers, both knowledge and awareness scores were significantly higher among those who had been vaccinated/made an appointment than those who intended to (P < .001 for knowledge, and P = .019 for awareness), whereas similar between the two groups across vaccination status among daughters (P = .694 for knowledge, and P = .737 for awareness).
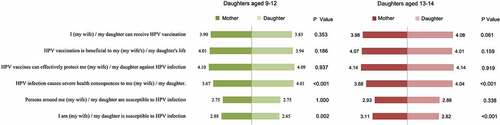
We compared parental awareness scores for mothers and for daughters using the same statements, stratified by two age groups of 9–12 and 13–14 (). In the statement “I am (my wife)/my daughter is susceptible to HPV infection,” the scores for mothers were significantly higher than that for daughters, in the group of 9–12 (P = .002) and 13–14 (P < .001). In contrast, in the statement “HPV infection causes severe health consequences to me (my wife)/my daughter,” the scores for mothers were lower than those for daughters, in the group of 9–12 (P < .001) and 13–14 (P < .001). In addition, in the two statements “I am (my wife)/my daughter is susceptible to HPV infection” and “Persons around me (my wife)/my daughter are susceptible to HPV infection,” the responses were likely to be neutral for both mothers and daughters, whereas positive (agree and strongly agree) in the other four statements.
Discussion
Our study identified a discrepancy in the HPV vaccine uptake between mothers (18.6%) and daughters (4.5%), including those who had been vaccinated and had made an appointment. In contrast, a Nigerian study reported that vaccine uptake among both mothers and daughters was much lower.Citation18 HPV vaccine uptake remains currently low in China, such as 11.82% among adult females in Guangzhou of southern China and 7.37% among females aged 9–45 in Shanghai of eastern China (the same city as our study),Citation19,Citation20 compared to the average global uptake of 58.7%.Citation21 In our study, the uptake rate of HPV vaccines was determined to be 14.1% among the mothers aged <45% and 4.6% among those ≥45. Accordingly, there is an urgent need of improving the HPV vaccine uptake, even in socioeconomically developed areas of China. Furthermore, uptake among girls aged 9–14 was much lower in our study, in line with Japan (1.0%) and Singapore (1.0%); however, it was significantly higher in some countries, including the United Kingdom (84.0%), the United States (62.0%), and South Africa (61.0%).Citation21 Thus, it remains a challenge to improve the HPV vaccine uptake among girls and reduce the discrepancy between mothers and their daughters.
In contrast, both HPV vaccination intents for mothers (81.3%) and for daughters (82.9%) were remarkably high in our study, suggesting another discrepancy between the vaccine uptake and intent. Multiple studies have shown similar discrepancy or gap between vaccination intent and behavior, which may occur in diverse vaccines and populations.Citation22,Citation23 This may be attributable to various reasons, such as service accessibility, price sensitivity, and knowledge and awareness toward vaccines and vaccine-preventable diseases.Citation23 For HPV vaccination, vaccine supply, price, and safety may be the most common concerns that affect the vaccination behavior.Citation24,Citation25 In China, multiple cities and regions have included pilot expanded program on HPV immunization since 2020, supported by governmental subsidies or payment by basic medical insurance.Citation26 These strategies are expected to reduce the barriers caused by supply and prices.
In this study, HPV vaccine uptake and intent among daughters were associated with sociodemographics, including number of children in family. Single children may increase parental awareness for better health protection.Citation27 Moreover, we noticed that approximately 6% of the parents did not intend to receive HPV vaccination for themselves or their wives, but they intended to vaccinate their daughters. It might be due to increasing health education and promotion for HPV vaccines in the expanded program on HPV immunization. Parental knowledge and awareness toward the HPV infection and vaccination substantially influenced the vaccine uptake and intent, as presented in our study and elsewhere.Citation14 Similar findings have been reported in the vaccines that target both adults and children, such as influenza and COVID-19 vaccines.Citation28,Citation29 It suggests knowledge and awareness remain crucial for increasing vaccination intent and behavior.
Multiple HPV vaccines have been approved for female aged 9–45 years in China’s mainland.Citation10 However, in the past, they were generally recommended for adult female, due to potentially neglected demand for girls, in addition to shortage in supply and high prices.Citation30 We found that parents who had higher knowledge and awareness were more likely to receive HPV vaccination for themselves (or their wives) as well as for their daughters. Notably, knowledge and awareness scores were higher among the parents who had received HPV vaccination than those who intended to across vaccination status among mothers, whereas similar between the two groups across vaccination status among daughters, suggesting different parental awareness for mothers and daughters. It was further confirmed by the parental awareness that mothers had higher susceptibility to HPV infection and lower health consequences, compared to their daughters, as shown in . In previous studies, awareness that “daughters are too young to have risk of HPV infection” has been documented to be associated with low uptake of HPV vaccines in children.Citation31,Citation32 Currently, the national expanded program on HPV immunization preferentially targets on girls 13–14 to reduce potential parental concerns. Thus, related knowledge and awareness may contribute to the decision-making of HPV vaccination. It warrants more specific health education and promotion for HPV vaccination for girls.
There are limitations and strengths in the study. First, we included a small sample size in the study, which might limit the generalizability. We conducted an online survey using a convenience sampling method, so we could not characterize the non-respondents, further resulting in potential bias. However, Minhang district of Shanghai has been selected as one of the first pilot cities and regions in China’s mainland. Our findings may provide direct and prompt evidence for further policy-making and vaccination strategies. Second, we investigated the HPV vaccine uptake and intent, similar to multiple previous studies. Our study further determined the discrepancy between the mothers and their daughters, which would facilitate improving the HPV vaccination among girls from a parental perspective. Third, we simply determined HPV vaccine uptake and intent in this study, which might be biased by the types of HPV vaccines, such as bivalent, quadrivalent, and 9-valent. We would further collect the data on the properties of HPV vaccines including valency and manufacturers to determine the influence.
In conclusion, HPV vaccine uptake was low among Chinese mothers and much lower among their daughters aged 9–14, suggesting a discrepancy. In contrast, their intents to receive HPV vaccination were both significantly high. Parental knowledge and awareness may improve vaccination intent for daughters. Certain health education and promotion toward susceptibility to HPV infection and health consequences may enhance the HPV vaccination among girls aged 9–14 in China.
Authors’ contribution
YL and JL conceived of this study. YL, XL, and WZ designed the questionnaire. QG and WZ prepared the online questionnaire and investigation. YL, WZ, and QG analyzed data and drafted the initial manuscript. XW and JL critically revised the manuscript and helped interpret data. All authors reviewed the final manuscript.
Supplemental Material
Download MS Word (24.7 KB)Acknowledgements
We appreciate all parents completing the online questionnaire.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2132801.
Additional information
Funding
References
- Centers for Disease Control and Prevention. Human Papillomavirus(HPV); 2022; [accessed 2022 Jul 1]. https://www.cdc.gov/std/HPV/STDFact-HPV.htm.
- Li K, Li Q, Song L, Wang D, Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019;125(7):1–7. doi:10.1002/cncr.32003. PMID: 30748006.
- World Health Organization. Cervical cancer; 2022; [accessed 2022 Jul 1]. https://www.who.int/health-topics/cervical-cancer#tab=tab_1.
- World Health Organization.New WHO guide to prevent and control cervical cancer. 2014; [accessed 2022 Jul 1]. https://www.who.int/news/item/03-12-2014-new-who-guide-to-prevent-and-control-cervical-cancer
- Advisory Committee on Immunization Practices. Vaccination Recommendations. 2021; [accessed 2022 Jul 1]. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6305a1.htm.
- Jit M, Brisson M. Potential lives saved in 73 countries by adopting multi-cohort vaccination of 9-14-year-old girls against human papillomavirus. Int J Cancer. 2018;143(2):317–23. doi:10.1002/ijc.31321. PMID: 29446090; PMCID: PMC6001440.
- Drolet M, Laprise JF, Martin D, Jit M, É B, Gingras G, Boily MC, Alary M, Baussano I, Hutubessy R, et al. Optimal human papillomavirus vaccination strategies to prevent cervical cancer in low-income and middle-income countries in the context of limited resources: a mathematical modelling analysis. Lancet Infect Dis. 2021;21(11):1598–610. doi:10.1016/S1473-3099(20)30860-4. PMID: 34245682; PMCID: PMC8554391.
- Chen S, Mei C, Huang W, Liu P, Wang H, Lin W, Yuan S, Wang Y. Human papillomavirus vaccination related knowledge, and recommendations among healthcare providers in Southern China: a cross-sectional survey. BMC Women's Health. 2022;22(1):169. doi:10.1186/s12905-022-01728-8. PMID: 35568870; PMCID: PMC9107117.
- Lin Y, Su Z, Chen F, Zhao Q, Zimet GD, Alias H, He S, Hu Z, Wong LP. Chinese mothers’ intention to vaccinate daughters against human papillomavirus (HPV), and their vaccine preferences: a study in Fujian Province. Hum Vaccin Immunother. 2021;17(1):304–15. doi:10.1080/21645515.2020.1756152. PMID: 32401617; PMCID: PMC7872083.
- National Medical Products Asministration. Knowledge | Popular science questions and answers about HPV vaccine. 2019; [accessed 2022 Jul 1]. https://www.nmpa.gov.cn/yaopin/ypjgdt/20190710110101674.html.
- Zou Z, Fairley CK, Ong JJ, Hocking J, Canfell K, Ma X, Chow EPF, Xu X, Zhang L, Zhuang G. Domestic HPV vaccine price and economic returns for cervical cancer prevention in China: a cost-effectiveness analysis. Lancet Glob Health. 2020;8(10):e1335–44. doi:10.1016/S2214-109X(20)30277-1. PMID: 32971056.
- Zhang Y, Wang Y, Liu L, Fan Y, Liu Z, Wang Y, Nie S. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16(1):216. doi:10.1186/s12889-016-2873-8. PMID: 26936076; PMCID: PMC4776385.
- Karafillakis E, Peretti-Watel P, Verger P, Chantler T, Larson HJ. The role of maturity in adolescent decision-making around HPV vaccination in France. Vaccine. 2021 Sep 24;39(40):5741–47. doi:10.1016/j.vaccine.2021.08.096. Epub 2021 Sep 2. PMID: 34483023.
- VanWormer JJ, Bendixsen CG, Vickers ER, Stokley S, McNeil MM, Gee J, Belongia EA, McLean HQ. Association between parent attitudes and receipt of human papillomavirus vaccine in adolescents. BMC Public Health. 2017 Oct 2;17(1):766. doi:10.1186/s12889-017-4787-5. PMID: 28969653; PMCID: PMC5625818.
- National Health Commission of the People’s Republic of China. Proposal on strengthening popular science publicity and improving HPV vaccination. 2021; [accessed 2022 Jul 1]. http://www.nhc.gov.cn/wjw/tia/202112/af51b14c0ca04799b55b8322559751ac.shtml.
- Shanghai women’s federation: recommend free HPV vaccine for girls aged 9-15. 2022; [accessed 2022 Sep 3]. http://service.shanghai.gov.cn/SHVideo/newvideoshow.aspx?id=F7C339986B828E7E.
- Si M, Jiang Y, Su X, Wang W, Zhang X, Gu X, Ma L, Li J, Zhang S, Ren Z, et al. Willingness to accept human papillomavirus vaccination and its influencing factors using information-motivation-behavior skills model: a cross-sectional study of female college freshmen in Mainland China. Cancer Control. 2021;28:10732748211032899. doi:10.1177/10732748211032899. PMID: 34634207; PMCID: PMC8516380.
- Azuogu BN, Umeokonkwo CD, Azuogu VC, Onwe OE, Okedo-Alex IN, Egbuji CC Appraisal of willingness to vaccinate daughters with human papilloma virus vaccine and cervical cancer screening uptake among mothers of adolescent students in Abakaliki, Nigeria. Niger J Clin Pract. 2019 Sep;22(9):1286–91. doi:10.4103/njcp.njcp_452_18. PMID: 31489868.
- Ma Y, Wang C, Liu F, Lian G, Li S, He Q, Li T. Human papillomavirus vaccination coverage and knowledge, perceptions and influencing factors among university students in Guangzhou, China. Hum Vaccin Immunother. 2021;17(10):3603–12. doi:10.1080/21645515.2021.1927411. PMID: 34156312; PMCID: PMC8437546.
- Song Y, Liu X, Yin Z, Yu W, Cao L, Cao L, Ye J, Li L, Wu J. Human papillomavirus vaccine coverage among the 9-45-year-old female population of China in 2018-2020. Chinese Journal of Vaccines and Immunization. 2021;27:570–75. doi:1006-916X(2021)27:5<570:22NZG9>2.0.TX;2-B.
- United Nations International Children’s Emergency Fund. Human papillomavirus (HPV) immunization coverage estimates. 2021; [accessed 2022 Jul 1]. https://data.unicef.org/topic/child-health/immunization/#,2021.
- Ye L, Fang T, Cui J, Zhu G, Ma R, Sun Y, Li P, Li H, Dong H, Xu G. The intentions to get vaccinated against influenza and actual vaccine uptake among diabetic patients in Ningbo, China: identifying motivators and barriers. Hum Vaccin Immunother. 2021;17(1):106–18. doi:10.1080/21645515.2020.1761201. PMID: 32460620; PMCID: PMC7877400.
- Lu X, Lu J, Zhang L, Mei K, Guan B, Lu Y. Gap between willingness and behavior in the vaccination against influenza, pneumonia, and herpes zoster among Chinese aged 50-69 years. Expert Rev Vaccines. 2021;20(9):1147–52. doi:10.1080/14760584.2021.1954910. PMID: 34287096.
- Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, Doukas N, Asey F. Parents’ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open. 2018;8(4):e019206. doi:10.1136/bmjopen-2017-019206. PMID: 29678965; PMCID: PMC5914890.
- Do EK, Rossi B, Miller CA, Ksinan AJ, Wheeler DC, Chukmaitov A, Cyrus JW, Fuemmeler BF. Area-level variation and human papillomavirus vaccination among adolescents and young adults in the United States: a systematic review. Cancer Epidemiol Biomarkers Prev. 2021;30(1):13–21. doi:10.1158/1055-9965.EPI-20-0617. PMID: 33008874; PMCID: PMC8108385.
- National Health Commission of the People’s Republic of China. Implementation plan of the national health commission of the people’s republic of china on implementing the 2021-2030 outline for the development of Chinese women and children. 2022; [accessed 2022 Jul 1]. http://www.nhc.gov.cn/fys/s7900/202204/acaaffebf2e44964a9b14fdddd173cfa.shtml.
- Lin W, Zhou L, Hu H, Chen B, Yuan S, Wu B, Liu Z, Wang Y. The number and gender of children synergistically impact on a mother’s practice of human papillomavirus testing and attitudes towards vaccination in Shenzhen, China. Cancer Epidemiol. 2020;65:101682. doi:10.1016/j.canep.2020.101682. PMID: 32036245.
- Padhi BK, Satapathy P, Rajagopal V, Rustagi N, Vij J, Jain L, Chakrapani V, Patro BK, Kar SS, Singh R, et al. Parents’ perceptions and intention to vaccinate their children against COVID-19: results from a cross-sectional national survey in India. Front Med (Lausanne). 2022;9:806702. doi:10.3389/fmed.2022.806702. PMID: 35665354; PMCID: PMC9159272.
- Temsah MH, Alhuzaimi AN, Aljamaan F, Bahkali F, Al-Eyadhy A, Alrabiaah A, Alhaboob A, Bashiri FA, Alshaer A, Temsah O, et al. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: a national survey. Front Public Health. 2021;9:752323. doi:10.3389/fpubh.2021.752323. PMID: 34722451; PMCID: PMC8548678.
- Wong LP, Han L, Li H, Zhao J, Zhao Q, Zimet GD. Current issues facing the introduction of human papillomavirus vaccine in China and future prospects. Hum Vaccin Immunother. 2019;15(7–8):1533–40. doi:10.1080/21645515.2019.1611157. PMID: 31017500; PMCID: PMC6746483.
- Yu Y, Xu M, Sun J, Li R, Li M, Wang J, Zhang D, Xu A, Liu X. Human papillomavirus infection and vaccination: awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong, China. PLoS One. 2016;11(1):e0146741. doi:10.1371/journal.pone.0146741. PMID: 26766565; PMCID: PMC4713086.
- Huon J-F, Grégoire A, Meireles A, Lefebvre M, Péré M, Coutherut J, Biron C, Raffi F, Briend-Godet V, Mugo NR. Evaluation of the acceptability in France of the vaccine against papillomavirus (HPV) among middle and high school students and their parents. PLoS One. 2020;15(10):e0234693. doi:10.1371/journal.pone.0234693. PMID: 33091021; PMCID: PMC7580947.