ABSTRACT
This study aimed to explore the contextual factors that may be associated with missed opportunities for vaccination (MOV) from the perspectives of healthcare providers and caregivers attending primary healthcare facilities in the Cape Town Metro Health District, South Africa. The ultimate goal of the assessment was to help inform the design and implementation of a contextually appropriate quality improvement programme targeted at reducing MOV in primary healthcare settings. We used a theory-informed exploratory qualitative research design involving focus group discussions with caregivers of children aged 0–23 months; and in-depth interviews of facility staff. A thematic template analysis approach, integrating the theoretical domains framework (TDF) and the capability, opportunity and motivation model of behavior (COM-B) was used to code and analyze the data. Three focus group sessions were conducted, each consisting of 5–8 caregivers and five in-depth interviews involving facility staff. Capability factors comprised caregivers’ knowledge, attitude and behavior toward children’s immunization. Opportunity factors included the organization of immunization services, long waiting time, vaccine stock out, staff shortage and health workers’ attitude, knowledge and capability to assess children’s immunization status and needs. Motivation factors included optimism and beliefs about immunization, fear of vaccine-preventable diseases and immunization safety concerns. This study identified important caregiver-, provider- and health system-related factors, which influence immunization outcomes; offering useful contextual insights for informing quality improvement strategies for reducing MOV at primary healthcare level.
Introduction
While significant investments and efforts have been made to ensure universal access to immunization services in South Africa, it is evident that many eligible children are missing out on this vital health intervention across districts and provinces.Citation1,Citation2 Recent estimates suggest that immunization coverage remains below the globally accepted optimal level of 90% across all routine childhood vaccine doses in South Africa.Citation3 outlines immunization coverage estimates as proportions of fully vaccinated children from a recent national immunization coverage survey.Citation4 Suboptimal immunization coverage among children in South Africa has been attributed to several factors. At the individual level, these include factors such as low awareness of the importance of immunization, misperceptions and low socioeconomic status; while at the health system level, they include factors such as human resource shortage, health facility staff’s immunization knowledge gaps, and vaccine stock-outs, among others.Citation2,Citation5–7
Table 1. Provincial immunization coverage estimates for fully vaccinated children at 12 and 18 months*.
To accelerate and sustain immunization coverage progress, the World Health Organization (WHO) recommends the provision of immunization services at every contact with the health system.Citation8 This is owing to the recognition of missed opportunities for vaccination (MOV) as a major contributor to sub-optimal immunization coverage globally.Citation8,Citation9 A missed opportunity for vaccination refers to any contact with health services by an individual who is eligible for vaccination (unvaccinated or not up-to-date, and free of contraindications to vaccination), which does not result in the individual receiving all the vaccine doses for which s/he is eligible.Citation10 The prevalence of MOV varies widely across countries, with an average of 32.2% in low- and middle-income countries (LMICs).Citation11 Factors commonly associated with MOV include the failure of health providers to screen patients for eligible vaccine doses; perceived contraindications to vaccination on the part of providers or parents; vaccine shortages; and the non-integration of vaccination services with curative and other healthcare services.Citation12
Since 2016, there has been an increasing momentum at global level to conduct MOV assessments, to better understand the burden and its structural and contextual mechanisms.Citation13–15 Consequently, research efforts in this area have increased in recent years, with the availability of an increasing body of evidence on the prevalence of MOV and its associated factors across the world over the last decade, including in African and other LMIC contexts.Citation13,Citation14,Citation16–19 To date, however, little is known about the burden and determinants of MOV in the South African context.Citation5
Understanding the burden and contextual enablers of MOV is important for policy and practice as it will provide valuable research evidence to enable policy makers and facility managers to consider context-appropriate interventions for strengthening immunization programmes. Such understanding has become even more important for mitigating the further disruption of immunization services by the COVID-19 pandemic.Citation9,Citation20 It will help inform the institution of locally responsive immunization strategies and interventions, to optimize immunization access and coverage.
As part of a mixed-methods baseline assessment, this study aimed to qualitatively explore the individual, health system and contextual factors that may be associated with MOV from the perspective of health care providers and caregivers of children aged 0–23 months attending primary health care (PHC) facilities in Cape Town. The ultimate goal of the assessment was to help inform the design and implementation of a contextually appropriate quality improvement programme targeted at reducing MOV in PHC settings. From the quantitative component of the pre-implementation baseline assessment, we found an average MOV prevalence of 14.1%, ranging from 9.1% to 18.9% across sub-districts in Cape Town.Citation21 Nonetheless, the quantitative nature of the findings masks the underlying circumstantial and contextual factors influencing MOV, the understanding of which will help complement and contribute deeper insights to the quantitative findings. Using a theory-informed approach, we therefore conducted a qualitative exploration of enabling and hindering factors of MOV from the perspectives of key immunization stakeholders like caregivers and health facility staff in PHC settings in Cape Town.
Methods
Study design
We used a theory-informed, exploratory qualitative research design involving focus group discussions (FGD) with caregivers of children aged 0–23 months attending PHC facilities and in-depth interviews (IDI) of PHC facility staff.
Conceptual framework
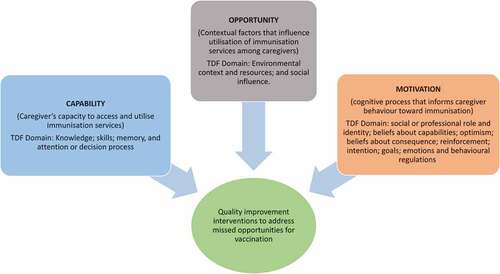
The theory-informed approach employed by this study integrates the theoretical domains framework (TDF)Citation22 and the capability, opportunity and motivation model of behavior (COM-B) model.Citation23 The TDF is a widely used integrative framework in qualitative research for exploring the factors that influence an outcome of interest. It consists of the following fourteen distinct, but interrelated, domains: knowledge; skills; social or professional role and identity; beliefs about capabilities; optimism; beliefs about consequence; reinforcement; intention; goals; memory, attention or decision processes; environmental context and resources; social influence; emotions and behavioral regulations.Citation22 To map identified factors to actionable goals, the capability, opportunity and motivation – behavior (COM-B) model was proposed to enable the translation of TDF findings into practical recommendations.Citation23 The COM-B model is a Behavior Change Wheel (BCW) approach useful for establishing a broad range of physical, psychological and external (contextual) mechanisms that can influence behavior.Citation23,Citation24 In the context of this model, capability refers to whether we have the knowledge, skills and abilities required to engage in a particular behavior. Opportunity entails the external factors which make the execution of a particular behavior possible, while motivation refers to the internal processes which influence our decision making and behaviors.Citation23
In the context of MOV, the capability construct of the COM-B model can be conceptualized to include caregiver’s capacity to access and utilize immunization services for their child when in contact with a health facility. That corresponds to the TDF domains of knowledge; skills; intention; memory, and attention or decision process. The opportunity construct entails contextual factors (health system, social and environmental) external to the caregiver that influence their decision to immunize their children when in contact with health facility, corresponding to the TDF domains of environmental context and resources, and emotion. The motivation construct comprises caregivers’ own cognitive processes that motivate or hinder behavior toward immunization. It corresponds to the TDF domains of social or professional role and identity; beliefs about capabilities; optimism; beliefs about consequence; reinforcement; intention; goals; and emotions and behavioral regulations. In the context of MOV, these allow for a systematic selection of interventions based on the various factors identified from qualitative analysis.
illustrates the relationship between the TDF and COM-B model in the context of MOV assessment and interventions.
Study setting
Administratively, South Africa is divided into nine provinces and 52 Districts. The metropolitan municipalities like Cape Town have the largest urban communities and perform the function of both district and local municipalities.Citation25 In the Western Cape Province, the Cape Town Metro Health district has 8 legislated sub-districts serving a population of 4.1 million persons.Citation26 There are 152 PHC facilities, 102 of which are managed by the City of Cape Town (local government) to augment PHC services provided by provincial facilities.Citation26 Like elsewhere in South Africa, routine immunization services in Cape Town are funded through the Expanded Programme on Immunization of South Africa (EPI-SA) and provided free of charge primarily through the PHC facilities.Citation1 While the Western Cape is often regarded as having a better resourced health system and health outcomes compared with other provinces, immunization coverage remains lower than optimal levels. For instance, a recent study has shown that more than a third (36.11%) of children in the province are incompletely immunized.Citation27 The current routine immunization schedule for children in South Africa is outlined in .
Table 2. Current routine childhood vaccination schedule in South Africa.
Sampling of participants
Eleven PHC facilities in the Cape Town Metro Health District participated in the study. Participants in the IDIs were selected from the participating facilities. To be eligible, they had to be current managers of the facility, should have been working there for a least a year at the time of the interview and willing to participate in the interview. For the FGD component, participants were caregivers of children aged 0–23 months who were aged 18 years or above attending any of the participating facilities, and resident in the catchment area of that facility. Potential IDI and FGD participants were approached by members of the research team at the clinics and informed about the research. Those who were interested and consented to participate were enrolled into the study. In all, three FGD sessions (each consisting of 5–8 caregivers) and five IDIs were conducted.
Data collection
Each FGD and IDI session was facilitated by two members of the research team experienced and trained in qualitative data collection and fluent in both English and local languages (Afrikaans and isiXhosa). The sessions were conducted using a semi-structured interview guide for the IDI and discussion guide for the FGD, both of which were adapted from the WHO’s MOV assessment guides for caregiver FGD and health worker IDI (attached as supplementary files).Citation10 The guides explored participants’ experiences, and perception in relation to immunization, MOV and ways to reduce MOV. Discussions were flexible to allow participants emphasize what they considered as important and to allow further probes into unanticipated topics emerging from participants’ responses. All sessions were recorded using an audio recorder and transcribed verbatim. Local language texts in the transcripts were translated to English by a professional translator. Back-translation from English to the original language was done to ensure accuracy of translation and that meanings are not lost in translation.
To supplement the audio recordings, one of the two facilitators jotted notes, reflections and captured non-verbal gestures such as facial expressions and nods. Each focus group lasted between 45 minutes and an hour, while each IDI session lasted 30–45 minutes. Attempts were made to ensure every participant was given the opportunity to contribute during discussions. All FGD and IDI sessions were held in private rooms at a mutually convenient time for the participants. Consent to participate was re-confirmed at the start of the IDIs. Upon initial coding and thematic analysis of audio recordings to keep track of emergent themes, it was decided that saturation had been reached at the third session of FGD and fourth session of the IDI.
Reflexivity
Given that the research team consisted of individuals who are knowledgeable and passionate about immunization, reflexivity was important to minimize the likelihood of researchers’ knowledge and potential bias influencing the research process, including how they asked questions and how they reacted to or interpreted participants’ responses.Citation28 Before the data collection and in one of the training sessions, the team engaged in reflexivity by collectively reflecting on expectations and assumptions within the context of the research and study participants. During the data collection process, the research team engaged in reflexivity through jotting notes about participants’ comments and non-verbal gestures that may add more meaning to responses. Furthermore, reflexivity was applied during coding and analysis of data, by continually reflecting and being mindful of personal and professional positionality in the interpretation of collected data.
Ethical considerations
Ethics clearance for this study was obtained from Human Research Ethical Committee (HREC) of the University of Cape Town (Reference number: HREC 579/2020). Signed informed consent was obtained from all study participants before data collection. It was explained to all study participants that participation is voluntary and that they can withdraw their participation any time without any prejudice. All data collected were anonymized. Audio recordings and transcripts were stored securely in password-protected devices and files accessible only to the research team, and were securely deleted once transcription was finalized and verified for accuracy.
Data analysis
A thematic template analysis approach was used for coding and organizing transcribed data segments for analysis.Citation29 This method allows for flexibility and contextual adaptability of thematic analysis.Citation30 Two codebooks were developed. In the first codebook, emerging themes were identified inductively from the transcripts, with illustrative quotations organized under each theme.Citation31 In the second codebook, the 14 domains of the TDF were specified and the themes identified in the first codebook were deductively adapted and matched to the corresponding domains of the TDF.Citation22 To enhance the accuracy and consistency of the analysis, the codes generated were independently verified against the raw data by the lead researcher. To avoid overlapping codes, only the most relevant codes were matched to a corresponding TDF domain. Each TDF domain was subsequently matched to the corresponding domain of the capability, opportunity and motivation model of behavior (COM-B).Citation23 The study was conducted in the pre-implementation phase of a quality improvement (QI) programme to reduce MOV in PHC facilities in Cape Town. Thus, the COM-B model was used to translate the findings from the second codebook into practical QI ideas capable of reducing MOV at the PHC level. This study was reported in accordance with the Standards for Reporting Qualitative Research (SRQR).Citation32
Results
Three FGD sessions, each consisting of 5–8 caregivers were conducted. Participating caregivers were all women, aged 20–42 years and resident in the Cape Town. At the time of enrollment into the study, all of them visited the health facilities with at least one child aged 0–23 months for reasons ranging from immunization and other preventive services to curative services. Of the five participants in the IDI, four were female while one was male. They were aged between 35 and 48 years with 10–15 years of experience as healthcare professionals. At the time of the interviews, all of them were staff and managers of their respective health facilities, with both administrative and clinical responsibilities.
In the sections below, findings from the FGD and IDI sessions are presented under the three constructs of the COM-B model (capability, opportunity and motivation) with reference to their corresponding TDF domains.
Capability construct
This construct comprises caregiver’s knowledge and capacity to access and utilize immunization services for their child when in contact with a health facility. It corresponds to TDF domains such as knowledge; skills; intention; memory, and attention or decision process. The findings are organized under the following emergent themes:
Caregivers’ knowledge of the importance of immunization
Many caregivers demonstrated good knowledge of the importance of vaccination. When asked what they thought were the ways by which common childhood illness could be prevented, many of the caregivers correctly identified immunization as one of such ways. For instance, one caregiver responded:
Immunization is very important as it helps and prevents diseases … I could say that it prevents something that has not occurred from occurring. So it is compulsory for people to always get immunization all the time. – FGD 1, P1
Another caregiver opined:
When a child has been immunized, this protects them. – FGD 1, P2
In addition to knowing the importance of immunization, some caregivers also had good knowledge of vaccine preventable diseases:
I feel it’s very important for the kid to have the immunization, it can prevent our kids from a lot of sickness like TB, poliomyelitis, like all those things. – FGD 2, P8
However, there were instances when caregivers’ responses reflected significant gaps in their knowledge about childhood immunization. For instance:
I am a grandmother to my child so I don’t have much knowledge … I don’t even know what I have brought the child for this time around. – FGD 1, P3
This trend was corroborated by facility staff, many of whom expressed concerns about the low level of immunization awareness and knowledge of some caregivers:
I’m telling you a lot of parents don’t know what the children is getting and they don’t know what it is for. – IDI P2
Another facility staff shared a similar experience:
To be honest with you there is still that level of not knowing or not understanding what is actually happening, what is the certain vaccine for. – IDI P3
Caregivers’ attitude and behavior toward children’s immunization services
Positive attitudes toward children’s immunization emerged from caregivers’ perspectives. Some caregivers narrated how they took personal responsibility and made conscious efforts to get their children immunized, such as by setting immunization appointment reminders:
For me, I set reminders on my phone, like write that on a particular date is the next appointment. Also I paste a paper on my wardrobe for both my children as well as for their appointment dates. – FGD 1, P2
Other emergent positive attitudes and practices included safe keeping of home-based immunization records documented in the Road to health booklets (RtHB), as expressed by this parent:
It is important for a parent to keep the child’s book safe and if it happens that you lose it, try by all means to get it again because you won’t know those dates without having that book with you. When you have the book, you can track that now the child will go for this particular injection and all. – FGD 1, P2
Moreover, some caregivers expressed their positive attitudes toward children’s immunization by asserting that they could spare a day off work; or ask a neighbor to take their children for immunization if they are unable to get a day off work:
The parent must have a mind-set of ‘As I am working today, the child must go for their immunization.’ You can even ask someone to take your child on your behalf while you work as the parent, but the child should not miss their vaccination date due to you saying you are going to work as the parent. – FGD2, P2
Conversely, many negative attitudes were also expressed and reported, one of the most common of which included caregivers not arriving early for their children’s immunization schedule:
I also wish that the parents could stop arriving late at the clinic. – FGD 3, P4
Another common attitude that came up during the discussions was the impatience of caregivers to wait for their children to be immunized, particularly during busy clinic days with longer waiting times:
There are parents that are impatient and won’t be able to stand in the queues – like myself – because I can’t go to the clinic at 06:00 am and then leave at 5:00 pm just waiting for an injection. So there needs to be a way in the clinics to ensure that parents don’t spend the whole day in the clinic. To not overbook people on certain days as well as ensure that there is enough stuff. – FGD1, P1
There were also reports by facility staff of caregivers being unwilling to allow clinic staff vaccinate their children, owing to personal reasons, notably misperceived concerns about vaccine safety. One facility staff noted:
If that mother doesn’t want that child vaccinated then what do I do? Because you cannot give a child immunization without mommies consent, because it becomes a problem. – IDI P2
Another facility staff added:
They think we’re giving the child a virus so the child is [going to] get the, the, the measles – especially the measles. – IDI P4
Opportunity construct
This construct comprises factors that are external to caregivers which influence whether or not children attending PHC facilities receive recommended vaccine doses during each facility visit. It corresponds to the TDF domains such as environmental context and resources, and emotion. At the PHC facility level, it comprises the organization of immunization services, as well as health workers’ attitudes, behaviors and capability to identify and administer missing immunization doses to children when in contact with a health facility.
Immunization services in clinics
Perceptions of facility managers regarding immunization services provided by their facilities were mostly positive. For instance, while immunization services are routinely provided on an appointment basis, there appeared be to efforts by health facilities to get children immunized at every clinic encounter from facility staff’s responses:
So it doesn’t mean that we’re strict on only the children that has appointments that we give the immunizations. If we notice that this child is coming for something else, but this child didn’t get maybe the measles injection then we’ll give it that same day. – IDI P1.
We have immunization register, we have appointment system…but we don’t depend that much on that schedule like for catch up. – IDI P4
According to some facility staff, their facilities make efforts to immunize children at every clinic visit even when children have not been given an immunization appointment, notwithstanding human resource shortages:
Even if there’s just one sister, we can’t defer immunizations. We must give that child […] even if the child comes 9, 3 o’clock for measles injection, we must open that vial. – IDI P1
These efforts were reinforced by health facilities’ compliance with existing vaccine multi-dose vial policies, as described by one facility staff:
Ten children can get a measles vial, but there’s a policy, there’s a policy in the City of Cape Town where it states that even if you have to open a vial for one child at 10 to 4, you do that. – IDI P4
There were also some indications of the integration of immunization services with other routine primary health care services:
We have an integrated approach, a holistic approach to care. Let’s say if the child is coming with the mommy who is coming for postnatal [sic: care] and the child happens to be 6 weeks, that sister in that [sic: postnatal] room … does immunizations. Her room is equipped. She’s got a cooler box, she’s got vaccinations in there, she’s attending to the mom, the baby must be sorted there as well. – IDI P5
Likewise, a facility staff from another PHC facility hinted on the facility-wide mainstreaming of vaccination and immunization services:
I’m trying to involve everybody so that one cannot work in that corner and the other one works in that corner everybody should know about the vaccination. IDI P3
The nature of immunization services provided at the clinics elicited intense concerns among caregivers. On a positive note, some caregivers expressed their satisfaction with the immunization services they received:
Yeah, and they do everything well. – FGD2, P1
Similarly, another caregiver noted:
I am happy with my own clinic, they are giving the best service and they don’t [sic: waste] time to help the children. I’m happy with their service. – FGD2, P6
Conversely, there were negative concerns and dissatisfactions expressed among caregivers about the quality of immunization services provided by the clinics. These concerns are organized under the following themes:
Attitude of health facility staff
One major concern commonly raised by caregivers was the unfriendly attitude of clinic staff:
Also you find that on the other hand the parents get shouted at. So I wish they could try and work hand-in-hand with the mothers so that the mothers are not intimidated by the nurses, feeling free to always go back to the clinic whenever they need help. – FGD1, P2
Another thing is that the nurses become rude once you miss the date and even when you tell them that your job does now allow you to attend the appointments, they tell you that, that is not their problem. What I wish to complain about is that even if the parent has missed the appointment date the child should be cared for. The child should get the immunization. The child should never leave the clinic without their immunization as there is nothing as important as immunization. – FGD1, P7
Caregivers also conveyed concerns about clinic staff not communicating effectively with them, leaving some parents unaware of reasons for their children’s clinic appointments or making some uncomfortable to ask questions about their children’s immunization schedules:
The nurses never explain to the parents the reason why the parent must bring the child for the appointment date. – FGD1, P3
Also you are normally scared to communicate with the nurses as they are often rude to the patients. – FGD1, P4
Many people are scared to ask because they fear that the nurse will be rude, so the nurses need to explain to the mothers with patients as some of the mothers are slow learners. – FGD 1, P3
Reports of unpleasant attitudes of PHC staff were corroborated during the IDI. For instance, one facility staff admitted:
Sometimes – like I say – we as nurses we aren’t really friendly. Sometimes not approachable. It’s the truth. – IDI, P4
Long waiting time
Dissatisfaction about long queues and long waiting times during immunization sessions was commonly voiced by caregivers:
You get there and sit the whole day without getting anything. – FGD 1, P1
You have an appointment at 10. You leave at home around to 10 because you know that it takes you 15 minutes to go to the clinic. You get there and wait. At 10 you pass at the reception and leave your child’s card and sit down. 10 passes by and you’re still sitting there – FGD2, P7
One parent gave a hint of how long (in duration) waiting times could be for caregivers:
Around 10:45 am when you take your child for the 11:00 am appointment you find that the clinic cards for the 8:00 am appointments have not been fetched from the parents. So when are you going to leave the clinic if they haven’t started with the 8:00 am appointments at 11:00 am?. – FGD2. P6.
Long waiting time was particularly concerning for caregivers who have to go to work:
There are cases where they say that from Monday to Thursday we are seeing children. When going there on Friday maybe that’s the only day you got an off-day from work, you go the clinic and they tell you that they can’t see you so you will need to come back some other day. So they need to prioritize the availability of the clinic. At any given time or day immunization should be available for parents. – FGD1, P1.
This was corroborated by a clinic staff:
The other day the lady they said Mr, when are you attending to us because at 9 o’clock I need to be at work. But I said my dear look here your queue, it’s a long queue. – IDI P2.
Vaccine availability
Some caregivers and facility staff expressed concerns about vaccine stockouts, although this issue was not raised by the majority of participants. A facility staff acknowledged:
There is a stockout of one of the immunizations and that happens very seldom but there has been incidences yeah where there was stock, stockouts. – IDI P5.
In some cases, caregivers described being asked to procure immunization services from local pharmacies. One caregiver narrated:
At the clinics I wish they could ensure that they have stock because they sometimes send us to Clicks and when you go to Clicks you find out that the injection is R400. – FGD 1, P1.
Staff shortages
Human resource shortages were almost unanimously pointed out as a major concern by caregivers and health workers alike. There were reports of children being sent home without vaccination in some of such cases:
At my clinic there is a shortage of staff since 2018 so they always book a small number of kids on the system that they cannot attend to in a day ending up having to send the parents back home. So I think this is the reason why some children miss their injections. – FGD 1, P6.
One of the nurses once said that I won’t attend the one that the child never came for, I will only do the one that they came for today. – FGD 1, P1.
And the staff, because they sometimes say ‘No, we only have two nurses,’ so those with their cards with them still must return home – FGD 1, P5.
Similarly, facility staff noted the impact of staff shortages:
You find here at the facility the professional nurse, I must say, it’s given a lot of work. You must do the admin; you must see the sick children, you understand. – IDI P2.
Use of road to health booklets (RtHB)
Both caregivers and facility managers shared mostly positive views on the importance and use of RtHBs for documenting and tracking children’s health status, including immunization status during clinic visits. Most caregivers take their children’s RtHBs with them during clinic visits. When asked the importance of the booklet, caregivers had these to say:
When you look at the card, the ages for a child’s immunization are stipulated. – FGD1, P4.
Once you lose that book you won’t know the injections that the child has already taken, and you will forget the written dates for the other appointments as you can’t keep them by heart. – FGD1, P4.
I can also add that it is important that the nurses look at the child’s book and follow the dates, starting from the previous ones to ensure that the child’s injections go as needed – FGD1, P5.
When asked about how frequently they checked children’s RtHBs for immunization status and missing vaccine doses, the majority of the health facility staff responded that they routinely did that. However, there were hints that this was not always the case, as one clinic staff admitted:
To be honest neh[sic], I am somebody [chuckles] what always check on the immunization chart. It is[…]I can’t say for the next person. – IDI P1
Staff shortages and excessive workloads were cited as some of the reasons why facility staff do not check the RtHBs:
I always check. Personally I always check. But the next person, […]They’re working so under pressure, neh[sic], they have like 40, 50 clients siting outside and maybe that client is coming for sick – neh[sic] the child’s maybe coming for sick, but they won’t take note of the immunization. They will focus only on that because their time is so limited. – IDI P1
Health workers’ knowledge and perception about contra-indications to vaccination
When asked to mention valid contraindications to vaccination, facility staff commonly identified fever as one:
So the only reason we won’t vaccinate a child if the child has a fever – obviously 38 and above. That’s the only time, and then we’ll obviously tell the mom maybe in the two days’ time we will tell the mommy to come back and then we’ll vaccinate if the child’s fever has settled then we will catch up on that. But that’s the only reason; if the child has a fever of 38 and above. – IDI P1
The only time, we have to it, we are actually forced, we making sure that every child that comes inside, if the child has been sick for instance if the child has had a high temperature more than, 38 and above we don’t immunize that child. – IDI P3.
Acute childhood illnesses were also commonly mentioned as a contraindication:
So even if the child comes in – the child is not sick; he’s coming for vaccination neh[sic] - we will give that child the immunization. – IDI P4.
Information on immunization and communication of adverse events following immunization
According to many caregivers, they were often not given information on immunization and possible adverse effects during immunization sessions: Caregivers shared their experiences on these:
They don’t even teach you anything. You just sit there whilst they are busy with your baby. They never explain to you what they are doing, especially when you are a mother for the first time. – FGD1, P1.
The nurses never explain to the parents the reason why the parent must bring the child for the appointment date. Also openness with the nurse at the clinic so that as the mother you can freely ask. – FGD1, P3.
But the problem is they just inject the baby and you don’t know what the injection is for, you understand. You know it’s the baby’s injection, but what is the injection for or what it protects the child from, you don’t know. – FGD2, P1.
As a result of not being informed about the possible adverse events following immunization, some caregivers reported not knowing what to do when an adverse event occurs following immunization:
The baby can have fever after the vaccination. They give to my baby the immunization. After one hour, two hour my baby was okay, and after three hours I said ‘No, no I must check my baby.’ I touched him, he had a fever. I went to the clinic and they said “You didn’t know, you were supposed to give him Panado,” but no one told me. No one explained. – FGD2, P3.
Motivation construct
This construct comprises personal and external (sociocultural) factors that may boost or hinder caregivers’ intrinsic motivation to immunize children during health facility visits. It corresponds to TDF domains such as beliefs about capabilities; optimism; beliefs about consequence; reinforcement; intention; goals; and behavioral regulations. The factors identified here include optimism about immunization, knowledge of the importance of vaccines, fear of vaccine-preventable diseases and concerns about adverse events following immunization.
Perceptions about common childhood diseases and the role of immunization
The fear of children becoming sick with vaccine-preventable illnesses was a major motivating factor for caregivers’ decision to immunize children. This underlying perception is that children who are immunized tend to be healthier than those who are not. Some caregivers shared their experiences and opinions on this:
I find that when they immunize the child, the child is protected from falling ill all the time. For example, with other children you will see that they are full of sores, but my children are fine as I take them regularly to the clinic. – FGD1 P2.
[…] so since I used to travel back and forth between Cape Town and the Eastern Cape, so I realized that my child missed the measles injection, so when the child was approaching 2 years the child fell ill with measles and when they looked they saw that the child had missed the measles injection. – FGD1 P3.
Perceptions, beliefs and sociocultural influences
Some sociocultural factors capable of influencing caregiver’s decision to immunize a child when visiting a health facility emerged from the FGDs. Notably, some caregivers mentioned the positive role of health support groups:
We do attend the groups. They teach us about everything as well as remind us that the child needs to attend their immunization appointments. So getting this information from these groups helps us a lot now. – FGD4 P1.
The influence of social media was also highlighted:
When you have opened that Facebook page, you get some advice from the other mothers. – FGD3 P3.
However, caregivers suggested that prevailing socio-cultural practices and beliefs exist that frequently dissuade them from allowing their children to be immunized. These included misperceptions and rumors that a child can become sick from immunization:
There are rumors and theories that once a child is immunized, they end up getting sick. – FGD2 P1.
Where I stay, no one cares about immunization. It is probably 5% out of 100% that go for immunization because they give each other wrong information. They tell each other lies that when you take your child for immunization the child will get sick. As a result, their children are always not well. – FGD1 P6.
Perceptions of vaccine safety
Fear of adverse events following immunization emerged as one of the factors potentially undermining caregivers’ motivation to immunize children. In addition to common side effects such as fever, caregivers also cited some implausible effects such as tumors:
I wish they can explain the side effects of immunization because I realized that with the one injected here, after some time it changes to become a pimple and so I Googled it and then realized that it was normal, but it was becoming a tumor. – FGD1 P1.
A major enabling factor of such misconceptions include gaps in knowledge of adverse events following immunization and clinic staff not informing caregivers about them:
I also agree that we should be taught by the clinic that after a certain vaccine there will be side effects so that we are not shocked when these things happen. – FGD1 P5.
It also seemed that these misperceptions persisted despite efforts by health facility staff to educate caregivers – as expressed by a facility staff:
We always explain to the parents “It’s not a live virus, it’s a dead – polio is dead that we’re giving. It’s just […] to build immunity. They think we’re giving the child a virus so the child is [going to] get the, the, the measles – especially the measles. – IDI P4
Discussion
Using a theory-informed, exploratory qualitative research approach this study explored the factors that influence missed opportunities for childhood vaccination from the perspectives of key stakeholders like caregivers and health facility staff. Various important opportunities for addressing MOV and immunization service delivery gaps in PHC settings were identified. These factors were mapped along the thematic domains of the TDF, and matched to their corresponding constructs of the COM-B model to establish the actionable elements of PHC-level quality improvement strategies targeted at reducing MOV. Importantly, the study complements and sheds contextual light on the findings from the quantitative component of our baseline assessment of the magnitude of MOV and factors associated with it across sub-districts in Cape Town.Citation21
Several capability factors that can influence MOV were identified in this study. While some caregivers were knowledgeable of the importance of immunization, there were however remarkable knowledge gaps, admitted by many of the caregivers themselves and corroborated by clinic staff. Caregivers’ attitude and behavior toward children’s immunization services that may contribute to MOV include arriving late for their children’s immunization appointments or not being patient enough to have children vaccinated before leaving the health facility. Consistent with the findings by previous studies in Nigeria and Timor-Leste, these factors can contribute to children not receiving age-eligible immunization during healthcare visits, thereby constituting common drivers of MOV.Citation18,Citation33 For instance, our quantitative study found that MOV was significantly associated with caregivers’ low levels of immunization awareness.Citation21
For any PHC-level intervention to effectively address MOV, these capability issues warrant due attention. Strategies for addressing caregivers’ immunization knowledge gaps and attitudinal factors include facility-level efforts aimed at improving both caregiver awareness and understanding of the importance of vaccines and possible adverse events following immunization. We found that caregivers repeatedly expressed the desire and willingness to be informed and learn about their children’s immunization. This is an important opportunity that could be leveraged for intensifying immunization messaging and communication. There is substantial evidence that immunization-themed health education interventions, when tailored to the target audience’s needs such as in local languages, can increase both caregivers’ immunization knowledge and intention to vaccinate.Citation34,Citation35 Education interventions can be implemented at the facility level through health talks during immunization sessions, and non-immunization areas such as waiting rooms; antenatal and postnatal clinics; and displaying posters and charts with information about immunization in prominent areas of PHC facilities.
In the opportunity construct, the study found factors relating to the organization of immunization services, availability of immunization resources as well as health workers’ attitudes, behaviors and ability to identify children missing immunization doses during PHC encounters. These factors are external to caregivers but can strongly influence whether or not children attending PHC facilities receive recommended vaccine doses during each facility visit. These findings substantiate those from our earlier quantitative assessment showing that long waiting time and staff shortages are common PHC facility-level challenges associated with MOV.Citation21 Other factors such as the unfriendly attitude of health workers and vaccine stock-outs can interact with caregivers capability and attitude toward children’s immunization. For instance, long immunization waiting time can discourage caregivers and make them impatient to wait for children to be vaccinated during facility visits for both immunization and non-immunization reasons. Likewise, caregivers not arriving early for immunization appointments can provoke or reinforce unfriendly attitudes of health workers toward them. These go to show the inter-relationship between individual and health system factors, and how one can reinforce the other in the context of MOV. Even if vaccines are available in a public primary health care facility, its utilization for children can still be influenced by contextual factors that are external to their caregiver, which can be social or environmental.
The finding that health facility staff do not always screen RtHBs for children’s immunization status is noteworthy. This can be attributed to factors such as staff shortages and non-integration of immunization services with other routine PHC services.Citation13,Citation36 Thus, it is important that PHC facility patient-flow policies and guidelines are revised to establish formal policies for facility-wide RtHB screening and immunization status checks at every health service encounter. There is a need for facility-wide service delivery policies to create an enabling environmental for all health facility staff, including immunization and non-immunization personnel to correctly screen children’s immunization status and identify opportunities for administering catch-up vaccine doses at all service delivery points. Additionally, efforts are also needed to encourage caregivers to retain and bring children’s RtHBs to every health service encounter to aid immunization status checks.
There were indications of health workers’ knowledge gaps, particularly in terms of national immunization policies and guidelines and valid contraindications to immunization. Notably, the common perception among health workers that fever is an absolute contraindication to immunization warrants due attention. Previous studies assessing MOV had similar findings.Citation13,Citation14,Citation33 PHC authorities and immunization should explore strategies for improving health worker knowledge and competences on vaccine eligibility, co-administration, valid contraindications and policies for opening multi-dose vials and catch-up of delayed vaccinations. This can be achieved through training and retraining to raise awareness about immunization among health workers; such knowledge is expected to have a positive spill-over effect to caregivers.Citation37 Also important is the re-organization of PHC services such that immunization services are well integrated with other routine PHC services. To ensure effective integration, it is important that vaccines and other immunization supplies are made available at non-immunization service delivery points. This is especially crucial for mitigating the rate of MOV in children accessing non-immunization services, given the evidence that the likelihood of MOV may be higher in such settings.Citation13,Citation19,Citation21
Another key finding of this study relates to vaccine availability. While vaccine stockouts were uncommon from the perspectives of the caregivers and health workers, some participants expressed particular concerns about them. In some cases, caregivers were asked to procure immunization services from local pharmacies. Cost is a recognized barrier to accessing immunizationCitation36,Citation38 As such, is it imperative that these supply-side constraints are taken into account when planning and implementing remedial measures against MOV.
Several personal and external factors that may enhance or undermine caregivers’ motivation to immunize their children during health facility encounters were found in this study. Notably, the fear of children becoming sick with vaccine-preventable illnesses was a major motivating factor. The awareness and beliefs about the consequences of vaccine-preventable diseases can reinforce motivation and positive behavior toward immunization.Citation39,Citation40 However, the fear of side effects emerged as one of the factors potentially undermining caregivers’ motivation for immunization. Studies have shown that concerns around vaccine safety, founded or unfounded can influence caregivers’ behavior and reduce their motivation to immunize children.Citation41,Citation42 In addition to common side effects such as fever, caregivers also cited some implausible effects such as tumors. A major enabling factor of such misconceptions include gaps in knowledge of adverse effects following immunization and the health workers not informing caregivers about side effects. Strategies for addressing these include those aimed at reinforcing immunization education; improving health workers’ communication of possible adverse events to caregivers; initiating personal conversations with caregivers with particular safety concerns or misperception to allay fears and dispel myths; and using more motivated and knowledgeable caregivers as local influencers to boost other caregivers’ attitude and perceptions toward immunization at the PHC facility level.
outlines the key MOV-related issues mapped under the three constructs of the COM-B model and corresponding TDF domains; and illustrative quality improvement strategies targeted at each issue.
Table 3. COM-B construct and TDF domain mapping of factors associated with MOV and their implications for PHC-level quality improvement.
Strengths and limitations
The theory-informed design of this study allowed for a methodologically rigorous and systematic exploration of the factors associated with MOV from the perspective of caregivers and health workers. It also enabled the identification of individual and external (sociocultural and health system) factors, while establishing the interrelationships between them in the context of MOV and broader immunization service delivery outcomes at the PHC level. Nonetheless, the study is not without limitations. First, the purposive sampling and small number of participants, a limitation inherent in qualitative designs, have implications for the generalizability of the findings and recommendations beyond the study context. Notwithstanding this limitation, the context-specific focus of the study also has some merit in being able to offer insights for the qualitative assessment of MOV, while informing the conceptualization of PHC-level immunization service quality improvement initiatives in different contexts.
The study is also prone to social desirability bias common in research of this nature. This was however mitigated by assuring participants of their anonymity and the confidentiality of their responses. Lastly, it is also worthy to note that the study’s convenience sampling, its focus on caregivers of children aged 0–23 months and health workers in public PHC facilities in an urban setting; and the fact that only female caregivers participated in the study, limit the generalizability of study findings and their implications to older children, male caregivers, non-PHC healthcare facilities and rural settings. However, this age-group restriction is consistent with the MOV assessment methods recommended by the WHO.Citation10 The participation of only female caregivers may also reflect the gendered nature of children’s healthcare experiences in the study context. Moreover, the majority of the children in the study setting rely on public PHC clinics for immunization, making the caregivers and health staff in these settings key stakeholders whose perspectives are likely to be more reflective of the lived experiences regarding MOV.
The above-mentioned limitations therefore underscore the need for future qualitative MOV assessments to involve a gender-diverse sample of participants; and health facilities across all care levels, in both public and private healthcare sectors and spanning both rural and urban settings. It would also be valuable for future studies to assess MOV in non-facility settings where children make contact with health services; such as mobile clinics and community health outreaches, where the burden of MOV may be more substantial.
Conclusion
This study identified important caregiver, provider and health system-related factors, which influence immunization outcomes and MOV among children in PHC settings in Cape Town. The findings offer useful practical and contextual insights for informing PHC-level quality improvement strategies for reducing MOV and ultimately improving immunization coverage at the population level.
Author contributions
Conceptualization, C.A.N., D.N. and C.S.W.; methodology, C.A.N., S.C., D.N. and C.S.W.; formal analysis, C.A.N. and D.N.; data curation, C.A.N. and D.N.; writing – original draft preparation, C.A.N.; writing – review and editing, C.A.N., D.N., S.C., A.M., L.L., T.M., N.K., M.L. and C.S.W.; supervision, D.N., M.L. and C.S.W.; project administration, C.AN. and D.N.; funding acquisition, D.N. and C.S.W. All authors have read and agreed to the published version of the manuscript.
Supplemental Material
Download PDF (570.1 KB)Supplemental Material
Download PDF (563.3 KB)Acknowledgments
We are grateful to colleagues at the Western Cape and City of Cape Town Departments of Health, facility managers and clinic staff for their cooperation and supports in various ways. We also owe a debt of gratitude to the field workers and research participants without whose valuable inputs and participation the study would not have been possible
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2162771
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Burnett RJ, Dlamini NR, Meyer JC, Fernandes L, Motloung BR, Ndlovu TH, Simango HA, Kibuuka DK, Dochez C, Montwedi DN, et al. Progress towards obtaining valid vaccination coverage data in South Africa. S Afr J Sci. 2019;115(5/6):4. doi:https://doi.org/10.17159/sajs.2019/6060.
- Mothiba TM, Tladi FM. Challenges faced by professional nurses when implementing the expanded programme on immunisation at rural clinics in Capricorn District, Limpopo. Afr J Prim Health Care Fam Med. 2016;8(2):e1–13. doi:10.4102/phcfm.v8i2.923.
- World Health Organization (WHO). WHO/UNICEF estimates of national immunization coverage; 2020 July [accessed 2022 Jan 11]. https://apps.who.int/immunization_monitoring/globalsummary/timeseries/tswucoveragedtp3.html.
- Republic of South Africa. Expanded programme on immunisation (EPI) national coverage survey report 2020. Department of Health Pretoria South Africa; 2020. https://www.health.gov.za/wp-content/uploads/2022/03/National-EPI-Coverage-Survey_Final-full-report-Dec-2020.pdf.
- Jacob N, Coetzee D. Missed opportunities for immunisation in health facilities in Cape Town, South Africa. South Afr Med J = Suid-Afrikaanse tydskrif vir geneeskunde. 2015;105(11):917–21. doi:10.7196/SAMJ.2015.v105i11.10194.
- Wiysonge CS, Ngcobo NJ, Jeena PM, Madhi SA, Schoub BD, Hawkridge A, Shey MS, Hussey GD. Advances in childhood immunisation in South Africa: where to now? programme managers’ views and evidence from systematic reviews. BMC Public Health. 2012;12(1):578. doi:10.1186/1471-2458-12-578.
- Burnett RJ, Mmoledi G, Ngcobo NJ, Dochez C, Seheri LM, Mphahlele MJ. Impact of vaccine stock-outs on infant vaccination coverage: a hospital-based survey from South Africa. Int Health. 2018;10(5):376–81. doi:10.1093/inthealth/ihy036.
- Hutchins SS, Jansen H, Robertson SE, Evans P, Kim-Farley RJ. Studies of missed opportunities for immunization in developing and industrialized countries. Bull World Health Organ. 1993;71(5):549.
- Nnaji CA, Ndwandwe D, Lesosky M, Mahomed H, Wiysonge CS. Tackling missed opportunities for vaccination in a new era of immunisation. Lancet. 2021;398:21. doi:10.1016/S0140-6736(21)01226-5.
- World Health Organization. Methodology for the assessment of missed opportunities for vaccination. Geneva (Switzerland): WHO; 2017.
- Sridhar S, Maleq N, Guillermet E, Colombini A., Gessner BD. A systematic literature review of missed opportunities for immunization in low- and middle-income countries. Vaccine. 2014;32(51):6870–79. doi:10.1016/j.vaccine.2014.10.063.
- World Health Organization (WHO). Methodology for the assessment of missed opportunities for vaccination. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2017.
- Ogbuanu IU, Li AJ, Anya BP, Tamadji M, Chirwa G, Chiwaya KW, Djalal MEH, Cheikh D, Machekanyanga Z, Okeibunor J, et al. Can vaccination coverage be improved by reducing missed opportunities for vaccination? findings from assessments in chad and malawi using the new WHO methodology. PloS One. 2019;14(1):e0210648. doi:10.1371/journal.pone.0210648.
- Okeibunor JC, Ogbuanu I, Blanche A, Chiwaya, K, Chirwa, G, Machekanyanga, Z, Mihigo, R, Zawaira, F. Towards a strategy for reducing missed opportunities for vaccination in malawi: implications of a qualitative health facility assessment. J Immunol Sci. 2018;2(SI1):46–54. doi:10.29245/2578-3009/2018/si.1107.
- Magadzire BP, Joao G, Shendale S, Ogbuanu, IU. Reducing missed opportunities for vaccination in selected provinces of Mozambique: a study protocol. Gates Open Res. 2017;1:5. doi:10.12688/gatesopenres.12761.1.
- Uthman OA, Sambala EZ, Adamu AA, Ndwandwe, D, Wiyeh, AB, Olukade, T, Bishwajit, G, Yaya, S, Okwo-Bele, J-M, Wiysonge, CS. Does it really matter where you live? A multilevel analysis of factors associated with missed opportunities for vaccination in sub-Saharan Africa. Hum Vaccin Immunother. 2018;14(10):2397–404. doi:10.1080/21645515.2018.1504524.
- Sambala EZ, Uthman OA, Adamu AA, Ndwandwe D, Wiyeh AB, Olukade T, Bishwajit G, Yaya S, Okwo-Bele J-M, Wiysonge CS. Mind the gap: what explains the education-related inequality in missed opportunities for vaccination in sub-Saharan Africa? Compositional and structural characteristics. Hum Vaccin Immunother. 2018;14(10):2365–72. doi:10.1080/21645515.2018.1460985.
- Li AJ, Peiris TSR, Sanderson C, Nic Lochlainn, L, Mausiry, M, da Silva, RBJBM, Ogbuanu, IU. Opportunities to improve vaccination coverage in a country with a fledgling health system: findings from an assessment of missed opportunities for vaccination among health center attendees—timor Leste, 2016. Vaccine. 2019;37(31):4281–90. doi:10.1016/j.vaccine.2019.06.041.
- Adamu AA, Uthman OA, Gadanya MA, Adetokunboh OO, Wiysonge CS. A multilevel analysis of the determinants of missed opportunities for vaccination among children attending primary healthcare facilities in Kano, Nigeria: findings from the pre-implementation phase of a collaborative quality improvement programme. PloS One. 2019;14(7):e0218572. doi:10.1371/journal.pone.0218572.
- Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, Hogan D, Dansereau E, Jit M, Flasche S; LSHTM CMMID COVID-19 Working Group. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020 Oct;8(10):e1264–e1272. doi:10.1016/S2214-109X(20)30308-9.
- Nnaji CA, Wiysonge CS, Adamu AA, Lesosky M, Mahomed H, Ndwandwe D. Missed opportunities for vaccination and associated factors among children attending primary health care facilities in Cape Town, South Africa: a pre-intervention multilevel analysis. Vaccines. 2022;10. doi:10.3390/vaccines10050785.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):37. doi:10.1186/1748-5908-7-37.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6:42. doi:10.1186/1748-5908-6-42.
- Barker F, Atkins L, de Lusignan S. Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. Int J Audiol. 2016;55(3):S90–8. doi:10.3109/14992027.2015.1120894.
- National Department of Health (NDoH), Statistics South Africa (Stats SA), South African Medical Research Council (SAMRC), and ICF. South Africa demographic and health survey 2016: key indicators. Pretoria (South Africa): NDoH, Stats SA, SAMRC, and ICF; 2019, p. 1–59. https://dhsprogram.com/publications/publication-fr337-dhs-final-reports.cfm
- Western Cape Provincial Department of Health. Cape metro district health plan 2018-2020 [accessed 2020 Jan 31]. http://www.health.gov.za/DHP/docs/DHP2018-21/Western_Cape/Metro_District_Health_Plan.pdf
- Ndwandwe D, Nnaji CA, Mashunye T, Uthman, OA, Wiysonge, CS. Incomplete vaccination and associated factors among children aged 12–23 months in South Africa: an analysis of the South African demographic and health survey 2016. Hum Vaccin Immunotherap. 2021;17(1):247–54. doi:10.1080/21645515.2020.1791509.
- Dodgson JE. Reflexivity in qualitative research. J Hum Lact. 2019;35(2):220–22. doi:10.1177/0890334419830990.
- Brooks J, McCluskey S, Turley E, King N. The utility of template analysis in qualitative psychology research. Qual Res Psychol. 2015;12(2):202–22. doi:10.1080/14780887.2014.955224.
- Cassell CM, Symon G. Qualitative organizational research: core methods and current challenges. London: Sage Publications Ltd; 2012. p. 408–96.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. doi:10.1097/ACM.0000000000000388.
- Fatiregun AA, Lochlainn LN, Kaboré L, Dosumu M, Isere E., Olaoye I, Akanbiemu FA, Olagbuji Y, Onyibe,R, Boateng K, Banda R, et al. Missed opportunities for vaccination among children aged 0–23 months visiting health facilities in a southwest State of Nigeria, December 2019. PloS One. 2021;16(8):e0252798. doi:10.1371/journal.pone.0252798.
- Kaufman J, Ryan R, Walsh L, Horey, D, Leask, J, Robinson, P, Hill, S. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2018;5: Cd010038 doi: 10.1002/14651858.CD010038.pub3.
- Saeterdal I, Lewin S, Austvoll-Dahlgren A, Glenton C, Munabi-Babigumira S Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst Rev. 2014: Cd010232. doi:10.1002/14651858.CD010232.pub2.
- Olorunsaiye CZ, Langhamer MS, Wallace AS, Watkins ML Missed opportunities and barriers for vaccination: a descriptive analysis of private and public health facilities in four African countries. Pan Afr Med J. 2017;27:6. doi:10.11604/pamj.supp.2017.27.3.12083.
- Cutilli CC. Seeking health information: what sources do your patients use? Orthopedic Nursing. 2010;29(3):214–19. doi:10.1097/NOR.0b013e3181db5471.
- Lieu TA, McGuire TG, Hinman AR. Overcoming economic barriers to the optimal use of vaccines. Health Aff Project Hope. 2005;24(3):666–79. doi:10.1377/hlthaff.24.3.666.
- Barello S, Maiorino G, Palamenghi L, Torri C, Acampora M, Gagliardi L. Exploring the motivational roots of getting vaccinated against covid-19 in a population of vaccinated pediatric healthcare professionals: evidence from an Italian cross-sectional study. Vaccines. 2022;10(3):467. doi:10.3390/vaccines10030467.
- Tarrant M, Gregory D. Exploring childhood immunization uptake with first nations mothers in north-western Ontario, Canada. J Adv Nurs. 2003;41(1):63–72. doi:10.1046/j.1365-2648.2003.02507.x.
- McKee C, Bohannon K. Exploring the reasons behind parental refusal of vaccines. J Pediatr Pharmacol Ther. 2016;21(2):104–09. doi:10.5863/1551-6776-21.2.104.
- Geoghegan S, O’Callaghan KP, Offit PA. Vaccine safety: myths and misinformation. Front Microbiol. 2020;11:372. doi:10.3389/fmicb.2020.00372.