ABSTRACT
To determine the estimated pertussis incidence in adults and the need for a booster dose by detecting pertussis and diphtheria antibody levels in adults in Shaanxi province, China. Blood samples were collected from healthy individuals aged 18–59 years in Shaanxi province in 2017. Serum immunoglobulin G (IgG) antibodies against pertussis toxin (PT) and diphtheria toxin (DT) were determined using enzyme-linked immunosorbent assay. The data on reported pertussis cases in Shaanxi province were collected from the China Information System for Disease Control and Prevention and compared with the results of this study. A total of 4307 subjects were enrolled. The mean concentration of anti-PT IgG was 19.6 IU/mL (95% CI = 18.9–20.3), and the positive rate (≥40 IU/mL) was 11.0% (474/4307), of which recent infections (≥100 IU/mL) accounted for 1.2% (53/4307). Only one adult case of pertussis was reported in 2017, which is much lower than the results of this study. The mean concentration of anti-DT IgG was 0.04 IU/mL (95% CI = 0.04–0.05), and the positive rate (≥0.01 IU/mL) was 82.3% (3543/4307). The mean concentration of anti-DT IgG decreased from 0.07 IU/mL in the 18–29 year-old group to 0.03 IU/mL in the 50–59 year-old-group, and the positivity rate decreased from 86.7% to 78.7%. Our study suggests that pertussis is not uncommon among adults. The existing surveillance system might have underestimated the true incidence of pertussis. The diphtheria antibody levels decreased with age. Booster vaccination against pertussis should be considered for adolescents and young adults.
Introduction
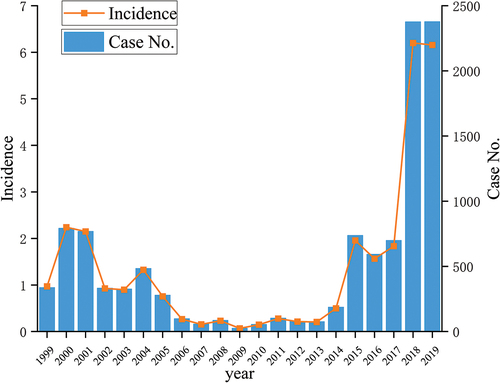
Pertussis (whooping cough) and diphtheria are highly infectious diseases caused by Bordetella pertussis and Corynebacterium diphtheria, respectively.Citation1,Citation2 Vaccinations have significantly reduced the incidence of both diseases.Citation3 However, in recent years, a resurgence of pertussis has occurred in a number of countries.Citation4 The World Health Organization estimated there were 16 million cases of pertussis around the world, and more than 190,000 children died of pertussis in 2008.Citation5 Pertussis has reemerged in a few developed countries with high vaccination rates, such as the United States, Australia, the United Kingdom and other European countries.Citation6–8 In 2019, the reported incidence of pertussis in Shaanxi had risen to 6.2/100,000 (). Undoubtedly, the resurgence of pertussis worldwide has become a global public health problem. Possible reasons for the reemergence of pertussis include increased awareness or more frequent use of diagnostic tests and improved diagnostic ability even in cases with an atypical presentation which may contribute to the increase in the incidence of pertussis.
Figure 1. Reported number of cases and incidence of pertussis in Shaanxi province from the China information system for disease control and prevention between 1999 and 2019.
Unidentified pertussis in vaccinated children, adolescents and adults plays an important role in transmitting pertussis to infants, and the disease is the most severe and often fatal to this group.Citation9,Citation10 The most common source is a mother with a cough that has not been recognized as pertussis by physicians, followed by other adult family members (siblings, fathers or grandparents) who are in close contact with infants.Citation11 Notably, the incidence, morbidity, and mortality of pertussis are higher in infants younger than two months old, whose routine vaccination schedule has not yet begun.Citation12,Citation13 Although newborns can passively acquire antibodies from their mothers for various reasons, most infants are not protected in the first few months of life.Citation11 Several countries have recently adopted maternal pertussis immunization practices to protect young infants.Citation14 The diphtheria-tetanus-acellular pertussis (Tdap) booster dose for adolescents and adults is included in the list of recommended immunizations in a few countries, such as Australia, Canada, Germany, and France.Citation15 Until now, a pertussis booster vaccination for adolescents and adults has not yet been recommended in China, and their level of pertussis antibodies remains unknown in many parts of China.
In China, no cases of diphtheria have been reported for more than 15 years, and no cases of diphtheria have been reported in Shaanxi since 1996. However, some imported diphtheria cases have been found in France, the United States, and neighboring countries in recent years.Citation16,Citation17 Nepal, Indonesia, and India present the highest number of diphtheria cases in Asia.Citation18,Citation19 It is worth noting that Nepal, Bangladesh, and India are all neighboring countries of China. Adolescents and adults who lack diphtheria vaccination or have low antibody levels might have an increased potential risk of diphtheria importation in China. Therefore, it is important to evaluate the diphtheria antibody levels in adults.
In China, a whole-cell pertussis vaccine combined with diphtheria and tetanus toxoids (DTwP) was introduced in the 1980s. A combined DTaP was introduced with basic immunization at three, four, and five months after birth in 2007. The children then receive booster immunization again at 18–24 months. During this period, both DTwP and DTaP were used in parallel. However, DTwP was completely replaced by DTaP from 2010. Immune-induced and infection-induced anti-PT IgG cannot be distinguished using laboratory techniques, such as enzyme-linked immunosorbent assay (ELISA). However, it is estimated that immunity after DTaP starts to decline after four to five years,Citation20 while the duration of immunity provided by DTwP is estimated to be four to 12 years.Citation21 Combined with a history of pertussis immunization, the effect of vaccination on the infection rate can be completely eliminated in adolescents and adults. Pertussis toxin (PT) is the most specific and protective antigen for pertussis in the general population.Citation22 Consequently, anti-PT IgG antibodies are specific indicators of active or recent B. pertussis infection in adolescents and adults.
Shaanxi province is economically underdeveloped in northwestern China. There were ten prefecture-level cities with a total population of 38.4 million. The vaccination program adopted in Shaanxi province is the same as the national program mentioned above, and the coverage rate of immunization has been over 95% in recent years. In previous studies, pertussis and diphtheria in adults have often been overlooked, and little is known about the prevalence of pertussis in this group. To the best of our knowledge, no large-scale studies have been conducted on the prevalence of pertussis and diphtheria in China. This study aimed to determine the concentrations of anti-PT IgG and anti-DT IgG in adults aged 18–59 years old and to provide a basis for understanding the seroepidemiology of pertussis and diphtheria in China.
Methods
Subjects and study design
A large-scale hepatitis B virus (HBV) epidemiological investigation was conducted in Shaanxi province (with a population of 38.4 million) by the Shaanxi Provincial Center for Disease Control and Prevention from October 2017 to December 2017. There are ten cities in this district with a total of 30 disease monitoring sites. Nearly 7,000 serum samples were obtained from individuals aged 1–59 years who resided in this district. All the serum samples used for the HBV serosurvey were stored at −20°C before analysis. No pertussis outbreaks occurred in Shaanxi during the study period. In our study, subjects were required to meet the following criteria: All individuals were aged ≥18 years, asymptomatic, and had not been vaccinated against pertussis within one year of entering the study. People with any symptoms of respiratory illness or that were immunocompromised were excluded. In total, 4307 individuals were included in this study.
Data collection
Basic demographic and epidemiological information, such as sex, age, occupation, and disease history, were collected through face-to-face interviews with structured questionnaires by the local Centers for Disease Control and Prevention (CDC). EpiData 3.1 (EpiData Association, Odense, Denmark) was used for double data entry and consistency checks. The reported incidence of pertussis in Shaanxi province was collected from the China Information System for Disease Control and Prevention.
Laboratory methods
After the questionnaire was completed, 5 mLof venous blood was drawn from each participant. Serum was extracted from blood samples within 3 h of arrival at the local CDC, stored at −20°C, and transported by cold chain transportation to the laboratory of Shaanxi CDC. Anti-PT IgG and anti-DT IgG levels were quantitatively measured using a commercial ELISA kit (Virion/Serion GmbH, Würzburg, Germany) according to the manufacturer’s instructions. Antibody activity is expressed in international units (IU)/mL. The results were interpreted according to the manufacturer’s instructions. An anti-PT IgG level ≥100 IU/mL was defined as recent exposure to B. pertussis (<one year), and levels between 40 and 100 IU/mL were defined as B. pertussis infection>one year prior. A < 40 IU/mL level was defined as non-infection (negative). An anti-DT IgG level<0.01 IU/mL was defined as no immune protection, and values ranging from 0.01 to 0.1 IU/mL, 0.1 to 1.0 IU/mL, and ≥1.0 IU/mL as minimal protection, safe protection, and long-term protection, respectively.
Statistical analysis
Concentrations of anti-PT IgG and anti-DT IgG were summarized as mean values and 95% confidence intervals (CIs) and antibody seroprevalence was calculated as a percentage. The Mann-Whitney test, Kruskal Wallis test, or Jonckheere-Terpstra test was used to compare the mean levels of antibodies between different groups, and the chi-squared test was used to compare the serum positive rates between subgroups. SPSS software (version 25.0; SPSS Inc., Chicago, IL, USA) was used for data analysis, and a P-value of <0.05 was considered significant.
Results
Sociodemographic characteristics of the study population
A total of 4307 participants aged 18–59 years old were included in this study. The median age was 37 (27–49) years. The male to female ratio was 1:1.3 (1889:2418). In terms of education level, 4.4% (190/4307) were illiterate, 16.5% (709/4307) had only primary school education, 43.9% (1891/4307) completed junior high school education, 20.5% (882/4307) completed senior high school education, 13.6% (585/4307) had completed a college education, and 1.2% (50/4307) were unknown.
Immunization history
Of 4307 subjects, 5.5% (236/4307) had been immunized against diphtheria (DTP or DT), 56.6% (2439/4307) had no diphtheria immunization history, and 37.9% (1632/4307) were unknown. Of 236 subjects immunized against diphtheria, 46.6% (110/236) had received five doses, 29.2% (69/236) had received four doses, 9.3% (22/236) had received three doses, 12.1% (30/236) had received one or two doses, and 2.1% (5/236) were unknown.
Of 4307 subjects, 5.1% (221/4307) had been immunized against pertussis (DTP), 57.2% (2464/4307) had no pertussis immunization history, and 37.7% (1622/4307) were unknown. Of 221 subjects immunized against pertussis, 74.7% (165/221) had received four doses, 15.8% (35/221) had received three doses, 0.9% (2/221) had received two doses, and 8.6% (19/221) were unknown.
Seroprevalence of anti-PT IgG
The mean concentration of anti-PT IgG in 4307 subjects was 19.6 IU/m L (95%CI: 18.9–20.3), and the positive rate (≥40 IU/mL) was 11.0% (474/4307). Of the 4307 subjects, 89.0% (3833/4307) had no infection, 9.8% (421/4307) had an infection >one year ago, and 1.2% (53/4307) had a recent infection (within one year). The mean anti-PT IgG concentrations differed between cities (x2 = 111.778, P < .01) and between the sexes (Z = −7.413, P < .01). The lowest mean concentration was found in the 18–29-year-old-group, 17.6 IU/mL (95% CI 16.4–18.8). Antibody concentration increased with age (Z = 9.582, P < .01). A difference in the positive rate was also found between the sexes (x2 = 20.469, P < .01) and between subjects living in cities (x2 = 36.524, P < .01). The positive rate increased with age (x2 = 7.222, P < .01), and the lowest positive rate was found in the 18–29-year-old group, which was 9.3% (144/1548) ().
Table 1. Seroprevalence of anti-PT IgG in 4307 adults.
Among 1224 women of childbearing age (20–39 years old), the mean anti-PT IgG concentration was 16.3 IU/m L (95%CI: 15.2–17.3), and the positive rate (≥40 IU/mL) was 8.9% (109/1224). Furthermore, 91.1% (1115/1224) had no infection, 8.3% (102/1224) had infection >one year ago, and 0.6% (7/1224) had recent infection (within one year).
Seroprevalence of anti-DT IgG
The mean concentration of anti-DT IgG in 4307 subjects was 0.04 IU/mL (95%CI: 0.04–0.05), and the positive rate (≥0.01IU/mL) was 82.3% (3543/4307). Of the 4307 subjects, 17.7% (764/4307) had no immune protection, 74.8% (3223/4307) had minimal protection, 7.0% (301/4307) had safe protection, and 0.4% (10/4307) had long-term protection (≥1.0 IU/mL). The mean concentration of anti-DT IgG differed between cities (x2 = 209.433, P < .01) and sexes (Z = −5.108, P < .01). The highest mean concentration was in the 18–29-year-old group, which was 0.07 IU/mL (95% CI 0.06–0.08). Antibody concentration decreased with age (Z = −14.118, P < .01). A difference in positive rate was also found between the sexes (x2 = 12.557, P < .01) and between subjects living in cities (x2 = 183.4, P < .01). The positive rate decreased with age (x2 = 36.102, P < .01), and the highest positive rate was found in the 18–29-year-old group, which was 86.7% (1342/1548) ().
Table 2. Seroprevalence of anti-DT IgG in 4307 adults.
Among 1224 women of childbearing age (20–39 years old), the mean anti-DT IgG concentration was 0.05 IU/mL (95%CI: 0.04–0.06), and the positive rate (≥0.01IU/mL) was 83.3% (1020/1224). Furthermore, 16.7% (204/1224) lacked protection, 74.4% (910/1224) subjects had minimal protection, and 8.5% (104/1224) had safe protection, 0.5%(6/1224) had long term protection (≥1.0 IU/mL).
Data on pertussis cases reported in Shaanxi province from the China information system for disease control and prevention
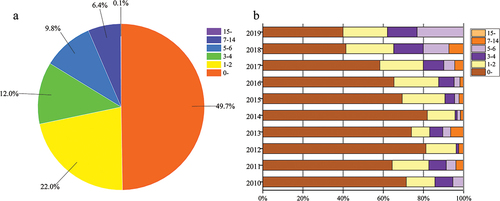
The average annual incidence of pertussis was 1.9/100,000, ranging from 0.2/100,000 to 6.2/100,000 each year during the period of 2010–2019 in Shaanxi province, and a total of 7, 295 pertussis cases were reported during this period; only six cases in people aged ≥ 15 years were reported(one case = 15 years old, five cases≥ 18 years old). Moreover, 49.7% (3628/7295) of reported cases were in infants under one year old, and the reported cases in those aged one to two years old, three to four years old, five to six years old, seven to 14 years old, and≥ 15 years old were 22.0%(1602/7295), 12.0%(879/7295), 9.8%(716/7295), 6.4%(464/7295) and 0.1%(6/7295), respectively (). In 2017, the incidence of pertussis was 1.2/100,000, and 700 pertussis cases were reported in Shaanxi province, of which only one adult case (≥15 years old) was reported. The reported cases in those aged <one year, one or two years old, three to four years old, five to six years, seven to 14 years old, and ≥ 15 years old were 58.3% (408/700), 21.6% (151/700), 10.3% (72/700), 5.4% (38/700), 4.3% (30/700), and 0.1% (1/700), respectively. The number of reported cases and incidence of pertussis in 2017 or between 2010 and 2019 in adults from the existing surveillance system was much lower than the results of this study ().
Discussion
To the best of our knowledge, no large-scale studies have been conducted on the seroprevalence of B. pertussis antibodies in adults in China. However, several similar studies have been conducted in some parts of China. The concentration of anti-PT IgG, positive rate (≥40 IU/mL) of pertussis, and recent infection (within one year) varied from region to region in China. Zhang et al. reported that the mean concentration of anti-PT IgG was 10.0 IU/mL (95% CI 8.5–11.4), with a positive rate of 5.2% (within one year) among adults in Shandong province.Citation23 Chen et al. reported that the mean concentration of anti-PT IgG was 13.8 IU/mL (95% CI, 12.4–15.2), subjects with anti-PT IgG levels≥ 40 IU/mL (positive) accounted for 5.1%, and anti-PT IgG levels ≥ 100 IU/mL (within a year) accounted for 1% of adults in the Chaoyang District. The positive rate of a recent infection was similar to this study (1.2%).Citation24 Zhang et al. compared the positivity rate of anti-PT IgG among adults of childbearing age in Beijing between 2010 and 2015/2016. The positive rate of anti-PT IgG (≥ 40 IU/mL) was 5.1% in 2010 and 4.0% in 2015/2016, and those ≥ 100 IU/mL were 1% in 2010 and 0.6% in 2015/2016.Citation25 In this study, we found that the seroprevalence of anti-PT IgG was 11.0% among adults aged 18–59 years old, and 1.2% had a recent infection (within one year). This study showed that the concentration and positivity rate of anti-PT IgG increased with increasing age. Age is an important factor that affects the seroepidemiology of pertussis. Some domestic scholars have also discovered that the positive rate of pertussis IgG increases with age.Citation26,Citation27 Interpersonal contact increased with age, and asymptomatic transmission may also explain these results.Citation28 Therefore, the increasing trend might be due to age-related cumulative exposure to pertussis. At the same time, there were regional differences in anti-PT IgG levels (x2 = 111.778, P < .01) and positivity rates (x2 = 36.524,P < .01) among different cities in Shaanxi province. The lowest positive rates were found in Yan’an(6.2%) and Hanzhong(4.0%) city, respectively, and there were no previous surveys on the level of anti-PT IgG in these two areas. It was speculated that this might be because of the geographical location of these two cities in mountainous areas with a relatively dispersed population density. In contrast, the highest positive rates were Yulin(15.8%) and Tongchuan city (13.6%). A significant difference was observed within the same province. These results further prove the necessity of monitoring the level of anti-PT IgG in this region and will provide a basis for formulating appropriate pertussis prevention and vaccination policies. In this study, anti-PT IgG concentrations and positivity rates showed significant differences between the sexes. There was no clear evidence for sex differences in pertussis antibody levels or positive rates. Li et al. found that the antibody levels of pertussis in males were higher than in females. This could be caused by sampling error.Citation29 Zhang et al. reported that the incidence of pertussis in males was higher than that in females, and the reasons for this difference remain to be further elucidated.Citation30 The sex differences in this study might have also been caused by sampling errors, as Li’s study.
On the one hand, adults are not only carriers of pertussis circulation and transmission, but also the reservoir for B. pertussis, posing a major threat to children’s health.Furthermore, most adults are also susceptible due to a lack of immune protection, of which mothers might pose the greatest threat to their babies. In response, maternal pertussis immunization practices have recently been adopted in some countries to protect young infants, whose illness is usually more severe, until they can accept their own routine primary vaccination program.Citation14 This measure can protect newborns through passive transplacental transfer, providing antibodies in the neonatal period from birth to two months old.Citation14 In Brazil, maternal immunization with the Tdap vaccine recommended vaccinating women at the 20th week of pregnancy.Citation31 In the United States, the Advisory Committee on Immunization Practices recommends that pregnant women receive one dose of Tdap during each pregnancy.Citation32,Citation33 Furthermore, some countries have implemented adolescent pertussis booster vaccinations following maternal vaccination.Citation34,Citation35 Several studies have been conducted to determine whether the immunization program for Tdap should be supported in women of childbearing age in China. Meng et al. revealed that 97.4% of newborns had no protection against pertussis in 194 paired cord and maternal blood samples.Citation36 Chen et al. found that 83.4% of infants (< three months) had undetectable anti-PT IgG (<5 IU/mL), and 2.0% of adults of childbearing age had true pertussis infection, which might be the main source of infant pertussis.Citation37 The above research suggests that booster vaccination in adults should be considered. However, until now, Tdap boosters for women of childbearing age, adolescents and adults have not been introduced in China.
Of all reported pertussis cases in China, 90% were infants or young children with classical “whooping cough” symptoms.Citation38 Studies have shown that only 40–50% of pertussis cases have the typical clinical manifestation of paroxysmal cough,Citation39 which is usually misdiagnosed as general respiratory infections and fails to investigate for pertussis. Because laboratory confirmation of pertussis by bacterial culture, polymerase chain reaction (PCR), or detection of a 4-fold increase in anti-PT IgG in serum is not routinely used in China, especially a 4-fold increase in anti-PT IgG which is hampered by low susceptibility in the later stages of the disease, the case definition of B. pertussis infection is mainly based on clinical diagnosis. Therefore, many cases of pertussis in vaccinated children, adolescents, and adults who do not have classical paroxysmal cough symptoms are unreported and might be considered common respiratory infections. In China, misdiagnoses have contributed to the low reported incidence (less than 1/100,000) since the 1990s. In Shaanxi, the average annual incidence of pertussis was reported to be 1.9/100,000, ranging from 0.2/100,000 to 6.2/100,000 each year from 2010–2019, according to the China Information System for Disease Control and Prevention. Only 26 (0.1/100,000) and 56 (0.2/100,000) cases were reported in 2009 and 2010, respectively. A total of 7,295 pertussis cases were reported in Shaanxi province from 2010 to 2019, of which only five adult cases were reported. In 2017, the same period as this study, only one adult case was reported in Shaanxi province by the China Information System for Disease Control and Prevention, which was much lower than this study (1.2%). The large difference in the incidence of pertussis reported in this study exposes a problem with the current pertussis surveillance system. This phenomenon can be attributed to several factors. First, from a technical point of view, we must admit that anti-PT IgG antibodies could reflect exposure/infection rather than clinical disease. Second, in terms of disease characteristics, pertussis symptoms are atypical under the current high vaccine coverage. Finally, because of the severity of the disease, the ability to seek medical care and diagnosis varies with age. Some teenagers and adults infected with pertussis may experience a slight cough and not go to the hospital, resulting in high underreporting rates, mainly among older children, adolescents, and adults. Only 42% of cases met a clinical definition of pertussis in 189 cases that tested positive for B. pertussis by PCR.Citation40 Pertussis without classic paroxysms is the cause of up to one-third of illnesses with prolonged cough in adolescents and adults.Citation41 Therefore, the existing surveillance system is no longer suitable for the daily surveillance of pertussis, especially for adults with atypical infections, and should be adjusted to adapt to new changes.
Unlike the high incidence of pertussis, no diphtheria cases have ever been reported in the past 26 years in Shaanxi province, and no cases have been reported since 2007 in China. This shows that the diphtheria vaccine had a good protective effect in both Shaanxi and China. Studies have shown that an effective immune barrier can be formed to prevent diphtheria outbreaks when the susceptibility rate of diphtheria (<0.01IU/mL) is lower than 25%.Citation42 In this study, the mean concentration of anti-DT IgG was 0.04 IU/mL (95% CI = 0.04–0.05), and the positive rate (≥0.01 IU/mL) was 82.3% (3543/4307). This finding is consistent with those of other provinces in China. Liang et al. found the positive rate of anti-DT IgG was 81.3%(1692/2081) in those aged 20–60 years old.Citation43 Yao et al. reported that 93.3% (167/179) of adults ≥20 years old were anti-DT IgG positive.Citation44 The positive rate was reported as high as 100% in a small sample (210 subjects).Citation23 Therefore, it can be considered that a strong population immune barrier has been established in China, including Shaanxi province, and it is unlikely that a diphtheria outbreak will occur. In contrast, Li et al in a cross-sectional study reported that the positive rate of anti-DT in different age groups was between 34.1% and 59.0% in adults over 20 years old.Citation29 Similarly, it is worth noting that the positive rate of anti-DT IgG among different cities in Shaanxi province still showed obvious regional differences(xCitation2=183.4,P < .01). The lowest positive rate in Yan’an was only 59.9% and the highest in Tongchuan was as high as 98.1%. In addition, diphtheria remains a problem in low-income countries with low immunization coverage. In 2017, Bangladesh experienced an outbreak of diphtheria in a large refugee camp.Citation45 Nepal, Indonesia and India currently have the most diphtheria cases in Asia.Citation18,Citation19 It is worth noting that Nepal, Bangladesh and India are all neighboring countries of China. In this study, 17.7% (764/4307) of adults did not have immune protection against diphtheria antibodies (<0.01 IU/mL), and they were at high risk of diphtheria infection. Even in a few countries with rather high immunization coverage, such as Iran and Thailand, there have been 513 and 157 outbreaks respectively, in recent years.Citation18,Citation19 Infants from birth to three months old, who do not obtain enough maternal antibodies, are at a high risk for diphtheria infection. A Tdap booster should be considered for women of childbearing age. In this study, the concentration of anti-DT IgG (x2 = 209.433, P < .01) and the positive rate (x2 = 36.102, P < .01) both showed a downward trend with age, which was consistent with other domestic research results. Zhu et al. found that anti-DT IgG levels decreased with age among subjects aged 0–49 years old in Guangdong province(r = −0. 43, P < . 01).Citation46 Geng et al. reported that the concentrations of anti-DT IgG(x2 = 226. 45, P < .01)and sero-positivity (F = 380.10, P < .01) decreased with increasing age in healthy people in Henan province.Citation47 Chen et al. reported a negative correlation between age and anti-DT IgG levels (r = −0.50, P = .01) among subjects aged 0–61 years old in Fujian province.Citation48 Therefore, Tdap vaccination should be considered for adults. Numerous studies have confirmed that there are no statistically significant differences in the level and positivity rate of anti-DT IgG in relation to sex. However, this survey showed that the positive rate and level of anti-DT IgG in males were higher than those in females in the Shaanxi province. Studies have shown that the antibody levels decrease with age. Chen et al. found that the level and positive rate of anti-DT IgG in males in Fujian province were higher than in females, and the reason for this phenomenon was that the proportion of males <15 years old was higher than that of females.Citation48 In this study, among males, the subjects ≤30 years old accounted for 55.0%, while among females, they only accounted for 38.3%. Therefore, the sex difference could be related to the difference in age group composition of the different sexes.
Conclusions
In summary, our study showed that, although high vaccination coverage among infants and young children has sharply reduced pertussis morbidity, B. pertussis is still circulating in China. Because adult pertussis is not uncommon, pertussis booster vaccination should be considered in adults in China, especially in pregnant women, to protect infants who are too young to be vaccinated. Moreover, the existing surveillance system is inadequate to identify adolescents and adults with mild pertussis and may underestimate the true incidence of pertussis in Shaanxi. Strong measures should be taken to increase the surveillance sensitivity. Although a high proportion of individuals had some immune protection against diphtheria, the antibody levels were found to decrease with age.
Ethical considerations
This study was approved by the ethics committee of the Shaanxi Provincial Center for Disease Control and Prevention. Informed consent was obtained from all participants before blood samples were collected.
Acknowledgments
The authors wish to thank all staff at the city/county CDC in Shaanxi involved in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Jakinovich A, Sood SK. Pertussis: still a cause of death, seven decades into vaccination. Curr Opin Pediatr. 2014;26(5):1–8. doi:10.1097/MOP.0000000000000139.
- Zamir CS, Dahan DB, Shoob H. Pertussis in infants under one year old: risk markers and vaccination status–a case-control study. Vaccine. 2015;33(17):2073–78. doi:10.1016/j.vaccine.2015.02.050.
- Organization WH. Pertussis global annual reported cases and DTP3 coverage, 1980-2015.
- Cherry JD. Epidemic pertussis in 2012–the resurgence of a vaccine-preventable disease. N Engl J Med. 2012;367(9):785–87. doi:10.1056/NEJMp1209051.
- World Health Organization. Pertussis vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85(40):385–400.
- Octavia S, Sintchenko V, Gilbert GL, Lawrence A, Keil AD, Hogg G, Lan R. Newly emerging clones of Bordetella pertussis carrying prn2 and ptxP3 alleles implicated in Australian pertussis epidemic in 2008-2010. J Infect Dis. 2012;205(8):1220–24. doi:10.1093/infdis/jis178.
- Amirthalingam G, Gupta S, Campbell H. Pertussis immunisation and control in England and Wales, 1957 to 2012: a historical review. Euro Surveill. 2013;18(38):20587.
- Winter K, Glaser C, Watt J, Harriman K. Pertussis epidemic–California, 2014. MMWR Morb Mortal Wkly Rep. 2014;63:1129–32.
- Mattoo S, Cherry JD. Molecular pathogenesis, epidemiology, and clinical manifestations of respiratory infections due to Bordetella pertussis and other Bordetella subspecies. Clin Microbiol Rev. 2005;18(2):326–82. doi:10.1128/CMR.18.2.326-382.2005.
- Castagnini LA, Munoz FM. Clinical characteristics and outcomes of neonatal pertussis: a comparative study. J Pediatr. 2010;156(3):498–500. doi:10.1016/j.jpeds.2009.10.013.
- Nooitgedagt JE, de Greeff SC, Elvers BH, de Melker HE, Notermans DW, van Huisseling H, Versteegh F. Seroprevalence of Bordetella pertussis infection during pregnancy measured by IgG antibodies against pertussis toxin. Clin Infect Dis. 2009;49(7):1086–89. doi:10.1086/605575.
- Guimaraes LM, Carneiro EL, Carvalho-Costa FA. Increasing incidence of pertussis in Brazil: a retrospective study using surveillance data. BMC Infect Dis. 2015;15(1):442. doi:10.1186/s12879-015-1222-3.
- Clark TA. Changing pertussis epidemiology: everything old is new again. J Infect Dis. 2014;209(7):978–81. doi:10.1093/infdis/jiu001.
- Gkentzi D, Katsakiori P, Marangos M, Hsia Y, Amirthalingam G, Heath PT, Ladhani S. Maternal vaccination against pertussis: a systematic review of the recent literature. Arch Dis Child Fetal Neonatal Ed. 2017;102(5):F456–F63. doi:10.1136/archdischild-2016-312341.
- Tan T, Trindade E, Skowronski D. Epidemiology of pertussis. Pediatr Infect Dis J. 2005;24(5):S10–8. doi:10.1097/01.inf.0000160708.43944.99.
- Lartigue MF, Monnet X, Le Flèche A, Grimont PA, Benet JJ, Durrbach A, Fabre M, Nordmann P. Corynebacterium ulcerans in an immunocompromised patient with diphtheria and her dog. J Clin Microbiol. 2005;43(2):999–1001. doi:10.1128/JCM.43.2.999-1001.2005.
- Tiwari TS, Golaz A, Yu DT, Ehresmann KR, Jones TF, Hill HE, Cassiday PK, Pawloski LC, Moran JS, Popovic T. Investigations of 2 cases of diphtheria-like illness due to toxigenic Corynebacterium ulcerans. Clin Infect Dis. 2008;46(3):395–401. doi:10.1086/525262.
- Dureab F, Al-Sakkaf M, Ismail O, Kuunibe N, Krisam J, Müller O, Jahn A. Diphtheria outbreak in Yemen: the impact of conflict on a fragile health system. Confl Health. 2019;13(1):19. doi:10.1186/s13031-019-0204-2.
- Sharma NC, Efstratiou A, Mokrousov I, Mutreja A, Das B, Ramamurthy T. Diphtheria. Nat Rev Dis Primers. 2019;5(1):81. doi:10.1038/s41572-019-0131-y.
- Forsyth KD, Campins-Marti M, Caro J, Cherry JD, Greenberg D, Guiso N, Heininger U, Schellekens J, Tan T, von Konig Carl-Heinz W. New pertussis vaccination strategies beyond infancy: recommendations by the global pertussis initiative. Clin Infect Dis. 2004;39(12):1802–09. doi:10.1086/426020.
- Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24(5):S58–61. doi:10.1097/01.inf.0000160914.59160.41.
- Hodder SL, Cherry JD, Mortimer EA Jr., Ford AB, Gornbein J, Papp K. Antibody responses to Bordetella pertussis antigens and clinical correlations in elderly community residents. Clin Infect Dis. 2000;31(1):7–14. doi:10.1086/313913.
- Zhang Q, Han F, Nie Q, Ren H, Zhang B, Liu Q, He Q, Shao Z. Seroprevalence of antibodies to pertussis and diphtheria among healthy adults in China. J Infect. 2011;63(6):441–46. doi:10.1016/j.jinf.2011.07.018.
- Chen Z, Zhang J, Cao L, Zhang N, Zhu J, Ping G, Zhao J, Li S, He Q. Seroprevalence of pertussis among adults in China where whole cell vaccines have been used for 50 years. J Infect. 2016;73(1):38–44. doi:10.1016/j.jinf.2016.04.004.
- Zhang Y, Chen Z, Zhao J, Zhang N, Chen N, Zhang J. Increased susceptibility to pertussis in adults at childbearing age as determined by comparative seroprevalence study, China 2010-2016. J Infect. 2019;79(1):1–6. doi:10.1016/j.jinf.2019.04.011.
- He H, Yao P, Zhou Y, Deng X, Pan J, Hozbor DF. Is pertussis infection neglected in China? Evidence from a seroepidemiology survey in Zhejiang, an Eastern Province of China. PLoS One. 2016;11(5):e0155965. doi:10.1371/journal.pone.0155965.
- Liu D, Cheng X, Wei S, Yuan L, Chen C, Yao K. Decline of serologic immunity to diphtheria, tetanus and pertussis with age suggested a full life vaccination in mainland China. Hum Vaccin Immunother. 2021;17(6):1757–62. doi:10.1080/21645515.2020.1840253.
- Althouse BM, Scarpino SV. Asymptomatic transmission and the resurgence of Bordetella pertussis. BMC Med. 2015;13(1):146. doi:10.1186/s12916-015-0382-8.
- Li X, Chen M, Zhang T, Li J, Zeng Y, Lu L. Seroepidemiology of diphtheria and pertussis in Beijing, China: a cross-sectional study. Hum Vaccin Immunother. 2015;11(10):2434–39. doi:10.1080/21645515.2015.1062954.
- Zhang J, Xie X. Epidemiological characteristics for reported cases of pertussis from 2009 to 2019 in Tai’an City. Prog in Microbiol Immunol. 2021;49:68–72. doi:10.1111/j.1574-695X.2006.00174.x.
- Vaz-de-lima LRA, Sato HK, Fernandes EG, Sato APS, Pawloski LC, Tondella ML, de Brito CA, Luna EJA, Carvalhanas TRMP, de Castilho EA, et al. Association between the timing of maternal vaccination and newborns’ anti-pertussis toxin antibody levels. Vaccine. 2019;37(36):5474–80. doi:10.1016/j.vaccine.2019.04.079.
- Kim DK, Riley LE, Harriman KH, Hunter P, Bridges CB. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older - United States, 2017. MMWR Morb Mortal Wkly Rep. 2017;66(5):136–38. doi:10.15585/mmwr.mm6605e2.
- Kim DK, Riley LE, Harriman KH, Hunter P, Bridges CB, Woods L, Wilson A . Recommended immunization schedule for adults aged 19 years or older, United States, 2017. Ann Intern Med. 2017;166(3):209–19. doi:10.7326/M16-2936.
- Clark TA, Bobo N. CDC update on pertussis surveillance and Tdap vaccine recommendations. NASN Sch Nurse. 2012;27(6):297–300. doi:10.1177/1942602X12452443.
- Zepp F, Heininger U, Mertsola J, Bernatowska E, Guiso N, Roord J, Tozzi A, Damme P, et al. Rationale for pertussis booster vaccination throughout life in Europe. Lancet Infect Dis. 2011;11(7):557–70. doi:10.1016/S1473-3099(11)70007-X.
- Meng QH, Liu Y, Yu JQ, Li LJ, Shi W, Shen YJ, Li L, Zhan SN, Yang F, Wang YJ, et al. Seroprevalence of maternal and cord antibodies specific for diphtheria, tetanus, pertussis, measles, mumps and rubella in Shunyi, Beijing. Sci Rep. 2018;8(1):13021. doi:10.1038/s41598-018-31283-y.
- Chen Z, Pang J, Zhang N, Chen N, Ding Y, He Q. Seroprevalence study of pertussis in adults at childbearing age and young infants reveals the necessity of booster immunizations in adults in China. Vaccines (Basel). 2022;10(1): 84 .
- Ning G, Gao Y, Wu D, Li J, Li Y, Shao Z, Yin Z . Epidemiology of pertussis in China, 2011-2017. Chin J Vaccines Immunization. 2018;24:264–7+73.
- Gordon M, Davies HD, Gold R. Clinical and microbiologic features of children presenting with pertussis to a Canadian pediatric hospital during an eleven-year period. Pediatr Infect Dis J. 1994;13(7):617–22. doi:10.1097/00006454-199407000-00007.
- Waters V, Jamieson F, Richardson SE, Finkelstein M, Wormsbecker A, Halperin SA. Outbreak of atypical pertussis detected by polymerase chain reaction in immunized preschool-aged children. Pediatr Infect Dis J. 2009;28(7):582–87. doi:10.1097/INF.0b013e318197fac1.
- Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ. Pertussis: microbiology, disease, treatment, and prevention. Clin Microbiol Rev. 2016;29(3):449–86. doi:10.1128/CMR.00083-15.
- Kjeldsen K, Simonsen O, Heron I. Immunity against diphtheria 25-30 years after primary vaccination in childhood. Lancet. 1985;1(8434):900–02. doi:10.1016/S0140-6736(85)91675-7.
- Liang L, Ma Y, Wei J, Deng L, Wei Y, Zhong G, Liu W. Antibody levels against diphtheria among a healthy population in Guangxi Zhuang autonomous region, 2013. Chin J Vaccines Immunization. 2016;22:175–79.
- Yao N, Zeng Q, Wang Q. Seroepidemiology of diphtheria and pertussis in Chongqing, China: serology-based evidence of Bordetella pertussis infection. Public Health. 2018;156:60–66. doi:10.1016/j.puhe.2017.12.009.
- Polonsky JA, Ivey M, Mazhar MKA, Rahman Z, le Polain de Waroux O, Karo B, Jalava K, Vong S, Baidjoe A, Diaz J, et al. Epidemiological, clinical, and public health response characteristics of a large outbreak of diphtheria among the Rohingya population in Cox’s Bazar, Bangladesh, 2017 to 2019: a retrospective study. PLoS Med. 2021;18(4):e1003587. doi:10.1371/journal.pmed.1003587.
- Zhu Q, Liu M, Wu C, Tan Q, Shao X, Xu X, Zheng H. Diphtheria antibody levels in selected regions of Guangdong province, 2014. Chin J Vaccines Immunization. 2016;22:267–70.
- Geng S, Zhao M, Guo S, Zhang D, Xia H, Wan S, Cong K, Zheng H. Diphtheria antibody levels and sero-prevalence among healthy people of Xuchang city in 2020. Chin J Vaccines Immunization. 2021;27:537–39.
- Chen Z, Zhang H, Wang Q, Zhang S, Li D, Yang X, Zhou Y, Zheng K. Diphtheria antibody levels among a community-dwelling population aged 0-61 years in Fujian province, 2018. Chin J Vaccines Immunization. 2020;26:521–24.